Overview
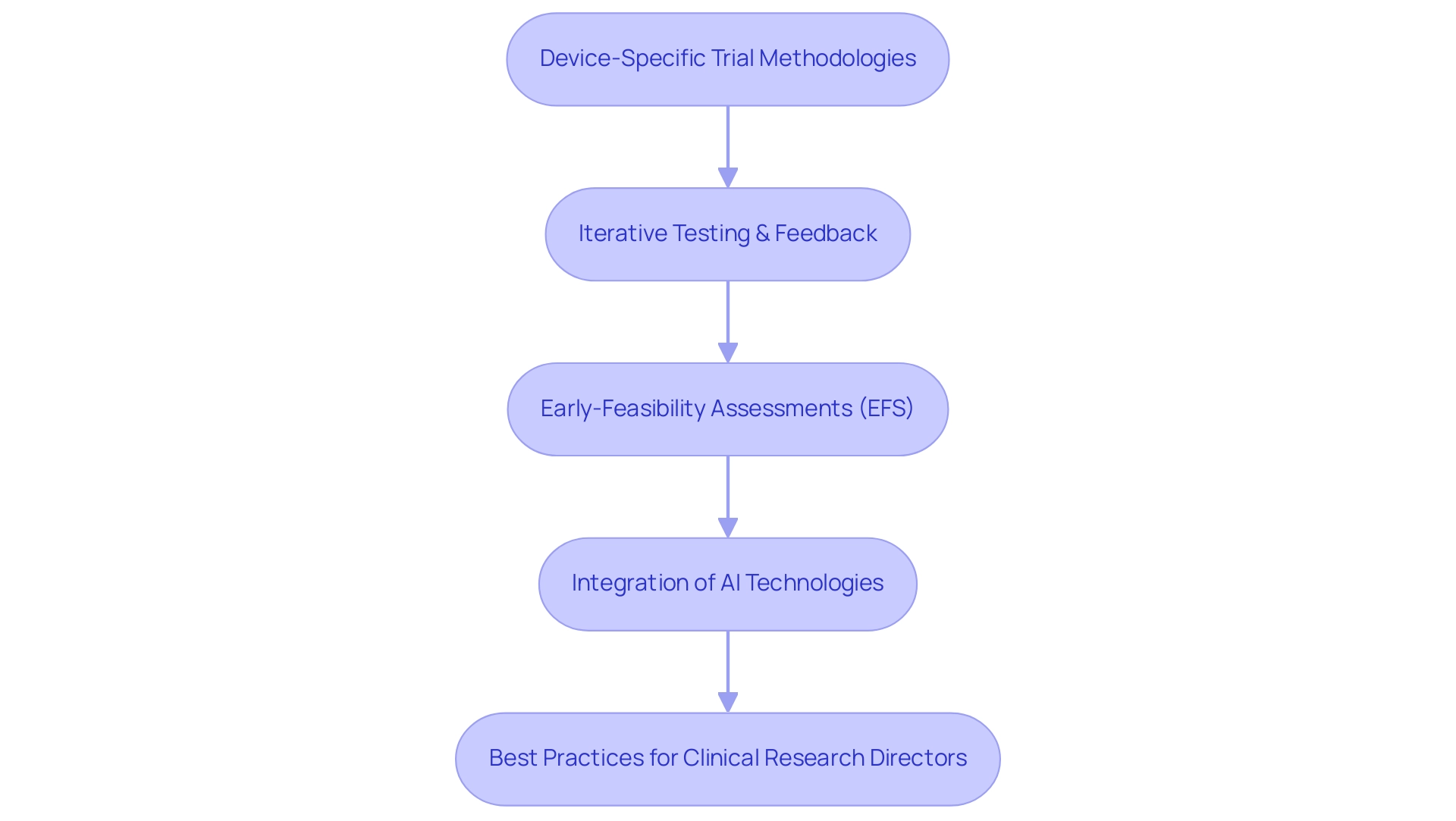
Device-specific trial methodologies are crucial for the effective evaluation of medical devices, addressing unique factors such as device functionality and user interaction, which differ significantly from traditional drug studies. This article underscores the critical importance of adopting best practices, including:
- Early-feasibility assessments
- Collaboration among multidisciplinary teams
Such strategies are essential for navigating the complexities of regulatory requirements and enhancing patient engagement in clinical research.
Introduction
In the rapidly evolving landscape of medical device trials, grasping the intricacies of device-specific methodologies is essential for success. Unlike traditional drug trials, these specialized approaches must navigate a complex web of regulatory requirements, patient recruitment challenges, and the imperative for real-world applicability. As the industry transitions towards innovative strategies such as early-feasibility studies and adaptive trial designs, stakeholders are increasingly acknowledging the significance of collaboration and technology integration. This article explores the key trends, challenges, and best practices that are shaping the future of medical device clinical trials, providing valuable insights for clinical research directors who seek to enhance trial efficiency and improve patient outcomes.
Understanding Device-Specific Trial Methodologies
Device-specific trial methodologies represent specialized approaches tailored to the unique characteristics of medical devices. In contrast to conventional drug studies, which primarily emphasize pharmacokinetics and pharmacodynamics, device evaluations must consider various factors, such as device functionality, user interaction, and real-world application. These methodologies often integrate iterative testing and feedback loops, facilitating continuous refinement of device design to ensure both safety and efficacy.
