Introduction
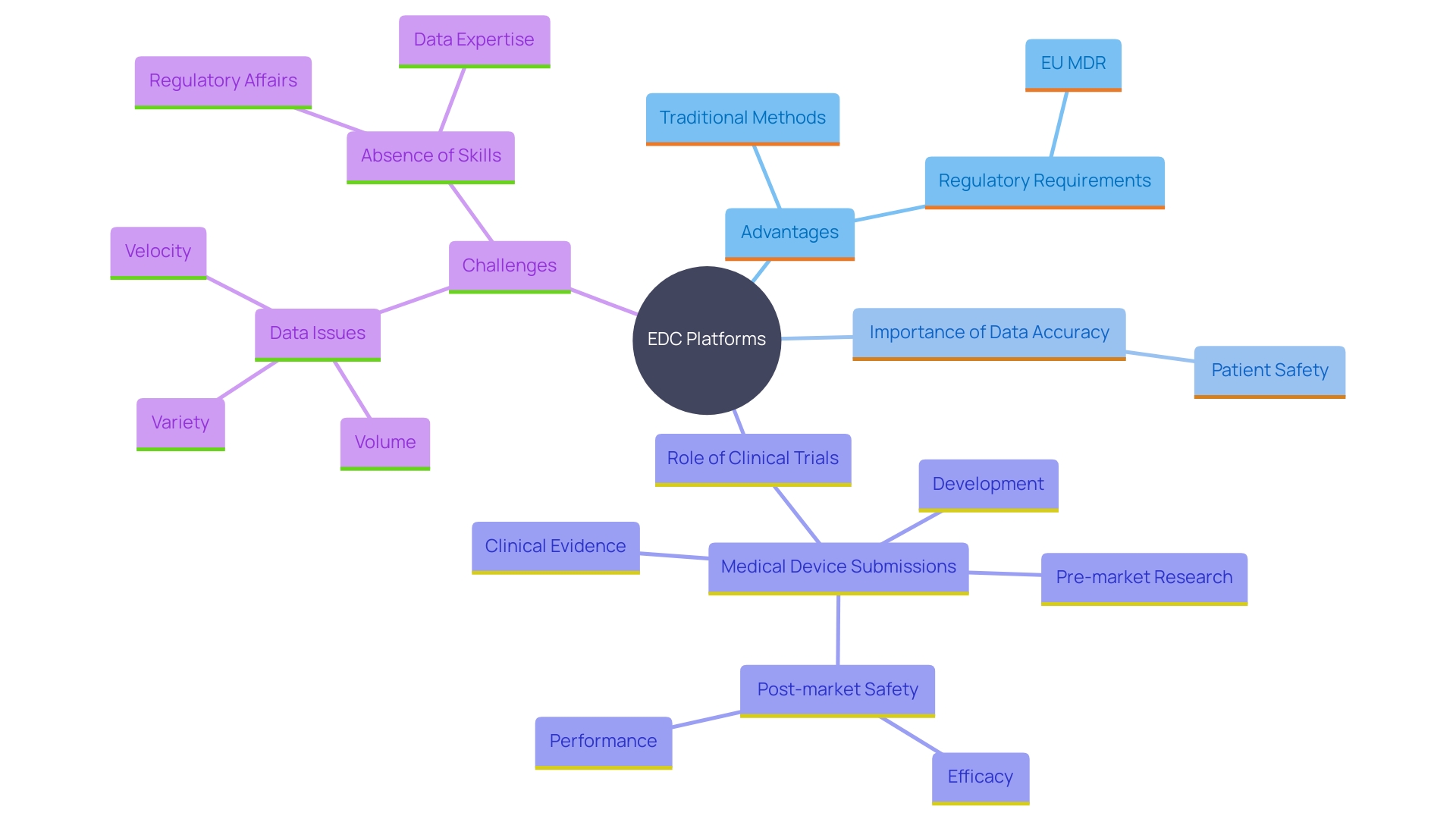
The landscape of clinical trials is undergoing a significant transformation with the advent of Electronic Data Capture (EDC) systems. These advanced digital solutions are designed to enhance the collection, management, and analysis of clinical trial data, moving away from traditional, paper-based methods. EDC systems enable real-time data entry and retrieval, which not only increases efficiency but also ensures compliance with stringent regulatory standards.
