Introduction
Clinical Research Organizations (CROs) play a vital role in the advancement of medical research, bridging the gap between scientific discoveries and the delivery of new treatments to patients. They bring expertise in managing clinical trials, which are crucial for assessing the safety and efficacy of medical interventions. However, the industry faces challenges, including recruitment and retention of trial participants.
To address these challenges, the clinical trial landscape is evolving, with innovations in technology and a growing emphasis on diversity and inclusion. CROs are also exploring novel treatment avenues and facilitating participation in trials for patients with rare diseases. This commitment to advancing medical research is mirrored in the dedication of CRO professionals and trial participants.
As we navigate a post-pandemic world, the role of CROs in driving innovation, ensuring participant safety, and advancing global health remains more critical than ever.
Why CRO Firms Are Essential for Medical Research
Clinical Research Organizations (CROs) are indispensable in the progression of medical research, providing a bridge between groundbreaking scientific discoveries and the delivery of new treatments to patients. CROss offer expertise in managing the intricate process of clinical trials, which are essential for determining the safety and efficacy of new medications, vaccines, medical devices, and procedures. For instance, professionals like Chris, with extensive experience in the medical device field, contribute their expertise to optimize clinical study management, ensuring that pivotal and post-market studies meet rigorous standards.
One of the significant challenges faced by the industry is the recruitment and retention of trial participants. With 80% of clinical trials failing to complete on schedule, and a staggering 20% experiencing delays of six months or more, the issue is multifaceted. A primary cause is that 85% of studies do not retain enough patients, and two-thirds of trial sites fall short of enrollment targets.
This not only affects the timeline but also has a considerable financial impact on both trial sponsors and CROs.
To address these challenges, the clinical trial landscape is evolving. Innovations in data usage, technology, and integrated workflows are being employed to enhance the efficiency of clinical trials. The integration of AI and machine learning, for instance, is reimagining clinical research by improving patient recruitment strategies, particularly in areas like oncology.
Additionally, there is a growing emphasis on diversity, equity, and inclusion in clinical trials, especially concerning rare diseases. The ambition to create a more diverse participant base is crucial for the generalizability of trial results and the development of treatments that are effective across diverse populations.
CROs are also at the forefront of exploring novel treatment avenues, such as the promising field of psychedelic treatments, and addressing the complexities of manufacturing cell therapies. For patients with rare diseases or those residing in remote locations, CROss are instrumental in facilitating participation in clinical trials that may offer lifesaving opportunities, albeit with logistical challenges such as international travel.
The commitment to advancing medical research is mirrored in the dedication of CRO professionals and the enthusiasm of trial participants. As we continue to navigate a post-pandemic world, the role of CROs in driving innovation, ensuring participant safety, and advancing global health remains more critical than ever.
Enhanced Efficiency in Clinical Trials
Clinical research organizations (CROs) are pivotal in the advancement of medical science, offering not only their expertise in the domain but also harnessing innovative technologies to enhance the clinical trial process. By integrating advanced algorithms trained on extensive databases of clinical trial protocols, CROs are adept at producing initial drafts for essential documents such as protocols, patient materials, and trial plans. The utilization of machine learning models for real-time monitoring of trial data aids in promptly identifying discrepancies and potential safety concerns, thereby maintaining the integrity of the research and upholding participant safety.
In the complex field of CNS/neurology research, the value of multidisciplinary collaboration cannot be overstated. It's critical to engage both clinical operations specialists and patients to ensure that clinical trials are not only scientifically robust but also practically feasible in terms of participant recruitment and adherence to real-world treatment patterns. Reflecting on the challenges faced by trials with restrictive inclusion criteria, it's evident that patient-centric approaches and collaborative frameworks are essential for achieving success in clinical studies.
Moreover, data integration and the acceleration of research timelines are becoming increasingly important in clinical trials. Recent discussions at the Outsourcing in Clinical Trials conference and initiatives like the MHRA Patient Involvement Strategy underscore the evolving landscape of clinical research in the UK, emphasizing the need for patient involvement from the early stages and incorporating patient experiences to ascertain the safety and efficacy of new treatments. As the UK prepares for an election that could reshape its clinical trial infrastructure, the industry is reminded of the importance of optimizing each decision in the research process to enhance outcomes and efficiency.
Access to Specialized Expertise
Clinical Research Organizations (CROs) are at the forefront of medical innovation, offering a vast array of professional expertise across multiple therapeutic areas. These firms are essential in the progression of medical research, providing services that range from medical writing to complex statistical analyses and comprehensive regulatory support. Their teams consist of seasoned industry veterans and passionate newcomers who contribute to the development of new treatments and medical advancements.
CROss deliver personalized attention and scientific rigor, making them a preferred partner for biotech companies that value agility and direct access to high-level expertise. They play a pivotal role in ensuring that clinical trials are not only scientifically sound but also cost-effective and efficient, thus accelerating the journey of new therapies from concept to market. Furthermore, CROss are integral in supporting patient-centric trials, which may involve complex logistics such as cross-border travel, ensuring that even the most challenging studies are conducted with the utmost care for participants' experiences.
