Introduction
The landscape of clinical research is undergoing a profound transformation, driven by the integration of digital health technologies (DHTs) that facilitate remote data acquisition. As the FDA establishes comprehensive guidelines to govern these innovations, the emphasis on regulatory compliance and data integrity has never been more critical.
This article delves into the multifaceted aspects of DHTs, examining:
- The essential considerations for their selection in clinical trials.
- The challenges and opportunities they present.
- The imperative of ensuring patient safety and data reliability.
By exploring the future implications of these technologies, it becomes evident that the intersection of digital health and clinical research not only enhances trial efficiency but also paves the way for more personalized and effective healthcare solutions.
Through an informed understanding of these dynamics, researchers can navigate the complexities of DHT integration, ultimately contributing to the advancement of clinical practices and improved patient outcomes.
Understanding FDA Guidance on Digital Health Technologies for Remote Data Acquisition
The FDA has established comprehensive guidelines governing the use of digital health technologies (DHTs) for remote information acquisition, underscoring the critical need for adherence to regulatory standards. Our service capabilities include:
- Feasibility and selection of research locations and primary investigators
- Review and feedback on study documents to ensure compliance with country requirements
- Setup and approval processes involving ethics committees and health ministries
- Project management and reporting
Key elements of these guidelines dictate that DHTs must comply with quality system regulations (QSR), which serve as a foundation for ensuring product quality and safety.
Moreover, verifying information sources is essential for upholding integrity and dependability throughout research investigations. The necessity for obtaining appropriate approvals for both software and hardware components utilized in trials cannot be overstated. Recent FDA guidance has clarified the pathways for incorporating mobile applications and wearable devices into healthcare workflows, presenting clear standards for information collection, enhancing patient engagement, and optimizing user experience.
Crucially, substantial changes in DHT measurements after updates may undermine investigation results, highlighting the necessity for thorough assessment and verification of these technologies. Understanding and implementing these regulations is imperative, as any deviations could jeopardize study approvals and compromise the overall quality of the data collected. As emphasized by Christopher M. Hartshorn, PhD, "Digital Health Technology Research Funded by the National Institutes of Health," there is a growing acknowledgment of the significance of these compliance measures in promoting effective medical practices.
