Introduction
Navigating the complex landscape of medical device trials requires a comprehensive understanding of the regulatory frameworks that govern these critical studies. As the industry evolves, adherence to guidelines set forth by key regulatory bodies such as the FDA and EMA becomes paramount for ensuring compliance and facilitating successful trials. This article delves into the essential components of conducting medical device trials, from the intricacies of regulatory compliance and cost-reduction strategies to the integration of advanced technologies and robust data management practices.
Furthermore, it emphasizes the importance of post-trial evaluations and market strategies that not only enhance the effectiveness of medical devices but also prioritize patient safety and well-being. Through a detailed exploration of these facets, a clearer picture emerges of how to optimize clinical trials in a way that meets both regulatory demands and the needs of the healthcare market.
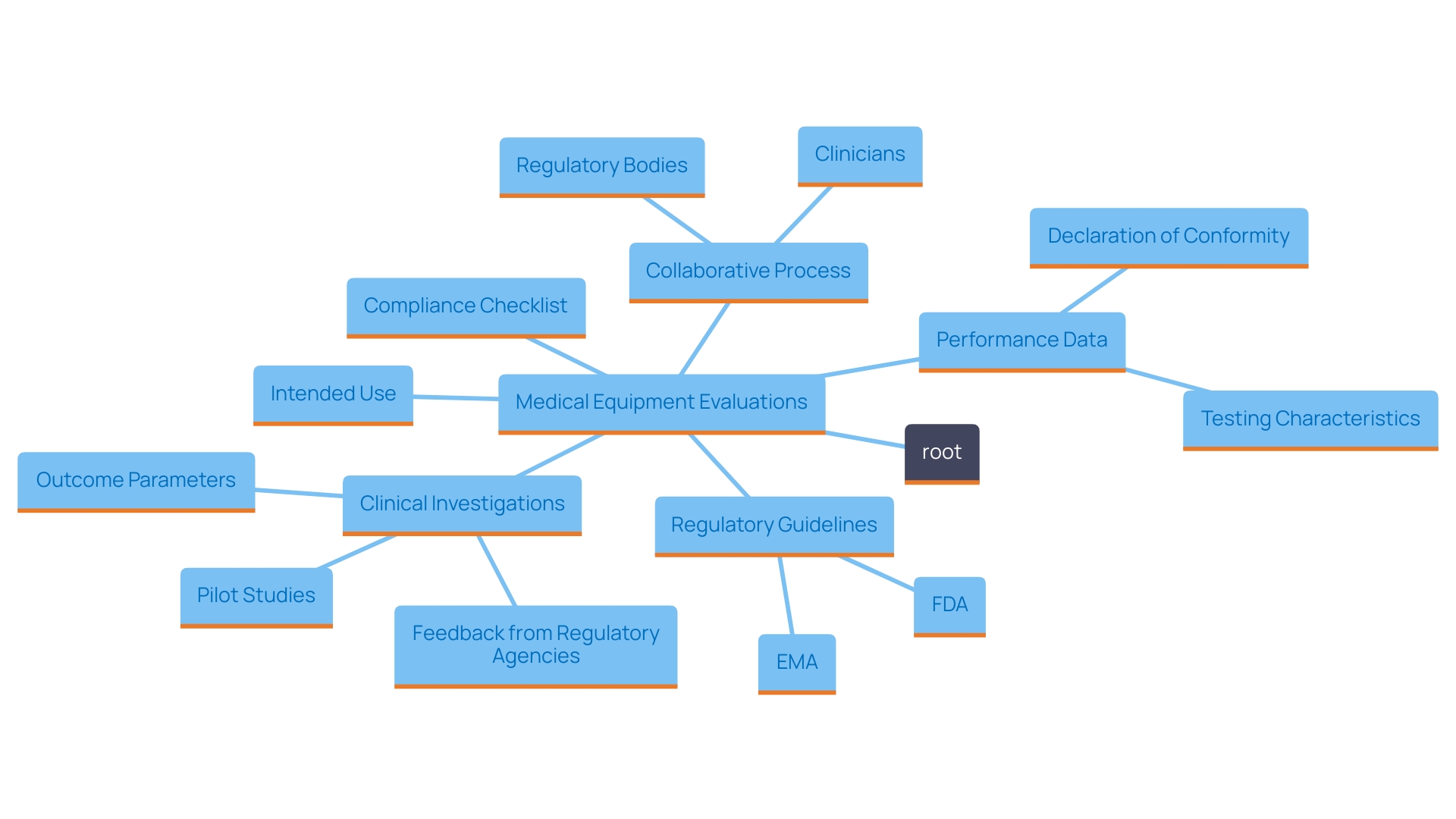
Understanding Regulatory Frameworks for Medical Device Trials
To ensure the success of medical equipment evaluations, it is essential to thoroughly comprehend the regulatory environment that oversees these studies. Familiarize yourself with the guidelines provided by key regulatory bodies such as the FDA and EMA, which delineate the essential compliance measures necessary for conducting trials. A well-structured approach begins with the development of a comprehensive checklist that encompasses all relevant regulations. This checklist should include critical factors related to the intended use of the medical instrument, as defined by the EU Medical Device Regulation (MDR). The intended use outlines the purpose, user demographics, targeted patient populations, medical conditions addressed, and the operational principles of the product.