By engaging with a CRO, researchers are tapping into a collaborative and innovative environment that fosters meaningful change in healthcare.
Cost-Effective Solutions
The realm of clinical trials is pivotal in the advancement of medical treatments, yet it is accompanied by substantial financial implications. Contract Research Organizations (CROs) have emerged as strategic partners that offer a blend of infrastructure, specialized knowledge, and operational prowess to enhance the efficacy of these trials. These firms are adept at steering the complex logistics of trials, from vendor negotiations to meticulous resource management.
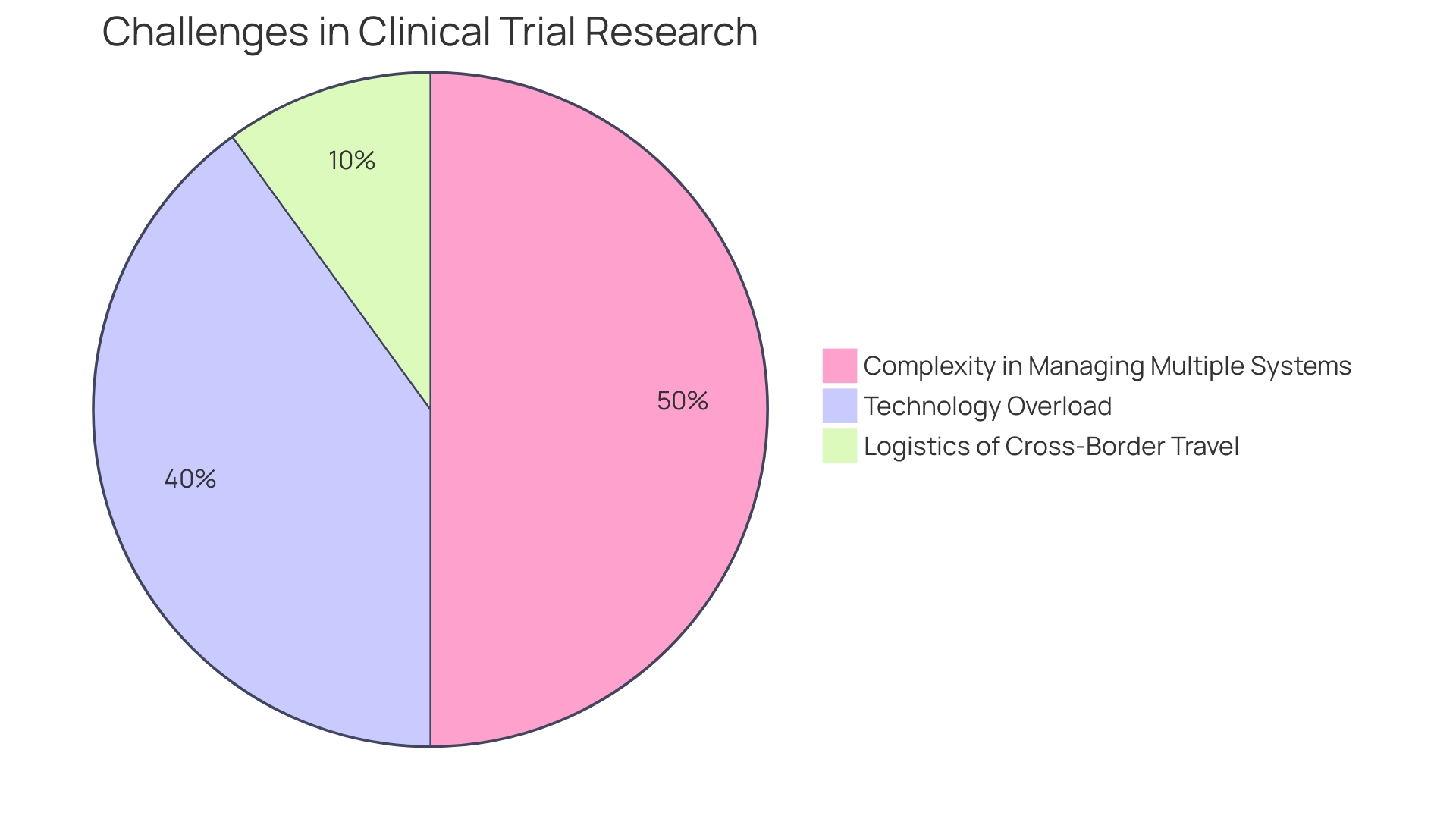
Their involvement ensures that the integrity of the research remains intact while optimizing expenses. Furthermore, the use of advanced technologies like Large Language Models for document drafting and machine learning for data monitoring underscores the innovative approaches CROss employ to streamline clinical trial processes. Such technological integration also addresses the issue of technological overload, which has been identified as a factor leading to longer trial durations and increased staff burnout.
By centralizing and simplifying the research workflow, CROss not only relieve the administrative burden but also contribute to the timely delivery of new medical solutions, ultimately benefiting patients in urgent need of novel treatments.
