Overview
This article underscores best practices and expert recommendations essential for ensuring patient safety in the design of clinical trials for medical devices. It highlights the necessity of robust patient protection protocols, continuous monitoring for adverse events, and strict adherence to regulatory frameworks. These elements are critical for maintaining participant safety and enhancing the credibility of research findings. By implementing these practices, stakeholders can significantly mitigate risks and foster a safer clinical research environment.
Introduction
In the realm of clinical trials, patient safety transcends being a mere regulatory checkbox; it forms the bedrock of trust and credibility. As the stakes escalate with the advent of innovative medical technologies, the unwavering commitment to safeguarding participants' rights and well-being emerges as paramount.
This article explores the multifaceted strategies that ensure patient safety throughout the clinical research process, encompassing everything from the initial phases of trial design to the critical monitoring of adverse events and post-market surveillance.
By examining best practices and expert recommendations, it underscores how organizations such as bioaccess® are at the forefront of prioritizing safety, ultimately enhancing the integrity of clinical trials and the efficacy of medical devices.
As the landscape of medical research continues to evolve, comprehending these principles is essential for advancing healthcare solutions that prioritize patient welfare.
The Crucial Role of Patient Safety in Clinical Trials
Patient protection serves as the cornerstone of clinical studies, ensuring the rights, security, and well-being of participants throughout the research process. This unwavering commitment not only cultivates trust among participants but also significantly enhances the credibility of research findings. Effective patient protection measures are essential for maintaining patient safety in device trial design, preventing adverse events, and ensuring that trials are conducted ethically and responsibly.
For instance, the implementation of robust protection protocols and continuous monitoring can substantially mitigate risks associated with new medical devices. This ultimately leads to improved patient outcomes and ensures patient safety in device trial design while facilitating regulatory approval.
In 2023, the total number of reports related to serious events and high-harm incidents saw an increase, underscoring the ongoing need for high-quality reporting and patient protection practices. This trend emphasizes the significance of fostering a culture that promotes error reporting and concentrates on system enhancement, which is essential for improving patient well-being. As noted by the Institute of Medicine (IOM), fatigue during shift work increases error rates and must be addressed to enhance patient well-being, further emphasizing the need for comprehensive protective measures.
Organizations like bioaccess® exemplify how prioritizing patient well-being can accelerate the development of innovative medical technologies in Latin America. With more than 20 years of experience in Medtech, bioaccess® effectively oversees a variety of studies, including:
- Early-Feasibility Studies (EFS)
- First-In-Human Studies (FIH)
- Pilot Studies
- Pivotal Studies
- Post-Market Follow-Up Studies (PMCF)
Their tailored method ensures that patient safety in device trial design is prioritized in clinical research, highlighting the value of applying thorough monitoring protocols.
A significant case examination is the BMT CTN 0601 investigation, which evaluated the effectiveness and protection of bone marrow transplants for children with severe sickle cell disease. This phase II study utilized monitoring protocols to track adverse outcomes within 100 days post-transplant. The research disclosed that no warning signals would have been identified under any of the monitoring guidelines evaluated, highlighting the need for careful design in oversight protocols.
Moreover, the Gs method has been recognized as possessing the greatest capability for detecting toxicity rates, underscoring the significance of employing effective statistical techniques in study design. By incorporating these optimal methods, research studies can guarantee participant protection and uphold patient safety in device trial design while also improving the overall integrity and success of medical device creation.

Understanding Regulatory Frameworks for Clinical Trials
Regulatory frameworks play a crucial role in shaping the structure and implementation of research studies, ensuring that patient safety in device trial design is upheld alongside the highest ethical standards and participant safety. Agencies such as the FDA and EMA provide comprehensive guidelines governing various aspects of research, including participant recruitment, informed consent, and adverse event reporting. For instance, the FDA's Good Clinical Practice (GCP) guidelines delineate the responsibilities of sponsors and investigators, emphasizing the necessity of safeguarding participant welfare throughout the trial process.
As we move into 2025, adherence to FDA and EMA regulations remains essential, especially as the healthcare landscape becomes increasingly competitive. The FDA has recognized the importance of electronic signatures for consent documentation, streamlining processes while maintaining rigorous standards for participant engagement. With the growing emphasis on commercial results, understanding these regulatory requirements is crucial for research organizations (CROs) like bioaccess®.
By effectively navigating the complexities of local and international regulations, researchers can not only reduce risks but also enhance the overall safety and integrity of medical studies. Bioaccess® offers an extensive service that includes feasibility and selection of research locations, investigator selection, and regulatory compliance, ensuring that all documents meet country-specific requirements. This proactive approach addresses common challenges faced by medical device startups, such as regulatory hurdles and recruitment issues, while also managing financial constraints through efficient project management and monitoring.
Additionally, special considerations must be made for vulnerable populations in clinical research, as emphasized in a recent case analysis on protections for these groups. This research underscores the ethical responsibilities to prioritize the rights and welfare of participants, particularly children, pregnant women, and individuals with impaired decision-making capacity. Ensuring that informed consent is obtained appropriately is paramount, reflecting a commitment to ethical research practices.
Moreover, participants should be informed about the reasons for study termination and any implications for their involvement in future studies, further protecting their rights and welfare. As the regulatory landscape evolves, staying informed about the latest updates and requirements is crucial for successful study design. Expert opinions suggest that a continued focus on optimizing development journeys will be necessary to achieve not only approval-enabling endpoints but also to qualify for commercial success. Max Baumann, Head of Execution, emphasizes this point, stating, "We expect continued focus on optimizing the development journeys of assets to achieve not only an approval-enabling endpoint but to qualify for commercial success."
By adhering to established regulatory frameworks and prioritizing data protection, bioaccess® can play a pivotal role in advancing medical devices while ensuring patient safety in device trial design and maintaining ethical integrity in clinical research. For any queries or concerns regarding data protection, please contact our Grievance Officer at IMH ASSETS CORP (doing business as "bioaccess®").