As we look to 2025, the landscape of device-specific testing methodologies is undergoing significant evolution, with a pronounced focus on early-feasibility assessments (EFS). These investigations are crucial for gathering initial data on device performance among a small patient cohort, allowing for necessary modifications prior to larger critical evaluations. Statistics indicate that early-feasibility studies are increasingly prevalent, reflecting a growing recognition of their value within the research process.
Moreover, the global market for precision oncology is projected to reach $98 billion this year, underscoring the critical role of effective device-specific trial methodologies in a rapidly expanding market.
Best practices for clinical research directors engaged in device studies include fostering collaboration among multidisciplinary teams to enhance user-centered design while ensuring compliance with the latest regulatory standards. The recent FDA proposal advocating for single Institutional Review Board (IRB) reviews for FDA-regulated research highlights the necessity of streamlining processes to expedite study initiation while maintaining rigorous oversight.
Expert insights underscore the distinctive features of medical device studies, emphasizing the need for a customized approach that prioritizes patient involvement and real-world applicability. The integration of artificial intelligence in clinical trials is revolutionizing methodologies by minimizing risks and costs, thereby enhancing patient engagement and accelerating the development of new therapies. As noted by the Head of Clinical Information Engineering, "Traditionally, management was outsourced to our CRO vendor partners."
This initiative aims to consolidate research in-house, enabling internal teams to adopt a more hands-on approach. By implementing research internally, we can take control of our data and deliver high-quality outcomes for our patients.
Successful examples illustrate the effectiveness of these methodologies, demonstrating how innovative approaches can yield improved results in medical device evaluations. For instance, ReGelTec's Early Feasibility Study on HYDRAFIL™ for treating chronic low back pain in Colombia exemplifies the successful application of EFS, showcasing how bioaccess®'s expertise in managing such studies can lead to significant advancements in patient care. Furthermore, AI technologies are being employed across various phases of drug development, from candidate selection to study administration, poised to transform the research process by reducing risks and costs, enhancing patient engagement, and potentially accelerating the creation of new treatments in a cost-conscious market.
As the industry adapts to these trends, research directors must remain vigilant in implementing best practices that align with the evolving landscape of medical device development.
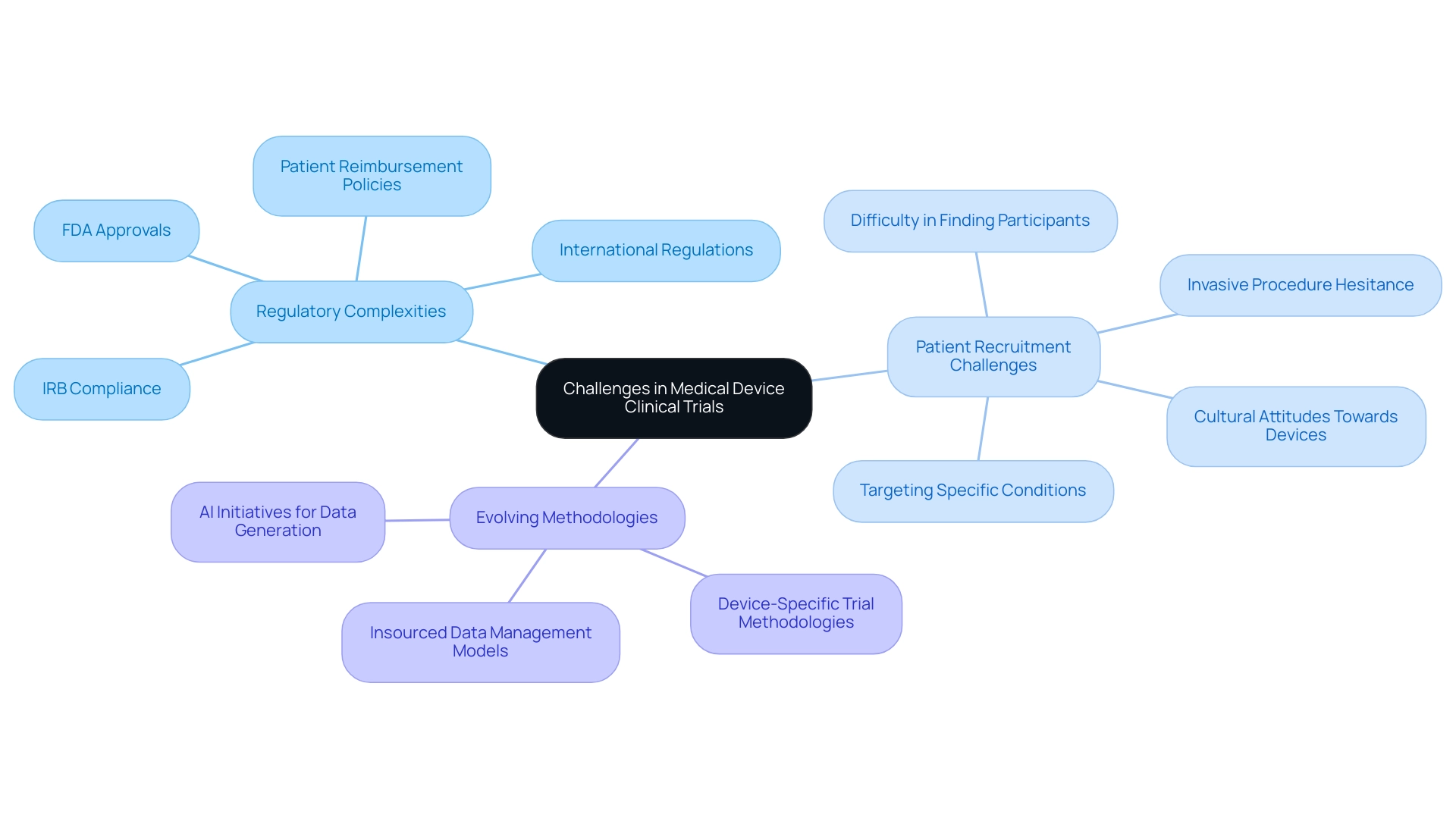
Challenges Unique to Medical Device Clinical Trials
Medical device clinical studies present a host of unique challenges, particularly in navigating regulatory complexities and patient recruitment. These challenges can be effectively managed through device-specific trial methodologies. Unlike pharmaceutical studies, device evaluations often require extensive preclinical testing and must traverse a multifaceted regulatory landscape that includes obtaining approvals from entities such as the FDA and Institutional Review Boards (IRBs). This complexity is further compounded by the necessity to comply with varying regulations across different countries, as highlighted by recent discussions among experts regarding the challenges posed by global studies.