Improved Data Management
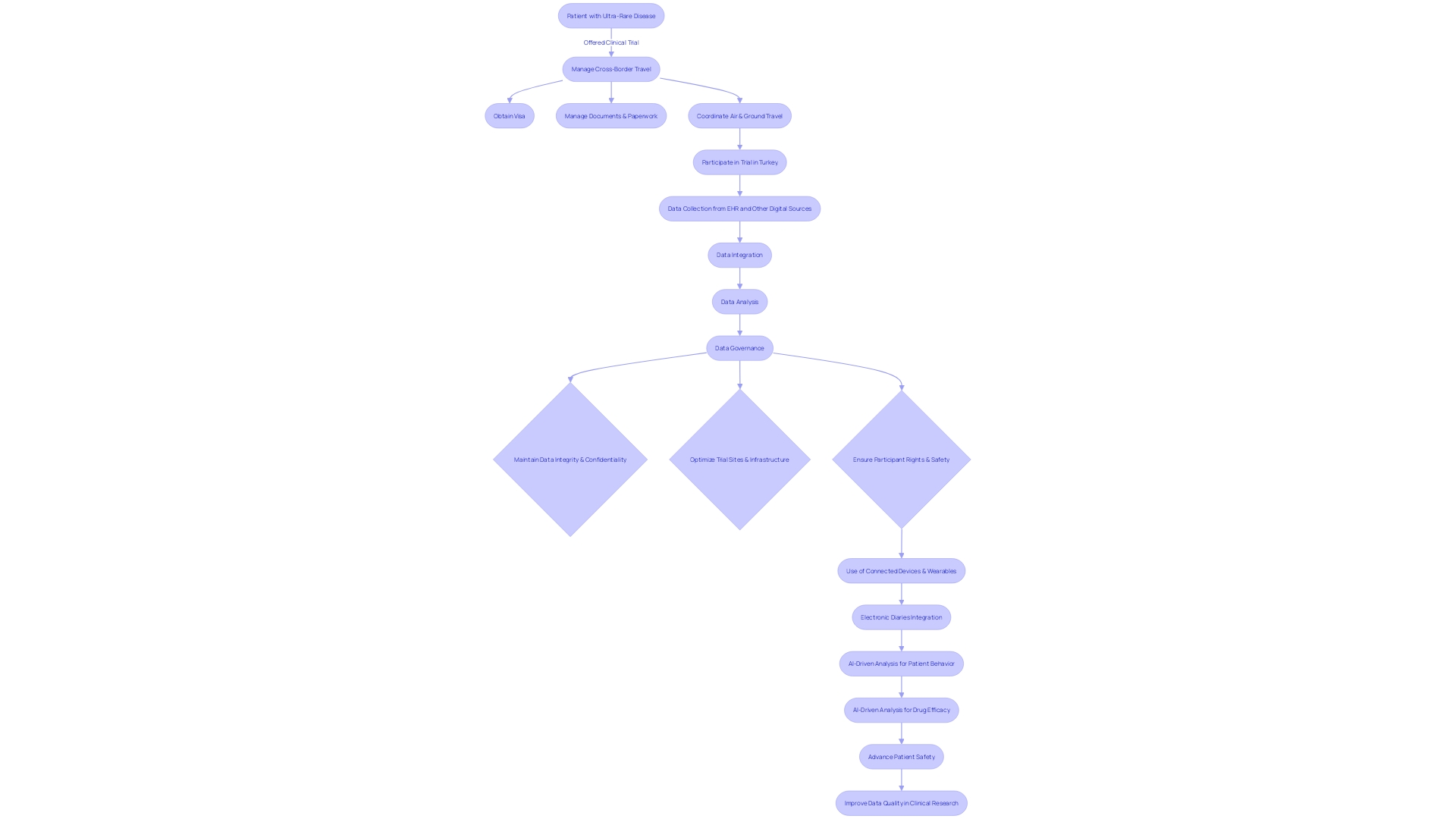
Clinical research organizations (CROs) are at the forefront of incorporating sophisticated data management systems to maintain the integrity and confidentiality of study data. With the implementation of electronic health records (EHR) and other digital data sources, CROss are tackling the challenges of EHR-sourced trials by ensuring that existing trial sites and infrastructures are optimized for operationalizing study goals. A demonstration project highlighted the use of EHR data to complement traditional data collection methods, emphasizing the importance of a central coordinating center to assist sites with technical, governance, and operational challenges.
The rapidly evolving landscape of clinical research demands a strategic approach to data management. The integration of connected devices, wearables, and electronic diaries has provided a wealth of patient-centered data, which, when coupled with AI-driven analysis, can yield profound insights into patient behavior and drug efficacy. However, the sheer volume of data necessitates a well-defined data strategy prior to protocol design.
This strategy must consider the optimal collection of both traditional and digital data sources and address the management of data flow.
Furthermore, the imminent update to the European good clinical practice (GCP) guidelines, with a dedicated section on data governance, underscores the necessity for stringent data management protocols. The guidelines advocate for clinical trials to be conducted with the utmost consideration for participant rights, safety, and the reliability of results, focusing on critical activities that are fundamental to achieving trial objectives.