Accurate data management is crucial for patient safety and regulatory submissions, as highlighted by global health authorities. This article delves into the myriad benefits of using EDC systems in clinical trials, explores their key features, offers guidance on selecting the right system, and outlines best practices for successful implementation. Furthermore, it examines the critical role of regulatory compliance and provides a forward-looking perspective on the future of EDC systems in clinical research.
What is an Electronic Data Capture (EDC) System?
An Electronic Data Capture (EDC) platform is a sophisticated digital solution created to enhance the gathering, management, and examination of research information. In contrast to conventional paper-based approaches, EDC platforms allow for immediate information entry and access, greatly enhancing the effectiveness of clinical trials. These systems not only ensure adherence to regulations but also uphold information accuracy and consistency, which are essential for dependable outcomes. 'According to the World Health Organization, there are approximately two million different kinds of medical devices on the market globally, making precise information management essential for patient safety and regulatory submissions.'. Article 62 of the European Union Medical Device Regulation (EU MDR) stresses that research must safeguard the rights and welfare of participants while producing scientifically valid and strong information. In the U.S., approximately 10-15% of successful 510(k) submissions for Class II devices and all Class III devices depend on extensive clinical trials, highlighting the significance of efficient information management frameworks in ensuring the safety and efficacy of medical devices.
Benefits of Using EDC Systems in Clinical Trials
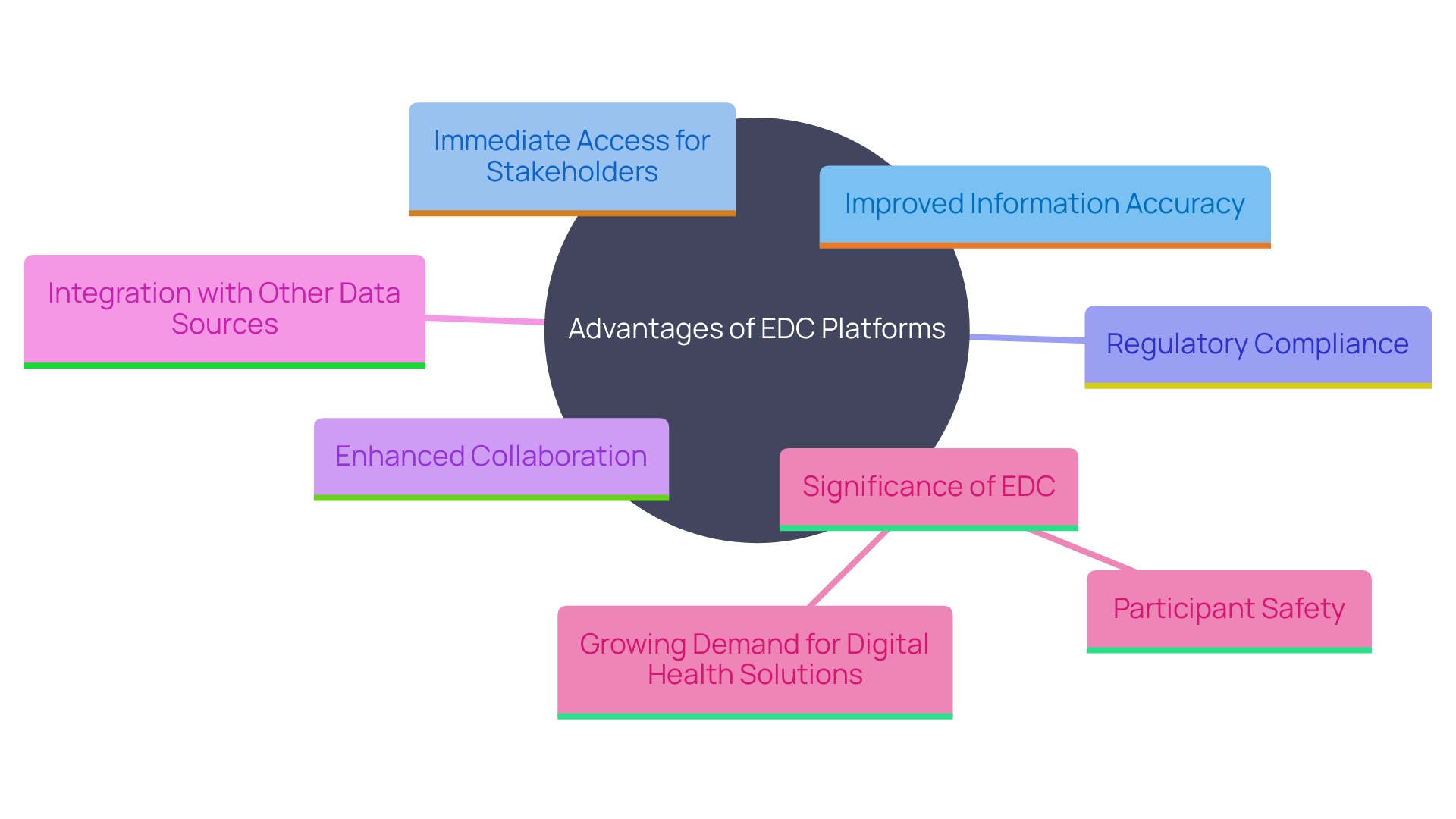
