Introduction
Good Clinical Practice (GCP) is a globally recognized framework that sets ethical and scientific standards for conducting clinical trials involving human participants. It ensures the protection of trial subjects' rights, safety, and well-being while also ensuring the reliability and credibility of clinical trial data. Clinical trials play a pivotal role in advancing medical knowledge, and GCP ensures that these trials adhere to rigorous testing phases to establish the safety and efficacy of new interventions.
There is also a growing emphasis on sustainability within the healthcare sector, leading to the integration of digital technologies and innovative methodologies to enhance trial efficiency and minimize environmental impact. GCP is rooted in historical events and ethical principles, such as the Nuremberg Code, and is supported by regulatory frameworks and organizations like the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use. Adhering to GCP not only upholds the rights of trial participants but also ensures the generation of reliable data crucial for the development of innovative treatments and the continual advancement of healthcare.
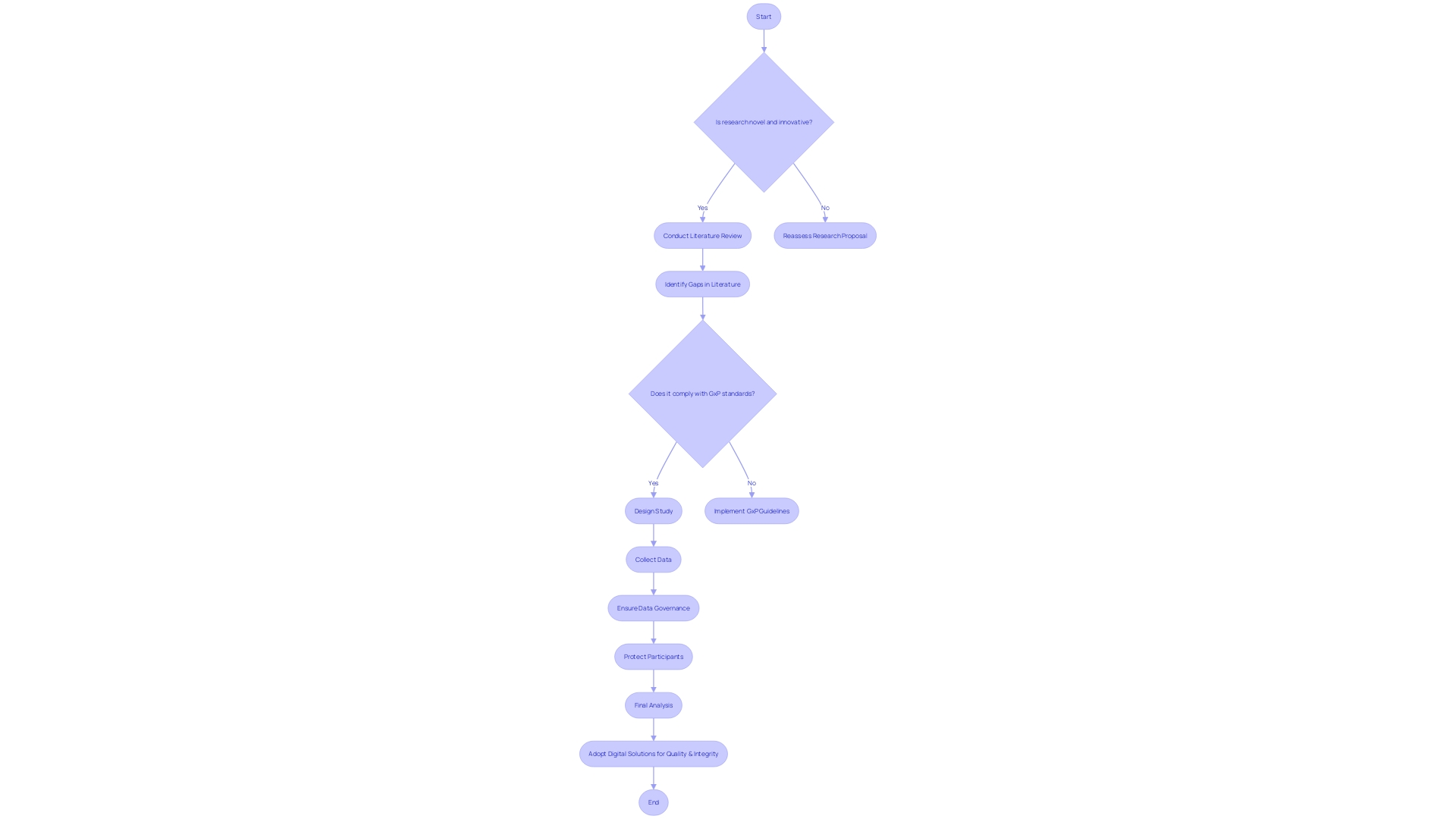
Challenges in implementing GCP include evolving regulatory landscapes and the integration of new technologies, but by embracing these challenges and leveraging advancements, clinical research can stay at the forefront of modern medicine.
Definition of Good Clinical Practice
Good Clinical Practice (GCP) is a globally recognized framework that outlines ethical and scientific standards for designing, conducting, recording, and reporting studies involving human participants. These standards ensure the rights, safety, and well-being of subjects are protected, while also providing assurance of the reliability and credibility of clinical data.