CROs must navigate these expectations and strategies by employing teams skilled in ensuring the quality integration of digital data and its downstream processes. This includes addressing data review expectations across various disciplines, mitigating study risks through data collection and flow strategies, and ensuring that data flow allows for risk oversight and informed decision-making. The goal is to safeguard data integrity, minimize burdens on trial sites, and utilize data to its fullest potential to advance patient safety and data quality in clinical research.
Regulatory Compliance Support
Clinical trial companies are at the forefront of medical research, conducting studies that are essential for the advancement of healthcare and treatment options. The process of managing these trials is intricate, involving the navigation of stringent regulatory requirements to ensure patient safety and the integrity of the data collected. It is imperative for these companies to maintain a deep understanding of both local and international regulations to successfully guide a study through the complex regulatory landscape.
With the MHRA overseeing the regulation of all medicines and medical devices in the UK, it emphasizes the need for robust and fact-based judgments to balance the potential benefits of a treatment against any risks. Similarly, the FDA and the EU have proposed guidelines to address the challenges posed by emerging technologies like AI, adopting a risk-based approach to safeguard against potential compliance issues in clinical trials.
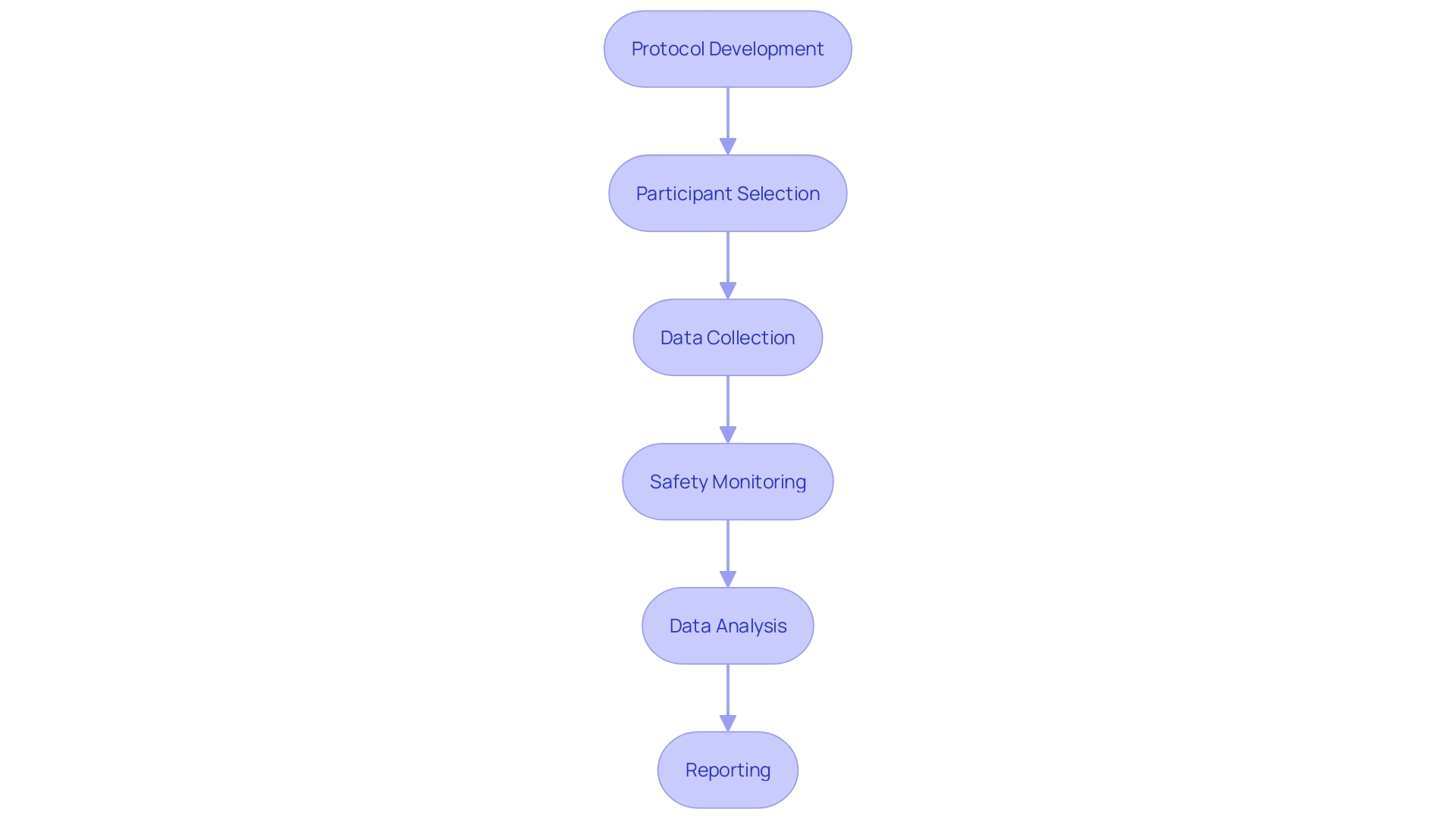
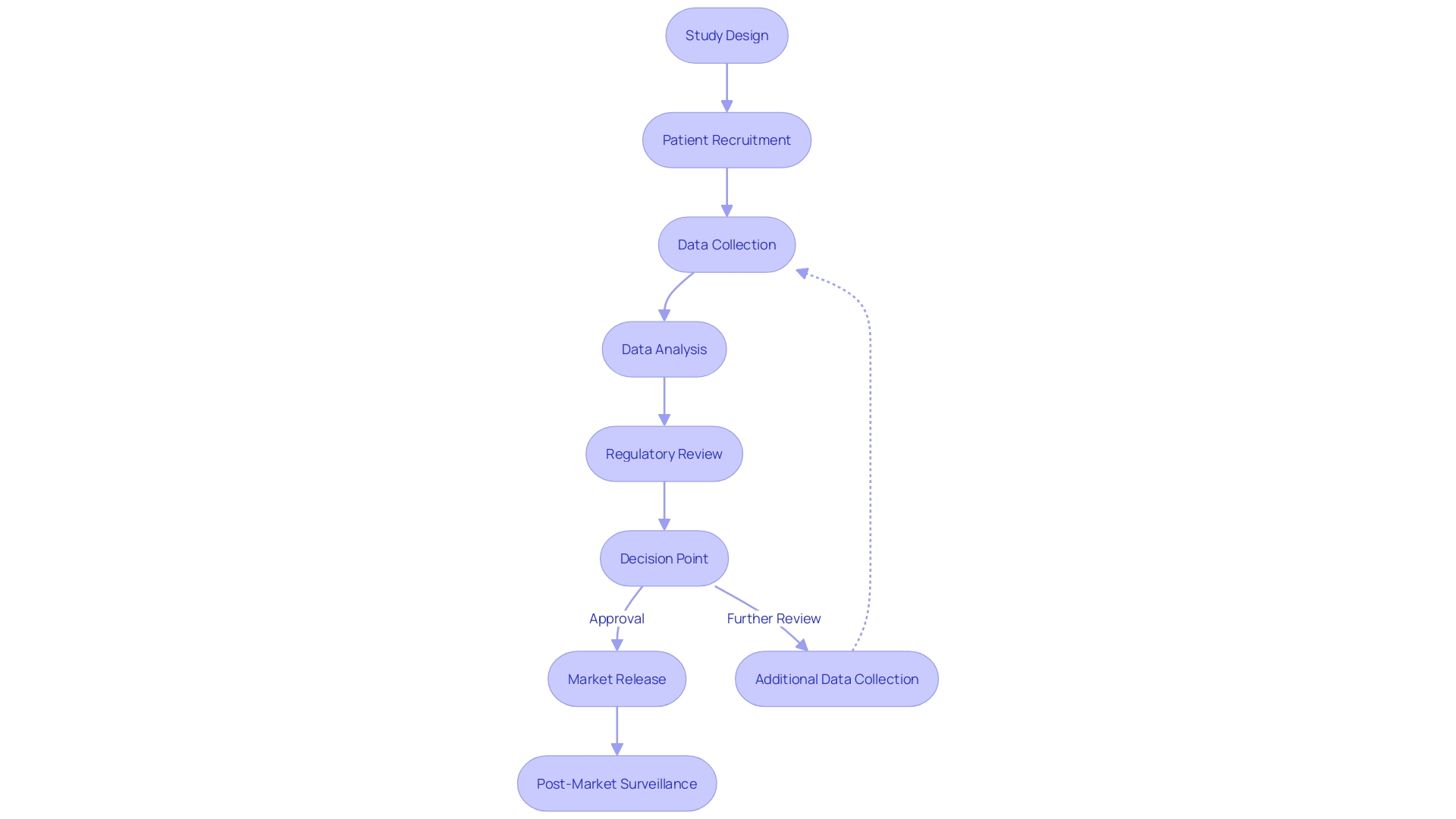
