Introduction
Serious Adverse Events (SAEs) play a crucial role in assessing the safety and efficacy of new medical interventions. These severe medical occurrences, such as those observed in clinical trials for COVID-19 vaccines, can have life-threatening consequences. SAEs are meticulously tracked during clinical trials, following rigorous surveillance protocols to ensure patient safety.
The accurate reporting of SAEs is essential for healthcare professionals and researchers to make informed treatment decisions and contribute to the integrity of drug development. This article explores the definition and criteria for identifying SAEs, provides examples of SAE outcomes, discusses reporting and documentation requirements, highlights investigator responsibilities, addresses special considerations for reporting, offers insights into operationalizing the SAE process, and presents tools and resources for managing SAEs. Additionally, international regulations and guidelines for SAE reporting are examined, and best practices for handling SAEs in clinical trials are discussed.
By adhering to these guidelines and standards, the medical community can prioritize patient safety and contribute to the advancement of scientific knowledge.
Definition of Serious Adverse Events
Serious Adverse Events (SAEs), which are pivotal in assessing the safety and efficacy of new medical interventions, encapsulate severe medical occurrences that could lead to death, pose immediate risk to a person's life, necessitate hospital admission or extended stay, result in substantial disability, or in the case of prenatal exposure, cause birth defects. These events are meticulously tracked during clinical trials, such as those for COVID-19 vaccines by Pfizer and Moderna, which are placebo-controlled, phase III randomized studies—a gold standard approach in pharmaceutical testing. For instance, the Brighton Collaboration's work on identifying adverse events of special interest post-COVID vaccinations is a testament to the rigorous surveillance protocols in place.
Moreover, real-world data, as observed in Pfizer's trials, can provide additional insights beyond the controlled environment of clinical trials, influencing physician prescribing patterns and ultimately impacting patient care.
Recent regulatory developments by the FDA, such as the "Direct-to-Consumer Prescription Drug Advertisements" final rule, underscore the importance of conveying information about SAEs transparently, ensuring that major side effects are presented in a clear, neutral, and easily understandable manner in media advertisements. This is crucial as it arms patients and healthcare professionals with essential information, potentially influencing treatment decisions.
Additionally, case studies highlight the gravity of SAEs. For example, an imbalance in neonatal deaths linked to bronchiolitis following the Beyfortus clinical trials reveals the unpredictability and seriousness of Sales, emphasizing the need for continuous vigilance. The FDA's mandate on safeguarding public health extends to monitoring these events, further exemplifying the critical role of regulatory agencies in the oversight of drug safety.
Clinical and policy researchers like Gamertsfelder and Osipenko emphasize the personal sacrifices of trial participants, who endure invasive tests and side effects with the hope of contributing to medical advancements that may benefit future generations. Their experiences highlight the ethical considerations and the profound impact of participating in clinical research, reinforcing the significance of Sales in the broader context of drug development and patient safety.
Criteria for Identifying SAEs
The identification of Serious Adverse Events (SAEs) is paramount in clinical research to safeguard patient health and contribute to the integrity of the study at hand. The definition of an SAE includes, but is not limited to, death, inpatient hospitalization or prolongation of existing hospitalization, a significant disability/incapacity, and other substantial medical occurrences. These events must be reported in a timely and accurate manner to maintain the quality and validity of the research.
The recommendations for SAE criteria focus on three pillars: quality and validity, transparency, and clear interpretation of the data. As stated by John Scanlon, PhD, this strategy not only strengthens individual research efforts but also empowers the broader community to assess the collective findings effectively. The ultimate goal is to establish good scientific practices that are accessible even to stakeholders outside the immediate field of expertise.
A critical issue in current research practices is the delay or failure in registering studies and reporting findings comprehensively, with discrepancies often found between study registrations and published reports. This selective reporting skews the data in favor of positive outcomes, undermining the authenticity and reliability of the research. To combat this, practical measures have been proposed to enhance reporting standards and transparency.
The importance of accurate SAE reporting is further underscored by the public nature of such information. Comments and data submitted to regulatory bodies like the Food and Drug Administration are made accessible to the public, emphasizing the responsibility of researchers to exclude confidential information from their reports. As the safety of medical interventions, including vaccines, falls under intense scrutiny, systems like the Vaccine Adverse Event Reporting System (VAERS) have proven instrumental in monitoring vaccine safety and debunking common myths surrounding it.