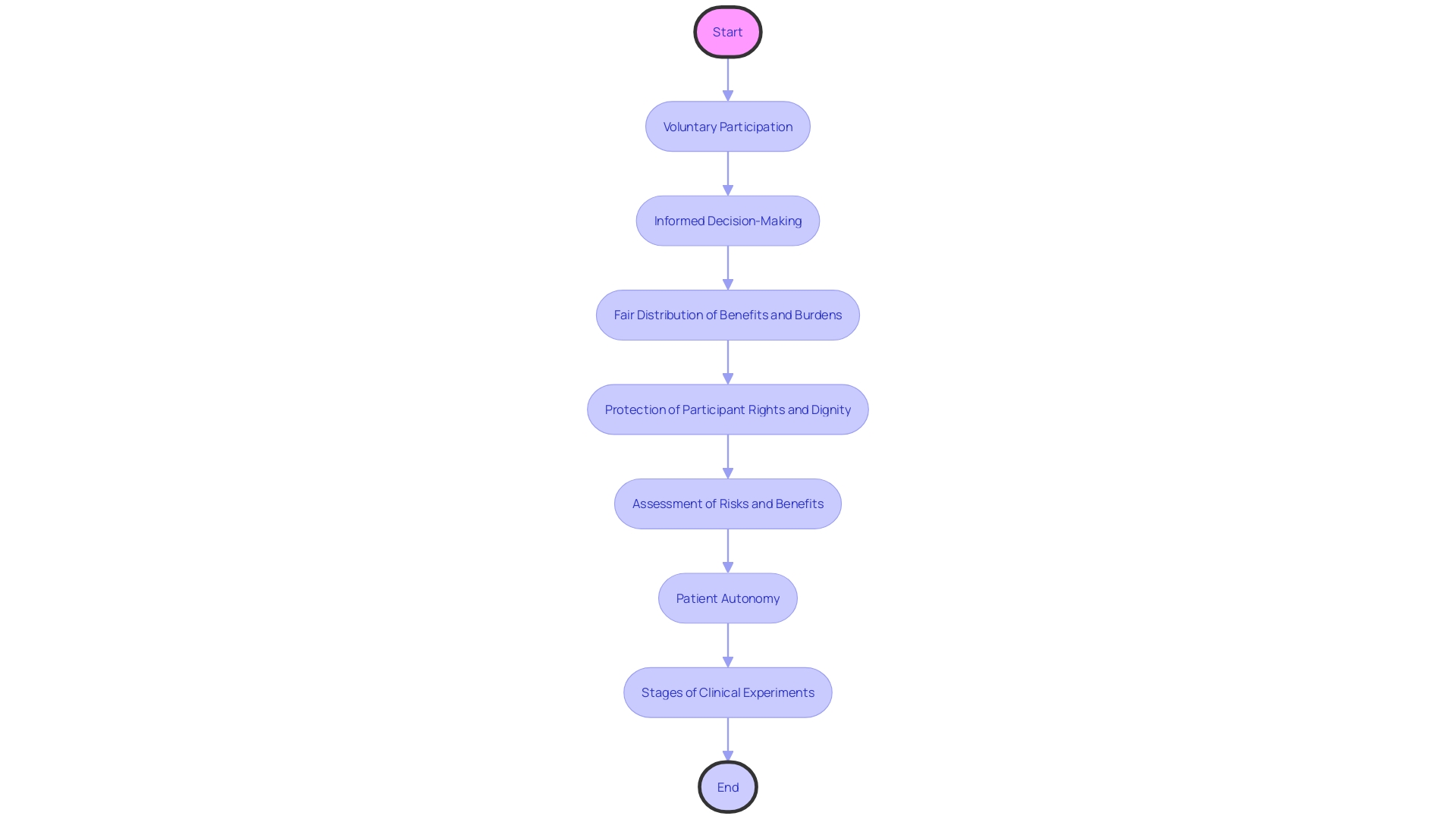
Clinical experiments, pivotal to medical advancements, consist of rigorous testing phases to establish the safety and efficacy of new interventions, such as drugs, devices, and behavioral therapies. In the first phase, a limited number of healthy participants are recruited to evaluate the safety of the treatment, whereas in the second phase, the scope is broadened to encompass patients, with the objective of assessing the efficacy of the treatment.
Drawing attention to the overlap of research in healthcare with wider societal issues, there is a growing focus on sustainability within the healthcare sector, which accounts for approximately 5% of global greenhouse gas emissions. In response, we're witnessing a merging of digital technologies and innovative methodologies to boost efficiency and reduce environmental impact. A significant undertaking is the implementation of a Carbon Emission Index in clinical experiments, serving as a crucial tool for teams to assess and enhance a study's carbon footprint.