Clinical trials are structured in stages, with each phase designed to meticulously assess the safety and efficacy of new treatments. Starting with a small group of healthy volunteers in phase one, the trials progress to larger groups including patients in phase two, before moving into the pivotal phase three trials.
Ensuring compliance is not only about adhering to ethical guidelines and obtaining the necessary approvals but also about maintaining clear and concise informed consent processes. The MHRA's commitment to providing predictable timescales for Clinical Trial Authorisation applications is a testament to the importance of efficient and reliable regulatory oversight in clinical research.
The expertise and pragmatic approach of regulatory bodies and the clinical trial companies that navigate these guidelines are crucial to the successful execution of clinical trials. As new treatments are tested and established, the ability to manage these regulatory requirements becomes integral to the development of medical products that can truly transform patient care and outcomes.
Accelerated Research Timelines
Clinical trial companies are pivotal in the intricate process of bringing new medical treatments to fruition. The development of vaccines, for example, progresses through a highly structured sequence of phases. Initially, Phase 1 trials enlist a small cohort to verify safety, followed by Phase 2, which expands the pool to several hundred participants to determine the immune response and appropriate dosing.
Reaching Phase 3, the vaccine is tested in large-scale, double-blind studies to confirm efficacy, a step that can span several years under normal circumstances.