Electronic Information Gathering (EDC) platforms provide numerous benefits compared to conventional collection techniques. These advantages encompass notably improved information precision by reducing manual input mistakes, immediate access to information for all stakeholders, and better adherence to strict regulatory standards. 'EDC solutions enhance information analysis and reporting procedures, which leads to faster trial schedules and lower expenses.'. Additionally, they facilitate superior collaboration among research teams, contributing to more efficient project management.
Clinical information management is essential for ensuring the safety and efficacy of medical devices and pharmaceuticals. Robust EDC frameworks play a crucial role in this process. For example, as mentioned in the European Union Medical Device Regulation (EU MDR), research studies must prioritize the rights, safety, dignity, and well-being of participants while ensuring that the information generated is scientifically valid, reliable, and robust. This adherence to strict standards not only protects participants but also provides the necessary proof to regulatory bodies that a device is safe and effective for its intended use.
The increasing demand for digital health solutions and the complexity of global medical device regulations further underscore the importance of efficient EDC systems. As the Software as a Medical Device (SaMD) market keeps expanding, with an expected compound annual growth rate of around 52% from 2023 to 2028, the necessity for precise and dependable health information becomes increasingly important.
Furthermore, the gathering of research information has traditionally been a time- and labor-consuming procedure, frequently missing simultaneous information from alternative sources that could offer useful insights. EDC frameworks tackle these limitations by incorporating information from different origins, such as electronic health records (EHRs) and real-world information, thus improving the validity and generalizability of trial findings. Public and private funding in health information digitization and interoperability have made significant progress in this area, further facilitating the adoption of advanced electronic capture solutions.