Furthermore, the smallest budget tier has demonstrated a significant rise in DHT funding, increasing from 4.6% in 2015 to 11.0% in 2023, highlighting the growing importance of DHTs in research.
Key Considerations for Selecting Digital Health Technologies in Clinical Trials
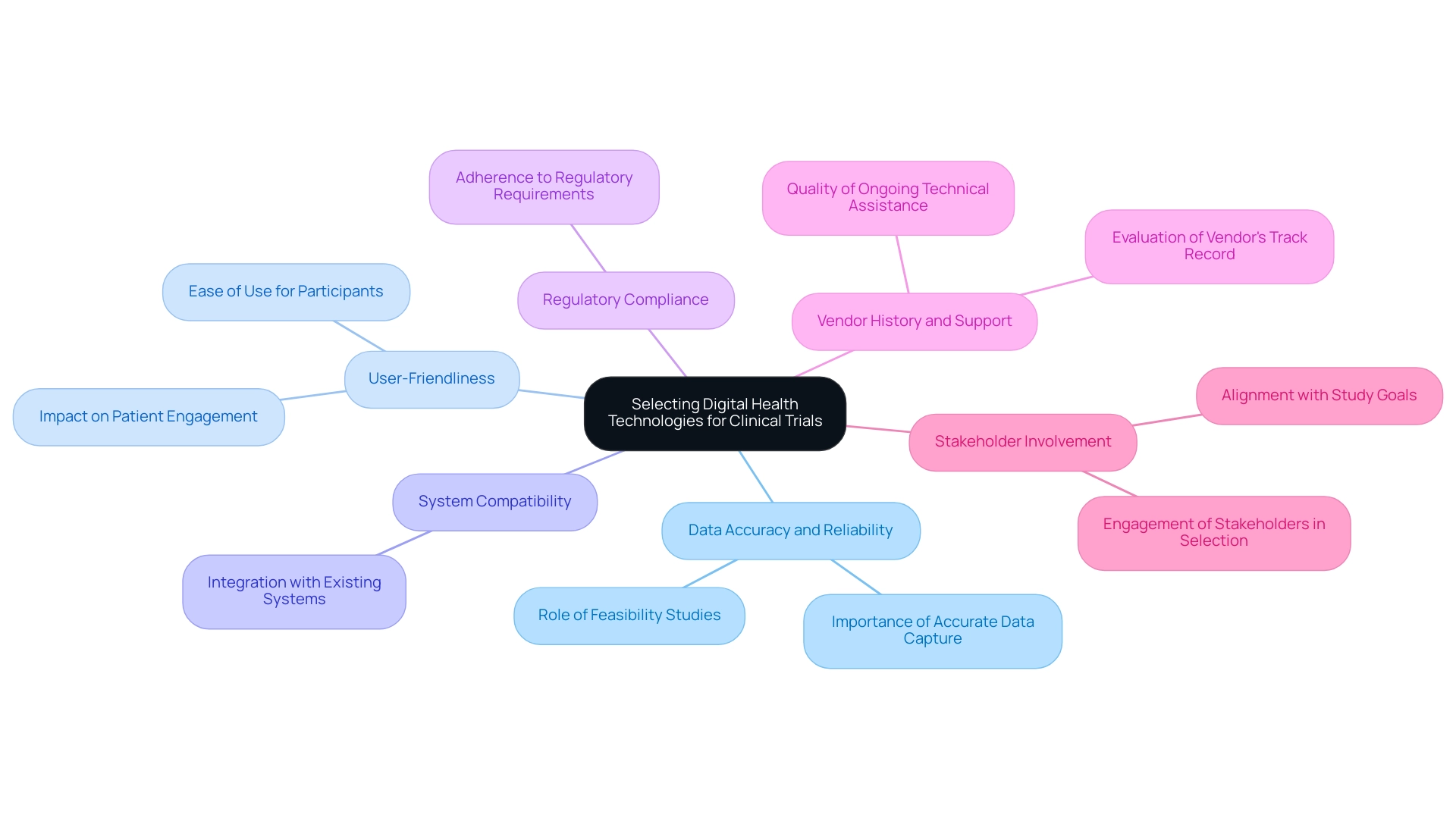
When selecting digital health technologies for remote data acquisition in clinical investigations, researchers must thoroughly evaluate various essential elements to ensure the success of their studies. Key considerations include:
- The system's capability to capture accurate and reliable data through digital health technologies for remote data acquisition in clinical investigations.
- User-friendliness for participants.
- Compatibility with existing systems.
- Adherence to regulatory requirements.
The significance of comprehensive clinical study management services—feasibility studies, site selection, compliance reviews, study setup, import permits, project management, reporting on serious and non-serious adverse events—cannot be overstated in this selection process. Notably, spending in DHT research for the largest budget tier has increased from $24,832,961 to $108,201,748 between 2015 and 2023, underscoring the financial commitment to selecting the right technologies for successful outcomes. As highlighted by Pablo Cure, MD, MPH, 'To reach the next level in the translation and implementation of DHTs, it is imperative to design and conduct rigorous, equitable, needs-based research and the corresponding validation studies to generate the necessary evidence to support their use in biomedical research and health care for the benefit of all.'
Moreover, evaluating the vendor's history and the quality of support services is crucial, as effective ongoing technical assistance can greatly affect results. For example, a recent case study on virtual messaging for recruitment showcased how incorporating text messaging efficiently recognized suitable patients for medical studies, speeding up the recruitment process and highlighting the capability of DHTs to improve participant involvement.
Involving stakeholders and potential users in the selection process is essential; it ensures that the chosen solutions not only meet user needs but also align with the overarching goals of the study.
For studies that utilize digital health technologies for remote data acquisition in clinical investigations, this alignment is particularly critical, as it facilitates both patient engagement and information accuracy, ultimately leading to more reliable health outcomes and contributing to job creation and healthcare improvements within local economies.