BOOK A MEETING.

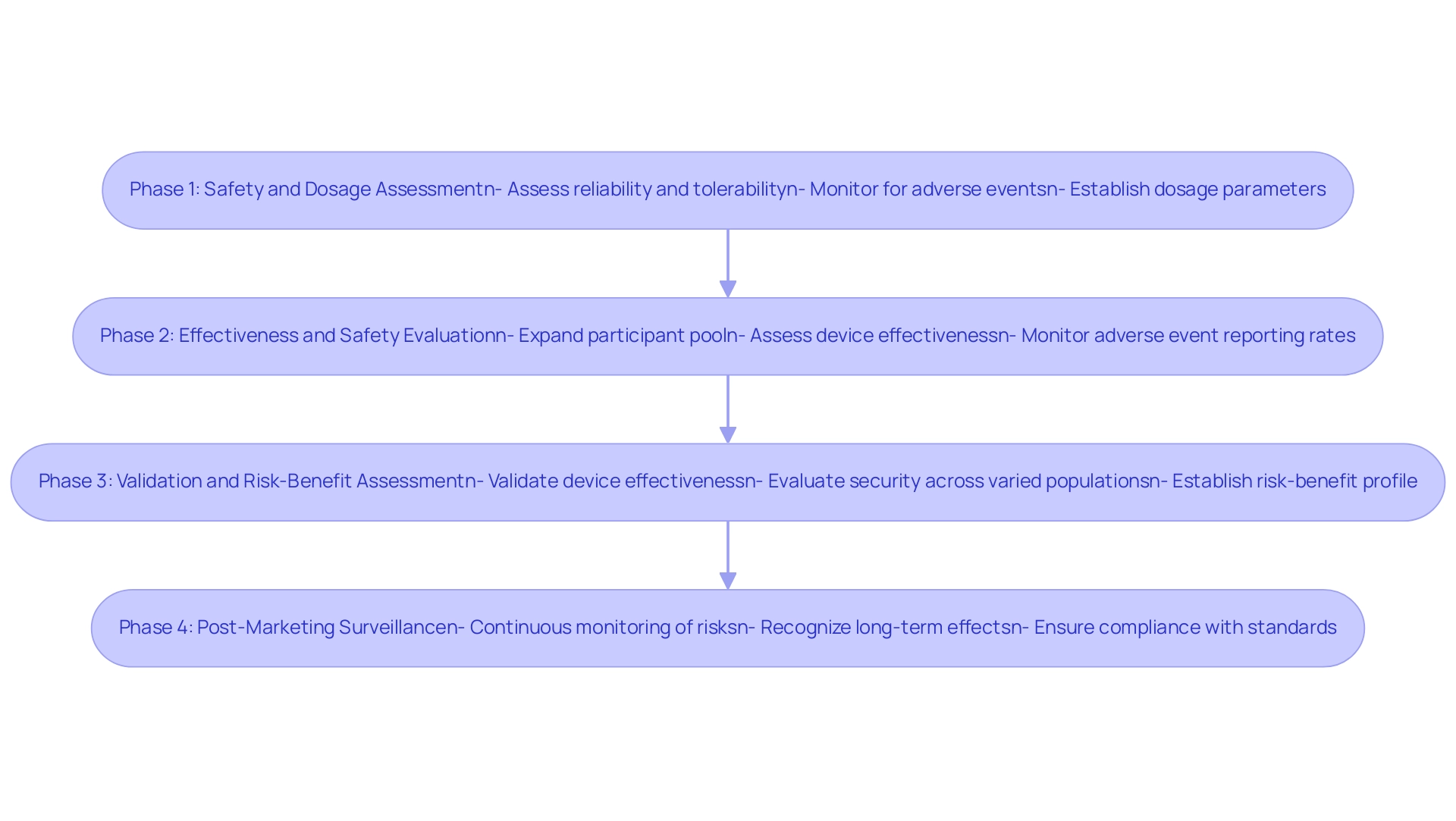
Navigating the Phases of Clinical Trials: Ensuring Safety at Every Step
Clinical studies are systematically classified into four phases, each defined by specific goals and precautionary measures. In Phase 1, the primary objective is to assess the reliability and tolerability of a new device among a limited group of participants. This phase is critical, involving rigorous monitoring for adverse events and establishing dosage parameters.
Recent trends indicate that monitoring protocols in Phase 1 are essential for swiftly identifying and addressing any adverse events, thereby ensuring participant well-being throughout the study. A case study titled 'The Significance of Phase 1 Clinical Evaluations in Drug Development' underscores how these assessments play a vital role in risk evaluation, dosage determination, and pharmacokinetic insights, providing essential data that guide the continuation of treatment development.
As the examination progresses to Phase 2, the participant pool expands, enabling a more thorough assessment of the device's effectiveness while maintaining a strong emphasis on security. This phase frequently uncovers crucial insights into the device's performance and potential risks, with adverse event reporting rates closely monitored to ensure that patient safety in device trial design concerns are promptly addressed.
Phase 3 studies involve extensive research aimed at validating the device's effectiveness and further evaluating security across varied populations. These assessments are pivotal in establishing the device's risk-benefit profile, particularly regarding patient safety in device trial design, before it reaches the market. Organizations such as bioaccess®, a prominent contract research organization supporting medical device evaluations in Latin America, implement customized protection protocols during this phase, ensuring that extensive monitoring systems are established to safeguard participant well-being.
Significantly, Dr. Jorge Hernando Ulloa recently presented one-year first-in-human data on the VenoValve® at the Charing Cross International Symposium, highlighting advancements in vascular medicine and the importance of thorough clinical study design.