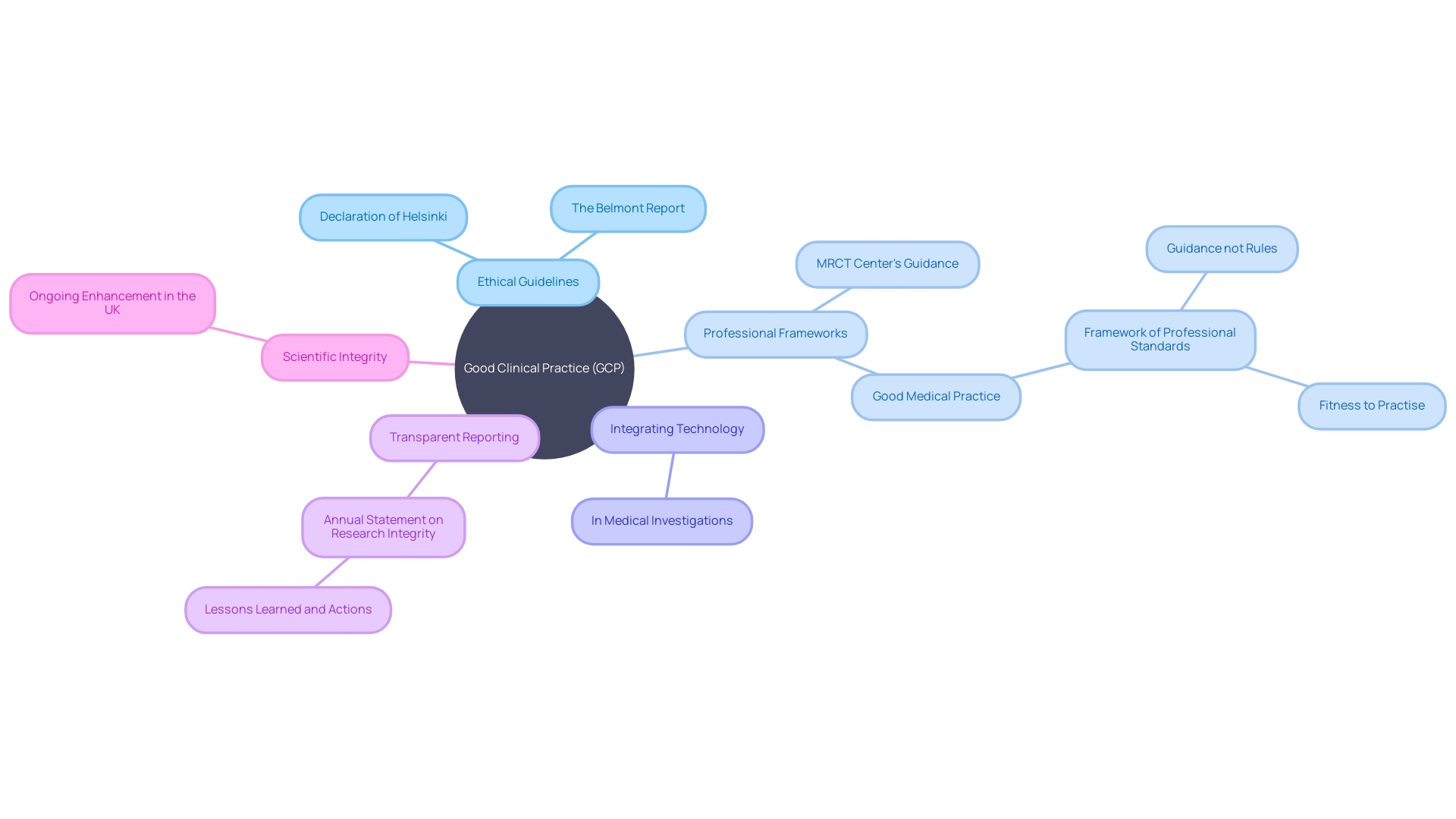
It's essential to acknowledge the evolving landscape of medical ethics over the years. Foundational texts like the Declaration of Helsinki and the Belmont Report have significantly shaped the ethical conduct of human studies, emphasizing informed consent and respect for participants. These principles are continually reassessed, most recently through guidance from the Multi-Regional Clinical Trials Center, ensuring they remain relevant in today's context.
Moreover, the standards of good medical practice are not static but adapt to feedback and changing circumstances. They guide healthcare professionals in exercising their judgment when caring for patients and collaborating with colleagues, underscoring the importance of personal responsibility and ethical conduct in the medical field.
The dedication to transparency in experiments and data sharing is also gaining momentum, despite variability among companies. The public availability of trial protocols, statistical analysis plans, and ultimately, raw data, is crucial for promoting transparency and reproducibility. While initiatives to enhance data sharing have been introduced, the adherence to these practices remains an area for improvement, highlighting the need for ongoing efforts to ensure scientific integrity and public trust.
Key Principles of Good Clinical Practice
Good Practice serves as the gold standard in research, ensuring the protection of human subjects and the integrity of data collected. The core of GCP lies in safeguarding participant rights, ensuring informed consent, and upholding confidentiality. These principles are not simply ethical guidelines but are crucial in validating the credibility of experiment results. For example, the recent expansion of the European GCP guidance with a dedicated section on data governance, as discussed by Silvia Perez at the Outsourcing in Trials Europe 2024 conference, underscores the evolving focus on meticulous evaluation of trial objectives against potential risks. The forthcoming guidance revision emphasizes critical activities necessary to preserve participant safety and data reliability, including the protection of participant data and the management of computer systems.
These updates resonate with the fundamental domains of Good Medical Practice, a framework that, while not prescriptive, mandates the use of professional judgment in adhering to standards. These standards, as highlighted in the feedback from the updated Good Medical Practice, relate to fitness to practice procedures and take into consideration factors such as the extent of deviation from norms, the intent behind actions, and the response to concerns raised, which align with the principles of GCP.
Moreover, the ethical backdrop of GCP is anchored in foundational documents such as the Declaration of Helsinki and The Belmont Report, which emphasize respect for individuals, beneficence, and justice. These documents have been crucial in shaping the ethical conduct of human investigation and continue to influence guidelines, such as the Multi-Regional Clinical Trials Center of Brigham and Women's Hospital and Harvard's Guidance, Toolkit, and Principles, which focus on the ethical return of individual data and results to participants.