Challenges and Opportunities in Implementing Digital Health Technologies
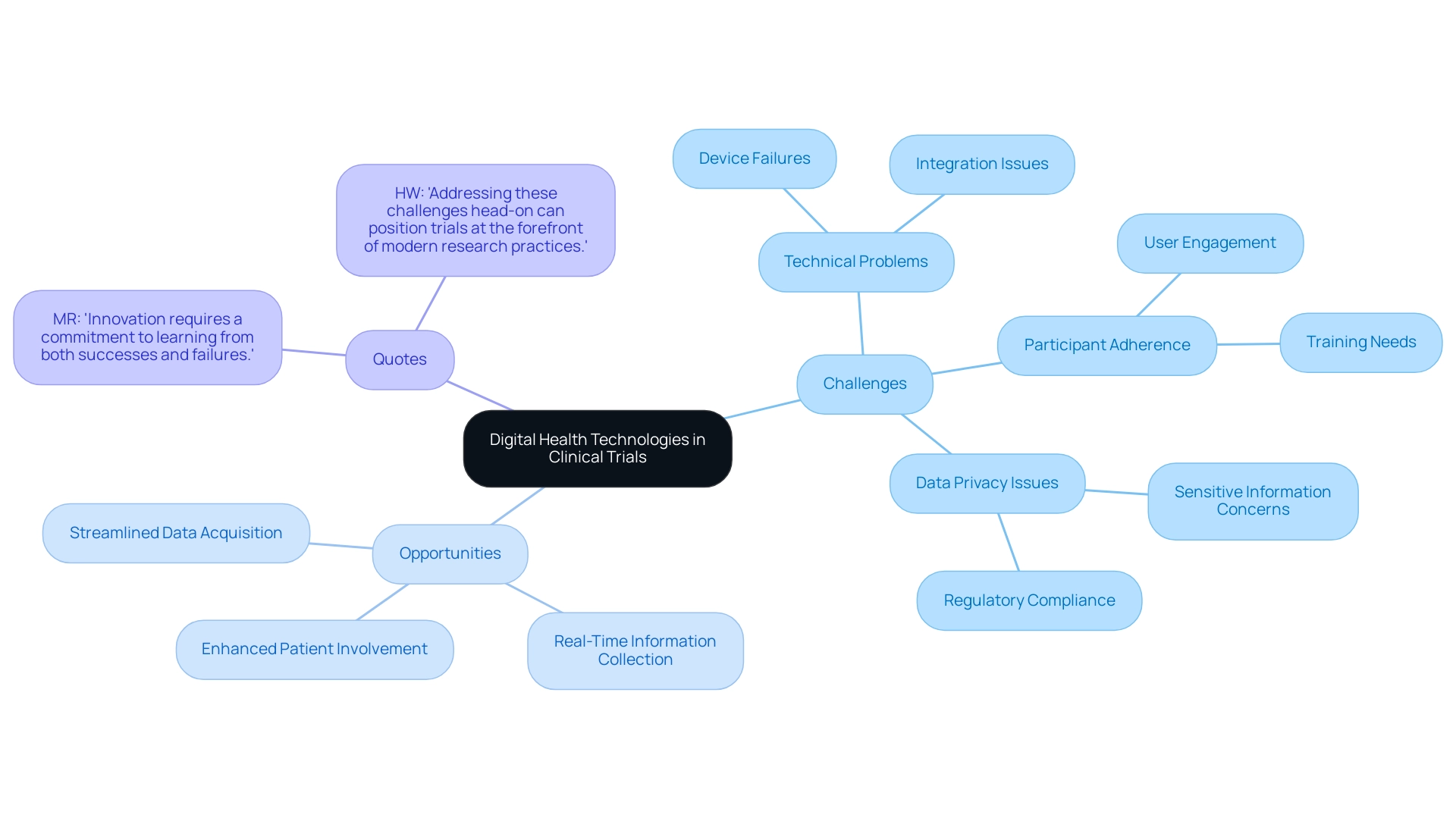
The incorporation of digital health technologies for remote data acquisition in clinical investigations presents a variety of challenges and opportunities, particularly in the context of comprehensive clinical trial management services. Main obstacles often faced involve technical problems like device failures and the difficulties related to incorporating these innovations into current information management systems. Additionally, ensuring participant adherence to the use of these tools remains a significant concern.