Ultimately, Phase 4 assessments, or post-marketing evaluations, serve an essential function in the continuous monitoring of risks once the device is accessible to the public. These studies assist in recognizing any long-term effects and ensure that the device continues to comply with standards. With over 15 years of expertise in the Medtech field, bioaccess® is dedicated to enhancing medical devices while emphasizing patient safety in device trial design through careful study design and optimization strategies.
This commitment is reflected in their approach to safety monitoring across all phases, ensuring that patient safety in device trial design is prioritized while also meeting regulatory requirements and enhancing patient outcomes. As part of our commitment to transparency and compliance, we encourage users to manage their cookie preferences by visiting our cookie settings page. For inquiries related to industry research agreements, please reach out to Tamika Merrick, Director of CTC-SR, at tmerrick@mednet.ucla.edu.
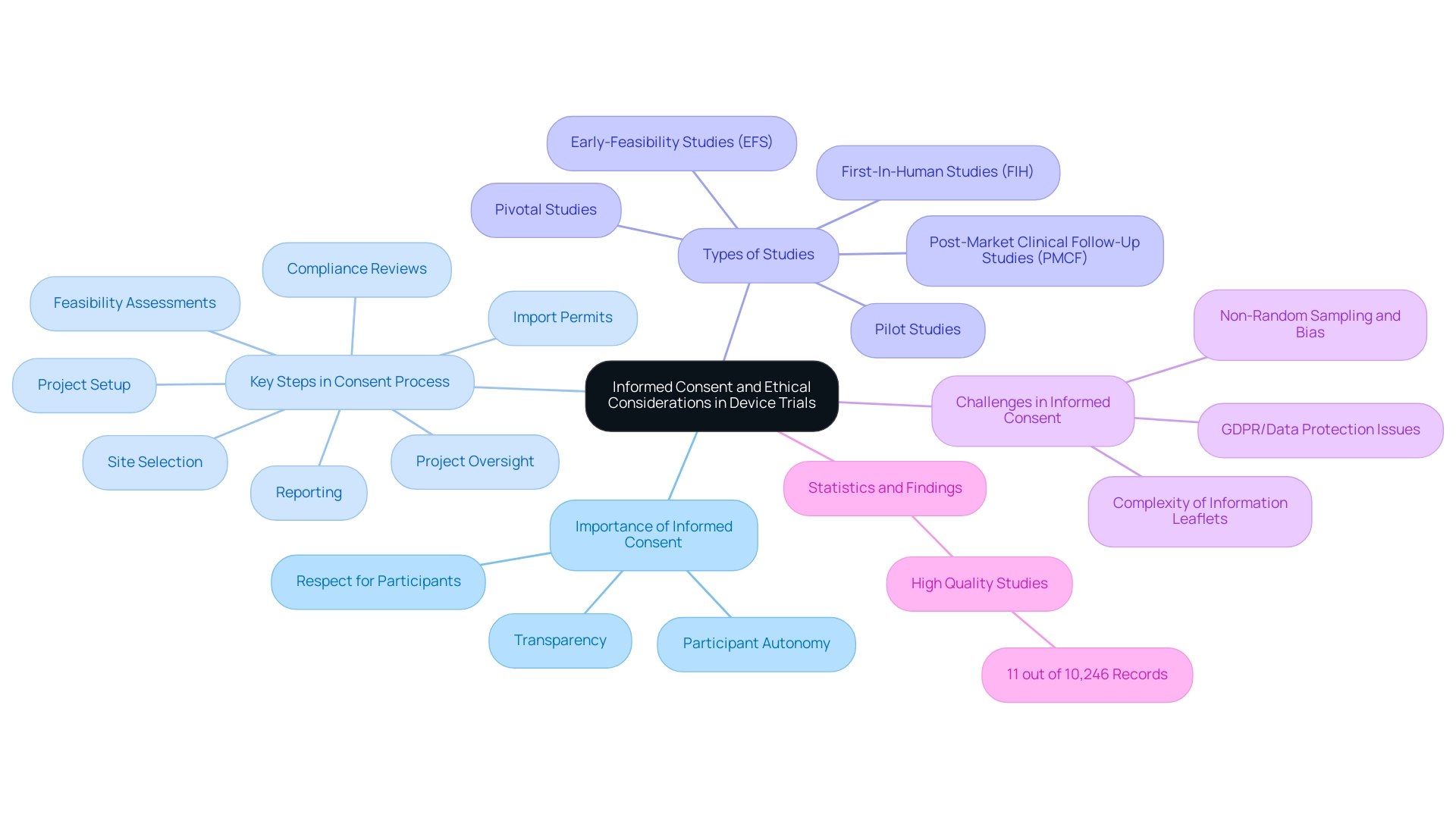
Informed Consent and Ethical Considerations in Device Trials
Informed consent stands as a cornerstone of medical studies, guaranteeing that participants are fully cognizant of the associated risks and benefits of their involvement. This process must be transparent, empowering participants to make informed decisions about their participation. Ethical considerations in research extend beyond mere compliance; they embody a profound respect for participant autonomy and the duty to furnish comprehensive information regarding the study's nature and implications.
Organizations like bioaccess® highlight the critical importance of clear communication throughout the consent process. With over 20 years of experience in Medtech, bioaccess® utilizes plain language and visual aids to bolster participants' understanding, which is essential for grasping informed consent. Their extensive clinical research management services include:
- Feasibility assessments
- Site selection
- Compliance reviews
- Project setup
- Import permits
- Project oversight
- Reporting
All of which fortify a robust informed consent process.
bioaccess® specializes in managing:
- Early-Feasibility Studies (EFS)
- First-In-Human Studies (FIH)
- Pilot Studies
- Pivotal Studies
- Post-Market Clinical Follow-Up Studies (PMCF)
Ensuring a tailored approach to each study.
Recent statistics reveal that only 11 out of a substantial pool of research, encompassing 10,246 records and resulting in 114 evaluations post-screening, were classified as high quality. This underscores the necessity for rigorous attention to ethical practices in clinical trials.