These studies must contend with diverse regulatory environments, which can significantly impact enrollment and retention rates. Such impacts arise from differences in patient reimbursement policies, cultural attitudes towards medical devices, and the application of device-specific trial methodologies. Recruiting suitable patients for device studies can also present significant hurdles, particularly for those targeting specific conditions or demographics. For instance, studies involving implantable devices often struggle to find participants willing to undergo invasive procedures, leading to delays and increased costs. Statistics indicate that patient recruitment difficulties remain a pressing issue, with many studies reporting that only a fraction of eligible patients ultimately participate in studies. This underscores the importance of developing targeted recruitment strategies that align with device-specific trial methodologies and resonate with potential participants.
Furthermore, the trend towards insourced models for information management is transforming how sponsors approach clinical studies. With a growing demand for increased information ownership and transparency, sponsors are seeking technology that allows direct access to live information, thereby enhancing decision-making and streamlining trial processes. For example, 45% of Alcon's information is entered on the same day as the visit date, showcasing a commitment to management efficiency.
Additionally, Ibrahim Kamstrup-Akkaoui, Vice President of Data Systems Innovation, noted, "We did a small AI initiative to see if we can generate meaningful test data for setting up and validating our systems. It turns out we can." This emphasizes the developing approaches in research studies that can assist in tackling these challenges.
As research directors navigate these complexities, understanding the regulatory landscape and patient recruitment challenges is essential for devising effective strategies that incorporate device-specific trial methodologies. bioaccess™ provides extensive management services for research projects, including feasibility assessments, site selection, compliance reviews, setup, import permits, project management, and reporting on serious and non-serious adverse events, all crucial for overcoming these obstacles. The partnership between bioaccess™ and Caribbean Health Group, backed by Colombia's Minister of Health, seeks to establish Barranquilla as a premier location for medical research in Latin America, further enhancing the environment for medical device evaluations.
The case study titled "Challenges of Global Trials Due to Regulatory Disparities" illustrates the intricacies of varying regulations, cultures, and standards that present significant challenges for sponsors and sites. By incorporating these insights, research directors can better prepare for the complex challenges of medical device studies. To learn more about how bioaccess™ can assist you, BOOK A MEETING today.