Moreover, manufacturers need to meticulously document how their device's intended use aligns with its functionalities and indications. This alignment is essential, as demonstrating safety and efficacy relies on the gathering of appropriate performance information. Engaging with regulatory bodies early in the process can provide valuable insights into the necessary performance criteria and the types of information required. This collaborative effort is essential, especially when defining outcome parameters in medical investigations, which should involve a multidisciplinary team of clinicians, patients, and experts to ensure the relevance and feasibility of the parameters being studied. Such diligence not only promotes compliance but also enhances the integrity and reliability of the information gathered during the study, ultimately facilitating smoother regulatory approvals.
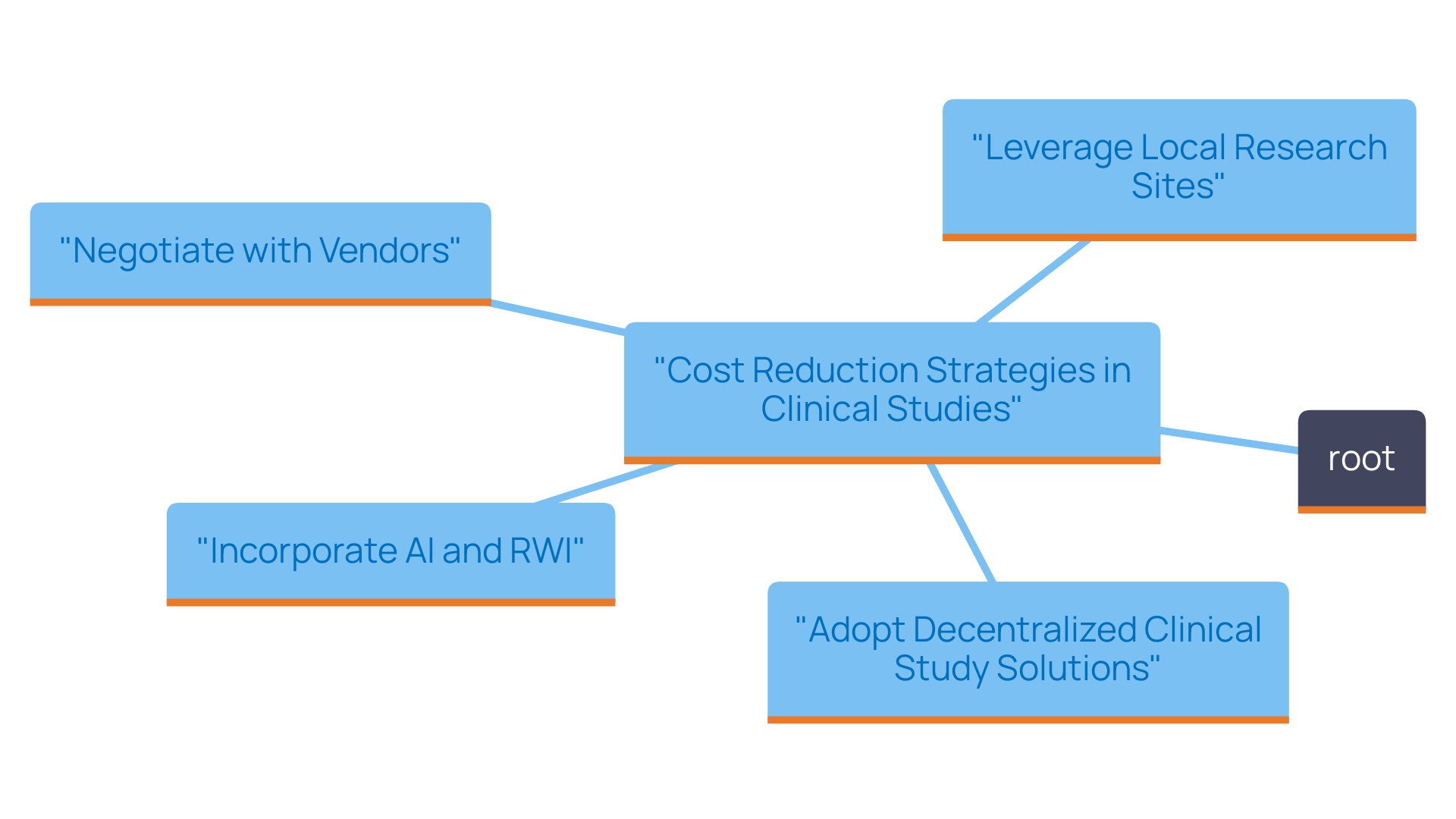
Strategies for Cost Reduction in Medical Device Trials
To effectively identify potential areas for cost reduction in clinical studies, a thorough evaluation of past study expenditures is essential. This involves analyzing historical data to pinpoint where expenses were highest and understanding the underlying causes. Strategies may include leveraging local research sites to cut travel costs, negotiating favorable terms with vendors to reduce overhead, and implementing a risk-based monitoring approach that allows for efficient