Furthermore, ongoing discussions regarding consent are particularly crucial in long-term research. These dialogues ensure that participants remain informed about any new risks or modifications in the research protocol, fostering a culture of transparency and trust. Case analyses have shown that well-organized informed consent procedures not only enhance participant retention but also improve the overall integrity of the research.
As highlighted in a recent analysis, limitations such as non-random sampling and potential biases in participant selection can influence the generalizability of findings, emphasizing the importance of meticulous consideration in research designs.
The complexity of information leaflets, especially concerning GDPR/data protection, presents additional challenges. As noted by Research staff 018, "Info leaflets are getting more complicated with GDPR/data protection information. It is almost impossible to make it shorter without risking rejection by ethics committee."
This emphasizes the necessity for clarity in informed consent documents.
As the landscape of medical research evolves, ensuring patient safety in device trial design will be vital for the success of medical device studies in 2025 and beyond. bioaccess®'s extensive experience in pilot projects, first-in-human trials, and other domains positions them uniquely to enhance best practices in informed consent processes, particularly in the context of Latin America.
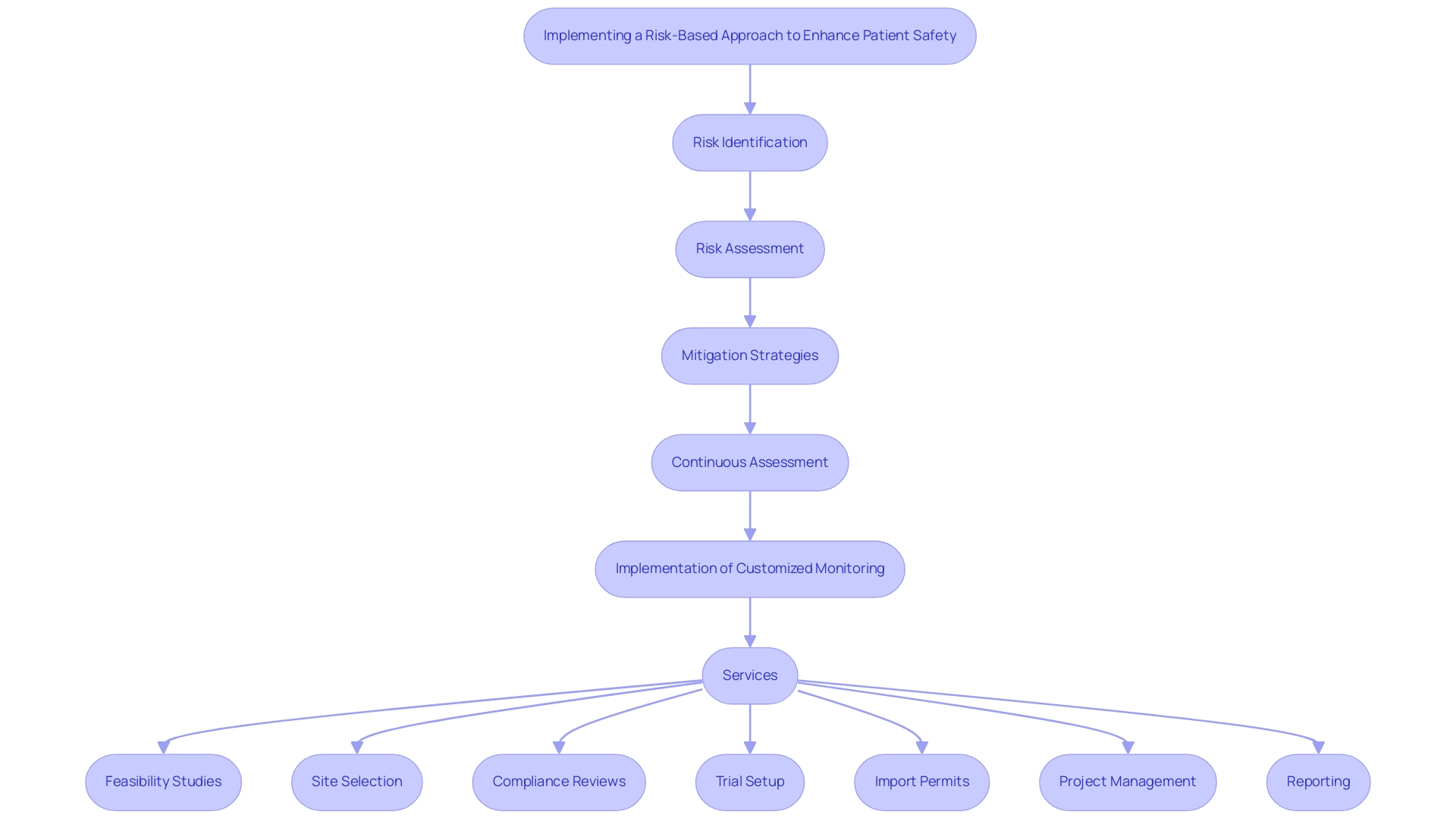
Implementing a Risk-Based Approach to Enhance Patient Safety
A risk-oriented strategy for study design is essential for enhancing patient safety in device trial design and maximizing resource distribution. This methodology emphasizes the early identification of potential risks, enabling researchers to implement targeted mitigation strategies. Comprehensive risk assessments can identify vulnerable populations and specific device-related risks that require increased monitoring efforts.
Organizations like bioaccess®, which specializes in accelerated medical device clinical research services in Latin America, strive to facilitate the advancement of medical devices from first-in-human trials to commercialization. They employ risk-based monitoring methods to customize protective measures based on the unique needs of each trial. By continuously assessing risks throughout the research process, bioaccess® ensures that patient safety in device trial design remains a top priority while adapting strategies in real-time.
