Introduction
The clinical evaluation process plays a crucial role in ensuring the safety and effectiveness of medical devices. It involves a thorough review of clinical data, both before and after a device enters the market, to support its claims of safety, performance, and therapeutic efficacy. The goal is to gather solid clinical evidence that not only supports the device's intended use but also establishes its risk-benefit balance compared to existing treatments.
Adhering to stringent regulations and promoting transparency are essential in this process. In this article, we will explore the purpose and scope of clinical evaluation, key components of a clinical evaluation plan template, the impact of device classification on clinical evaluation, and step-by-step guidance on creating a comprehensive plan. By following these guidelines, device manufacturers can ensure the safety and effectiveness of their products throughout their lifecycle.
Understanding the Purpose and Scope of Clinical Evaluation
The assessment procedure is fundamental in ensuring that medical instruments are both safe and efficient for patient use. This meticulous procedure entails a comprehensive examination of all pertinent medical data, encompassing both pre- and post-market studies, to substantiate a product's assertions of safety, functionality, and therapeutic effectiveness. The ultimate goal is to collect strong medical proof that not only backs the intended use of the apparatus but also validates its risk-benefit balance in comparison to existing treatment alternatives.
For example, the advancement of machine learning/artificial intelligence medical equipment (Names) is similar to the introduction of a new pharmaceutical agent, necessitating a series of developmental milestones, crucial assessments for safety and effectiveness, and eventual acceptance by healthcare providers and coverage by payers. The journey from conception to successful adoption sets a high bar, paralleling the stringent pathways navigated by new drug entities.
To navigate the intricacies of clinical evaluation, manufacturers must comply with rigorous Medical Device Reporting (MDR) regulations. This includes diligent reporting of unfavorable events by healthcare personnel, which contributes to a deeper comprehension of equipment risks and improves patient safety. Such compliance is not just regulatory; it is a cornerstone of responsible gadget stewardship as articulated by the FDA's guidance for industry and consumer education.
Within this landscape, the role of transparency is paramount. It entails the clear communication of critical information about a medical instrument, including its intended use, development, performance, and underlying logic, to relevant stakeholders. This transparency is essential for conveying the potential impact on risks and patient outcomes, ensuring that users have the necessary information within the appropriate context.
The development of a assessment plan template must consider the complete range of the device's lifecycle, from design to deployment in healthcare settings. In this context, service design becomes critical, as it considers the experiences and requirements of all stakeholders involved in patient care, including clinicians, nurses, and hospital maintenance staff, who all play vital roles in the efficacy of patient outcomes.
To demonstrate the importance of assessing patients, consider the commentary by an industry expert with over 30 years in healthcare who emphasizes the significance of thorough analysis and organized presentation of medical data. Discrepancies in documentation, such as reports on medical assessment and files on risk management, can weaken the reliability of the conclusions derived from the data. Similarly, post-market surveillance data, though often underutilized, should be subjected to the same level of scrutiny as primary data to maintain the integrity of clinical evaluations.
Highlighting the significance of comprehensive risk management in the healthcare apparatus industry, Bijan Elahi, with almost thirty years of expertise, emphasizes the requirement for coherent reasoning and assurance among professionals. In 'Safety Risk Management for Healthcare Equipment - Second Edition', Elahi provides an invaluable resource, offering clarity on complex topics like defining risk acceptance criteria and ensuring compliance with ISO 14971, the international standard for healthcare equipment risk management.
In the end, the extent of the examination covers a thorough analysis that not only evaluates the equipment's risk-benefit profile but also situates it within the wider framework of technological advancement and patient-focused treatment, as exemplified by industry pioneers like Medtronic. Their objective to relieve suffering, restore well-being, and prolong life reflects the overarching aim of evaluation in the healthcare field—to provide transformative health advantages safely and efficiently.
Key Components of a Clinical Evaluation Plan Template
Creating a thorough assessment strategy for healthcare products is an essential stage in guaranteeing the safety and effectiveness of healthcare items. This systematic process involves several key components designed to gather the required clinical evidence.