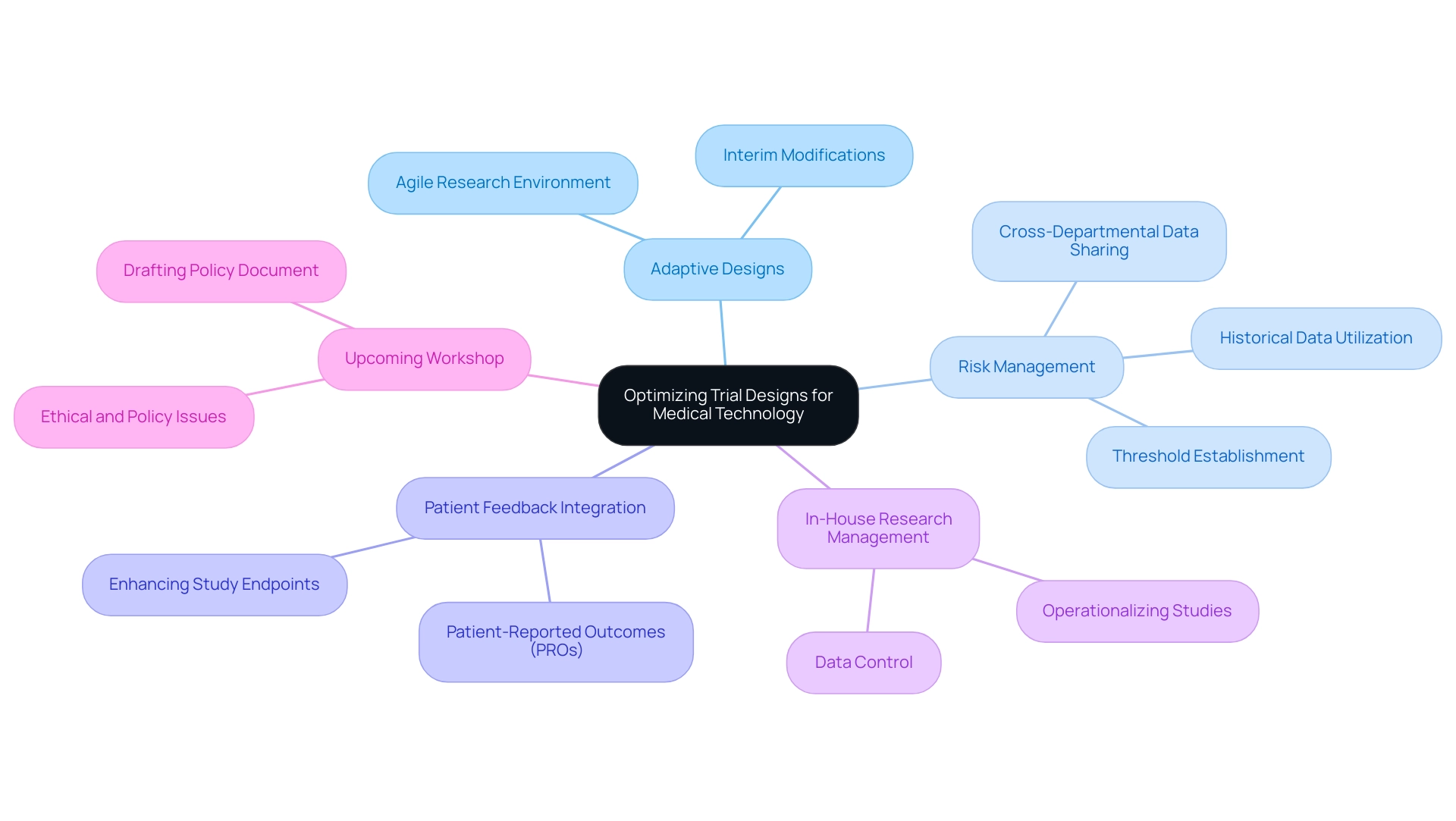
Optimizing Trial Designs for Medical Technology
Optimizing experimental designs for medical technology in 2025 necessitates the adoption of several pivotal strategies, with adaptive designs standing out as a key approach. These designs enable modifications based on interim results, fostering a more agile research environment that can lead to efficient resource utilization and expedited decision-making processes. Sponsors are increasingly utilizing historical trend information to proactively manage issues during clinical trials.
By establishing thresholds and facilitating cross-departmental data sharing, teams can monitor evolving trends and document remediation efforts, ultimately enhancing risk management and data quality. This proactive approach is exemplified in the case study titled "Proactive Issue Management Using Historical Data," which illustrates how sponsors can enhance risk management by identifying tolerable risks with mitigation plans in place.
Incorporating patient feedback into the study design process is another critical strategy that can significantly enhance the relevance of study endpoints and boost participant engagement. Utilizing patient-reported outcomes (PROs) allows researchers to gain valuable insights into how a device impacts quality of life, ensuring that the studies are aligned with patient needs. This approach not only meets regulatory requirements but also addresses the expectations of stakeholders, thereby increasing the likelihood of successful outcomes.
As mentioned by the Head of Clinical Information Engineering, "Traditionally, management was outsourced to our CRO vendor partners." Part of the initiative is to bring all our research in-house so that our internal teams can start working on it. They can be more hands-on, and we implement research in-house, allowing us to take control of our data and deliver high-quality results for our patients.
As research directors navigate the complexities of medical device studies, concentrating on these optimization strategies—such as adaptive study designs and the integration of patient feedback—will be essential for developing robust methodologies that drive innovation and enhance patient outcomes in the Medtech sector. Furthermore, utilizing extensive research management services such as those provided by bioaccess®, which encompass Early-Feasibility Studies (EFS), First-In-Human Studies (FIH), Pilot Studies, Pivotal Studies, and Post-Market Follow-Up Studies (PMCF), can further improve the efficacy of these strategies. The forthcoming workshop on April 25 at the MRC Biostatistics Unit will include discussions on essential ethical and policy issues in adaptive studies, further highlighting the significance of these methodologies in contemporary research practices.
Frank Bretz PhD, a key figure in methodological development in pharmaceutical statistics, supports the ongoing evolution of adaptive study designs, lending authority to this critical area of research.