In summary, the definition and reporting of SAEs are critical components of clinical research that require clear guidelines and transparency to ensure the safety and efficacy of medical interventions. Stakeholders across the spectrum, from health professionals to researchers, contribute to a system that prioritizes public health and the integrity of scientific inquiry.
Examples of SAE Outcomes
Serious Adverse Events (SAEs) in clinical research are critical incidents that demand comprehensive scrutiny. These events can range from intense allergic reactions and organ dysfunction to grave complications from medical procedures and unexpected reactions to treatments. Sales underscore the gravity of safety monitoring within clinical trials.
For instance, a patient treated with lecanemab for Alzheimer's disease experienced debilitating headaches post-infusion, eventually leading to cognitive decline, illustrating the intricate nature of SAE responses. Moreover, NSAIDs, widely used for their anti-inflammatory properties, have been associated with hypersensitivity reactions, highlighting the need for vigilant SAE monitoring. Despite rigorous safety systems like the Vaccine Adverse Event Reporting System (VAERS) bolstering vaccine safety, the intricacies of Sales remain a concern, as evidenced by the delayed FDA approval of a needle-free treatment for severe allergic reactions by RS Pharma.
These examples emphasize the imperative of meticulous investigation and transparent reporting of sales to ensure patient safety and uphold the integrity of clinical research.
Reporting and Documentation Requirements for SAEs
The meticulous documentation and reporting of Serious Adverse Events (SAEs) form a foundational aspect of clinical research that cannot be overstated. It is imperative for researchers and study personnel to rigorously adhere to established guidelines and protocols. This ensures all Sales are meticulously captured and conveyed to pertinent regulatory authorities, including the FDA, and ethics committees.
The process must encapsulate a comprehensive account of the event, encapsulating the intensity, temporal span, and any correlations with the investigational product, in a uniform and standardized approach.
The FDA recently underscored the importance of clear communication in patient safety with the publication of the "Direct-to-Consumer Prescription Drug Advertisements" rule. This rule mandates that drug advertisements convey major side effects and contraindications in an understandable and neutral manner, employing consumer-friendly language and ensuring that audio and textual information are synchronized in television ads.
Additionally, the FDA's Adverse Events Reporting System (FAERS) and the MedWatch program invite healthcare professionals, patients, and the public to contribute to the safety monitoring of drugs and biological products. These platforms reinforce the notion that individual adverse event reports are invaluable for updating safety information post-approval.
When disseminating research findings, the authorship should reflect those who have significantly contributed to the study's conception, design, data acquisition, analysis, or interpretation. As per the International Committee of Medical Journal Editors (ICMJE) guidelines, authorship should be reserved for those who will take public responsibility for part of the content, underscoring the integrity of clinical research.
In light of recent research showcasing demographic and regional disparities in adverse event reporting rates across the United States, it is clear that ensuring equitable and comprehensive reporting is crucial. For instance, a study identified variation in reporting rates influenced by sociodemographic factors, revealing a pressing need to address such disparities to enhance postmarketing surveillance efforts.
Ultimately, these stringent reporting requirements and collaborative efforts aim to safeguard public health by enabling more accurate tracking and assessment of medication safety, thereby contributing to the overarching goal of delivering safe and effective therapeutics to all members of society.