Integrating technology in medical investigations has become essential. The National Health Service (NHS) has pioneered the use of technology in healthcare, as noted in The Times, and this extends to clinical trials. Technology enables direct patient care, enhances the efficiency of the NHS, and gathers data for future medical studies. As part of the digital-assurance process, the NHS ensures that new technologies meet rigorous standards of security, appropriateness, and compliance before adoption. This diligence is reflective of the principles of GCP, which demand rigorous assessment of new interventions to establish their safety and efficacy, ultimately influencing patient care.
Considering the importance of GCP, the data on integrity in the UK highlight the need for transparent reporting and ongoing enhancement. Yearly statements on scientific integrity, suggested by the Concordat to promote scientific integrity, demonstrate this dedication to maintaining moral principles in scientific inquiry. The iterative process of trials, from phase one to phase two, necessitates a framework that not only protects participants but also ensures that the outcomes of such trials are robust and actionable. The GCP guidelines offer this structure, allowing investigators to navigate the intricate terrain of medical studies with an ethical compass and a dedication to quality.
Importance of Good Clinical Practice
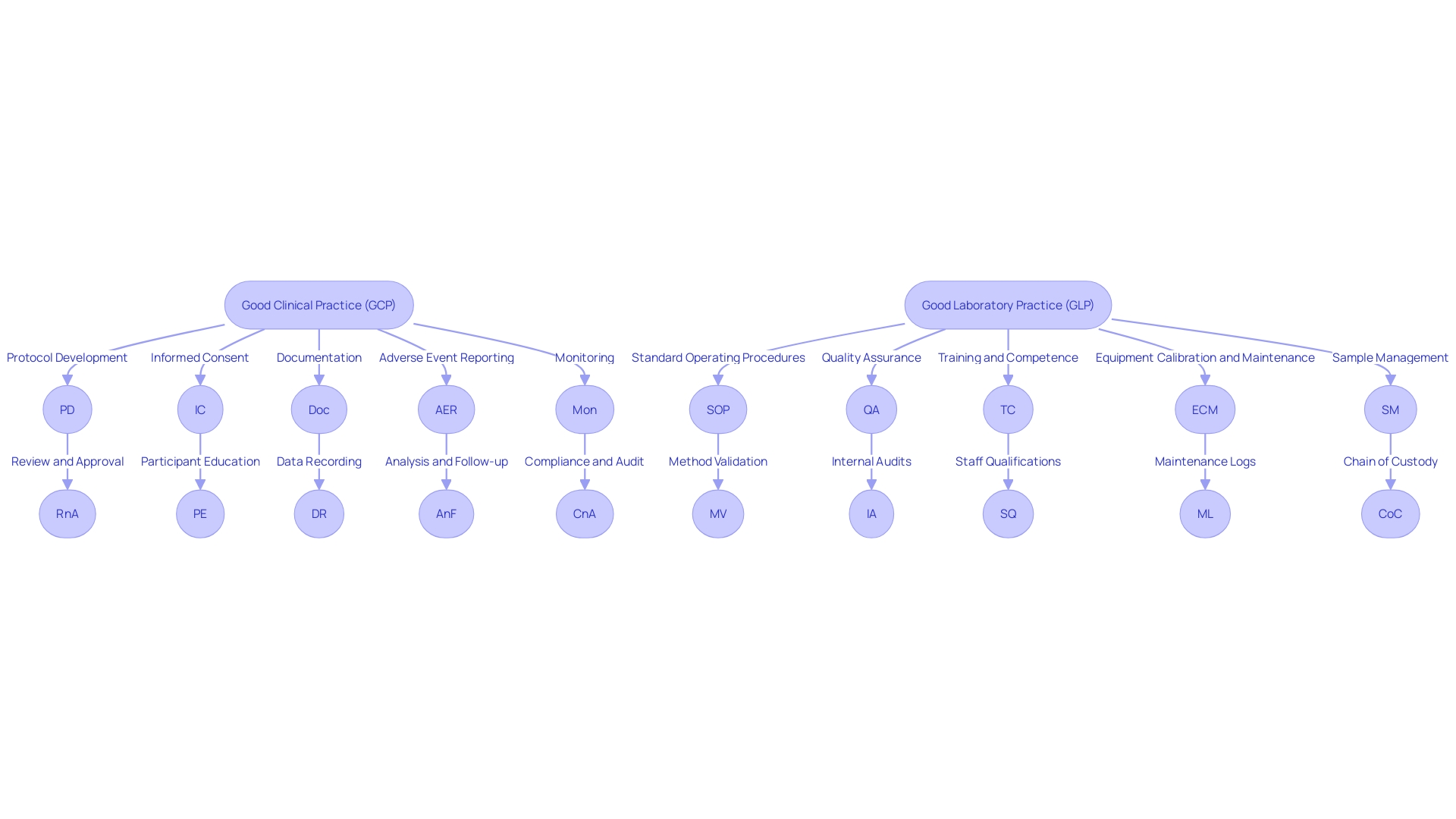
Effective Clinical Practice (GCP) and Effective Laboratory Practice (GLP) are vital elements in the realm of research, serving as the foundation for safeguarding the rights, safety, and welfare of research participants. By following these guidelines, researchers can guarantee the honesty and reliability of data collected during medical experiments. This, in turn, strengthens the trust placed by stakeholders and regulatory authorities in the study findings. For instance, the European GCP guidance has introduced a dedicated section on data governance, which underscores the importance of protecting participant data and managing computer systems effectively. These measures are crucial for preserving the integrity of the process, from randomization to the final analysis. As Silvia Perez, director of quality compliance for patient studies at AstraZeneca, emphasized during the Outsourcing in Clinical Studies (OCT) Europe 2024 conference, the revised guidelines highlight crucial aspects of study design and processes to reduce risk while ensuring patient safety and the achievement of goals.