In summary, EDC solutions not only enhance data management and compliance but also speed up research timelines and lower expenses. By utilizing these frameworks, research groups can attain more precise, effective, and cooperative results in medical studies.
Key Features of EDC Systems
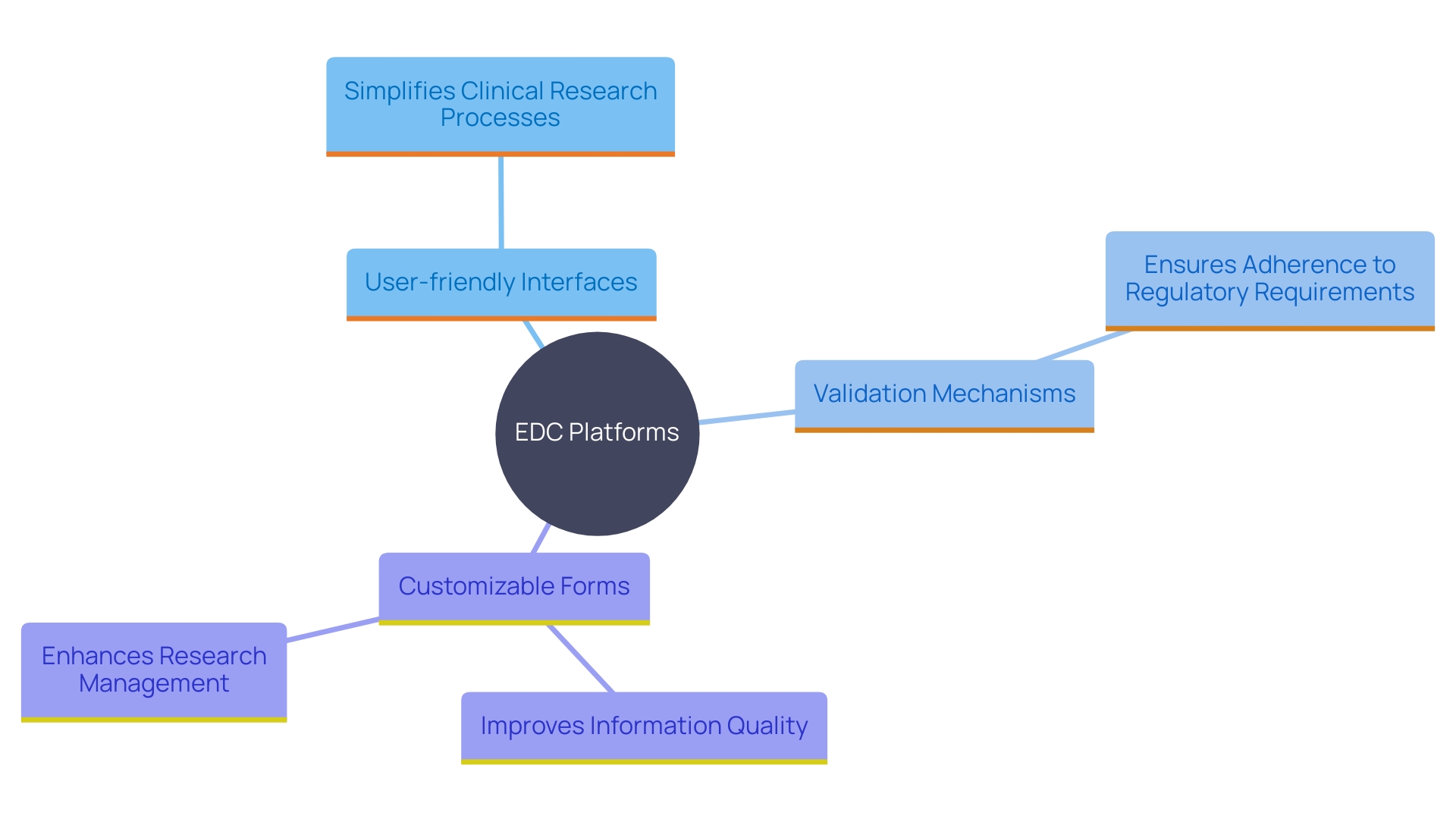
Contemporary EDC platforms are now outfitted with a variety of sophisticated functionalities intended to simplify clinical research procedures and guarantee adherence to regulatory requirements. One of the key features is the user-friendly interface that simplifies information entry, making it accessible even for those with minimal technical expertise. These systems also provide strong validation mechanisms to maintain high information quality, reducing the risk of errors that can compromise trial outcomes.
Customizable forms are another important aspect, enabling researchers to adjust information gathering to meet the specific needs of their studies. This flexibility ensures that all necessary information points are captured accurately and efficiently. Furthermore, the integration of electronic signatures and audit trails not only enhances information integrity but also ensures compliance with stringent regulatory requirements, such as those outlined in the European Union Medical Device Regulation (EU MDR).
Furthermore, EDC frameworks frequently feature export functionalities, enabling smooth information sharing among stakeholders and enhancing openness. This is especially crucial for upholding regulatory adherence and for the effective management of research studies. The incorporation of these attributes into contemporary electronic records platforms tackles numerous obstacles encountered in healthcare information administration, such as information quality concerns and the effort involved in establishing studies, ultimately resulting in more effective and trustworthy research evaluations.