allocation of resources without compromising the integrity of the study. Furthermore, the adoption of decentralized clinical studies (DCT) solutions, accelerated by the COVID-19 pandemic, offers innovative ways to mitigate costs. With 89% of sponsors now utilizing decentralized technology, studies can be conducted remotely, allowing for greater participant diversity and retention—especially from rural areas—thus potentially lowering participant-related costs. Incorporating artificial intelligence (AI) and real-world information (RWI) can further improve efficiency, shortening study durations and overall costs while ensuring that the quality of information remains strong. As emphasized by industry specialists, enhancing research design and actively incorporating patient input can result in more efficient cost management approaches that ultimately aid in the creation of innovative therapies.
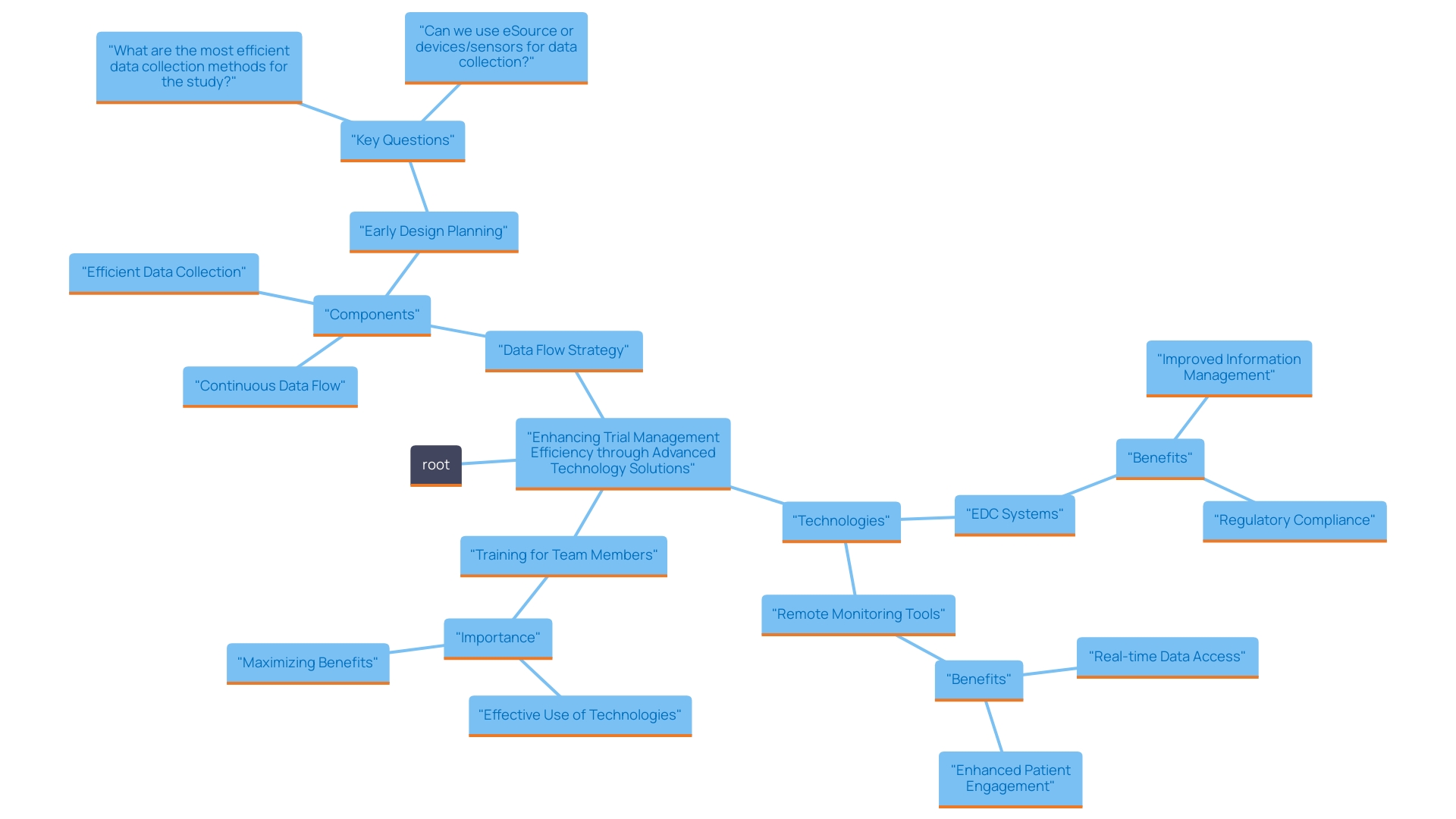
Leveraging Technology for Efficient Medical Device Trials
To enhance the efficiency of trial management processes, it is essential to implement advanced technology solutions such as electronic information capture (EDC) systems, remote monitoring tools, and comprehensive project management software. EDC systems transform the gathering and storage of health information, reducing the laborious and error-prone aspects of manual information entry. These systems not only enhance information management but also include built-in validation checks that strengthen information reliability, a factor critically important to regulatory compliance and the overall integrity of the research study.
Moreover, the utilization of remote monitoring tools and decentralized clinical research (DCT) technologies, which have gained traction post-pandemic, provides the flexibility needed to engage participants from diverse locations without the restrictions of geographical proximity to research sites. In fact, studies indicate that 89% of sponsors are now employing decentralized technologies for at least one aspect of their trials, allowing for the capture of real-time information through electronic patient-reported outcomes (ePRO) and digital monitoring solutions.
To ensure that these tools are utilized to their fullest potential, comprehensive training for all team members is vital. This training should encompass not only the operational aspects of the software but also the importance of maintaining information accuracy and participant engagement. By adopting these technological innovations, teams can significantly decrease the time dedicated to manual tasks, thereby enabling a more concentrated approach to patient care and information integrity. Ultimately, the success of trials relies on the seamless integration of technology with oversight, ensuring that the rights and well-being of participants are prioritized while producing robust and reliable information.