Additionally, the concept of GxP encompasses various quality practices that life science organizations must comply with, such as Good Manufacturing Practice (GMP), which is essential for maintaining product safety and efficacy. These standards are not rigid rules but frameworks that guide professional conduct, allowing for informed judgment in specific circumstances. The adoption of such practices is evidenced by the rigorous digital-assurance processes implemented within the NHS, ensuring that any new technology meets high standards of security and compliance. This careful approach to adopting digital solutions reflects the overarching principles of GCP and GLP, which prioritize the quality and integrity of trials and the safety of all participants involved.
Ethical Foundations of Good Clinical Practice
Good Clinical Practice (GCP) is not just a set of rigid rules but a dynamic framework that integrates ethical principles such as respect for individuals, beneficence, and justice. These ethical underpinnings ensure voluntary participation and mandate that subjects are provided with sufficient information to make informed decisions. Moreover, GCP enshrines the fair distribution of both the benefits and burdens of research, safeguarding the rights and dignity of participants. At its core, GCP is about protecting the welfare of human subjects and ensuring integrity in the collection of medical data.
Central to GCP is the principle of non-maleficence, encapsulated by the Latin phrase "primum non nocere"—"first, do no harm." This principle is crucial in assessing the risks and benefits of clinical procedures, ensuring they are conducted by qualified professionals. Additionally, patient autonomy is paramount; patients must have the final say in their healthcare choices. This requires healthcare professionals to furnish all pertinent information regarding risks, benefits, and alternatives to empower patients to make informed decisions about their care.
Clinical experiments, which are at the core of GCP, go through rigorous stages to establish safety and efficacy before treatments reach patients. Commencing with a small group of healthy volunteers in Phase one to evaluate safety, and advancing through larger, more diverse participant groups in Phase two and beyond, these studies are crucial in advancing medical understanding and enhancing patient outcomes. The updated 'Good medical practice' standards reflect this commitment to ethical conduct and patient-centric care, ensuring that the evaluation of a medical professional's conduct takes into account their judgment, intent, and the context of their actions.
Historical Background of Good Clinical Practice
The origin of Good Clinical Practice (GCP) is deeply rooted in ethical principles that emerged from historical events, notably the establishment of the Nuremberg Code post-World War II, which laid down fundamental ethical guidelines for human experimentation. These foundational principles have been shaped over time into a robust set of guidelines, as medical research grew in complexity and necessitated standardized practices. GCP has become a cornerstone for ensuring that the rights, safety, and well-being of trial subjects are protected, and that the trial data generated is credible.
The concept of Good Medical Practice (GMP) complements GCP by providing a framework of professional standards that guide medical practice and decision-making in various circumstances. While GMP sets forth standards of good practice, it is not prescriptive; rather, it expects individuals to apply these standards with sound judgment tailored to the specific context they encounter. The updated GMP framework also clarifies how these standards relate to fitness to practice procedures, ensuring that concerns raised are assessed with a view to the individual circumstances, including factors such as the extent of deviation from standards, the nature of the behavior, and the context within the healthcare environment.
In a similar vein, the principles of Evidence-Based Practice (EBP) are integral to the implementation of GCP, ensuring that the latest scientific evidence, expertise in healthcare, and patient preferences are incorporated into care. This process of review, analysis, and translation of scientific evidence into practice helps in making informed decisions for patient care.
The development of GCP demonstrates a continuous global cooperative endeavor, with regulatory measures shaping it into the comprehensive structure that governs today's clinical studies. This framework is not only a testament to our scientific advancement but also a tribute to the dignity of those who were part of historical research under unethical conditions, as we continue to uphold the integrity of medical research and practice.
Goals of Good Clinical Practice
Good Clinical Practice (GCP) is an international ethical and scientific quality standard for designing, conducting, recording, and reporting studies that involve the participation of human subjects. Adherence to these standards ensures public confidence that the rights, safety, and well-being of study participants are safeguarded, in line with the principles that stem from the Declaration of Helsinki, and that the data from the research study are reliable.
The FDA highlights the significance of GCP in protecting human subjects involved in studies, while also ensuring data integrity and the effectiveness of new medical interventions. Similarly, the European GCP guidance, particularly with its recent updates, underscores the necessity of meticulous data governance and risk assessment in clinical trials, focusing on activities critical to trial objectives.
Embracing Good Laboratory Practice (GLP) alongside GCP, institutions and regulatory bodies strive to maintain a high standard of practice that is not rigidly rule-based but allows for professional judgment in response to varying circumstances. This versatile approach ensures that individual case factors, such as the degree of a professional's deviation from standards and the context of their working environment, are duly considered, reflecting a commitment to the ethical conduct of investigation.
In essence, GCP and GLP are not only about adhering to rules; they signify a dedication to moral investigation and high-quality knowledge, guaranteeing that the welfare of the patient is always the top priority, and that the outcomes of experimental studies are strong and trustworthy.
Components of Good Clinical Practice
'Good Clinical Practice (GCP) and Good Laboratory Practice (GLP) are crucial frameworks that guarantee the quality, safety, and integrity of medical investigations and laboratory procedures.'. These practices are guided by a set of components crucial for the conduct of trials and laboratory work. They encompass the development of rigorous protocols, securing informed consent, meticulous documentation, reporting adverse events, and continuous monitoring.