Choosing the Right EDC System for Your Clinical Trial
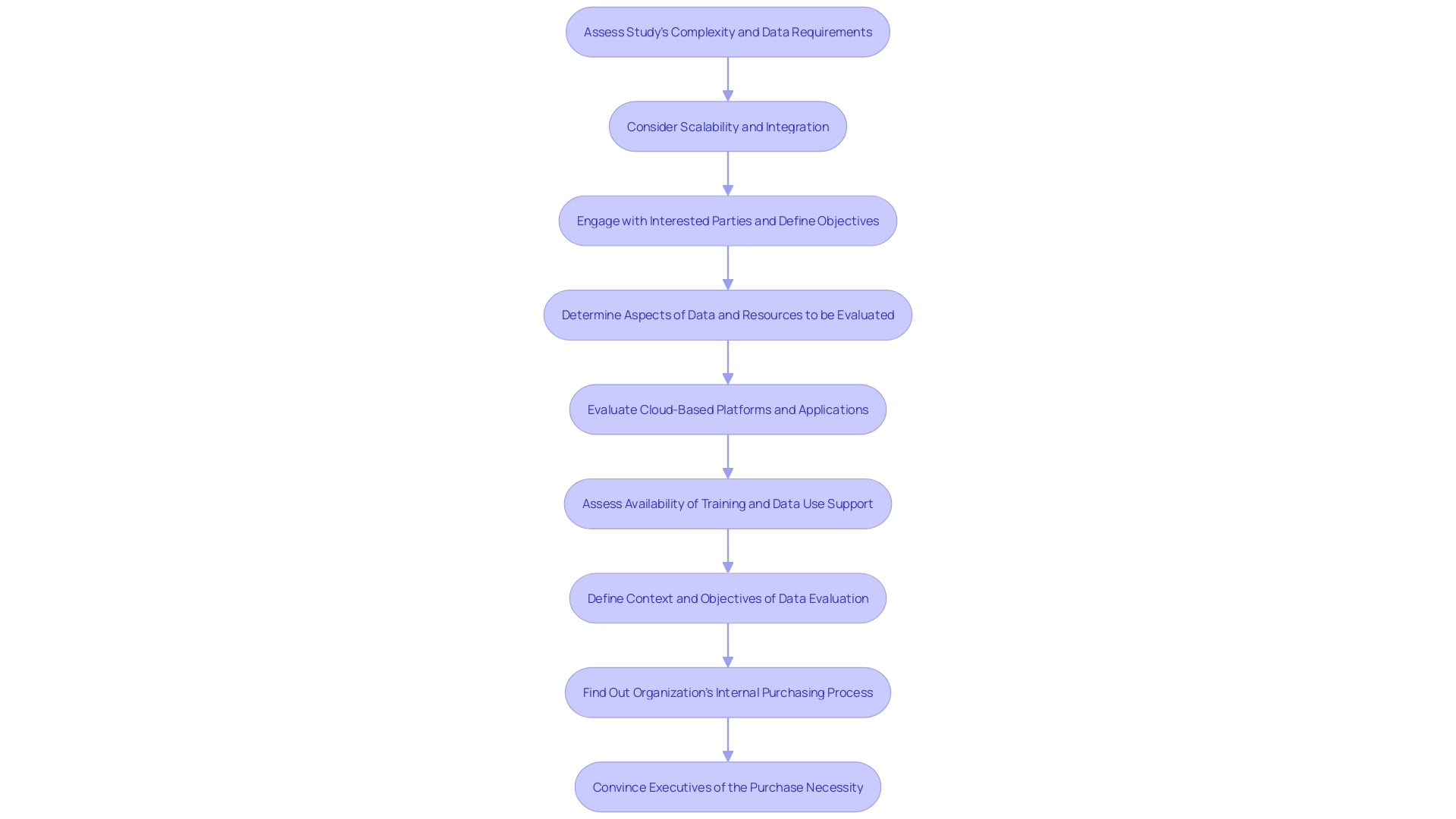
Selecting the appropriate Electronic Data Capture (EDC) solution is essential for the success of clinical trials. Key considerations include the study's complexity, the number of involved sites, and specific data requirements. Assessing the scalability, user support, and integration capabilities with other platforms is essential. For instance, systems like those approved by the European Medicines Agency and the US Food and Drug Administration, after studies at institutions like Memorial Sloan Kettering Hospital, have demonstrated significant reductions in human error and site burden. Additionally, a thorough cost-benefit analysis is essential. This process should address challenges such as data quality issues and compliance with clinical standards like ISO 14155:2020. Engaging stakeholders and defining objectives early in the evaluation process can lead to more informed decisions that align with the trial's needs.
