Introduction
In the realm of clinical trials, the selection of appropriate endpoints is a cornerstone that determines the trajectory and outcome of the research. This article delves into the critical aspects of primary and secondary endpoints, elucidating their roles, characteristics, and the challenges associated with their selection. Primary endpoints serve as the definitive measures of a treatment's effectiveness, while secondary endpoints provide additional insights that enhance the understanding of the intervention's broader impact.
The discussion extends to the nuances of endpoint selection, emphasizing the importance of statistical rigor, bias mitigation, and adherence to regulatory standards. Through detailed exploration, examples from real-world studies and expert opinions, the article aims to equip researchers and stakeholders with the knowledge necessary to conduct robust and impactful clinical trials.
Understanding Primary Endpoints
Main objectives act as the crucial metrics in research studies, assessing the efficacy of a therapy or intervention. 'These points must be selected based on their direct relevance to the disease under investigation and their capacity to demonstrate the therapeutic benefits clearly.'. Common examples include overall survival, disease-free survival, and symptom relief. For instance, in a retrospective study by Dr. Lisa Hess and her team at Eli Lilly, overall survival was among the key outcomes assessed to understand treatment patterns in mantle cell lymphoma patients. Moreover, efficient and well-structured clinical research, as highlighted by the FDA, depends on precisely defined primary goals to guide regulatory choices and ensure patient safety and effectiveness of medical products.
Characteristics of Primary Endpoints
Main objectives must be meticulously defined, measurable, and clinically relevant to ensure the robust evaluation of treatment effects. 'These targets should be grounded in robust statistical methods, such as Bayesian approaches, which are especially beneficial as they permit more regular evaluations and can prolong promising research without drawbacks.'. For example, Bayesian methods enable the continuous incorporation of new data, enhancing the accuracy of the treatment effect estimation by updating the posterior probability calculation with each new dataset.
Furthermore, the main goal should be attainable within the trial’s timeline and take into account the specific patient population involved. Making sure this alignment is essential for the conclusion to represent significant health results precisely. Randomized Controlled Trials (RCTs), despite their imperfections, remain the gold standard for generating trustworthy information, provided they are well-designed to minimize biases and enhance generalizability.