This proactive approach not only enhances the effectiveness of oversight but also contributes to cost reduction. Data from completed risk-based monitoring studies indicate that the implementation of RBM can improve patient safety in device trial design while simultaneously enhancing the efficiency and effectiveness of oversight.
Moreover, the adoption of risk-based quality management (RBQM) practices is on the rise, yet there remains significant potential for improvement in research methodologies. Expert recommendations underscore the importance of conducting risk assessments 'as early as possible' to safeguard patient safety in device trial design, aligning with insights from regulatory bodies that advocate for proactive risk management.
A notable case analysis titled "Random Sampling Method in Medical Experiments" illustrates the effective application of a random sampling technique in medical experiments. This approach involved evaluating overall research risks and documenting critical variables to develop a monitoring plan that integrates both fixed and random variable monitoring. The result was a representative set of critical variables for monitoring, culminating in a Study Monitoring Report that summarized significant findings and data trends.
This process enabled sponsors to effectively assess study status and make timely adjustments to their monitoring activities, demonstrating the advantages of a structured risk-based strategy in research design.
In addition to these methodologies, bioaccess® offers a comprehensive range of services including:
- Feasibility Studies
- Site Selection
- Compliance Reviews
- Trial Setup
- Import Permits
- Project Management
- Reporting
All tailored to meet the specific requirements of studies in Latin America.
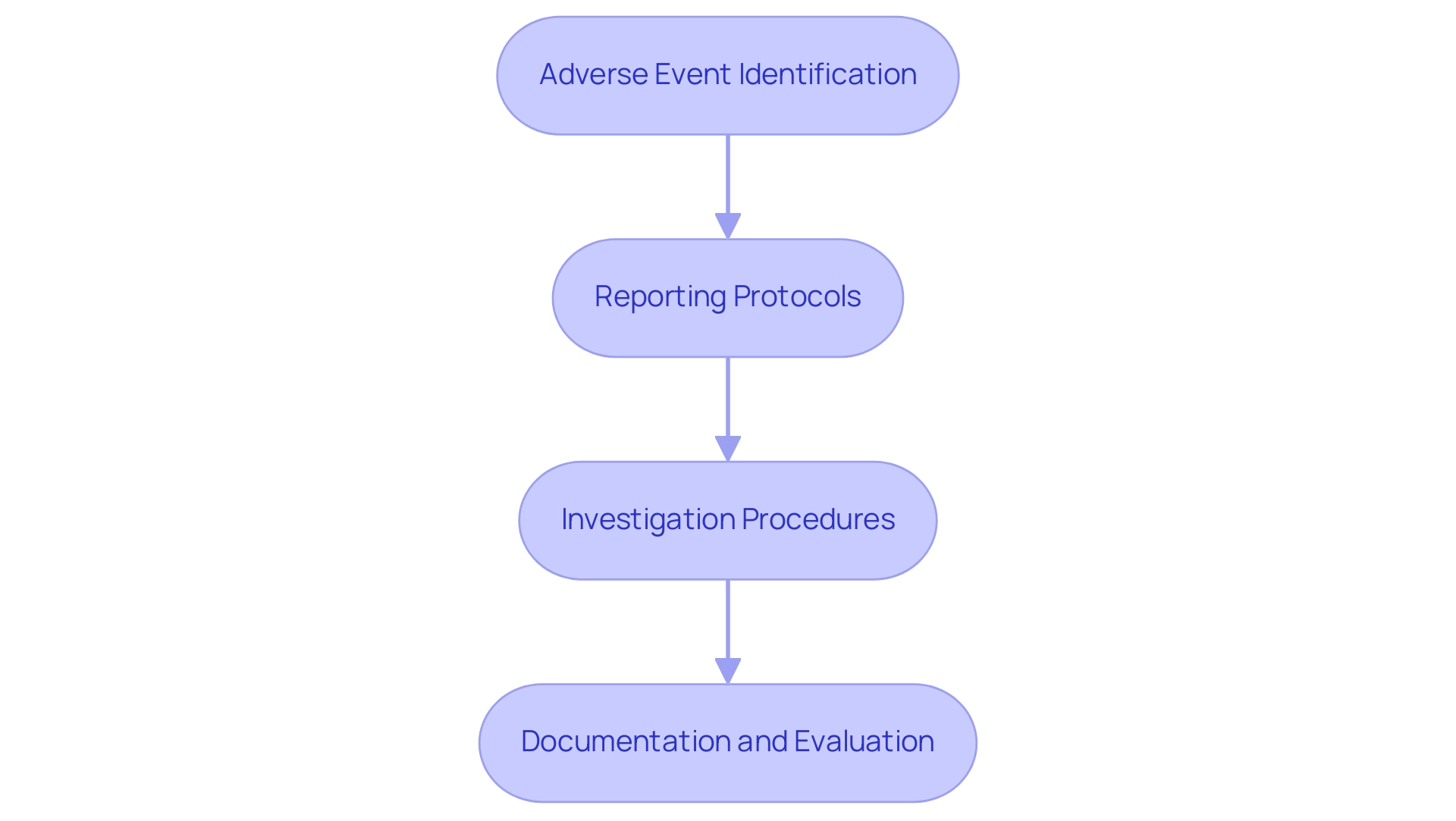
Monitoring Adverse Events: A Key Component of Patient Safety
Monitoring adverse events is crucial for ensuring patient safety in the design of device trials. A well-organized adverse event reporting system enables researchers to promptly identify and address concerns as they arise. This system must include clear protocols for reporting, investigating, and documenting adverse events, ensuring that every incident is meticulously evaluated.
Organizations like bioaccess®, a leading contract research entity in Latin America, implement comprehensive monitoring strategies that encompass regular evaluations and thorough data audits. By leveraging their extensive research management services—including feasibility assessments, site selection, compliance evaluations, project setup, import permits, project oversight, and reporting—bioaccess® cultivates a culture of transparency and accountability. This significantly enhances participant well-being and safeguards the integrity of the research.