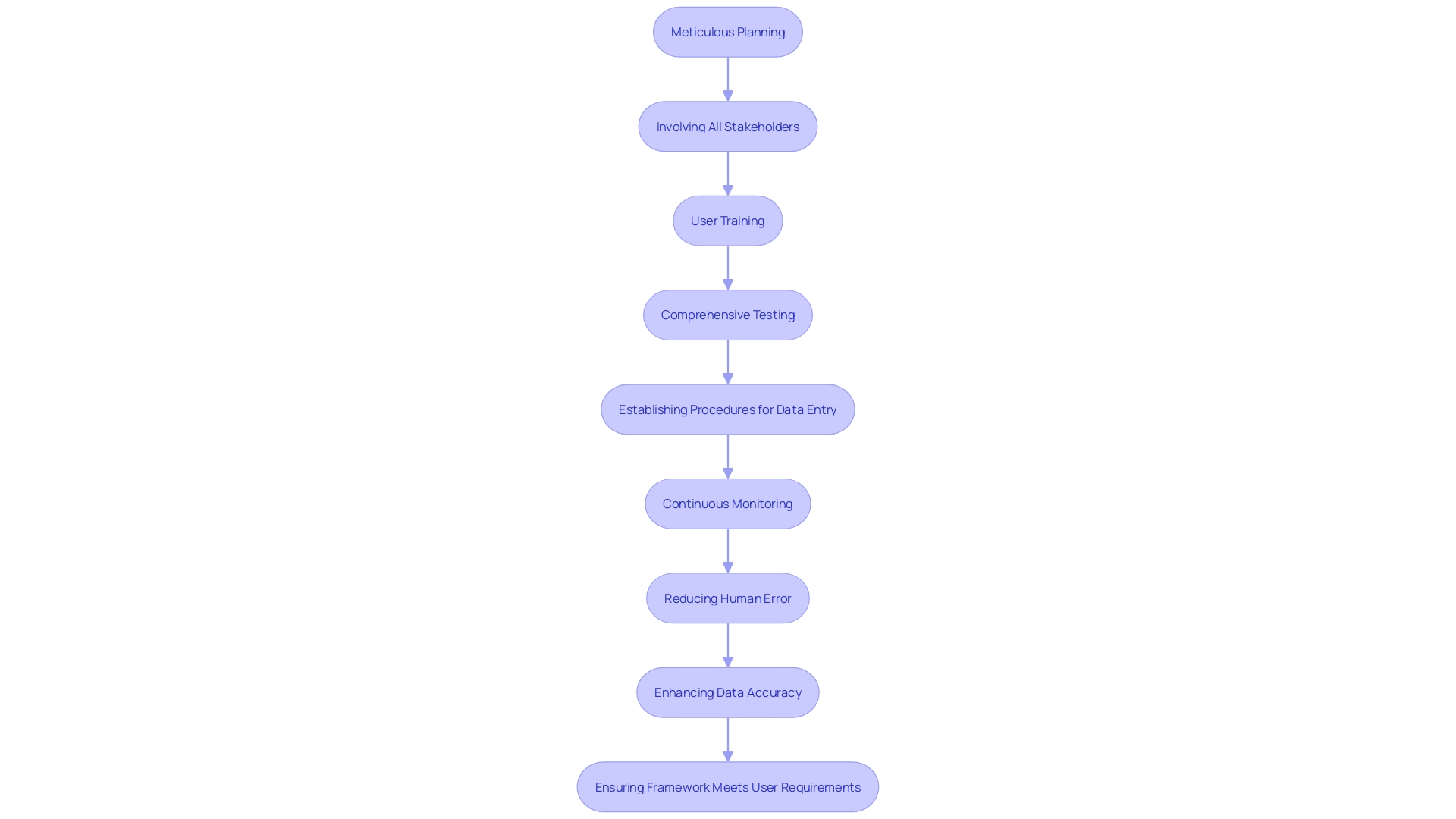
Implementing EDC Systems: Best Practices
'Implementing EDC processes effectively demands meticulous planning and execution.'. Involving all pertinent parties from the beginning is essential to guarantee that the framework fulfills the requirements of all users. Thorough instruction of users is essential to enhance utility and reduce mistakes, considering that human error in manual information transfer can result in considerable inaccuracies. Comprehensive testing prior to complete rollout assists in recognizing and addressing possible problems early, guaranteeing the reliability of the setup.
Setting up clear procedures for information entry and management is crucial, especially since clinical research information frequently comes from multiple origins, such as electronic health records and real-world information. Continuous monitoring and feedback mechanisms must be in place to ascertain that the framework operates optimally throughout the trial. This approach not only enhances information accuracy and reduces site burden but also lowers research and development costs by minimizing errors.