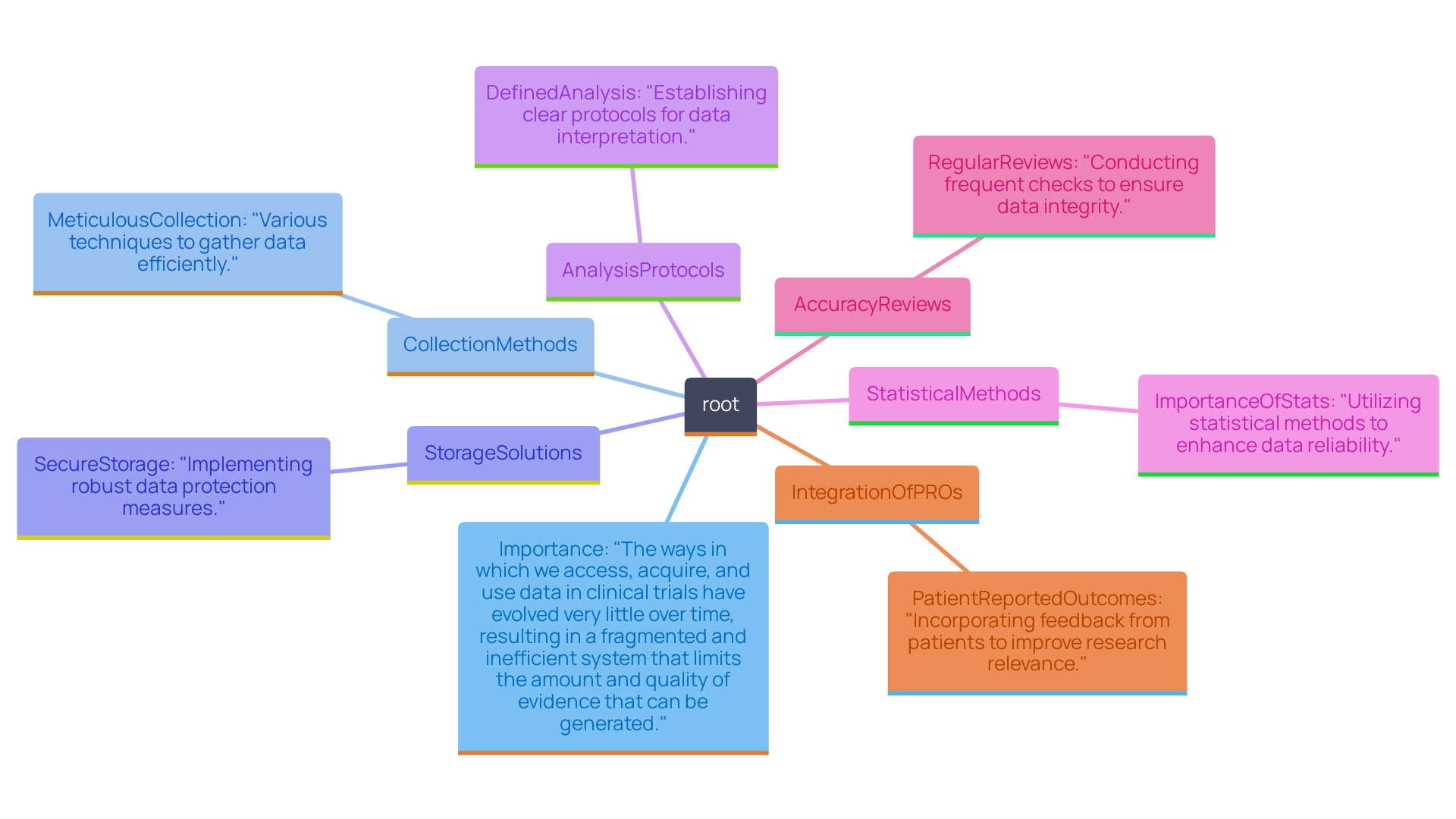
Data Management and Analysis in Medical Device Trials
To ensure the integrity and reliability of clinical research, establishing a comprehensive information management plan is essential. This plan should encompass various facets of information handling, including meticulous collection methods, secure storage solutions, and well-defined analysis protocols. The choice of suitable statistical methods is essential for analyzing trial outcomes, which not only helps in accurately interpreting the information but also guarantees that valid conclusions are derived from it. Regular reviews of information accuracy are paramount, as discrepancies can lead to costly errors that undermine the research's credibility and outcomes.