Applying these principles in choice of targets not only guarantees the integrity of the research study but also aids in regulatory approval and promotes the ultimate aim of enhancing patient outcomes. For example, Voiant’s extensive network and experienced personnel have consistently shown the significance of dependable data points in ophthalmic imaging and ocular safety studies, highlighting the essential role of clearly defined primary objectives in clinical research.
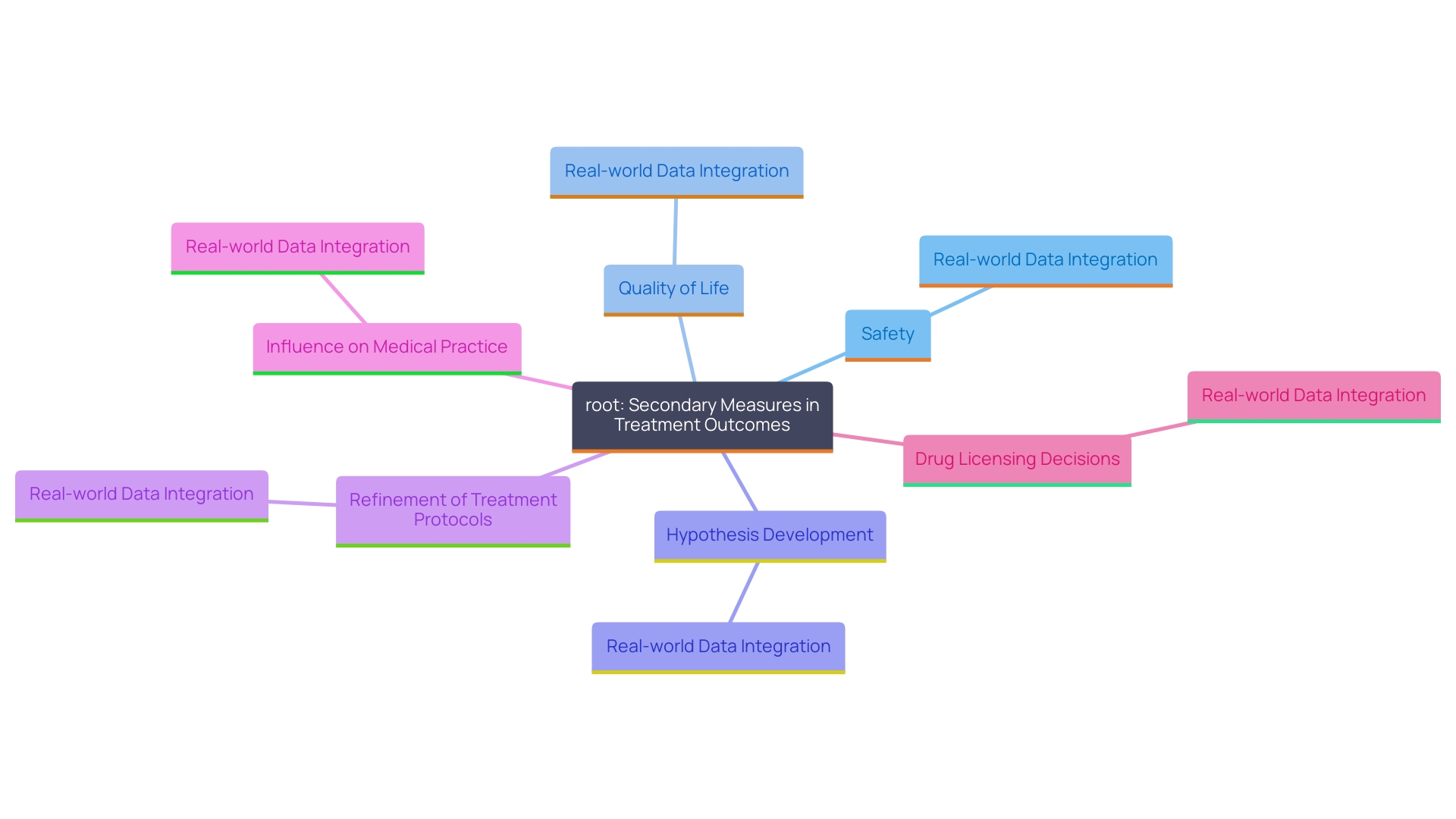
Secondary Endpoints: Definition and Use
Secondary measures are crucial additional outcomes that enrich our understanding of a treatment’s effects beyond the primary objectives. 'These reference points encompass a wide range of factors, including safety, quality of life, and other metrics that can offer a more comprehensive view of the intervention’s overall impact.'. 'For example, real-world data integration, as employed by England’s NHS, can include various patient populations to improve the overall applicability of clinical study outcomes.'. Additionally, secondary objectives often aid in hypothesis development for future studies, establishing a basis for later research efforts. By comparing outcomes across various patient groups, as observed in study emulation, researchers can identify the broader implications of treatment methods. This systematic approach helps in refining treatment protocols and can significantly influence medical practice and drug licensing decisions.
Key Differences Between Primary and Secondary Endpoints
The main difference between main and secondary objectives in clinical studies lies in their respective roles. Main objectives are essential in evaluating the fundamental hypothesis of a study, supplying the crucial information needed to ascertain the study's success or failure. These points are carefully specified in the research guidelines to ensure that the main goals of the study are achieved with clarity and accuracy. In contrast, secondary endpoints provide extra insights that enhance the primary findings, often addressing wider questions or exploratory objectives that were not the main focus of the study. 'This delineation is essential not only for the accurate interpretation of experimental results but also for regulatory submissions, as it ensures that both primary and secondary information are gathered and examined systematically.'.
The design, execution, and analysis of medical studies are further complicated by the choice between frequentist and Bayesian approaches. Bayesian methods, for instance, offer greater flexibility and efficiency in evaluating treatments, allowing for more frequent assessments and the possibility to extend promising studies without penalty.
In practice, research studies must follow strict protocols to obtain high-quality information and dependable results. Traditional medical guidelines aim to enhance the quality, equity, and consistency of care, though they may sometimes fall short in addressing individual patient needs. Identifying these subtleties aids in grasping the extensive influence of main and secondary goals on the overall achievement and regulatory approval of research studies.