The description of the equipment should include a comprehensive explanation of the medical instrument, outlining its function, indications for use, and technical features. It is crucial for clinicians to have a clear understanding of these specifications to ensure proper application.
Recognizing and gathering medical information, which may involve medical examinations, post-market medical follow-up, and examination of scientific literature, establishes the foundation of the medical assessment. This data must be collected according to robust methodologies and study designs, tailored to the device being evaluated. Design considerations involve the precise definition of the study population, appropriate sample size calculations, endpoints selection, and the statistical analysis plan.
Data collection and analysis procedures must be meticulously planned, describing data management practices, monitoring strategies, and the statistical methods to be employed. The analysis should be thorough, aligning with the insights from the evaluation report (CER) and risk management files to maintain consistency across all documentation.
Risk management is integral to the CEP, detailing how device-related risks will be systematically identified, evaluated, and mitigated during the clinical assessment phase. Moreover, the plan must address regulatory compliance, ensuring adherence to the applicable regulatory frameworks and guidelines, such as those established by the FDA.
The significance of active post-market surveillance is emphasized by statistics indicating that, during a 10-year timeframe, over 1.7 million injuries and 83,000 deaths in the United States were potentially associated with medical instruments. Thus, the CEP should include strategies for ongoing evidence review to detect safety issues that may emerge after the product enters the market.
By including these essential components, the assessment strategy transforms into a strategic record that not just aids in regulatory submissions but also directs the ongoing surveillance of the product throughout its lifespan.
Classification of Medical Devices and Its Impact on Clinical Evaluation
Categorizing medical instruments is crucial in influencing the course of evaluations in healthcare. These tools are categorized based on their usage, risk factors, and level of invasiveness. This categorization system is essential for both regulatory agencies and manufacturers in determining the required resources and the extent of evidence needed for each category.
-
Class I Devices: Considered low-risk, Class I products usually go through general controls. Although a wealth of empirical information may not be necessary, these instruments frequently must exhibit comparability to established prototype instruments.
-
Class II Products: Representing a moderate risk, Class II products necessitate supplementary controls for ensuring safety and effectiveness. The process of assessing these products typically involves a greater volume of data from medical sources, which can include trials and post-market surveillance efforts.
-
Class III Instruments: At the high-risk spectrum, Class III instruments are subject to the most rigorous regulatory demands. Their clinical evaluations usually call for thorough clinical trials, extended follow-ups, and a comprehensive collection of clinical data.
For example, Software as a Medical Instrument (Sand) that meets the FDA's standards for a Class III apparatus necessitates meticulous attention to detail. Identifying the classification entails referring to the Code of Federal Regulations (21 CFR Parts 862-892) where more than 1,700 kinds of products are categorized. The FDA’s classification database offers an additional resource for manufacturers to determine the risk class of their product by searching with the product’s name.
In the field of cutting-edge technologies, artificial intelligence (AI) is establishing a substantial presence in the development of healthcare equipment. The majority of AI technologies approved for healthcare use are designed to assist physicians in tasks such as diagnosing radiologic and pathologic abnormalities, medicine dosing, and disease progression prediction. With AI’s ability to learn through algorithmic data processing, developers must ensure that the technology is capable of generalizing beyond the training data to produce accurate, unseen solutions.
The field of healthcare equipment regulation is constantly changing. Significantly, the Medicines and Healthcare products Regulatory Agency (MHRA) recently declared a policy aimed at the global acceptance of healthcare instruments, indicating a flexible method to regulatory harmonization.
Recognizing the importance of transparency, the FDA emphasizes that information regarding the intended use, development, performance, and logic of a Machine Learning Medical Device (MLMD) should be clearly communicated. This ensures that information potentially impacting risk and patient outcomes is disclosed to relevant stakeholders.
Prior to marketing a product in the U.S., it is vital to determine the accurate FDA classification to select the suitable registration pathway, which can be Premarket Notification (510(k)), Premarket Approval (PMA), or the De Novo process, with the product needing to be either FDA Cleared, Approved, or Granted.