Data privacy and security issues further complicate the widespread adoption of DHTs, as apprehensions about safeguarding sensitive information can deter both researchers and participants from fully embracing these innovations. This ambivalence reflects the complex reactions to integration of digital solutions in care practices, underscoring that while some may appreciate the benefits, others may feel discomfort or skepticism regarding their use.
An illustrative case study titled 'Ambivalence in Digital Health Integration' explored the experiences of HIV patients regarding digital health tools. The study revealed that patients may appreciate certain features of digital devices while simultaneously experiencing discomfort with others, indicating a nuanced perspective on digital health.
Conversely, the challenges posed by DHTs are accompanied by substantial opportunities. These digital health technologies for remote data acquisition in clinical investigations enhance patient involvement by offering more interactive and personalized experiences, facilitate real-time information collection, and improve overall quality.
By adopting digital health technologies for remote data acquisition in clinical investigations alongside robust services such as feasibility studies, site selection, and compliance reviews, researchers can streamline data acquisition processes, potentially leading to a reduction in study duration. Furthermore, fostering a culture of adaptability and continuous learning within research teams is essential for overcoming these implementation challenges. As MR noted, 'Innovation requires a commitment to learning from both successes and failures,' which underscores the importance of an atmosphere that encourages flexibility.
HW also emphasizes that 'addressing these challenges head-on can position trials at the forefront of modern research practices.' Together, these insights underscore the critical need for a balanced approach to the integration of digital health solutions, reinforcing bioaccess®'s commitment to leading medtech clinical research in Latin America with a focus on innovation and regulatory excellence.
Ensuring Data Integrity and Patient Safety with Digital Health Technologies
To maintain information integrity in the implementation of digital health solutions (DHTs), researchers must establish comprehensive information management practices. This encompasses:
- Establishing rigorous validation protocols for the information gathered.
- Performing regular audits of the systems employed.
- Keeping detailed records of all procedures and choices for clarity and responsibility.
Given the rapid growth of DHTs, with 87 net new product additions in the prescription digital therapeutic market since May 2021, prioritizing patient safety is critical.
This can be achieved through:
- Continuous monitoring of device performance.
- Swift resolution of any issues that may arise.
A key element in enhancing information quality is effective training for participants on the use of these technologies, which also mitigates potential risks associated with their deployment. Additionally, adhering to regulatory compliance, particularly with the oversight of INVIMA as a Level 4 health authority by PAHO/WHO, is non-negotiable, ensuring that patient information is managed with the highest standards of confidentiality and security.
The FDA has underscored the importance of developing regulatory frameworks that encompass innovations in artificial intelligence and machine learning, which are crucial for informing best practices in data integrity and patient safety in clinical investigations. Furthermore, robust project management practices are essential for overseeing the entire setup process, ensuring that all aspects of the study are executed efficiently and in compliance with regulatory standards. Reporting on study status, including serious and non-serious adverse events, is vital for maintaining accountability and transparency throughout the trial.
This commitment to protecting information integrity and patient welfare is essential for cultivating trust in digital health technologies for remote data acquisition in clinical investigations. Moreover, the recent Series A funding of $5 million obtained by ThoroughCare from Empactful Capital illustrates how financial backing can enhance the development of digital health services, ultimately contributing to better integrity practices.