Public and private sector initiatives, such as those propelled by federal legislative actions in the US, have advanced health information interoperability and standards, establishing a strong framework for EDC frameworks. Utilizing current health IT resources can further improve information accessibility and application in research, addressing gaps in information gathering and enhancing the validity and generalizability of study results.
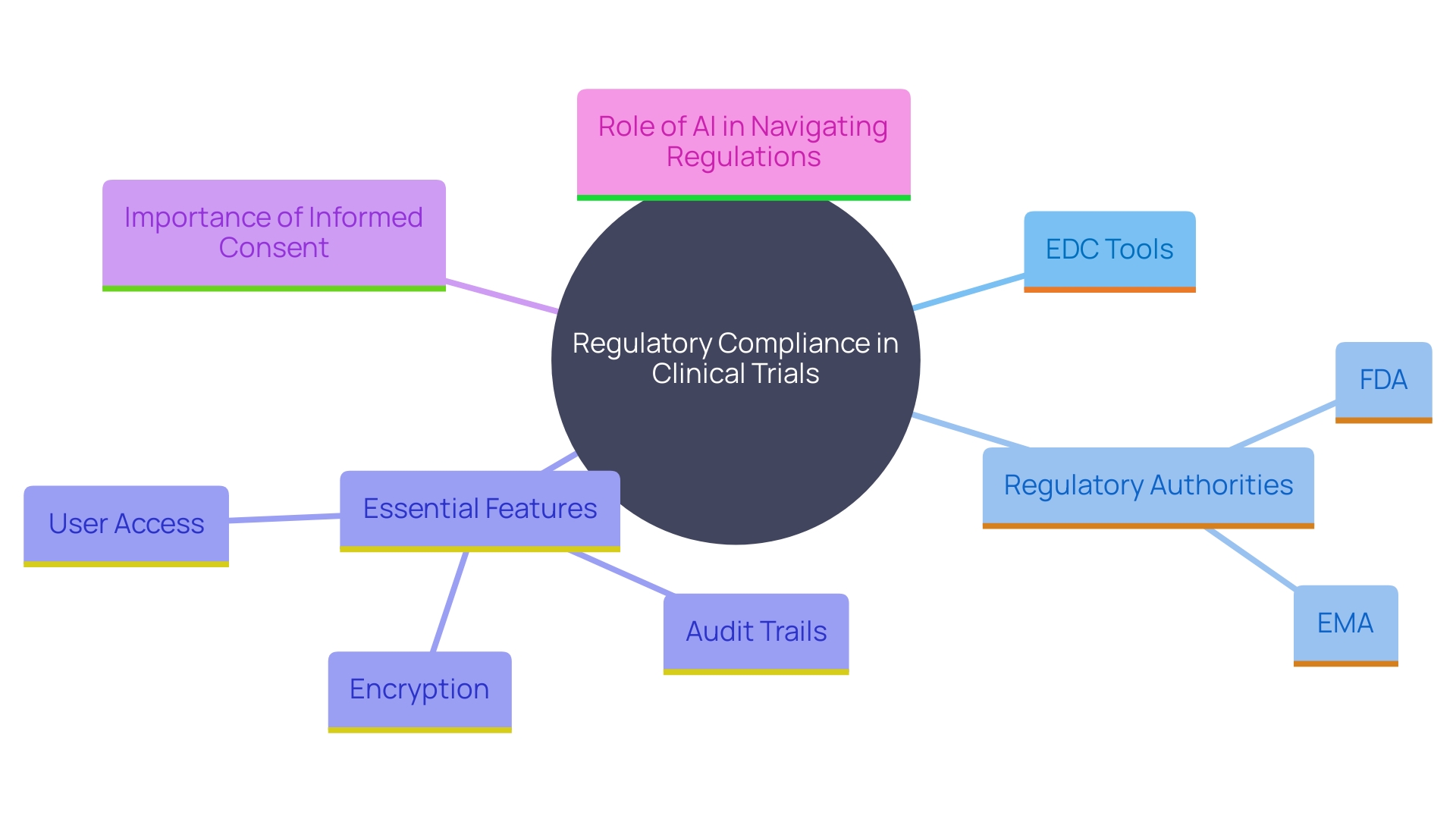
Regulatory Compliance and EDC Systems
Ensuring regulatory compliance is a critical aspect of clinical trials, and Electronic Data Capture (EDC) tools are central to this process. These frameworks must adhere to guidelines set by regulatory authorities such as the FDA and EMA, which require strong features like audit trails, information encryption, and secure user access controls. The FDA emphasizes the importance of well-designed studies and reliable data to support the safety and effectiveness of medical products, aligning with their public health mission to advance medical research.