Furthermore, with guidelines like Article 62 of the European Union Medical Device Regulation (EU MDR) highlighting the necessity for scientifically valid and dependable research findings, the significance of a strong information management strategy cannot be overstated. The necessity for medical information goes beyond simple adherence; it acts as the basis for applications to regulatory authorities, confirming that health instruments are both safe and effective for end-users. In the realm of research studies, especially for high-risk devices, comprehensive information gathering through techniques such as case report forms (CRFs) becomes essential. As the industry shifts towards electronic CRFs (eCRFs), the benefits of increased efficiency and reduced error rates are evident.
Furthermore, incorporating patient-reported outcomes (PROs) into information collection is essential. These insights not only align with regulatory expectations but also reinforce the focus on patient welfare throughout the research study process. By prioritizing the patient's perspective, researchers can gather invaluable information that enhances the understanding of a device's real-world performance, thereby supporting better regulatory submissions and ultimately improving patient outcomes. In summary, a well-structured information management strategy is not merely a procedural requirement; it is a critical element that supports the success and integrity of research endeavors.
Post-Trial Evaluation and Market Strategies for Medical Devices
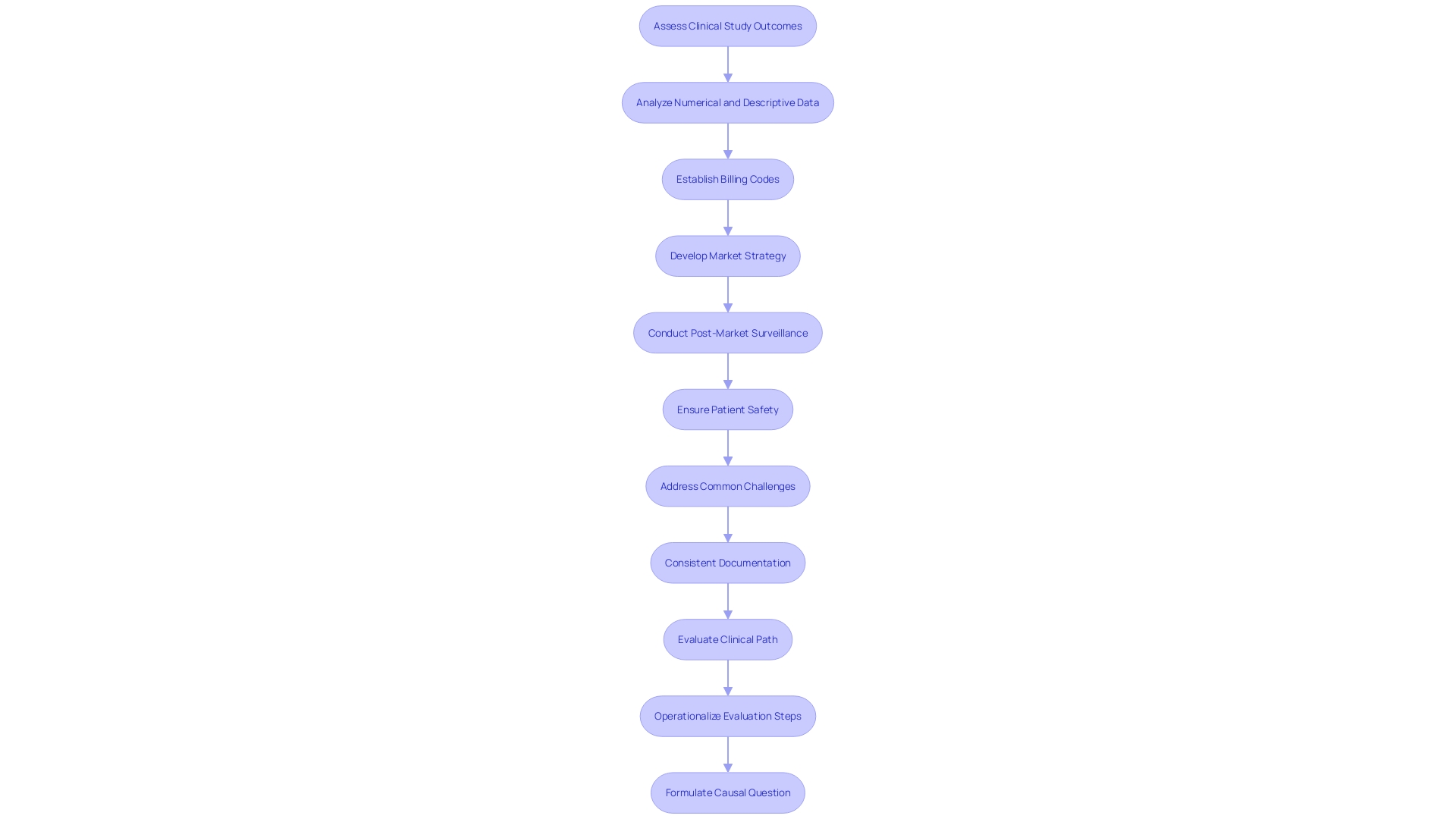
Conducting a thorough post-trial evaluation is essential for assessing the outcomes of clinical studies and identifying valuable lessons learned. This assessment should include a thorough examination of both the numerical and descriptive information gathered during the experiment, enabling a deeper insight into the effectiveness and safety profile. By utilizing this information, teams can improve their processes and enhance the design of future experiments, ultimately driving better patient outcomes.
Moreover, developing a robust market strategy based on trial results is crucial for positioning the medical product effectively within the competitive landscape. This strategy must consider the reimbursement landscape, ensuring that appropriate billing codes are established so healthcare providers can charge for the equipment seamlessly. A well-informed market strategy will not only meet stakeholder needs but also facilitate smoother adoption by healthcare professionals.