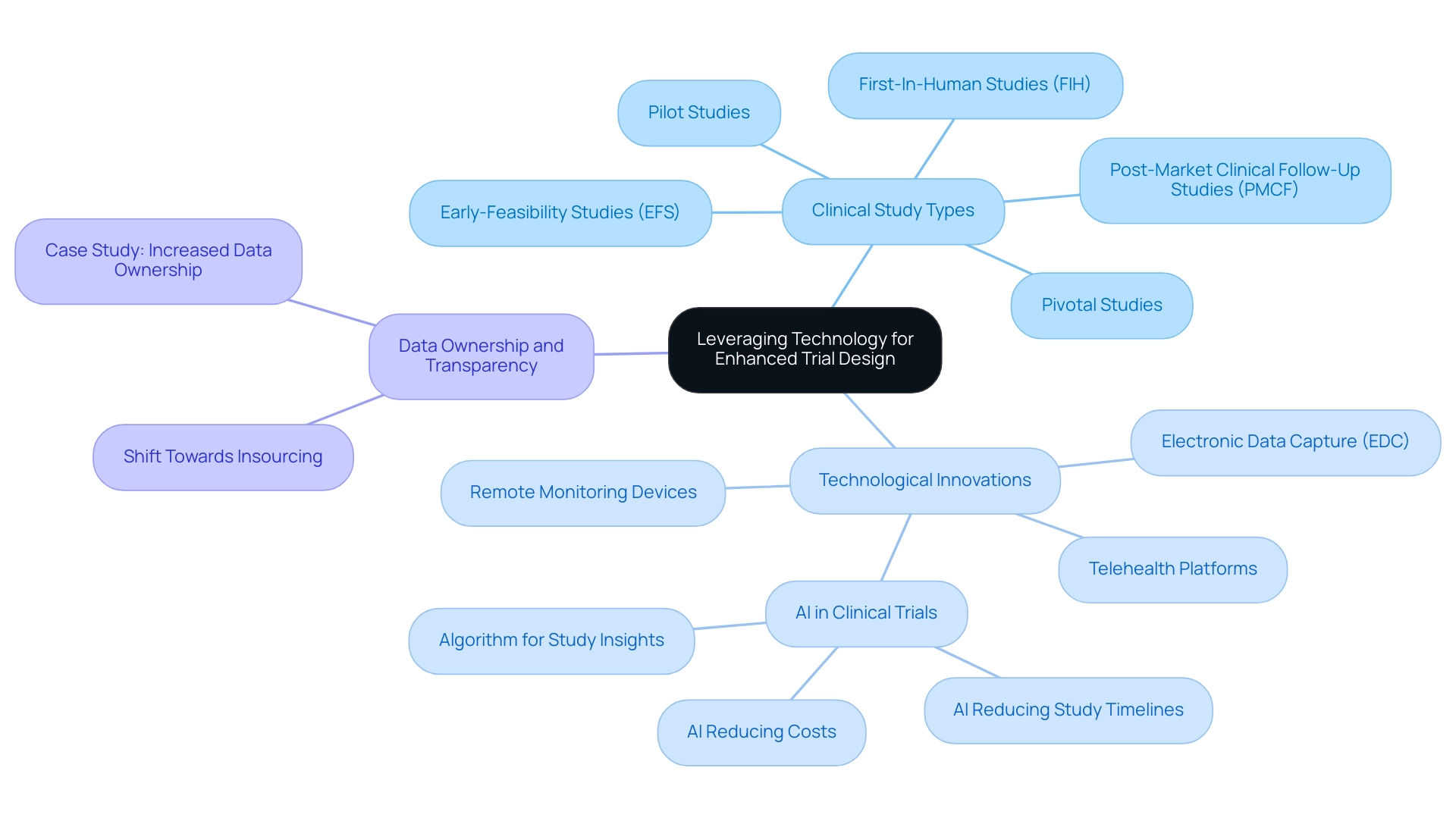
Leveraging Technology for Enhanced Trial Design
Utilizing device-specific trial methodologies in clinical study design is essential for enhancing efficiency and ensuring high-quality information. The adoption of electronic data capture (EDC) systems, remote monitoring devices, and telehealth platforms facilitates real-time data collection and fosters greater patient engagement through these methodologies. For instance, wearable devices that continuously monitor patient health metrics yield valuable insights that can significantly impact study outcomes.
At bioaccess®, we specialize in comprehensive clinical study management services, including:
- Early-Feasibility Studies (EFS)
- First-In-Human Studies (FIH)
- Pilot Studies
- Pivotal Studies
- Post-Market Clinical Follow-Up Studies (PMCF)
Our expertise guarantees that studies are crafted with the utmost accuracy and adaptability, incorporating device-specific trial methodologies to address the unique challenges of the Medtech sector in Latin America.
The impact of artificial intelligence (AI) on medical device evaluations is particularly noteworthy. AI-powered analysis can reveal patterns and enhance patient recruitment strategies, simplifying the overall study process. Recent studies indicate that integrating AI and machine learning in clinical trials can reduce study timelines by up to 30% and lower costs by as much as 20%.
This shift towards technology not only enhances operational efficiency but also aligns with the growing demand for device-specific trial methodologies that promote information transparency and ownership among sponsors. Moreover, the trend towards insourcing information management allows sponsors to maintain direct access to live data, thereby enhancing quality and delivery for patients. A case analysis titled 'Increased Information Ownership and Transparency for Sponsors' exemplifies this shift, highlighting how sponsors are increasingly seeking greater ownership and clarity of their information. This trend has resulted in completely insourced models that implement studies internally, improving information quality and operational efficiency.
Additionally, the global market for precision oncology is projected to reach $98 billion by 2025, underscoring the significance of advancements in device-specific trial methodologies within a growing market. As Ibrahim Kamstrup-Akkaoui, Vice President of Data Systems Innovation, noted, "We did a small AI initiative to see if we can generate meaningful test information for setting up and validating our systems." It turns out we can. An algorithm we developed examines past studies we set up, learns from the actual data collected, and utilizes it to generate insights for new studies. By adopting these technological innovations and leveraging the expertise of bioaccess®, research directors can enhance study designs and results by implementing device-specific trial methodologies while ensuring compliance with regulatory standards, ultimately advancing the field of medical technology.
Collaboration Among Stakeholders: Best Practices
Collaboration among stakeholders—including sponsors, investigators, regulatory bodies, and patients—is essential for the success of clinical studies. To promote effective partnerships, it is crucial to create clear communication channels, set mutual goals, and involve stakeholders early in the design process. Establishing advisory boards that include varied viewpoints can significantly enhance the relevance of study designs and improve patient recruitment strategies.
The FDA is actively encouraging sponsors to develop Diversity Action Plans, aimed at improving diversity in research studies, which aligns with the need for varied perspectives in study designs.
Furthermore, maintaining regular updates and feedback loops allows for timely addressing of concerns and adaptation to evolving circumstances. Notably, only 29% of sites report adequate training on new technologies and procedures, highlighting the necessity for effective communication and collaboration to overcome these training gaps. As Jim Reilly noted, "Now that sponsors see the limits of disconnected, best-of-breed solutions, the industry is ready to standardize and simplify."