Recent advancements in adverse event monitoring further underscore its significance. For instance, the BMT CTN 0601 study applied stopping rules to mitigate the risk of negative outcomes, utilizing the Pocock test, which indicated the lowest anticipated numbers of assessed patients and adverse events. This approach exemplifies how effective monitoring can lead to improved patient outcomes.
Moreover, a study advocating for enhanced reporting standards in research trials, particularly concerning COVID-19 drugs, emphasized the necessity for stricter submission requirements and adherence to CONSORT harms recommendations. These policy changes aim to bolster the completeness and reliability of data reporting on protection, ultimately enhancing drug security for patients. This aligns with findings from six articles published between 2004 and 2013, which proposed eight Bayesian methods to analyze emerging adverse event data, further highlighting the need for robust analytical frameworks in monitoring.
Integrating best practices in adverse event reporting systems not only bolsters patient safety in device trial design but also elevates the overall quality of medical research. As Rachel Phillips stated, "All authors have read and approved the manuscript," reflecting a commitment to rigorous reporting standards. By prioritizing the oversight of negative occurrences, entities like bioaccess® can ensure that research studies uphold patient safety in device trial design while adhering to the highest principles of protection and effectiveness.
The case study titled 'Policy Recommendations for Improving Reporting Standards' serves as a concrete example of the pressing need for enhanced data reporting, reinforcing the argument for better practices in clinical trials.
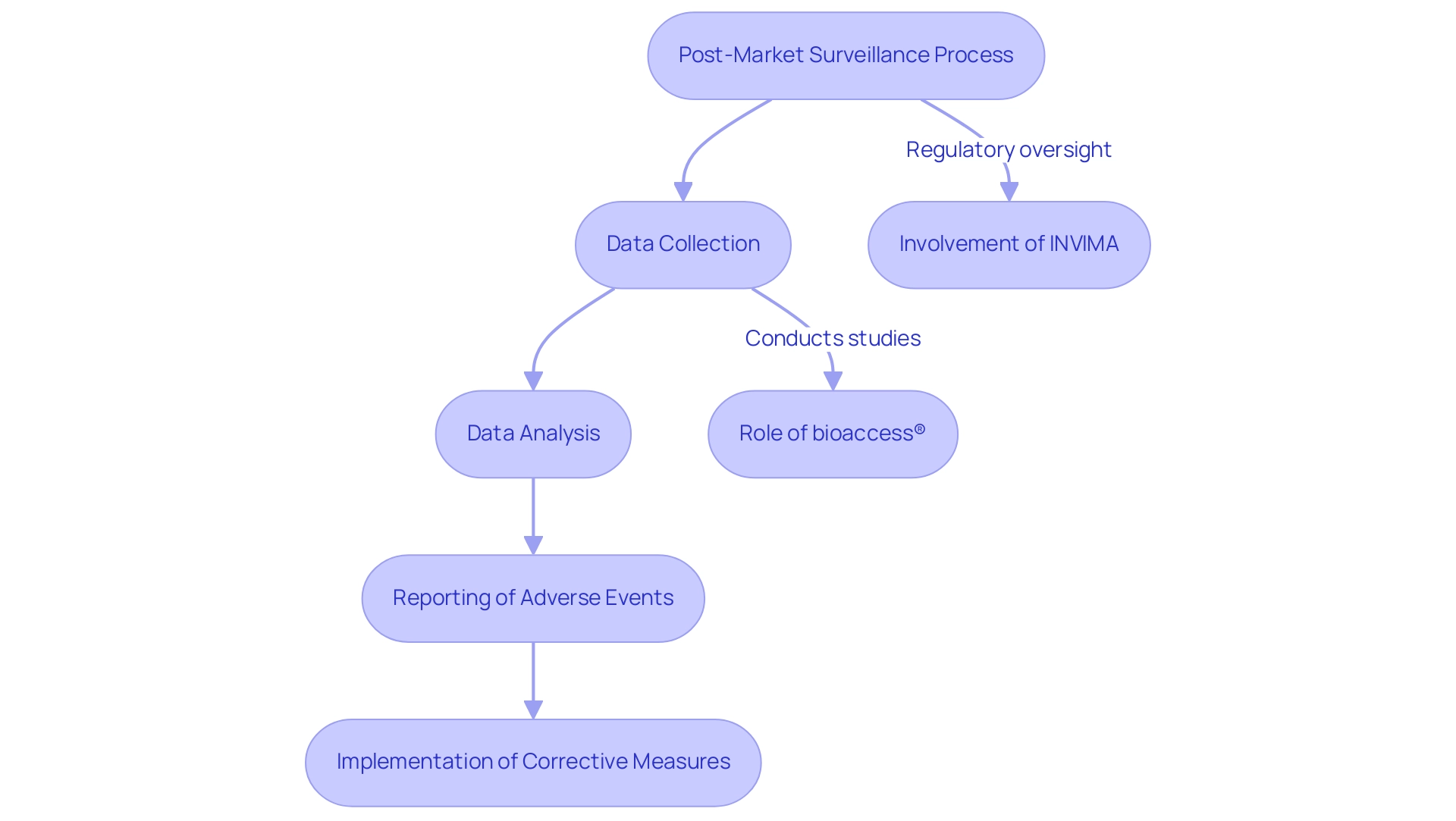
Post-Market Surveillance: Ensuring Long-Term Patient Safety
Post-market surveillance (PMS) is a critical process that extends beyond the initial approval of a medical device, focusing on the continuous monitoring of its reliability and effectiveness in real-world settings. This ongoing supervision is essential for identifying any long-term concerns that may emerge once a device is widely utilized. Regulatory agencies, including INVIMA in Colombia, require manufacturers to develop robust post-market surveillance plans, which involve systematic data collection, thorough analysis, and timely reporting of adverse events.