The urgency to streamline this process is underscored by organizations like CEPI, which aims to reduce vaccine development time from years to merely 100 days. Achieving such a rapid timeline necessitates innovation in both the scientific and operational aspects of clinical testing, as well as in navigating the complexities of regulatory approvals. This is where the expertise of Clinical Research Organizations (CROs) becomes indispensable.
They harness their resources and knowledge to expedite patient recruitment, data collection, and analysis, ensuring trials advance swiftly and efficiently.
In the context of medical device development, the emphasis on product requirements that enhance performance, safety, and quality without unnecessary complexity is critical. Strategies include focusing on essential features, potentially deferring 'nice-to-have' attributes for future updates, and integrating User Experience (UX) design principles to create devices that are not only effective but also intuitive for clinicians and patients.
CROs' ability to manage these multifaceted challenges is vital for delivering innovative medical solutions to patients in need, particularly in a landscape where accelerated approval pathways are increasingly utilized for treatments addressing serious conditions with unmet medical needs. Such pathways allow for earlier market entry based on surrogate endpoints, with subsequent confirmatory trials to cement clinical benefits. This approach underscores the balance between rapid innovation and rigorous validation that cross adeptly navigate.
Global Reach and Accessibility
Clinical Research Organizations (CROs) are not only pivotal in the advancement of medical knowledge but also function as global entities, connecting a diverse array of investigators, research sites, and patient populations. The international scope of CROss is critical in assembling a comprehensive and representative sample, which is fundamental to the validity and applicability of research outcomes. By leveraging multi-center trials, CROs enhance the feasibility of conducting expansive studies, which is especially beneficial for conditions that are geographically dispersed or vary in prevalence across different populations.
The logistics of global clinical trials are intricate, often involving cross-border coordination and language barriers. Patients, like the one from rural Pennsylvania seeking treatment for a rare disease in Turkey, face challenges such as visa procurement, navigating foreign legal requirements, and language obstacles. CROss provide indispensable support in these scenarios, ensuring that trials are accessible and that patient-centricity is at the forefront, a notion supported by the Vice President of Digital Offerings at RWS, Daniel J Herron, who emphasizes the importance of patient involvement in trial design and the clarity of information provided to them.
Statistically, the post-pandemic landscape has seen a shift towards more adaptive and innovative clinical trial methods. The use of AI and machine learning is on the rise, aiming to enhance patient recruitment and the efficiency of trials, as noted by the CEO of WCG. Moreover, the push for diversity, equity, and inclusion in clinical research is gaining momentum, recognizing the nuanced differences in disease manifestation across various demographics.
CROs are instrumental in orchestrating these trials, often bridging the gap between disparate healthcare systems and regulatory frameworks. A Finnish lab collaborating with a Canadian CRO exemplifies this synergy, allowing for the exchange of expertise and adherence to local regulations while broadening the patient base and enriching the research.
Ellen Cappellino of Klick Health discusses the challenge of synergizing the clinical narrative with the value story for market access, stressing the rapid advancements in fields like oncology and personalized medicine. This highlights the CROs' role in not only managing trials but also in aligning scientific discovery with market needs. The collaboration between various functions within the industry and the integration of AI in market access strategies further exemplify the evolving role of CROs in shaping the future of clinical research.

Advanced Technology and Resources
Clinical trial companies, known as Contract Research Organizations (CROs), are integral in advancing medical knowledge and improving patient outcomes through the management of clinical trials. They leverage state-of-the-art technological advancements to increase the precision and efficiency of research studies. For example, the use of large language models (LLMs) trained on extensive clinical trial protocols facilitates the creation of initial drafts for essential documents, which streamlines the trial preparation process.
Moreover, simple machine learning models are employed to monitor clinical trial data in real time, enhancing safety by promptly identifying errors or potential adverse events.
The significance of incorporating advanced technology and resources in clinical trials is further underscored by the push for multi-disciplinary collaboration in complex fields like CNS/neurology research. Organizations such as Lindus Health emphasize the need for diverse input, including clinical operations specialists and patient voices, to ensure the success of clinical trials. This holistic approach is critical in navigating the intricacies of trial design and participant recruitment, which are often hindered by restrictive inclusion criteria and practical considerations on treatment procedures.
The integration of technology in clinical trials is also evident in the use of digital patient engagement tools, wearable devices, and sensors. These tools facilitate faster outcome assessments and generate consistent data, thereby improving patient compliance and reducing entry errors. Furthermore, the automatic transmission of data from devices like blood pressure monitors and digital scales to researchers minimizes manual handling, enabling immediate data analysis and identification of safety issues.
The integration of electronic medical records (EMRs) with clinical trials further eliminates redundant data submission, simplifying the research process.
However, the digitalization of clinical trials is not without its challenges, including ethical and privacy concerns associated with the use of technology. As the global user base for wearable technology reached 1.1 billion in 2022, the potential for digital surveillance or misuse of sensitive data, such as fertility-related metrics, poses significant risks that must be addressed.
Experts in the field advocate for a structured data strategy to harness the full potential of technology in clinical trials. As stated by a leading industry professional, the exponential growth of data from connected devices and advanced AI-driven methodologies requires a deliberate approach to collecting and analyzing clinical data. Such a strategy ensures that patient safety and data quality are at the forefront of drug development decisions.