In this context, bioaccess™ provides an extensive range of management services for research studies, including:
- Feasibility assessments
- Site selection
- Compliance evaluations
- Setup
- Import permits
- Project management
- Reporting
This comprehensive approach not only tackles the regulatory obstacles and recruitment difficulties encountered by medical device startups but also establishes Barranquilla as a prominent hub for research in Latin America, backed by the partnership with Caribbean Health Group and the support of Colombia's Minister of Health.
Prioritizing collaboration streamlines processes and cultivates a more cohesive and efficient environment, ultimately leading to better outcomes and advancements in medical technology. Additionally, improving outcome measurement in clinical studies through patient-reported outcomes and biomarker identification can be significantly enhanced by stakeholder collaboration, illustrating the practical benefits of working together.

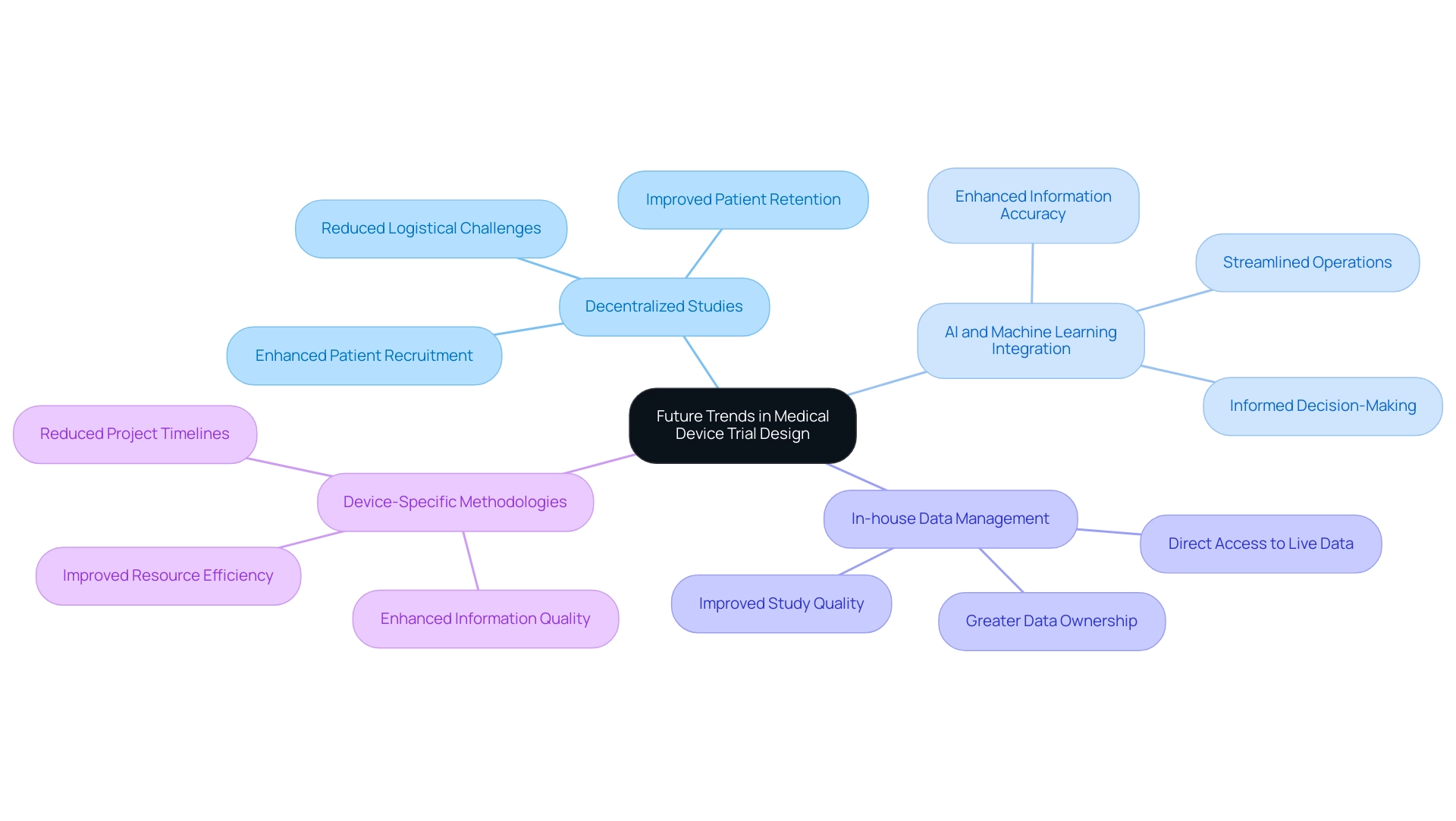
Future Trends in Medical Device Trial Design
The landscape of medical device study design is on the brink of significant transformation, particularly through the adoption of device-specific trial methodologies driven by several pivotal trends. One of the most remarkable trends is the rise of decentralized studies, which facilitate remote patient observation and information gathering. This innovative approach not only enhances patient recruitment and retention but also alleviates the logistical challenges associated with in-person visits.
By reducing the burden on participants, decentralized studies can lead to more comprehensive information gathering and increased patient involvement. Furthermore, ICH E6 R2 (and R3 revisions) mandates sponsors to manage risk in a manner that lessens the burden on sites, reinforcing the value of decentralized methodologies.
