Introduction
Clinical trials are crucial for evaluating the safety and efficacy of new medical interventions. Compliance with ethical, regulatory, and legal mandates is essential for the integrity of these studies, as they have the potential to revolutionize patient care. This article will explore key considerations for ensuring compliance in clinical trials, including the importance of informed consent, adherence to Good Clinical Practice (GCP) guidelines, and the challenges posed by emerging technologies.
It will also discuss best practices for maintaining compliance, such as training and education, standard operating procedures, quality assurance, and documentation. Furthermore, a case study will be presented to highlight the successful compliance measures in a phase III clinical trial for an anti-cancer drug. By understanding the importance of compliance and implementing best practices, clinical trials can achieve higher standards and contribute to significant advancements in medical treatments.
Key Considerations for Ensuring Compliance
Clinical trials embody essential medical research mechanisms that critically appraise the safety and efficacy of new medical interventions, which range from drugs to devices and behavioral therapies. Compliance with ethical, regulatory, and legal mandates is a non-negotiable cornerstone of these studies, given their potential to revolutionize patient care and directly impact patient outcomes.
Ensuring informed consent is more than a procedural step; it is an ethical imperative, fostering participants' autonomy and comprehension of the trial's scope. Institutional Review Boards (IRBs) extend their guardianship of human subjects by scrutinizing the protocols and informed consent forms to affirm the protection of participants' rights and welfare.
Good Clinical Practice (GCP) guidelines are the gold standard to which researchers must rigorously adhere, thus safeguarding trial integrity and the credibility of data collected. Navigating the complexities of regulatory compliance necessitates acute awareness and operational adaptation to evolving standards, notably with emerging technologies such as artificial intelligence and machine learning within the life sciences sector.
The introduction of guidelines like the EU AI Act underscores the importance of a "risk-based approach" and increased transparency. On a pragmatic level, EHR-sourced studies unveil challenges and opportunities as they leverage existing trial sites to fulfill study aims effectively. However, at times, subject participation could mean facing logistical hurdles, such as when a patient from rural Pennsylvania considers joining a trial in Turkey—a scenario that exemplifies both the global reach of clinical studies and the intricate personal considerations it entails, including data privacy and participant confidentiality. As Kaplan, an expert in clinical research standards, posits, the robustness of a trial's data is directly linked to its adherence to high standards, historically involving multiple controlled investigations but now also accommodating the evolving FDA approval processes catalyzed by the 21st Century Cures Act, which allows a single well-executed trial to suffice. Ethical considerations have evolved to recognize the validity of compensating participants fairly for their contributions, paralleling other public services roles, ensuring that public health advancements don't come at the unfair expense of those participating in the crucial trials enabling these advancements.
Best Practices for Clinical Trial Compliance
Clinical trials, pivotal for ensuring the safety and efficacy of new medical treatments, are governed by stringent compliance protocols to protect patient welfare and maintain data integrity. Key practices that fortify adherence to these protocols include:
- Training and Education: Ensuring all personnel are well-versed in regulatory requirements mitigates non-compliance risks.
Not only does this foundational knowledge support the trial's integrity, but it empowers teams to confidently manage unforeseen challenges. 2. Standard Operating Procedures (SOPs): Mandating SOPs for trial conduct, data management, and crucial reporting practices secures consistent compliance across the study's operations.
Streamlining procedures through SOPs fosters uniform understanding among team members. 3. Quality Assurance and Auditing: Proactive internal audits and quality checks reveal early indicators of non-compliance, allowing for immediate rectification.
Moreover, readiness for external audits fortifies a trial's standing with regulatory bodies. 4. Documentation and Record Keeping: Comprehensive and methodical documentation practices are paramount for trial transparency, ensuring that every aspect from enrollment to adverse event reporting is accurately recorded.
- Pharmacovigilance: Vigilant monitoring and reporting of safety data is a linchpin of trial compliance. Effective pharmacovigilance systems not only underscore participant safety, but they also ensure adherence to reporting protocols.