Organizations like bioaccess® play a pivotal role in conducting these post-market studies, drawing on over 20 years of Medtech expertise to ensure that medical devices consistently meet quality standards. By leveraging real-world data and participant feedback, bioaccess® researchers can swiftly identify potential risk concerns and implement necessary corrective measures. This proactive approach not only enhances device security but also fosters patient safety in device trial design, building trust among healthcare providers and patients alike.
Current trends in post-market surveillance underscore the growing significance of long-term monitoring strategies for well-being. For example, biostatistical analysis has proven effective in supporting updates to product labeling, including new indications and dosage adjustments. This statistic highlights the effectiveness of PMS in adapting to evolving medical needs.
Moreover, the integration of advanced informatics capabilities, exemplified by the NIH CTSA teams collaborating with the FDA and CMS, is transforming how data is collected and analyzed, resulting in more informed decision-making.
The importance of post-market evaluations cannot be overstated; they are vital in ensuring device reliability and effectiveness over time. As the landscape of medical technology evolves, so too must the strategies employed for post-market monitoring. Ongoing training and enhancement in PMS procedures are essential, as demonstrated by the case study titled 'Training and Continuous Improvement in PMS,' which illustrates that frequent staff training boosts the efficiency of surveillance systems, ultimately leading to improved device reliability and customer satisfaction.
In 2025, the emphasis on post-market health monitoring is more pronounced than ever, with expert opinions underscoring the necessity of these practices for patient safety in device trial design. Dr. Walker aptly noted, "The cost of implementing the envisioned system pales in comparison with the billion dollars being spent to renovate the Hard Rock Cafe in Las Vegas," emphasizing the value of investing in PMS. Furthermore, the significance of PMS spans multiple medical device categories, including psychiatric medications, where post-market monitoring could address concerns that often lag behind other drugs in investigation.
As the medical device industry continues to innovate, ensuring patient safety in device trial design through thorough post-market monitoring will remain a fundamental aspect of clinical research, guaranteeing that devices not only meet initial quality standards but also adapt to the realities of patient use.
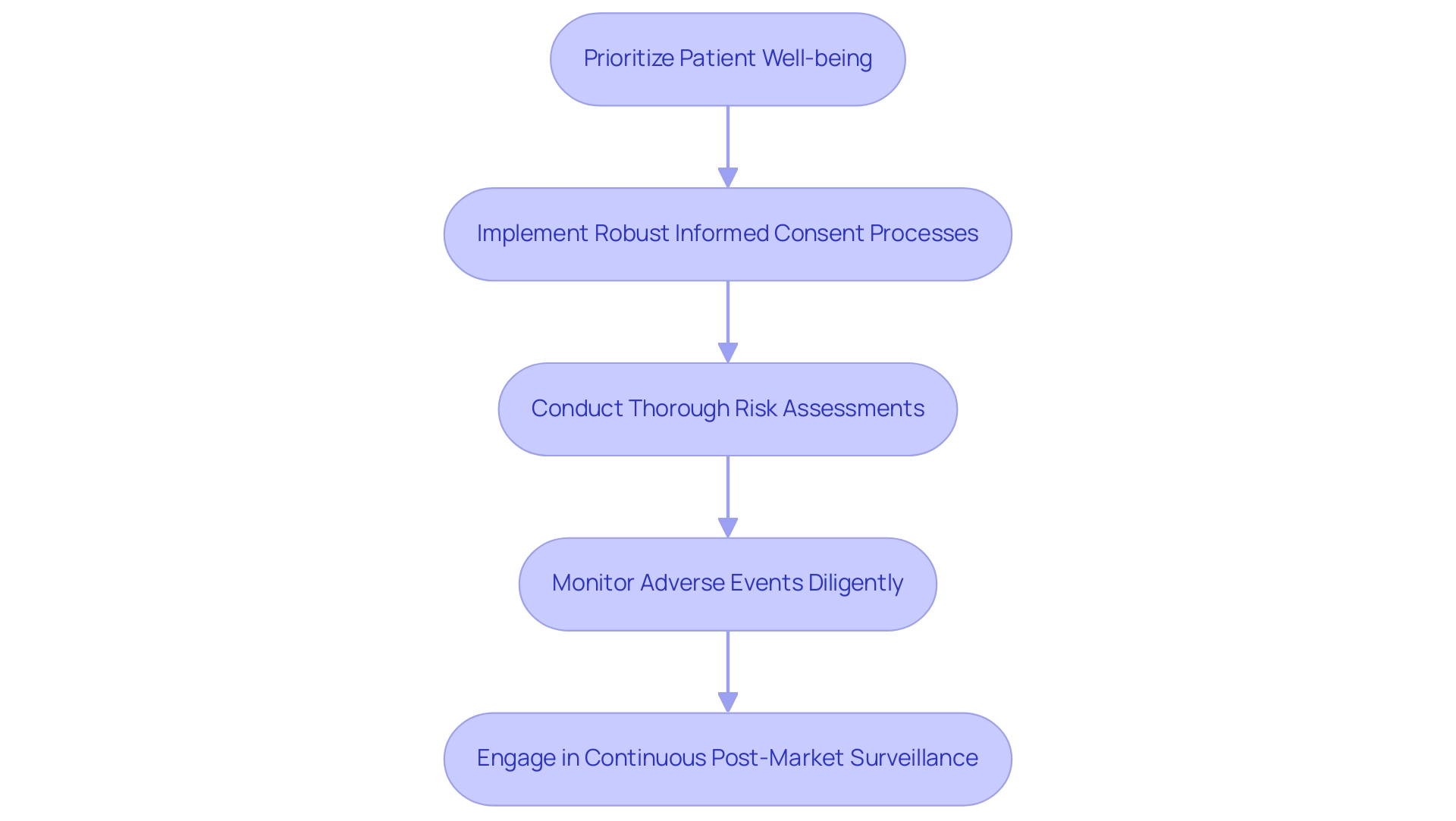
Best Practices and Expert Recommendations for Safe Device Trials
To ensure patient safety in device trials, researchers must adopt best practices that are both effective and ethical:
- Prioritize Patient Well-being: Cultivating a culture that emphasizes patient well-being at every organizational level is crucial. This commitment should be evident in all testing processes and decision-making. Given that patient harm is the third leading cause of death in the U.S., ensuring patient safety in device trial design transcends regulatory compliance; it is a moral imperative.