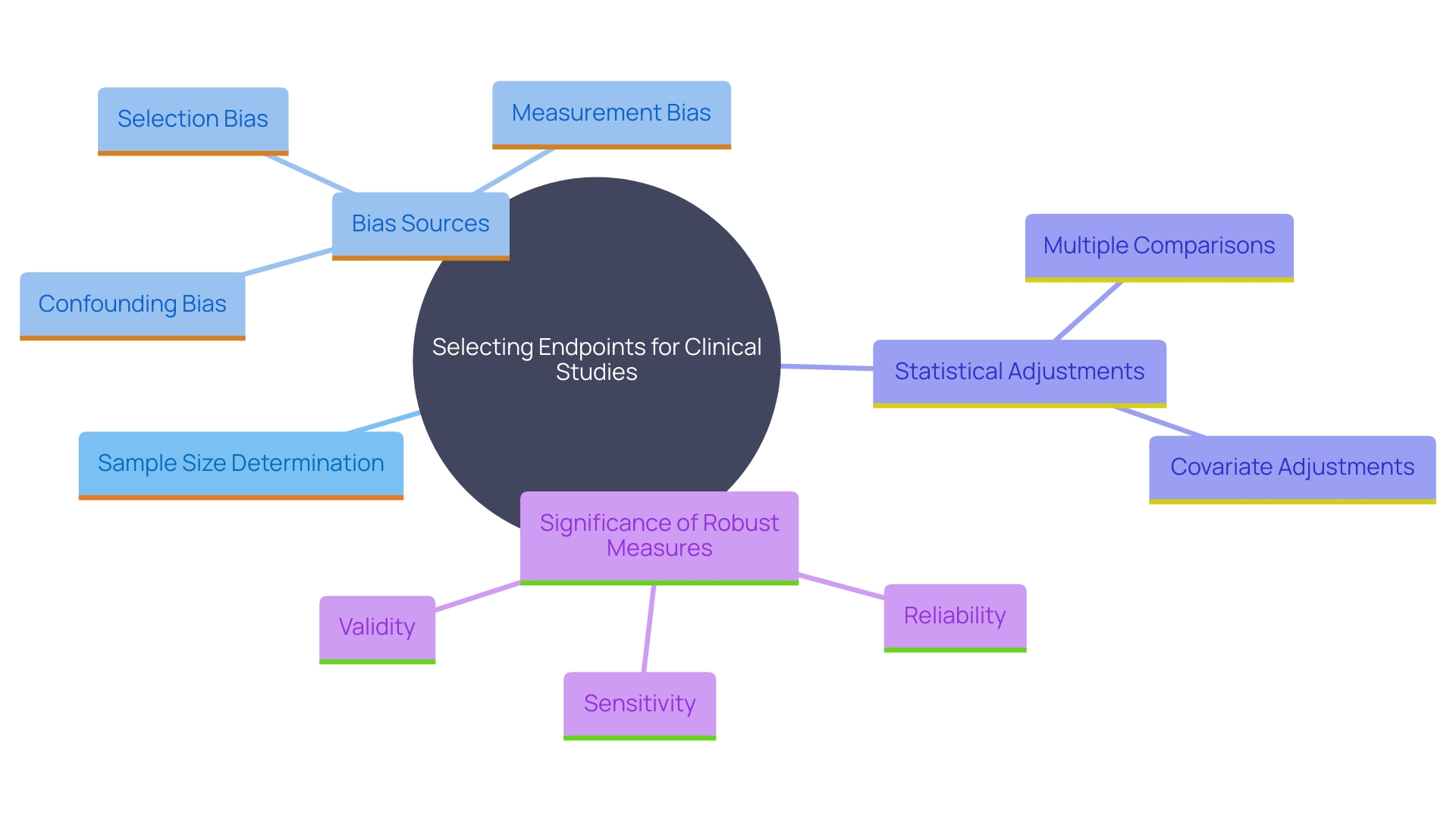
Challenges in Selecting Endpoints: Statistical Considerations
Choosing suitable endpoints requires careful statistical factors to guarantee the integrity and validity of clinical studies. One paramount concern is determining a sufficient sample size to achieve adequate power for detecting clinically meaningful effects. This is critical as underpowered studies may fail to identify significant differences, potentially leading to erroneous conclusions.