To stay compliant with evolving regulations, EDC platforms require regular updates and maintenance. This is particularly relevant in the context of global medical device regulations, where the Same market is experiencing significant growth. Navigating this complex regulatory landscape necessitates a firm grasp of regional nuances, documentation requirements, and compliance processes. Leveraging AI-driven regulatory tools can streamline these processes by promptly alerting professionals to global updates and highlighting key changes.
'Informed consent, as mandated by regulations like 21 CFR Part 50, is a non-negotiable component of research trials.'. 'A compliant eConsent tool integrated within an EDC platform ensures that all records are securely stored and maintained, providing confidence in regulatory adherence.'. Moreover, the digitization of health records and public investment in health information connectivity have enabled greater standardization and interoperability, further improving regulatory compliance in medical research.
Future of EDC Systems in Clinical Trials
The future of EDC systems in research studies is marked by ongoing innovation and technological progress. A key trend is the integration of artificial intelligence (AI) and machine learning, which enhances information analysis and predictive modeling capabilities. As an FDA representative highlights, AI is being employed to examine extensive quantities of information from both research studies and observational investigations, providing greater insights and enabling more flexible and inclusive experiments.
Moreover, there is a growing utilization of mobile devices for data gathering, which simplifies procedures and reduces some of the challenges typically linked to medical studies. The increasing acceptance of decentralized research studies (DCTs) and digital health technologies (DHTs) also aid in the advancement of study designs and execution. The worldwide decentralized research market, for example, is anticipated to expand at a compound annual growth rate of 30.1% from 2021 to 2026.
As research trials progress, EDC systems are concentrating more on enhancing patient involvement and information interoperability. The use of connected devices, wearables, and electronic diaries enables the gathering of more comprehensive patient-reported information and real-world insights. This not only enhances the information reservoir but also offers a more comprehensive perspective on a participant's health, capturing insights beyond the limits of medical environments.
Public investment in the digitization of health records has supported initiatives to standardize health information elements and achieve greater connectivity and interoperability. Significant federal legislative measures in the US, such as the Health Information Technology for Economic and Clinical Health (HITECH) Act, have spurred advancements in this area. The capacity to combine information from diverse origins will ultimately create opportunities for more efficient and effective research, addressing the critical need for strong evidence in healthcare.
In summary, the future of EDC systems in clinical trials is set to be transformative, driven by AI, mobile technology, and enhanced data interoperability, which together will lead to more patient-centered and data-rich research methodologies.
Conclusion
The transition from traditional paper-based methods to Electronic Data Capture (EDC) systems marks a significant advancement in clinical trials. EDC systems enhance data collection, management, and analysis, ensuring compliance with regulatory standards while maintaining accuracy and integrity. Their role in ensuring patient safety and reliable outcomes is underscored by global health authorities.
These systems offer numerous benefits, including improved data accuracy, real-time access, and enhanced collaboration among research teams. By integrating data from various sources, EDC systems address historical limitations in clinical data collection, facilitating more efficient project management. As the demand for digital health solutions grows, the necessity for robust EDC systems becomes increasingly critical.
Key features, such as user-friendly interfaces and customizable forms, enhance the effectiveness of EDC systems. Selecting the right system requires careful consideration of study complexity and scalability, while best practices in implementation—like stakeholder engagement and comprehensive training—further contribute to success.
Regulatory compliance remains essential in clinical trials, with EDC systems playing a vital role in meeting established requirements. The ongoing evolution of these systems, driven by technological advancements and improved data interoperability, promises a future focused on enhanced patient engagement and comprehensive data collection.
In summary, EDC systems are transformative in clinical trials, promoting efficiency, accuracy, and compliance. Their continuous innovation will lead to more effective and patient-centered research, ultimately improving health outcomes.