Overall, the investment in advanced technology by CRO firms is a testament to their commitment to enhancing the quality and efficiency of clinical research. With the right strategies and ethical considerations, these technological resources can continue to shape the future of medical treatment development and contribute to the broader goal of improving healthcare outcomes.
Risk Management and Mitigation
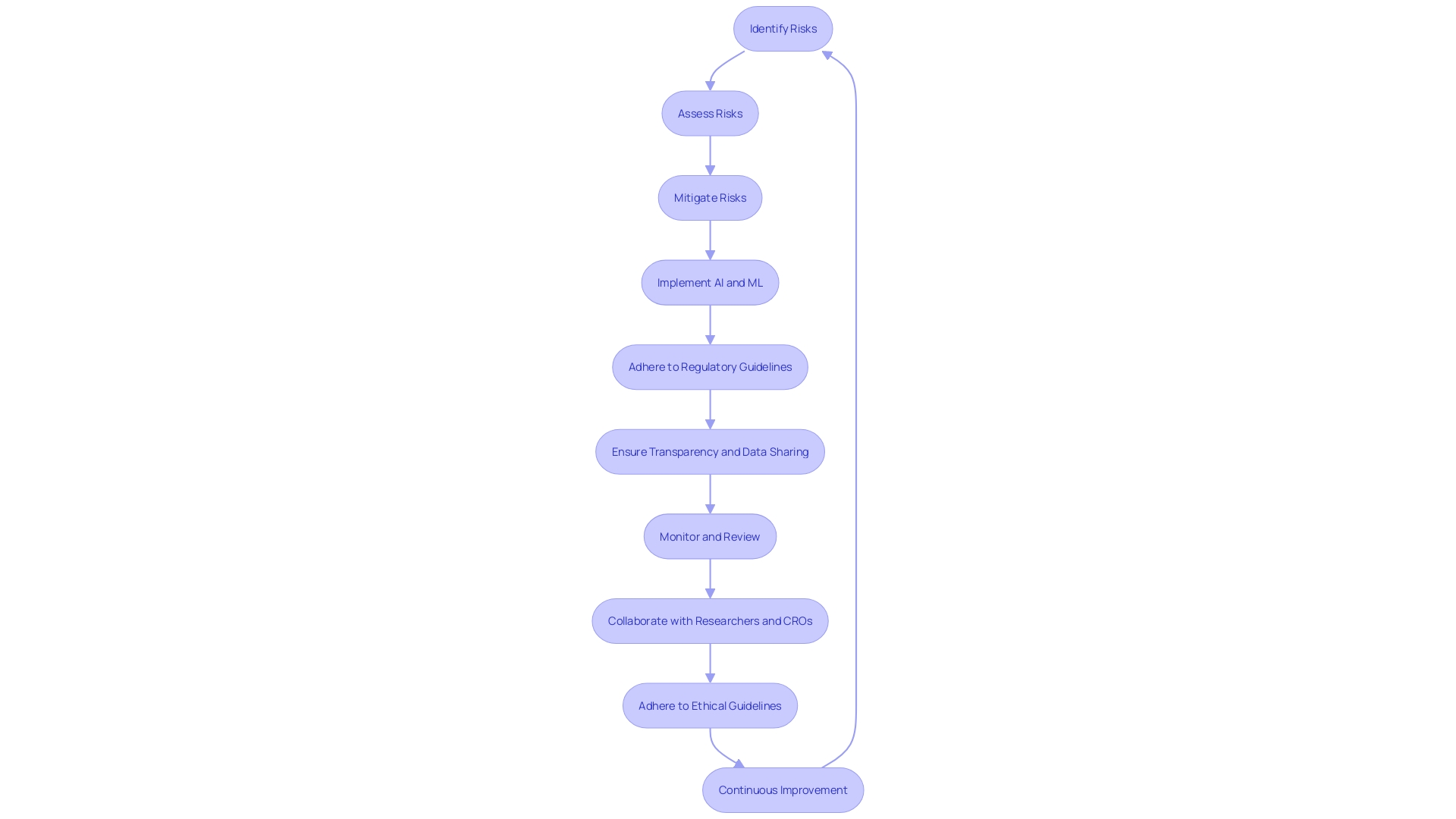
Clinical trial companies, also known as Contract Research Organizations (CROs), are pivotal in navigating the intricate landscape of clinical research, which is fraught with potential risks that could jeopardize patient safety, data integrity, and compliance with regulatory frameworks. To counter these risks, CROss deploy meticulous risk management strategies that encompass thorough identification, assessment, and mitigation processes. These strategies are fortified by robust quality control systems and intensive monitoring procedures that collectively aim to safeguard the research process against any risks that could impair its integrity.
For instance, the case of a patient from rural Pennsylvania highlights the complexity of participating in a clinical trial located in a foreign country such as Turkey. In this scenario, the multifaceted challenges include visa acquisition, navigating language barriers in document processing, and coordinating international travel. This underscores the critical importance of risk management in addressing logistical and safety concerns that participants may encounter.