Additionally, researchers must be vigilant about the potential for bias. Bias can emerge from different origins, such as sampling errors, measurement inaccuracies, or analysis flaws. To mitigate these risks, it is essential to use rigorous methods and validated tools. For instance, Bayesian approaches offer flexibility and efficiency, especially in early-stage experiments, by allowing more frequent data assessments and extending promising studies without penalties.
Another significant consideration is the risk of multiple comparisons, which can increase the likelihood of false positives. Researchers need to adjust their statistical analyses to account for these multiple tests, ensuring that the reported findings are robust and reliable.
Endpoints must be carefully chosen to be resistant to confounding factors that could skew the results. This involves choosing targets that directly assess the intended outcomes and are not affected by external variables. For instance, utilizing overall survival as a goal in cancer trials is a standard practice to capture the true efficacy of the treatment.
In the realm of ophthalmic imaging, Voiant exemplifies the importance of reliable and reproducible information. 'Their extensive experience, coupled with a network of over 2,000 registered sites, underscores the necessity of having experts who can manage complex imaging data, ensuring high-quality outcomes.'.
In summary, choosing suitable targets requires a comprehensive approach that encompasses statistical rigor, bias mitigation, and the careful selection of resistant measures. By adhering to these principles, researchers can ensure that their findings are both accurate and meaningful.
Best Practices for Endpoint Selection in Clinical Trials
Involving stakeholders early in the design process is vital for choosing suitable targets, as it guarantees that all viewpoints are taken into account. Aligning endpoints with regulatory expectations is another key practice, which can be facilitated by drawing on established frameworks like the PRINCIPLED process, a five-step guide for planning and analyzing non-interventional studies. This approach can enhance transparency and communication between stakeholders and regulatory bodies.
Incorporating patient-reported outcomes (PROs) is increasingly important, as they provide valuable insights into the patient experience and treatment effectiveness. With advancements in technology, the collection of PRO information has shifted from paper-based methods to electronic information capture, often utilizing participants' own devices (BYOD). This transition not only enhances accuracy of information but also boosts participant engagement.
Carrying out a comprehensive literature review to identify frequently utilized measures in comparable studies is crucial for contextual relevance and regulatory compliance. Furthermore, preserving the ability to adjust targets based on new information and continuous conversations with regulatory bodies can greatly improve a study's influence. The capacity to adjust goals as new data emerges guarantees that the research stays pertinent and in harmony with present scientific and regulatory environments.
In summary, best practices for selecting endpoints include early stakeholder engagement, alignment with regulatory expectations, incorporation of Pros, comprehensive literature reviews, and flexibility in adapting to new data. These practices collectively contribute to more robust and impactful clinical trials.
Conclusion
The selection of appropriate endpoints in clinical trials is fundamental to the success and integrity of research outcomes. Primary endpoints serve as the definitive measures of a treatment's effectiveness, while secondary endpoints enrich the understanding of the intervention's broader implications. Both types of endpoints must be meticulously defined, measurable, and relevant to ensure a robust evaluation of the treatment effects.
Statistical considerations play a pivotal role in endpoint selection. Researchers must determine sufficient sample sizes, mitigate biases, and account for multiple comparisons to validate their findings. Applying rigorous statistical methodologies, such as Bayesian approaches, enhances the flexibility and efficiency of clinical trials, allowing for ongoing assessments and adjustments as new data emerge.
Furthermore, best practices for endpoint selection emphasize the importance of engaging stakeholders early in the design process, aligning with regulatory expectations, and incorporating patient-reported outcomes. These strategies not only enhance the quality and reliability of clinical trials but also ensure that the research remains relevant and impactful in advancing medical knowledge and improving patient care.
In summary, a comprehensive approach to endpoint selection, grounded in statistical rigor and stakeholder collaboration, is essential for conducting successful clinical trials. This diligence ultimately supports the goal of delivering effective treatments and improving patient outcomes in various therapeutic areas.