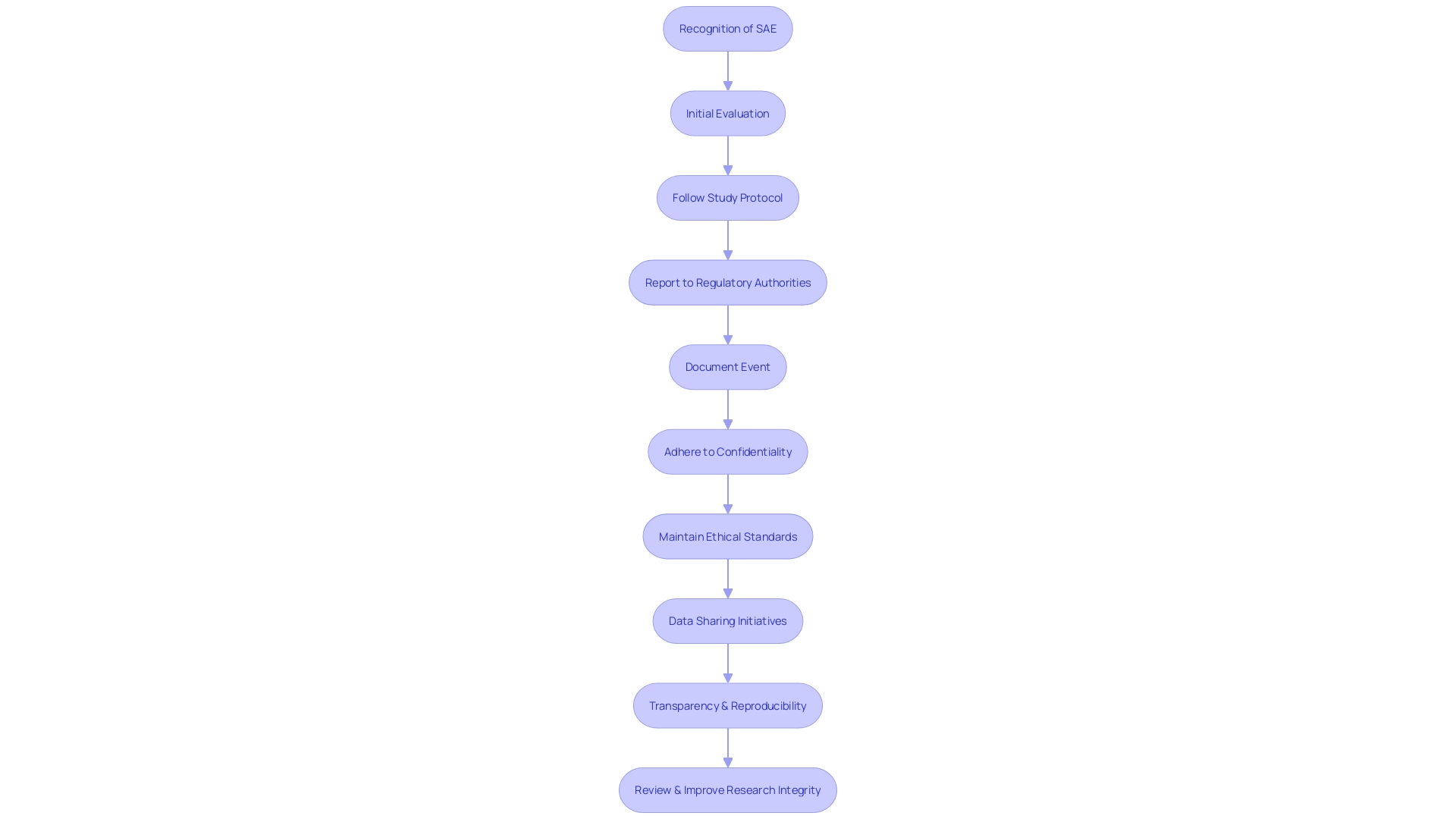
Investigator Responsibilities in SAE Reporting
In the meticulous realm of clinical research, the role of investigators is paramount, especially when it comes to the vigilant reporting of Serious Adverse Events (SAEs). These dedicated professionals bear the responsibility of promptly recognizing and evaluating any SAEs that may arise during a study. It is crucial for investigators to adhere strictly to the study protocol and regulatory demands, ensuring that every SAE is documented in a timely and accurate manner.
This adherence is not just a procedural formality; it's a safeguard for the integrity of the research and the well-being of participants.
In the context of confidentiality, investigators must navigate the dual mandate of transparent reporting and the protection of participant privacy. This delicate balance is akin to the protocols followed by the U.S. National Transportation Safety Board in investigations, where transparency is maintained within the limits of legal and ethical boundaries, as seen in Boeing's participation in the investigation of Alaska Airlines flight 1282.
Furthermore, the significance of maintaining confidentiality in research extends beyond the reporting of SAEs—it's a critical component of the entire clinical research process. This is exemplified by the situation faced by Dr. ABC, who encountered potential plagiarism while serving as a peer reviewer. The incident underscores the ethical imperative to safeguard confidentiality and the trust placed in the research community.
Investigators are also tasked with identifying events that deviate from good manufacturing practice, regulations, standards, or specifications that may impact the safety, purity, or potency of a biological product. This responsibility is demonstrated in the Vaccine Adverse Event Reporting System (VAERS), which is an integral part of the U.S. vaccine safety system, highlighting the system's success in identifying safety issues and dispelling myths.