Moreover, the integration of artificial intelligence (AI) and machine learning into study design and information analysis is set to revolutionize the clinical research process. These technologies promise to streamline operations, enhance information accuracy, and support more informed decision-making throughout the trial lifecycle. As the Head of Clinical Information Engineering noted, "Traditionally, management was outsourced to our CRO vendor partners."
Part of the initiative is to bring all our research in-house, allowing our internal teams to engage more directly with the work. This hands-on approach enables us to implement research internally, gain control over our data, and deliver high-quality outcomes for our patients. This perspective underscores the shift towards greater ownership and quality of information.
Statistics indicate that the transition towards device-specific trial methodologies in medical research is expected to enhance information quality, improve resource efficiency, and reduce project timelines. This evolution is crucial, especially considering the economic challenges faced by the industry, which often lead to delays in new product development and diminished workforce capacities. The comprehensive clinical research management services provided by bioaccess—including feasibility assessments, site selection, compliance reviews, setup, import permits, project management, and reporting—are designed to effectively navigate these challenges.
Additionally, the case study titled "Increased Data Ownership and Transparency by Sponsors" illustrates how organizations are adapting to new guidelines, moving towards insourced models for data management, thereby improving the quality of their studies. By embracing these forward-thinking methodologies, organizations can not only address current challenges but also position themselves for future success in the competitive medtech landscape.
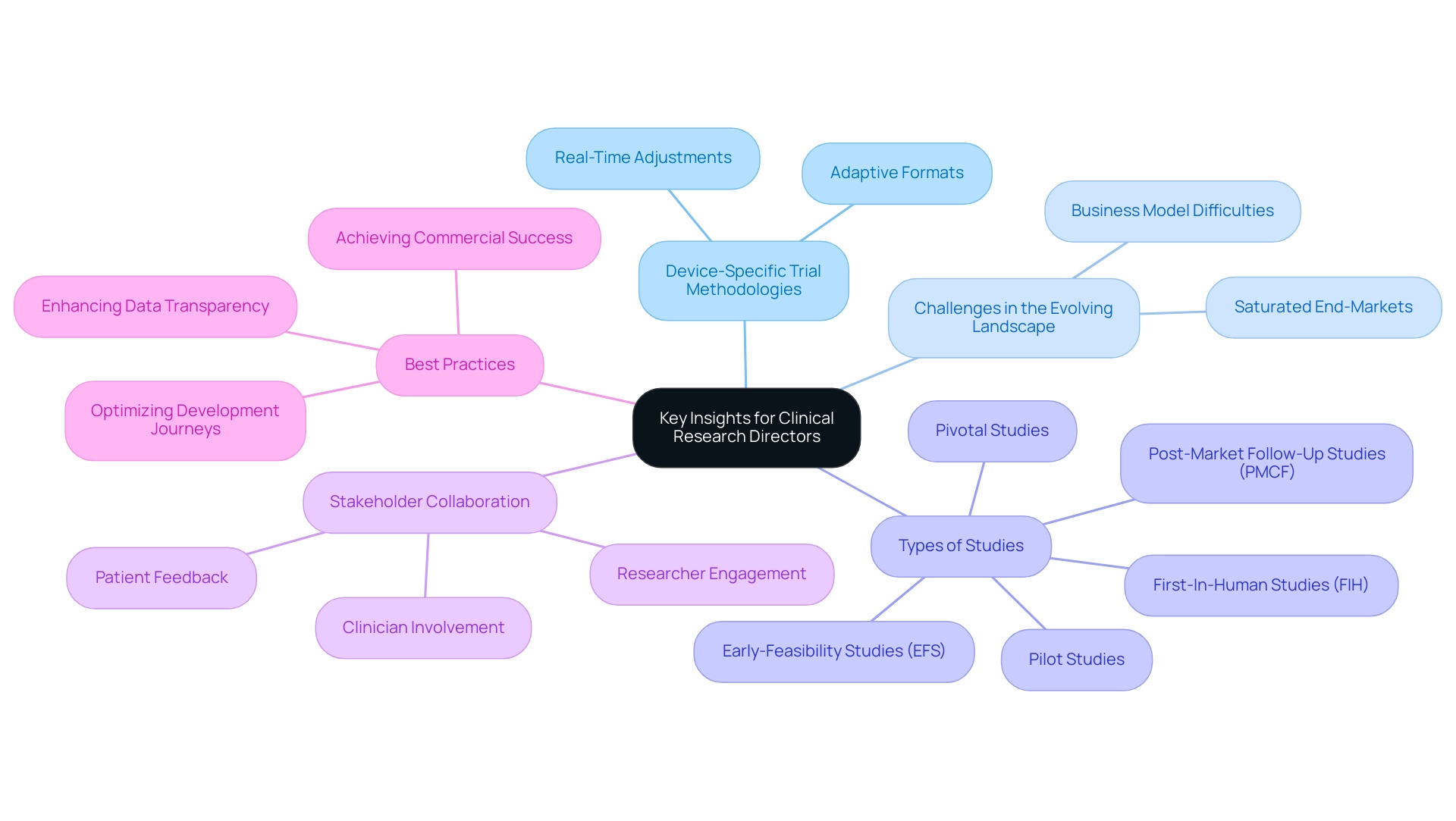
Key Insights and Best Practices for Clinical Research Directors
Clinical research directors must prioritize a comprehensive understanding of device-specific trial methodologies to navigate the unique challenges inherent in medical device studies. As the landscape evolves in 2025, optimizing experimental designs becomes crucial, particularly through the adoption of adaptive formats that allow for real-time adjustments based on interim results. This adaptability not only improves the effectiveness of studies but also significantly influences research results by aligning them more closely with patient needs and regulatory expectations.
bioaccess® provides accelerated medical device research study services in Latin America, leveraging over 20 years of expertise in managing:
- Early-Feasibility Studies (EFS)
- First-In-Human Studies (FIH)
- Pilot Studies
- Pivotal Studies
- Post-Market Follow-Up Studies (PMCF)
This specialized knowledge is essential for research directors aiming to effectively navigate the complexities of medical device trials through device-specific trial methodologies.