Furthermore, clinical trials integrate a series of progressive phases, each essential to the clinical research narrative. Early phases concentrate on safety and proof of concept in a small cohort, while subsequent stages expand focus on treatment efficacy within the targeted patient population, ultimately influencing clinical guidelines and patient care. However, the complexity of clinical trials extends beyond procedural compliance, touching upon the human aspect of clinical research.
Envision a patient from rural Pennsylvania, poised to join a life-saving trial abroad, grappling with logistical hurdles such as travel and language barriers. Such challenges underscore the multifaceted nature of trial participation and the dire need for comprehensive participant support systems. By marrying strict compliance practices with compassionate participant engagement, clinical trials can reach new pinnacles of success.
Case Study: Successful Compliance in Clinical Trials
Clinical trials are the backbone of medical advances, meticulously examining new interventions such as drugs, devices, or behavioral therapies. In the ecosystem of patient care, the integrity of these trials is foundational for ensuring treatment safety and efficacy.
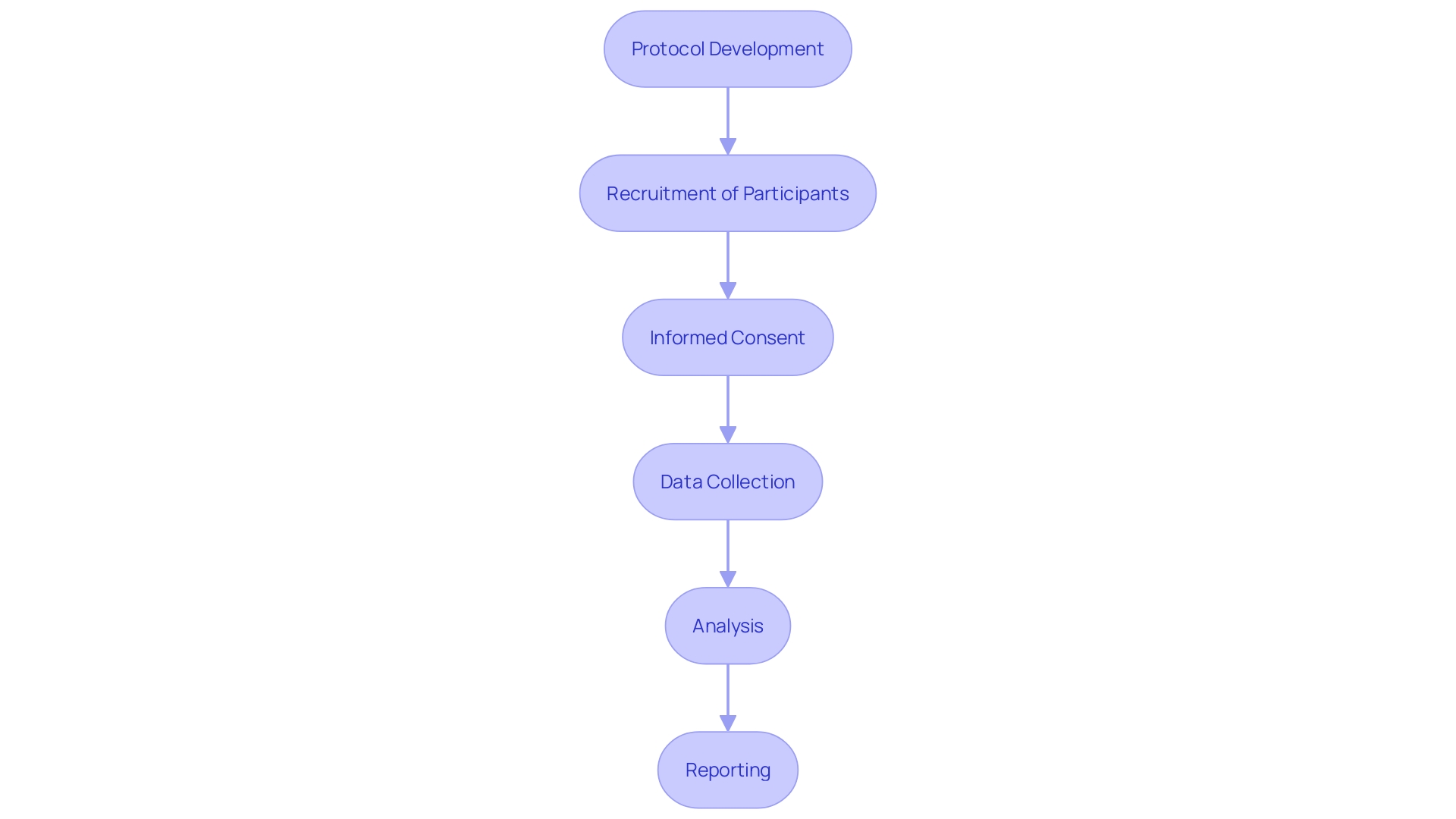
A clinical trial's journey is marked by various stages, commencing with phase one where the safety of a new treatment is scrutinized with a small cohort of healthy volunteers. Progressing to phase two, researchers enlist patients who can potentially benefit from the intervention, aiming to gauge its effectiveness as well as safety.
The paramount nature of these trials is evident when considering their impact: the advancement of superior treatments that can revolutionize patient outcomes. In navigating the ethical terrain of clinical trials, there's a contemporary shift.
Where previously payments to participants might have been seen as potential conflicts, today's perspective acknowledges the importance of fair treatment. As ethical considerations evolve, it becomes apparent that participants, much like first responders, should be justly compensated for their contributions, which extend beyond personal benefit to societal advancements in public health.