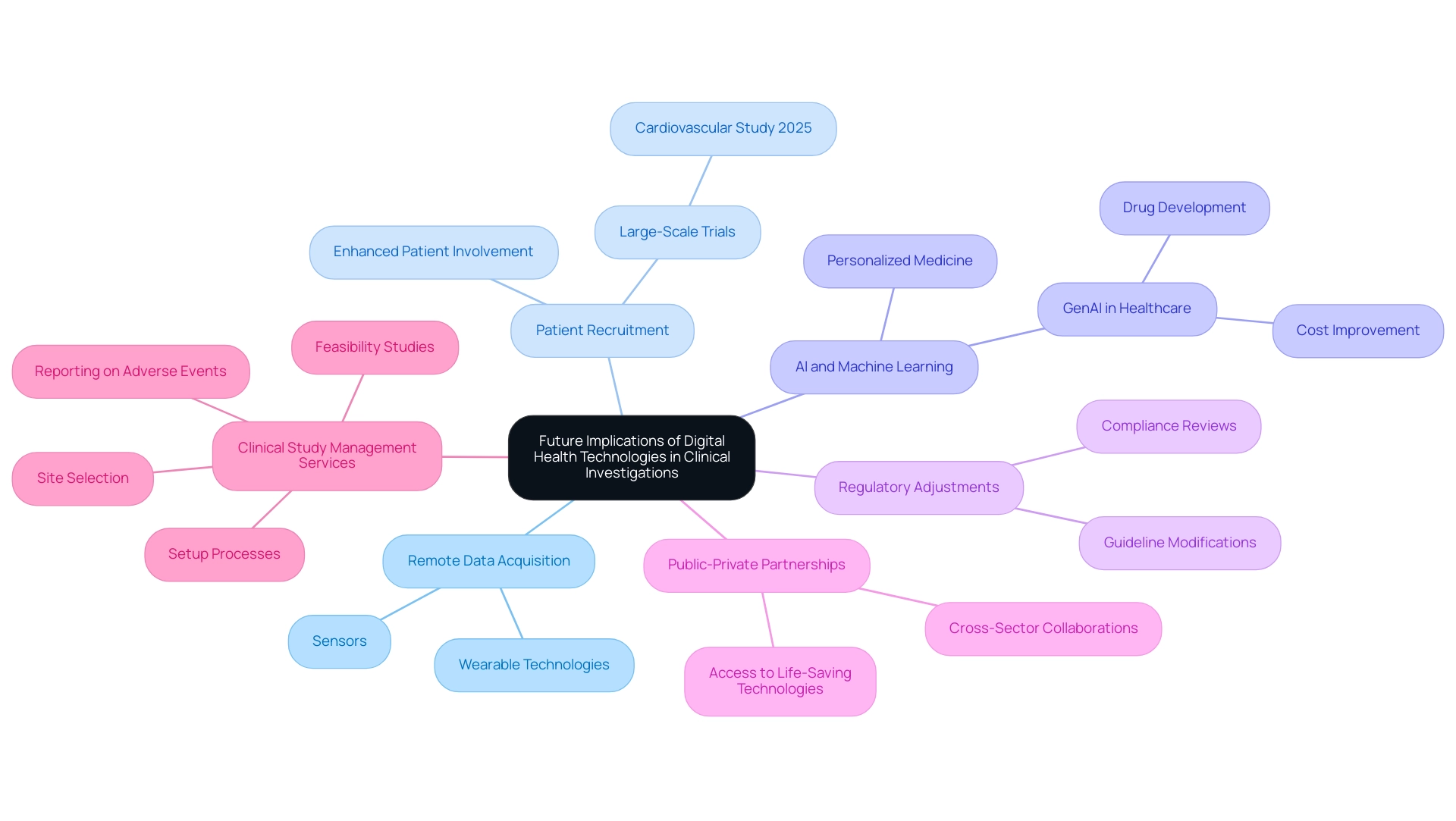
Future Implications of Digital Health Technologies in Clinical Investigations
The future of digital health technologies for remote data acquisition in clinical investigations is poised for significant advancement, particularly with the rapid evolution of artificial intelligence (AI), machine learning, and wearable technologies. These innovations in digital health technologies for remote data acquisition in clinical investigations are poised to transform data acquisition processes, streamline patient recruitment, and enhance real-time data analysis. Notably, our comprehensive clinical study management services encompass crucial support in:
- Feasibility studies
- Site selection
- Compliance reviews
- Setup processes
- Import permits
- Reporting on serious and non-serious adverse events
For instance, a large-scale cardiovascular study in Europe, planned for 2025, aims to recruit 50,000 participants remotely by utilizing digital health technologies for remote data acquisition in clinical investigations, showcasing the shift towards more accessible and efficient research methodologies. The incorporation of AI is not simply a trend; it is expected to enable personalized medicine strategies, providing customized treatments based on individual patient data.