The protocol development is the cornerstone of clinical investigation, defining the objectives, design, methodology, statistical considerations, and organization of a study. It ensures that the study is scientifically sound and that it respects the rights and welfare of the participants. For instance, in a multi-faceted diabetes care project, the protocol outlined a convergent parallel design across five interconnected studies, focusing on patient experiences and outcomes, further supporting the replication of the study for other chronic diseases.
Informed consent is a pivotal process that empowers participants with the knowledge and understanding necessary to make an educated decision about their involvement in a study. The consent process must present essential information in a clear and concise manner, as highlighted by the positive experiences reported in the Kidney Precision Medicine Project, where participants' understanding of the informed consent process was notably high due to their altruistic motivations.
Documenting every aspect of the study is vital for maintaining transparency and accountability. The recent emphasis on data governance in the European GCP guidelines underscores the importance of protecting participant data and ensuring the reliability of research results. With the upcoming implementation of the revised guidelines, there is a focus on designing experiments that prioritize participant safety, the evaluation of scientific objectives, and the mitigation of risks.
Adverse event reporting is a crucial element that guarantees participant safety by monitoring and assessing any negative outcomes linked to the study. This enables researchers to take timely action to address any potential risks to participants.
Monitoring, both internal and external, is integral to ensuring that the study is conducted in accordance with the established protocol and GCP guidelines. The implementation of decentralized experiments (DCTs) has emphasized the requirement for strong monitoring techniques, as these experiments often involve remote areas and virtual interactions.
Collectively, these elements of GCP and GLP constitute a comprehensive range of practices that are essential to the ethical conduct of medical research, protecting both the participants and the integrity of the data collected.
Regulatory Frameworks Supporting Good Clinical Practice
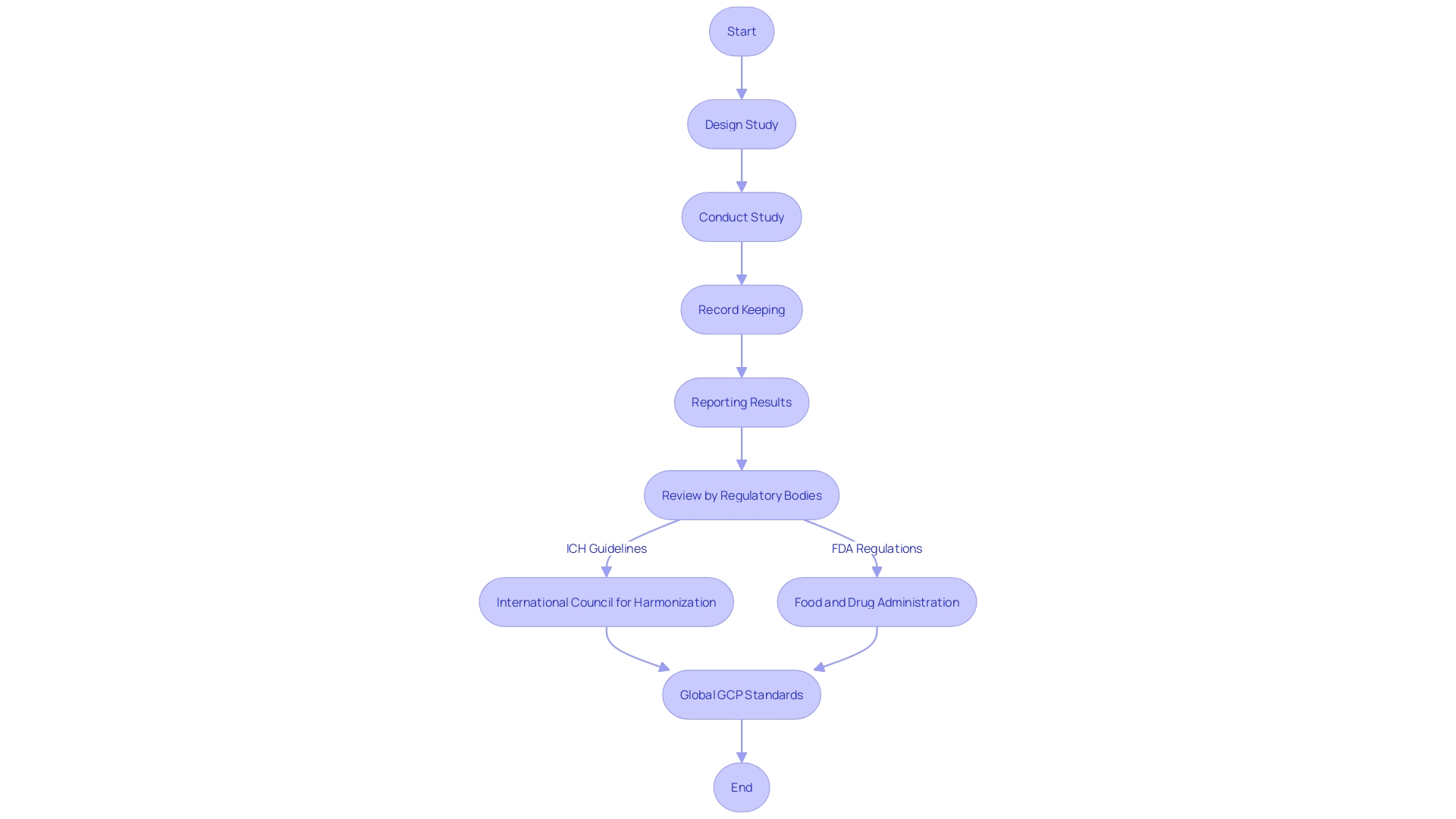
Good Clinical Practice (GCP) is a collection of globally acknowledged ethical and scientific quality standards that are crucial in guaranteeing the safeguarding of participants' rights, safety, and well-being in medical experiments. The main objective of GCP is to ensure that data from experiments is both reliable and credible. To accomplish this, GCP guidelines cover different aspects of the study process including design, conduct, record-keeping, and reporting.