- Implement Robust Informed Consent Processes: It is essential to guarantee that participants are thoroughly informed about the risks and benefits associated with the study. Clear communication fosters trust and empowers patients to make informed decisions.
- Conduct Thorough Risk Assessments: Early identification of potential risks allows for the development of effective mitigation strategies. Thorough risk evaluations must be a fundamental component of the design process, particularly to ensure patient safety in device trial design concerning bioaccess®'s proficiency in handling Early-Feasibility and First-In-Human investigations.
- Monitor Adverse Events Diligently: Establishing clear protocols for the reporting and management of adverse events is vital. Continuous monitoring throughout the trial ensures that patient safety in device trial design is upheld by promptly and effectively addressing any concerns regarding well-being. As highlighted in the case study on statistical techniques for stopping criteria, a careful balance is necessary when selecting stopping rules to minimize expected toxicities while maintaining statistical power.
- Engage in Continuous Post-Market Surveillance: Ongoing monitoring of device performance and security after market approval is essential for maintaining patient well-being. This practice not only protects patients but also provides valuable insights for future enhancements, aligning with bioaccess®'s dedication to comprehensive management services.
By adhering to these recommendations, organizations like bioaccess® can significantly enhance the security and effectiveness of medical studies. This proactive approach not only leads to improved patient outcomes but also ensures patient safety in device trial design, facilitating the successful commercialization of innovative medical devices and ultimately contributing to enhanced healthcare solutions. As Ram Mishra aptly questions, "Is this Time to Redefine the Clinical Evidence Pyramid?"—a reflection that underscores the need for evolving practices in clinical trial design to prioritize patient safety.
Conclusion
Patient safety remains the cornerstone of clinical trials, essential for maintaining trust and credibility in medical research. This article has thoroughly explored various strategies that organizations like bioaccess® implement to ensure participant safety, from robust informed consent processes to diligent monitoring of adverse events. Each phase of clinical trials, from initial design to post-market surveillance, emphasizes the necessity of prioritizing patient welfare through comprehensive risk assessments and ongoing oversight.
The commitment to patient safety is not merely a regulatory obligation; it is a moral imperative that enhances the integrity of clinical research and ultimately leads to improved healthcare outcomes. By adopting best practices such as rigorous monitoring, transparent communication, and continuous post-market evaluation, researchers can significantly mitigate risks and safeguard participants throughout the trial process.
As the landscape of medical innovation evolves, so too must the methodologies that underpin clinical trials. Organizations like bioaccess® exemplify how a proactive approach to patient safety can facilitate the successful development of groundbreaking medical devices. The insights and recommendations outlined in this article serve as a critical reminder that prioritizing patient safety is not just beneficial for participants but also vital for the advancement of healthcare solutions that can transform lives.
Frequently Asked Questions
What is the primary focus of patient protection in clinical studies?
Patient protection serves as the cornerstone of clinical studies, ensuring the rights, security, and well-being of participants throughout the research process.
How does patient protection impact research credibility?
A strong commitment to patient protection cultivates trust among participants and significantly enhances the credibility of research findings.
Why are effective patient protection measures important in device trials?
They are essential for maintaining patient safety, preventing adverse events, and ensuring that trials are conducted ethically and responsibly.
What role does continuous monitoring play in patient protection?
Continuous monitoring helps mitigate risks associated with new medical devices, leading to improved patient outcomes and facilitating regulatory approval.
What recent trend has been observed regarding serious events in clinical studies?
In 2023, there was an increase in reports related to serious events and high-harm incidents, highlighting the need for high-quality reporting and patient protection practices.
What is the significance of fostering a culture that promotes error reporting?
It is essential for improving patient well-being and addressing factors like fatigue during shift work, which can increase error rates.
What types of studies does bioaccess® oversee?
Bioaccess® oversees various studies, including Early-Feasibility Studies (EFS), First-In-Human Studies (FIH), Pilot Studies, Pivotal Studies, and Post-Market Follow-Up Studies (PMCF).
Can you provide an example of a significant case study in patient protection?
The BMT CTN 0601 investigation evaluated the effectiveness and protection of bone marrow transplants for children with severe sickle cell disease, utilizing monitoring protocols to track adverse outcomes.
What is the Gs method, and why is it important?
The Gs method is recognized for its capability to detect toxicity rates, emphasizing the importance of employing effective statistical techniques in study design.
How do regulatory frameworks impact clinical research?
Regulatory frameworks ensure that patient safety in device trial design is upheld alongside ethical standards, governing aspects like participant recruitment and informed consent.
What role do agencies like the FDA and EMA play in clinical studies?
They provide comprehensive guidelines that govern various aspects of research, including participant welfare and adverse event reporting.
How does bioaccess® assist researchers with regulatory compliance?
Bioaccess® offers services that include feasibility and selection of research locations, investigator selection, and ensuring that all documents meet country-specific requirements.
What special considerations are necessary for vulnerable populations in clinical research?
Ethical responsibilities must prioritize the rights and welfare of participants, particularly for children, pregnant women, and individuals with impaired decision-making capacity.
What should participants be informed about regarding study termination?
Participants should be informed about the reasons for study termination and any implications for their involvement in future studies.
Why is it important to stay informed about regulatory updates?
Staying informed about the latest updates and requirements is crucial for successful study design and ensuring compliance with established regulatory frameworks.