Furthermore, the integration of artificial intelligence (AI) and machine learning (ML) into clinical research introduces a new dimension of risk that must be meticulously regulated. Regulatory bodies, including the FDA, EU, and EMA, are proactively establishing guidelines to manage these risks effectively. These guidelines advocate for a "risk-based approach" to AI deployment in clinical trials and demand transparency from technology providers, ensuring that innovation does not compromise patient safety or data integrity.
Historically, clinical research has adhered to stringent guidelines to ensure the ethical treatment of participants and the credibility of data collected. These principles remain steadfast despite the advent of new technologies. For example, the FDA's Software as a Medical Device (SaMD) regulations categorize risks associated with software and algorithms used in clinical treatment planning and monitoring, guiding the application of best practices in design, development, and validation.
By aligning with a CRO, researchers gain access to a wealth of expertise and experience in managing the multifarious aspects of clinical trials. This collaboration provides researchers with the assurance that their studies are conducted within a framework of rigorous risk management, ultimately contributing to the advancement of medical science and the betterment of patient outcomes.
Enhanced Patient Safety
Clinical trial companies, or Contract Research Organizations (CROs), are at the forefront of medical innovation, ensuring that new treatments and medical devices are both safe and effective. These firms bring a wealth of experience to the table, managing the complexities of trial protocols and participant care. A vital aspect of their role is safeguarding participants, a responsibility taken seriously as evidenced by rigorous monitoring for adverse events and strict adherence to ethical standards.
The commitment to patient safety is unwavering, with transparent communication and learning from harm events, as proposed by initiatives like the Pathway to Accountability, Compassion, and Transparency (PACT).
CROs are also navigating the integration of cutting-edge technologies such as AI and ML while remaining compliant with evolving regulatory frameworks like the EU AI Act, which mandates a risk-based approach to AI usage. As technological breakthroughs present new opportunities for clinical research, these organizations ensure that innovation does not come at the cost of patient welfare. Historical precedence from guidelines such as the Harmonized Tripartite Guideline for Good Clinical Practice reinforces the longstanding commitment to upholding the rights and safety of trial participants.
Furthermore, in the wake of findings that a significant number of studies fail to report their results, the role of CROs in promoting transparency and accountability has never been more critical. They stand as vigilant protectors of patient well-being, while also driving the advancement of medical science.
How to Choose the Right CRO Firm for Your Medical Research
Selecting a Contract Research Organization (CRO) is a critical step in ensuring the successful execution of a clinical study. It's important to assess various factors to make an informed decision. Consider not only the CRO's expertise and track record managing clinical studies for medical devices or drugs but also its ability to work collaboratively.
For example, Chris, a biomedical engineer with extensive experience in managing clinical studies, highlights the importance of a CRO's capability to showcase solutions effectively.
Furthermore, a CRO should be adept at incorporating multi-disciplinary approaches, especially for complex fields like CNS/neurology research. Meri, from Lindus Health, emphasizes the significance of including clinical operations specialists and patient perspectives to overcome challenges in participant recruitment and study feasibility.
Additionally, the rise of telehealth companies like Lemonaid Health, which faced obstacles in market growth due to a complicated media strategy, serves as a reminder of the importance of a CRO's ability to adapt and innovate in a rapidly evolving industry. The ability to pivot and implement efficient strategies for unique challenges is essential.
In light of the evolving clinical trial landscape, it's also wise to consider the flexibility and adaptability of a CRO. The industry is moving towards a more patient-centric approach, grappling with logistics like cross-border travel for trial participants. A CRO that can navigate these complexities and support patients throughout the process is invaluable.
Lastly, the integrity of clinical research is paramount. As Dr. Dror Kolodkin-Gal of Proofig AI points out, the accuracy of data, including image integrity, is fundamental. With a significant percentage of manuscripts flagged for image-related issues, selecting a CRO that upholds the highest standards of data integrity is crucial to the credibility of your research.
In conclusion, when choosing a CRO, weigh their expertise, collaborative abilities, adaptability, patient-centric approaches, and commitment to data integrity. These considerations will guide you to a partnership that supports the success of your study and ultimately contributes to advancements in healthcare.
Conclusion
In conclusion, Clinical Research Organizations (CROs) are essential for advancing medical research by managing clinical trials and assessing the safety and efficacy of treatments. To address challenges in recruitment and retention, CROs are embracing technology, diversity, and inclusion.
CROs explore novel treatment avenues and facilitate participation for patients with rare diseases or in remote locations. They provide specialized expertise, ensuring scientifically sound and cost-effective trials. CROs also prioritize data management and regulatory compliance to maintain integrity and protect participant rights.
With advanced technology, CROs enhance precision and efficiency in trials, using AI, machine learning, and digital tools. They manage risks, prioritize patient safety, and accelerate research timelines. When selecting a CRO, consider expertise, collaboration, adaptability, patient-centric approaches, and data integrity.
In a post-pandemic world, the role of CROs in driving innovation, ensuring participant safety, and advancing global health is crucial. Their dedication and the commitment of professionals and trial participants contribute to shaping the future of medical treatment development and improving healthcare outcomes. CROs continue to play a pivotal role in the advancement of medical research.