As regulatory bodies adjust their guidelines to embrace these advanced innovations, it is crucial for researchers to remain knowledgeable and proactive about how these modifications will impact their studies. Florence Mowlem, PhD, Vice President of Science for ObvioHealth, encapsulates this sentiment when she states,
I hope this can be a turning point for the industry with regard to comparability testing. We can stop having comparability conversations so frequently, and instead we can start talking about optimizing our electronic measures for all individuals.
This perspective underscores the importance of optimizing electronic measures to enhance study comparability and effectiveness, which is at the heart of our service capabilities. Looking ahead to 2024, embracing innovation and cross-sector collaboration will be essential for researchers aiming to fully realize the potential of digital health technologies for remote data acquisition in clinical investigations. By fostering public-private partnerships, the healthcare sector can broaden access to life-saving technologies, ultimately enhancing efficiency in research and aligning more closely with patient needs. The growing application of digital health technologies for remote data acquisition in clinical investigations, including sensors and wearables, further exemplifies this trend, enhancing data collection and patient involvement.
Moreover, as highlighted in the case study on the role of GenAI in healthcare, the integration of AI is expected to profoundly transform various areas, including drug development and cost improvement. As patient advocacy groups gain influence, their participation will further enhance the relevance and impact of clinical trials in the digital age.
Conclusion
The integration of digital health technologies (DHTs) into clinical research represents a pivotal shift towards more efficient and personalized healthcare solutions. As outlined, the FDA's comprehensive guidelines emphasize the importance of regulatory compliance and data integrity, which are paramount in ensuring the success and reliability of clinical trials. Key considerations in selecting DHTs include:
- Their ability to provide accurate data
- User-friendliness
- Compatibility with existing systems
All of which contribute to enhanced patient engagement and streamlined data collection processes.
While challenges such as technical issues and data privacy concerns persist, the opportunities presented by DHTs are substantial. These technologies not only facilitate real-time data acquisition but also foster a culture of adaptability within research teams, enabling them to overcome hurdles and embrace innovation. Ensuring patient safety and maintaining data integrity through rigorous validation protocols and comprehensive training for participants are crucial steps in this evolution.
Looking ahead, the future of DHTs in clinical investigations is bright, driven by advancements in artificial intelligence, machine learning, and wearable technologies. Researchers must remain vigilant and proactive in adapting to regulatory changes and leveraging these innovations to optimize trial methodologies. By embracing cross-sector collaboration and engaging patient advocacy groups, the healthcare industry can enhance trial efficiency and align more closely with patient needs, ultimately leading to improved health outcomes and a more effective clinical research landscape.
Frequently Asked Questions
What are digital health technologies (DHTs) and their significance in remote data acquisition?
Digital health technologies (DHTs) are tools used for remote information acquisition in clinical investigations. They are significant as they enhance data collection, improve patient engagement, and optimize user experience.
What guidelines has the FDA established for DHTs?
The FDA has established comprehensive guidelines that require DHTs to comply with quality system regulations (QSR) to ensure product quality and safety. These guidelines also emphasize the importance of verifying information sources and obtaining necessary approvals for software and hardware used in trials.
What services are included in the management of DHT research?
Services include feasibility and selection of research locations and primary investigators, review and feedback on study documents for compliance, setup and approval processes involving ethics committees and health ministries, and project management and reporting.
Why is it crucial to assess DHT measurements after updates?
Substantial changes in DHT measurements after updates may undermine investigation results, making thorough assessment and verification essential to maintain the integrity of the research.
What considerations should researchers evaluate when selecting DHTs for clinical investigations?
Researchers should evaluate the system's capability to capture accurate data, user-friendliness, compatibility with existing systems, and adherence to regulatory requirements.
How has funding for DHT research changed from 2015 to 2023?
Funding for DHT research has significantly increased, with the smallest budget tier rising from 4.6% in 2015 to 11.0% in 2023, and spending in the largest budget tier increasing from $24,832,961 to $108,201,748.
What role do stakeholders and potential users play in the selection process of DHTs?
Involving stakeholders and potential users is essential to ensure that the selected DHTs meet user needs and align with the study's goals, facilitating patient engagement and information accuracy.
What impact do DHTs have on local economies and healthcare improvements?
DHTs contribute to job creation and healthcare improvements within local economies by enhancing the quality and efficiency of clinical research and patient care.