Through rigorous reporting and a commitment to ethical standards, investigators play a vital role in preserving the sanctity of clinical research and the trust of those who rely on its findings.
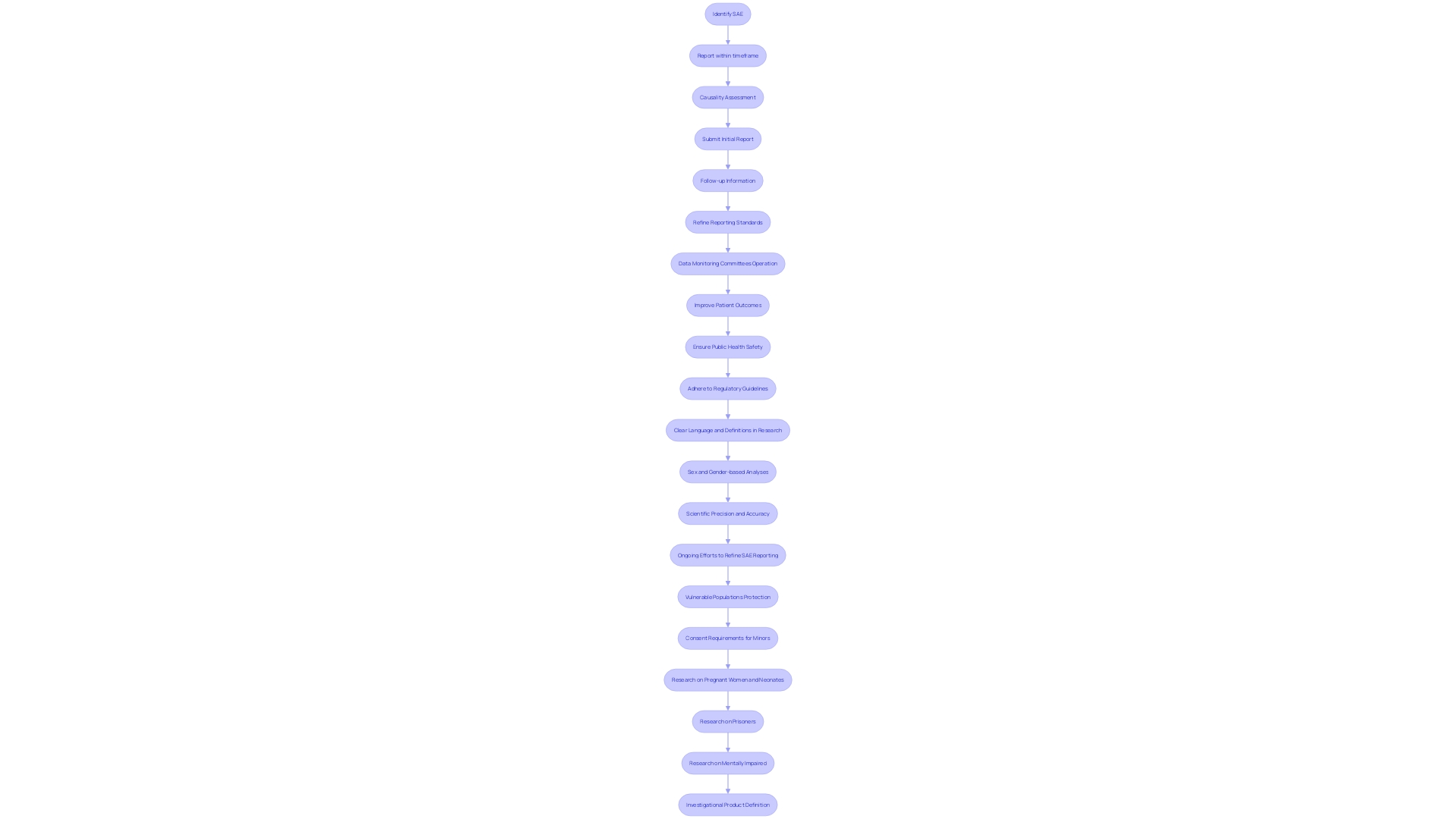
Special Considerations for SAE Reporting
Adherence to regulatory guidelines is a vital part of reporting serious adverse events (SAEs) in clinical research. The process involves a comprehensive understanding of the timeframe within which SAEs must be reported, a thorough causality assessment, and the provision of additional follow-up information. These guidelines are continually evolving to enhance scientific precision and accuracy.