With the introduction of new technologies, industry leaders like Medtronic continue to deliver innovative solutions. Medtronic’s worldwide existence and extensive array of health technologies—spanning from cardiac apparatus to surgical robotics—showcase the company's dedication to improving patient care through knowledge-driven technologies.
The utilization of agreement norms, created by Standards Development Organizations (SDOs) following the rules of openness and fair treatment, is essential to the regulatory quality of healthcare apparatus. Conformity assessments and standard utilization play a crucial role in promoting innovation and standardization, which is necessary for patient access to new healthcare equipment.
As the healthcare equipment industry progresses, specialists like Bijan Elahi underscore the significance of thorough safety risk management. Elahi's vast expertise and contributions to the field are priceless assets for those involved in risk management of instruments used in the medical field.
Creating a Clinical Evaluation Plan: Step-by-Step Guide
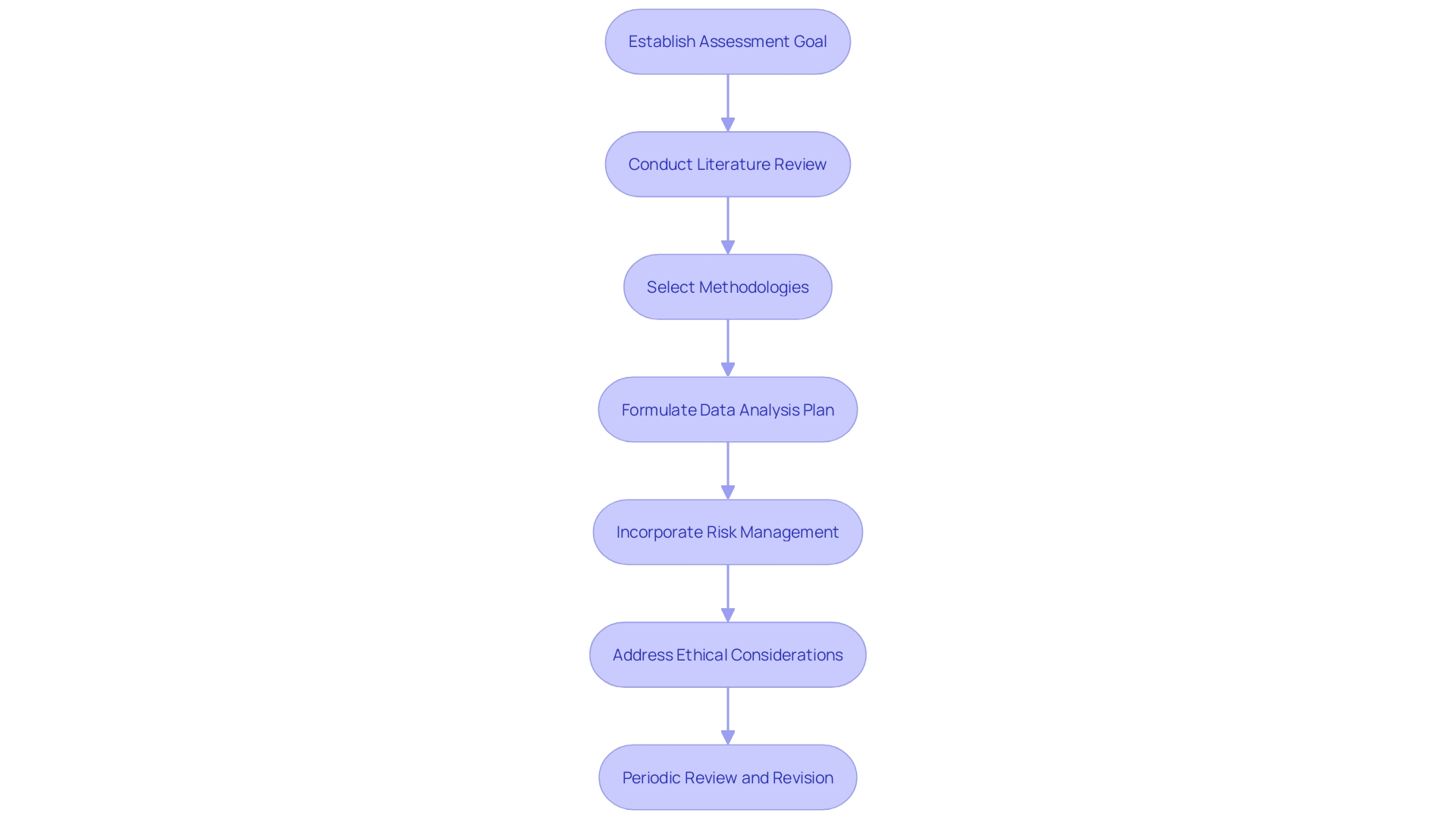
In order to create a comprehensive assessment strategy for a medical instrument, it is crucial to adopt a thorough and organized method. Start by establishing the goal of the assessment, outlining the particular inquiries that need to be answered and the kind of evidence necessary to confirm the safety and effectiveness of the apparatus. Next, familiarize yourself with the pertinent regulations and guidelines, such as those issued by the FDA, to ensure your plan adheres to all necessary compliance requirements.
A thorough examination of the literature is essential for comprehending the available information on comparable devices, which aids in determining the present status of the field and pinpointing areas where knowledge is lacking. Identifying the required data types is a subsequent step; this may include data from investigations, post-market surveillance, and existing scientific literature.
Selecting the right methodologies and study designs is essential for gathering the required data effectively. Considerations include the target study population, sample size, endpoints, and statistical methods for data analysis. To maintain consistency in data collection, develop standardized tools like case report forms.
Formulate a data analysis plan, specifying the statistical techniques to be employed. Risk management must also be incorporated into the assessment strategy to anticipate, assess, and mitigate potential risks linked to the equipment. Ethical considerations, including informed consent and the safeguarding of patient privacy, are non-negotiable aspects of the plan.