Furthermore, it is crucial to participate in active post-market surveillance (PMS), which plays a vital role in the continuous monitoring of medical products after their market introduction. Various data collection methods, including electronic health records and administrative databases, should be utilized to detect any safety issues that may not have been apparent during pre-market testing. This ongoing oversight is particularly important given the troubling statistics regarding medical equipment safety, including more than 1.7 million injuries and 83,000 deaths potentially linked to medical equipment over a decade. The FDA's efforts to enhance post-market surveillance systems are a step towards addressing these challenges and ensuring the long-term safety and effectiveness of medical devices in real-world settings.
Conclusion
Navigating the complexities of medical device trials necessitates a deep understanding of regulatory frameworks, strategic cost management, technological integration, meticulous data management, and thorough post-trial evaluations. Key regulatory bodies like the FDA and EMA set forth guidelines that are essential for compliance and successful trial outcomes. By developing comprehensive checklists and engaging with these regulatory authorities early, manufacturers can ensure that their trials are well-structured and aligned with necessary compliance measures.
Cost reduction strategies, such as utilizing decentralized clinical trial solutions and leveraging technology like artificial intelligence, can significantly enhance the efficiency of trials while ensuring data quality. The integration of advanced technologies, including electronic data capture systems and remote monitoring tools, allows for better data management and participant engagement, ultimately streamlining the trial process.
Moreover, establishing a robust data management plan is crucial for maintaining the integrity and reliability of clinical research. This includes employing appropriate statistical methods and regularly reviewing data to prevent discrepancies. The emphasis on patient-reported outcomes further ensures that the focus remains on patient welfare, enhancing the real-world applicability of the results.
Finally, post-trial evaluations and effective market strategies are vital for analyzing outcomes and ensuring the successful adoption of medical devices. Engaging in active post-market surveillance not only addresses safety concerns but also reinforces the commitment to patient safety and device efficacy in real-world settings.
In summary, optimizing medical device trials requires a multifaceted approach that balances regulatory compliance, cost efficiency, technological innovation, and a strong focus on data integrity and patient safety. By prioritizing these elements, stakeholders can enhance the effectiveness of clinical trials and ultimately contribute to better health outcomes for patients.