As reflected in the updated directives on sex and gender-based analyses, the language and definitions used in research are critical for ensuring the equity, rigor, and reproducibility of scientific findings.
For instance, the recent expansion of guidelines across numerous journals has emphasized the importance of precision in the language of sex and gender, recognizing that the historical flexibility in these terms can lead to varied interpretations that may not align with current scientific understanding. These improvements in guideline accuracy not only advance the quality of research but also address the need for clear, consumer-friendly language as mandated by agencies like the FDA. This is particularly important when communicating SAEs, as clarity in reporting is crucial for the safety and security of public health.
Moreover, the draft guidance from the FDA on the establishment and operation of Data Monitoring Committees (DMCs) underscores the necessity for clear, thoughtful reporting practices in clinical trials. This guidance, although not yet finalized, is indicative of the ongoing efforts to refine SAE reporting standards to safeguard trial integrity and participant welfare.
In the realm of clinical research, the implications of accurate SAE reporting are significant. Studies indicate patients who partake in clinical trials support the sharing of their data to foster scientific advancement. This sentiment is echoed in the creation of research data management documents that outline how data will be collected, managed, and shared post-study, reinforcing the collective responsibility to contribute to the safety of medical products and the public at large.
Thus, it is imperative for all involved—manufacturers, healthcare professionals, researchers, and public health officials—to diligently comply with the specific SAE reporting guidelines set forth by regulatory authorities and ethics committees. Such compliance not only ensures the integrity of clinical data but also contributes to the overarching goal of improving patient outcomes and public health.
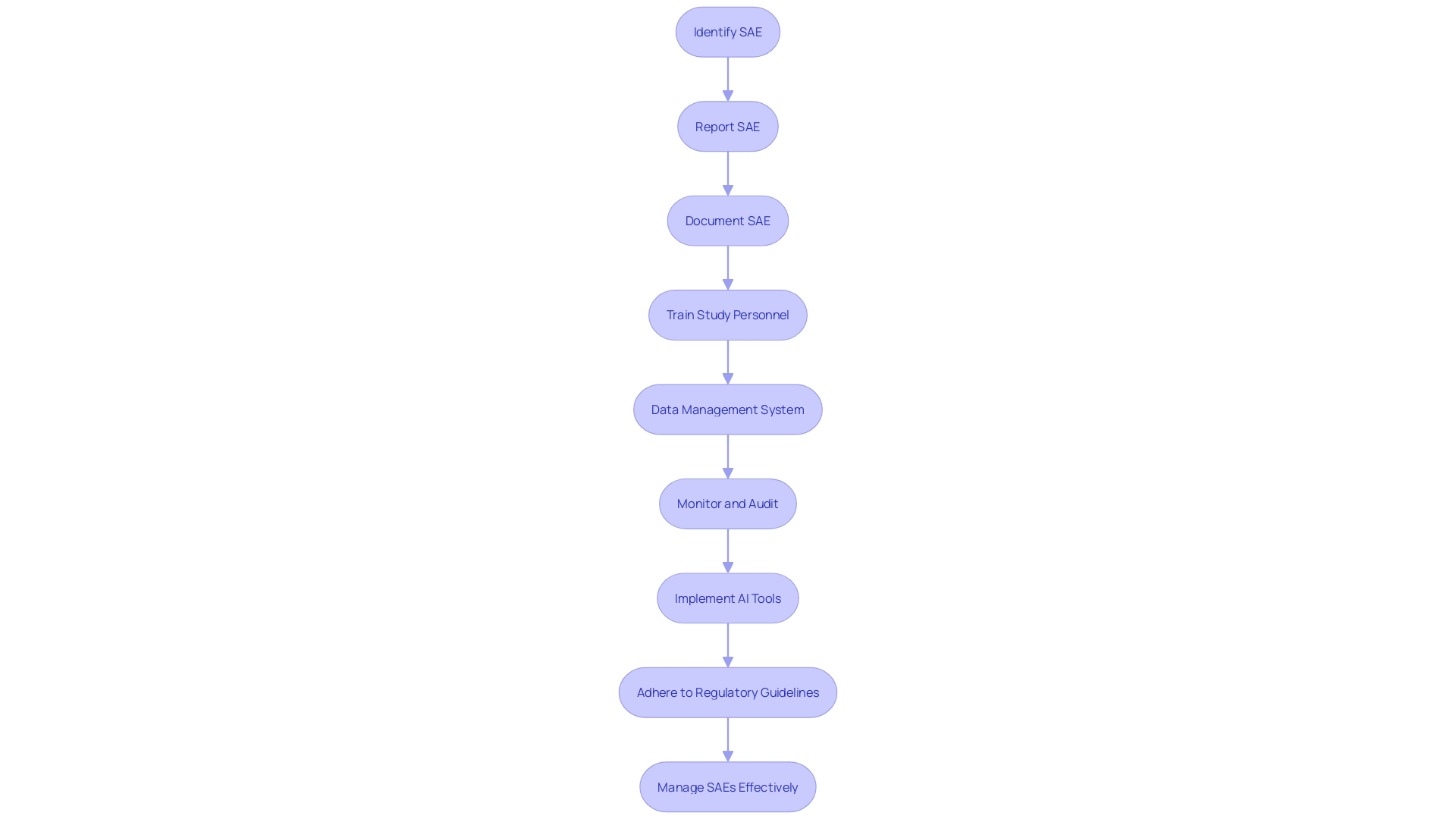
Operationalizing the SAE Process in Clinical Research