Max Baumann, Head of Execution at Treehill Partners, observes, "As we approach 2025, we still see biotech encountering essential business model difficulties as end-markets become increasingly saturated." This statement emphasizes the necessity for research directors to adapt their strategies in response to an increasingly competitive environment.
In 2022, there were around 106 early phase-I interventional studies and a total of 2,478 phase-I interventional studies, highlighting the growing complexity and volume of clinical trials. Utilizing technology is crucial for enhancing information collection and analysis. Sponsors are increasingly demanding solutions that provide direct access to live information, which facilitates informed decision-making while still allowing for the outsourcing of certain functions to contract research organizations (CROs).
This shift towards a more insourced model emphasizes the importance of full data transparency, enabling sponsors to maintain control over their data assets.
Encouraging cooperation among stakeholders—including researchers, clinicians, and patients—can yield valuable insights that improve study designs. Leveraging patient feedback not only guides the development process but also ensures that studies are aligned with real-world needs, ultimately leading to improved patient outcomes.
The case study titled "Commercial Outcomes in Drug Development" illustrates the challenges faced by the biopharma industry, emphasizing the need for optimizing development journeys to achieve not only approval-enabling endpoints but also commercial success. By implementing these best practices, clinical research directors can significantly improve the efficiency and effectiveness of medical device trials through device-specific trial methodologies. This proactive approach not only supports successful product commercialization but also contributes to the advancement of innovative medical technologies that can transform patient care.
Conclusion
The medical device trial landscape is evolving rapidly, making it imperative for clinical research directors to grasp device-specific methodologies to enhance trial efficiency and patient outcomes. Emerging trends, including early-feasibility studies and adaptive trial designs, are revolutionizing trial conduct. These shifts underscore the necessity for collaboration among stakeholders and the integration of technology, streamlining processes while ensuring trials align with real-world applications. This alignment ultimately fosters better patient engagement and improved results.
Unique challenges in medical device trials, particularly regulatory complexities and patient recruitment, demand targeted strategies. The transition to insourced data management models and the incorporation of artificial intelligence in trial design further emphasize the need for transparency and efficiency in clinical research. By embracing these innovative approaches, clinical research directors can mitigate risks and adeptly navigate the intricate regulatory landscape.
Looking forward, the adoption of decentralized trial designs and advanced technologies will be crucial in transforming clinical trials. This evolution promises enhanced data quality, reduced study timelines, and improved patient experiences. By prioritizing collaboration, optimizing trial designs, and leveraging cutting-edge technologies, clinical research directors can strategically position themselves for success in an increasingly competitive medtech environment. Embracing these best practices will not only advance innovative medical technologies but also ensure that today’s trials pave the way for tomorrow’s breakthroughs.
Frequently Asked Questions
What are device-specific trial methodologies?
Device-specific trial methodologies are specialized approaches designed to evaluate medical devices, taking into account factors like device functionality, user interaction, and real-world application, which differ from conventional drug studies.
How do device evaluations differ from conventional drug studies?
Unlike drug studies that focus on pharmacokinetics and pharmacodynamics, device evaluations emphasize the device's functionality, user interaction, and real-world applications, incorporating iterative testing and feedback loops to refine design for safety and efficacy.
What is the significance of early-feasibility assessments (EFS)?
Early-feasibility assessments are critical for gathering initial performance data on a device among a small patient cohort, allowing for necessary modifications before larger evaluations, and their prevalence is increasing in the research process.
What is the projected market size for precision oncology?
The global market for precision oncology is projected to reach $98 billion, highlighting the importance of effective device-specific trial methodologies in this expanding market.
What best practices should clinical research directors follow in device studies?
Best practices include fostering collaboration among multidisciplinary teams to enhance user-centered design and ensuring compliance with regulatory standards, such as the recent FDA proposal for single Institutional Review Board (IRB) reviews.
How is artificial intelligence impacting clinical trials for medical devices?
The integration of artificial intelligence in clinical trials is revolutionizing methodologies by minimizing risks and costs, enhancing patient engagement, and accelerating the development of new therapies.
What challenges do medical device clinical studies face?
Medical device studies encounter regulatory complexities, patient recruitment difficulties, and the need for extensive preclinical testing, often requiring navigation through various regulatory environments.
Why is patient recruitment a significant issue in device studies?
Recruiting suitable patients can be challenging, especially for studies involving invasive procedures, leading to delays and increased costs, with many studies reporting low participation rates among eligible patients.
What is the trend towards insourced models for information management in clinical studies?
There is a growing demand for increased information ownership and transparency, leading sponsors to seek technology that provides direct access to live information, enhancing decision-making and trial efficiency.
How can bioaccess™ assist with the challenges of medical device studies?
bioaccess™ offers extensive management services for research projects, including feasibility assessments, site selection, compliance reviews, project management, and reporting on adverse events, which are essential for overcoming study obstacles.