The International Council for Harmonization of Technical Requirements for Pharmaceuticals for Human Use (ICH) alongside regulatory bodies such as the Food and Drug Administration (FDA) have laid down comprehensive frameworks to uphold GCP. These frameworks are designed to be universally applicable, ensuring consistency and integrity in the conduct of medical experiments globally, regardless of location.
Furthermore, the most recent revisions to the European GCP guidance have implemented a specialized section on data governance, showcasing the changing environment of clinical study oversight. This revision emphasizes the importance of carefully evaluating scientific objectives and associated risks, with a focus on critical activities necessary for achieving objectives.
In the broader context of product quality and safety, GCP is part of the 'GxP' family of regulations, which includes Good Manufacturing Practice (GMP). GMP guidelines focus on preventing errors in the manufacturing process, which can have drastic consequences for patient health. In the same way, GCP guarantees that the evaluations that establish the effectiveness and safety of those produced items are equally thorough and free of mistakes.
Understanding the implications of GCP and related practices like GMP is more than a regulatory requirement; it's a commitment to patient safety and the integrity of medical research. These guidelines serve as a foundation for the trust placed in healthcare products and treatments by patients, healthcare providers, and the public at large.
Implementation and Enforcement of Good Clinical Practice
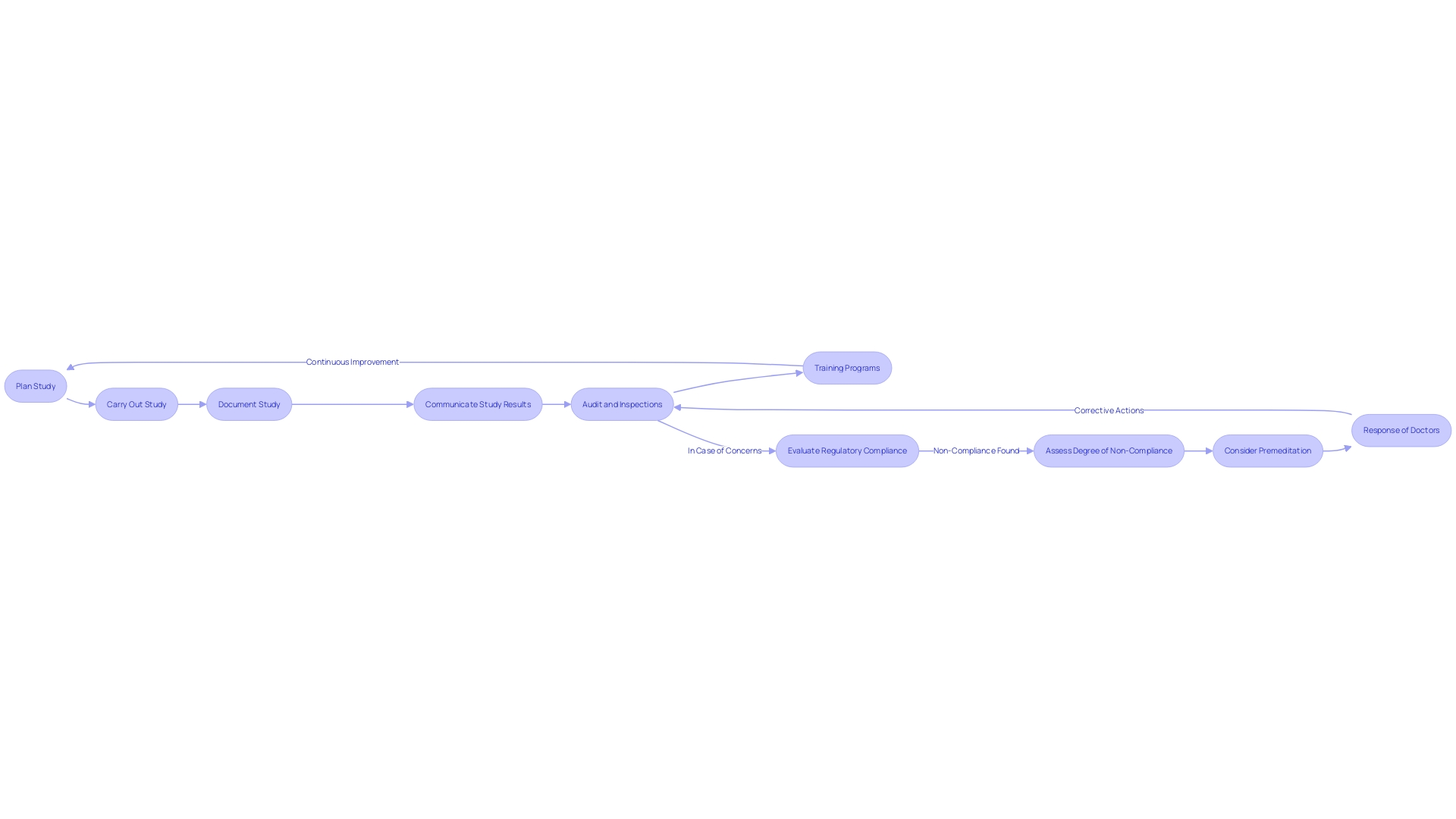
To uphold the utmost standards of practice, organizations must comply with Good Clinical Practice (GCP), a set of ethical and scientific quality standards for planning, carrying out, documenting, and communicating studies that involve human subjects. Compliance with GCP ensures the rights, integrity, and confidentiality of trial participants are protected, while also ensuring that clinical trial data is credible. GCP guidelines are not rigid rules, but rather principles that require careful application and judgment based on the specific circumstances of a study.