The management of Serious Adverse Events (SAEs) in clinical research is a critical component that requires meticulous planning and execution. To ensure the integrity of the clinical trial and the safety of participants, it is essential to have a well-defined workflow. This workflow should outline the steps for reporting and documenting Sales, emphasize comprehensive training for study personnel on the identification and reporting of these events, and highlight the importance of a robust data management system to capture and analyze SAE data effectively.
Moreover, regular monitoring and auditing of the SAE reporting process play a pivotal role in the early detection and resolution of potential issues. For instance, the strategic initiative to reduce inpatient mortality through an innovation competition showcases the necessity of integrating advanced tools, like AI, into the clinical workflow to enhance the monitoring and management of patient outcomes.
In line with the latest industry developments, such as Regeneron Pharmaceuticals' dialogue with the FDA on study definitions, it is evident that a harmonized approach to SAE management is beneficial. Adhering to consistent guidelines across different regulatory environments helps in maintaining the credibility and comparability of clinical trial data.
The essence of managing SAEs effectively lies in the ability to collect and manage data in a structured manner, thereby facilitating accurate analysis and reporting of results. As emphasized by the guidance on clinical trial data monitoring committees, establishing clear procedures and practices for trial monitoring is vital. This ensures that any SAEs are addressed promptly and appropriately, thereby safeguarding participant welfare and maintaining the integrity of the research study.
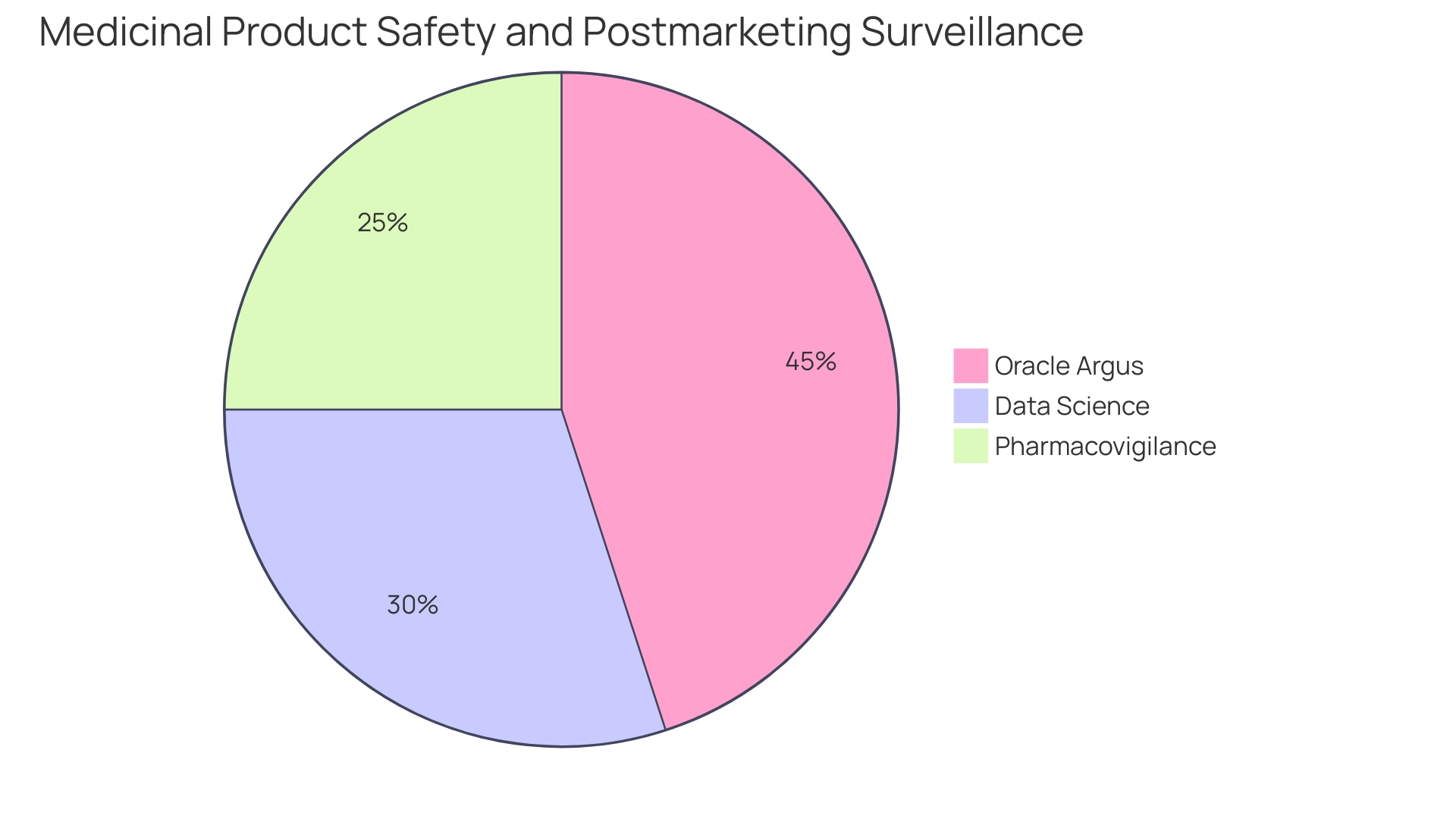
Tools and Resources for Managing SAEs
In the realm of clinical research, monitoring and managing Serious Adverse Events (SAEs) is paramount to safeguarding participant well-being and maintaining the integrity of study data. To support these efforts, a variety of tools and methodologies are employed, including advanced electronic data capture (EDC) systems. These EDC systems facilitate the swift and accurate recording of adverse event data, contributing to the enhancement of data quality and reinforcing adherence to reporting standards.