It is imperative to periodically review and revise the plan to integrate new findings, address emergent risks, and accommodate regulatory changes. Such diligence ensures a thorough and effective clinical evaluation process.
Given the latest advancements made by the MHRA concerning the worldwide acknowledgement of healthcare equipment, it is becoming more crucial to take into account global regulatory environments when developing these strategies. This not only ensures safety and quality but also facilitates market access across different regions, benefiting patient health and supporting innovation.
Moreover, the strategy should consider the intricacies of the healthcare ecosystem, acknowledging that the effectiveness of healthcare equipment is influenced by a variety of participants, such as doctors, administrative personnel, and maintenance staff. A user-centered design philosophy that incorporates service blueprinting and holistic approaches can enhance the experience of all users, not just patients, ensuring that the technology functions optimally within the wider healthcare service structure.
By adhering to these guidelines and considering the broader healthcare context, a clinical evaluation plan can effectively support the lifecycle of a medical device, from its inception to its everyday use in clinical settings, ensuring it meets the evolving needs of all stakeholders involved.
Conclusion
In conclusion, the clinical evaluation process is crucial for ensuring the safety and effectiveness of medical devices. Adhering to regulations and promoting transparency are essential in this process. A comprehensive clinical evaluation plan template is a critical component, including a device description, identification of clinical data, data collection and analysis procedures, risk management strategies, and regulatory compliance considerations.
The classification of medical devices shapes the trajectory of evaluations, with different categories requiring varying levels of evidence. Creating a clinical evaluation plan involves a structured approach, including defining the objective, conducting a literature review, selecting methodologies, formulating a data analysis plan, and integrating risk management. Considering the broader healthcare context and involving stakeholders are vital in creating an effective plan.
By following these guidelines, manufacturers can ensure the safety and effectiveness of their products, delivering innovative solutions that enhance patient care and improve health outcomes.