Regular audits, inspections, and training programs are fundamental components in upholding GCP. These measures help to identify and rectify any deviations from the established standards, ensuring ongoing compliance. The importance of GCP adherence is emphasized by the fact that if concerns arise, regulatory authorities evaluate each case in its unique context, considering factors such as the degree of non-compliance, the premeditation of the behavior, and the doctor's response to the concern, including evidence of insight into their actions.
In addition to GCP, Good Laboratory Practice (GLP) is another critical set of regulations that ensure the consistency, reliability, safety, and auditability of non-clinical laboratory studies. These practices are designed to protect the quality of the study while establishing a foundation for the mutual acceptance of test data.
For instance, the adoption of new digital technologies within the healthcare sector, such as in the NHS, requires a rigorous process to ensure these solutions meet GCP and GLP standards. This process includes initial assessments to determine if the technology is secure, appropriate, and in line with necessary approvals, highlighting the comprehensive nature of GxP regulations.
In the end, GCP and GLP are not only about compliance; they embody a dedication to ethical investigation and scientific integrity, which is essential for advancing medical knowledge and enhancing patient outcomes. As professionals operate within these guidelines, they contribute to a culture of excellence in the field of medical investigation that benefits all stakeholders, including sponsors, investigators, ethics committees, and, most importantly, patients.
Benefits of Adhering to Good Clinical Practice
The implementation of Good Clinical Practice (GCP) is crucial in guaranteeing the integrity and credibility of data from research, which contributes to securing regulatory approvals and advancing medical science. For instance, the Medicines and Healthcare products Regulatory Agency (MHRA) requires that medical products must be demonstrated to be effective and safe, highlighting the importance of strong clinical testing. AstraZeneca, a leading biopharmaceutical company, adheres to these practices, underscoring the importance of GxP regulations that encompass a range of quality practices including Good Manufacturing Practice (GMP) to prevent errors in manufacturing that could affect patient health.
Upcoming updates to the European GCP guidelines, particularly concerning data governance, highlight this commitment to safeguarding patient rights and well-being. The expected modifications, as described by Silvia Perez at Arena International's Outsourcing in Clinical Trials Europe 2024 conference, are intended to guarantee that experiments are conducted with an emphasis on patient safety and dependable outcomes. The guidelines recommend evaluating scientific objectives and associated risks, emphasizing the protection of patient data and the integrity of experimentation processes.
Clinical experiments, which are the foundation of medical research, are conducted in stages to evaluate the safety and effectiveness of new treatments. For example, phase one tests the safety of a treatment with healthy volunteers, while phase two expands to include affected individuals to evaluate both effectiveness and safety.
The significance of GCP compliance is further demonstrated by the scrutiny of evidence influencing decision-making frameworks, such as those of the UK's National Institute for Health and Care Excellence (NICE). Research conducted by Consilium Scientific revealed that the quality of medical data often falls short, emphasizing the necessity of conducting medical trials with rigor and transparency to ensure that treatments deliver genuine benefits to patients.
In summary, following GCP not only upholds the safety and rights of study participants but also ensures the generation of reliable, accurate data crucial for the development of innovative treatments and the continual advancement of healthcare.
Challenges and Future Directions in Good Clinical Practice
Good Clinical Practice (GCP) remains a fundamental aspect of medical investigations, guaranteeing the integrity of data and the safeguarding of patient rights. However, challenges persist, such as intricate study designs and evolving regulatory landscapes that necessitate the integration of new technologies. For instance, the NHS has experienced challenges with technology requests, finding that requested solutions were often already available within the trust, unknown to the requestors. This underlines the importance of thorough assessments by digital service teams to ensure security, appropriateness, and compliance.
The advancements in electronic medical records in Rwanda, supported by the ICT Sector Strategic Plan, showcase how digital platforms can enhance healthcare delivery. This successful implementation demonstrates the potential for technology to improve data quality and patient care. Similarly, the digital health interventions for ADHD in young people highlight the critical role of access to primary care and digital resources in healthcare practice.
Furthermore, the updated Good medical practice framework emphasizes the application of professional standards with judgment, reflecting on individual circumstances, and the extent of deviation from expectations. Such considerations are vital when addressing concerns about fitness to practice.
To address these challenges and build on GCP's future, it is imperative to leverage technological advancements, uphold data quality and integrity, and foster international collaborations. By doing so, we can enhance the efficiency and effectiveness of clinical research, ensuring that it keeps pace with the demands of modern medicine and patient care needs.
Conclusion
In conclusion, Good Clinical Practice (GCP) is a globally recognized framework that sets ethical and scientific standards for clinical trials. It ensures participant rights, safety, and credible data. GCP aligns with sustainability efforts and integrates digital technologies.
Adhering to GCP is crucial for maintaining trial integrity and generating reliable data. It is supported by regulatory bodies like the FDA and ICH. GCP benefits include regulatory approvals, advancing medical science, and patient safety.
Challenges exist, but embracing advancements and collaborations can shape the future of GCP. GCP plays a pivotal role in ethical trials, protecting participants, and improving patient outcomes.