Alongside these systems are comprehensive adverse event reporting databases which serve as repositories for SAE data, enabling researchers to analyze trends and identify potential safety signals more effectively.
Standardized reporting forms, often devised in accordance with regulatory guidelines, help streamline the SAE documentation process, ensuring that reports are thorough and consistent. These forms often align with the principles of research integrity, which encompass honesty, accountability, professional courtesy, and good stewardship of research on behalf of others. Such principles are critical as they uphold the ethical conduct required in clinical research, despite the variability in disciplinary cultures and norms.
Moreover, regulatory authorities provide robust guidelines that aim to establish a harmonized approach to SAE reporting. This is crucial when considering the discrepancies observed in various definitions, such as the divergence between FDA's and EMA's interpretations of non-interventional studies. Regulatory guidance also extends to the planning and assessment of drug safety, emphasizing the importance of pre-defining key risks and tailoring trial designs to facilitate thorough safety assessments upon trial completion.
In the wake of public health emergencies, the FDA has adapted its guidelines to apply to a broader range of scenarios beyond the COVID-19 pandemic, addressing logistical and risk-based considerations in clinical trial monitoring. Such adaptive measures underscore the importance of an efficient and secure exchange of data across all levels of public health to prevent the spread of diseases and to support communities effectively.
To further the capabilities in SAE management, the Office of Science and Engineering Laboratories (OSEL) focuses on developing practical regulatory science tools that span the entire lifecycle of medical devices. These tools include lab methods and validation processes for AI models, which can significantly impact the evaluation of new and promising products, ensuring that life-saving interventions are thoroughly assessed and made available to the public in a timely manner.