This recognition balances the responsibility of participant involvement with the deserved acknowledgment of their sacrifices for the common good. In light of a case study focused on a phase III clinical trial for an anti-cancer drug, key compliance measures become salient. From informed consent that empowers patients through understanding to rigorous adherence to Good Clinical Practice (GCP) guidelines, these steps are indispensable. The sustenance of such trials rests on the precepts of regulatory compliance, safeguarding participant rights, and the accrual of incontrovertible data. Such was the case with the investigational drug's trial, which, through steadfast compliance, yielded results that promise a leap in patient treatment. The study's compelling findings exemplify the pivotal role that well-governed clinical trials play in heralding new, efficacious medical therapies that may significantly improve patient survival rates.
Conclusion
In conclusion, compliance is a vital aspect of clinical trials, ensuring the integrity of the studies and the potential to revolutionize patient care. Key considerations for ensuring compliance include obtaining informed consent and adhering to Good Clinical Practice (GCP) guidelines.
The challenges posed by emerging technologies, such as artificial intelligence and machine learning, require a risk-based approach and increased transparency. Furthermore, best practices for maintaining compliance include training and education, standard operating procedures, quality assurance, and thorough documentation.
These measures contribute to the high standards necessary for clinical trials to achieve significant advancements in medical treatments. It is crucial to recognize that clinical trials are not just about procedural compliance but also about the human aspect of research.
Participant support systems and comprehensive engagement are necessary to address logistical hurdles and ensure the success of trials. By combining strict compliance practices with compassionate participant care, clinical trials can reach new levels of success.
A case study focusing on a phase III clinical trial for an anti-cancer drug exemplifies the importance of compliance measures. By obtaining informed consent and adhering to GCP guidelines, this trial yielded compelling results that have the potential to significantly improve patient survival rates. This case study highlights how well-governed clinical trials play a pivotal role in advancing medical therapies. In conclusion, maintaining compliance in clinical trials is not only ethically and legally crucial but also critical for driving medical advancements. By implementing best practices and upholding high standards, clinical trials can continue to contribute to significant improvements in patient care and outcomes.