In conclusion, the integration of EDC systems, standardized reporting, regulatory guidance, and the development of regulatory science tools form the bedrock of effective SAE management. These resources, underpinned by the overarching principles of research integrity and bolstered by advancements in data science and informatics, are essential for fostering a robust and responsive clinical research environment that prioritizes patient safety and the reliability of study outcomes.
International Regulations and Guidelines for SAE Reporting
Understanding the complexities of serious adverse event (SAE) reporting is pivotal in clinical research. Internationally recognized guidelines stipulate the timely submission of SAE reports, detailing essential information and identifying the appropriate regulatory bodies for submission. These stringent standards are in place to safeguard participants and maintain ethical integrity within medical studies.
Clinical trials, which assess the safety and efficacy of new treatments, are fundamental to advancing patient care. With trials ranging from small-scale phase one studies focused on safety to later stages assessing treatment efficacy, the meticulous documentation and disclosure of results are crucial. Yet, challenges persist, such as the underreporting of clinical trials, with a staggering 41% not registered before patient recruitment, and 68% either not reported or published, according to a decade-long study of Canadian trials.
This lack of reporting can lead to selective results that impact the evidence base for patient treatment. Moreover, the World Medical Association's Declaration of Helsinki emphasizes the necessity to register every clinical trial in a publicly accessible database prior to starting, and to publish all study outcomes to counter publication bias. Regulatory agencies such as the FDA underscore the importance of clear, understandable communication of drug information, including side effects, to the public.
This transparency is essential to maintain trust and informed decision-making among healthcare providers and patients alike. The adherence to these regulations and guidelines, including the accurate reporting of sex- and gender-based analysis, is not only a regulatory compliance matter but also a commitment to research equity and impact. Ultimately, the integrity of clinical research hinges on the consistent and thorough application of these SAE reporting requirements, ensuring that each study contributes valuable knowledge to the medical community and helps improve patient outcomes.
Best Practices for Handling SAEs in Clinical Trials
Managing Serious Adverse Events (SAEs) effectively in clinical trials is crucial to maintain the safety of participants and the credibility of the data. To accomplish this, it is essential to establish a robust framework for documentation, investigation, safety monitoring, and communication. Each SAE occurrence must be meticulously documented, reflecting a comprehensive and clear understanding of the event.
A thorough investigation into the causes and contributing factors is imperative, as it can provide insights into preventing future incidents. Proactive measures for safety monitoring should be a continuous process, anticipating potential Sales and mitigating risks early on. Additionally, fostering open communication among stakeholders, including sponsors, investigators, and ethics committees, is pivotal to the responsible management of Sales.
Collaboration and transparency not only support compliance with the latest guidelines, such as the European good clinical practice (GCP) guidance, but also reinforce the safeguarding of participant welfare and data integrity. The draft guidance by the International Council for Harmonization (ICH) E6 GCP (revision three) emphasizes the design of clinical trials to prioritize participant safety and data reliability, suggesting a focus on critical trial activities. By adhering to these best practices and recommended procedures, clinical trials can effectively address SAEs while ensuring the study's scientific objectives are met without compromise.
Conclusion
In conclusion, Serious Adverse Events (SAEs) are crucial in assessing the safety and efficacy of medical interventions. Accurate reporting is essential for informed treatment decisions and maintaining the integrity of drug development. International regulations stress transparent communication of SAE information to patients and healthcare professionals.
Examples of SAE outcomes highlight the need for continuous vigilance and thorough investigation. Reporting and documentation requirements ensure the quality and validity of clinical research. Investigators play a vital role in recognizing and evaluating SAEs while upholding research integrity.
Special considerations include precise language, harmonization of standards, and clear communication of SAEs. Operationalizing the SAE process requires well-defined workflows, comprehensive training, and robust data management systems.
Tools and resources, such as electronic data capture systems and standardized reporting forms, support effective SAE management. Adherence to regulatory guidelines and the development of regulatory science tools enhance reporting standards and prioritize patient safety.
International regulations and guidelines emphasize timely SAE reporting to safeguard participants and maintain ethical integrity. Best practices for handling SAEs include comprehensive documentation, thorough investigation, proactive safety monitoring, and open communication.
By adhering to these guidelines and best practices, the medical community can prioritize patient safety, contribute to scientific knowledge, and deliver safe and effective therapeutics to all.




