Introduction
The process of identifying clinical trial sites plays a crucial role in the success and efficiency of a study. Selecting the right sites is essential for recruiting eligible participants and gathering reliable data. However, this process is multifaceted and involves evaluating factors such as patient demographics, site capabilities, and regulatory compliance.
In the era of electronic health records (EHR), integrating EHR data with traditional trial methods presents additional challenges. Clinical trials often face recruitment, engagement, and retention hurdles, leading to delays and financial consequences. Strategic site selection and management are crucial in overcoming these obstacles and advancing medical research.
This article explores the background, challenges, strategies, and outcomes of clinical trial site identification, highlighting the importance of a comprehensive and data-driven approach.
Background and Importance of Clinical Trial Site Identification
The identification of clinical trial sites is a pivotal step that can significantly influence the outcomes and efficiency of a study. Selecting the right sites for clinical trials is critical to not only recruit eligible participants but also to gather dependable data. This multifaceted process requires a thorough evaluation of factors including patient demographics, the capabilities of the site, and adherence to regulatory compliance.
In the era of electronic health records (EHR), trials sourcing data from EHR systems face challenges regarding the utilization of existing trial sites and infrastructure to meet study objectives. A recent demonstration project described in Trials (2023) 24:566 exemplifies how EHR data was integrated with data collected from a multi-center pharmaceutical industry outcomes trial, underscoring the need for evidence supporting the use of EHRs in clinical trial settings. The coordination of technical, governance, and operational support by a central coordinating center was essential in this context.
Moreover, the efficiency of clinical trials is often impeded by recruitment, engagement, and retention hurdles, with nearly 80% failing to finish on schedule and 20% experiencing delays of six months or more, as noted in the medical research field. This is compounded by more than two-thirds of trial sites falling short of meeting their enrollment targets, which can have substantial financial repercussions for trial sponsors and clinical research organizations (CROs). As such, the strategic selection and management of clinical trial sites are instrumental in mitigating these issues and propelling the advancement of medical research.
Challenges in Clinical Trial Site Identification
Identifying suitable clinical trial sites is a complex and critical task that faces numerous barriers. Limited access to diverse patient populations poses a significant challenge, as clinical trials often fail to represent the full spectrum of potential patients. For example, Walgreens is leveraging its established presence in communities to address these accessibility issues and increase the representation in clinical research by offering clinical trial services in its stores and pharmacies.
Competition for qualified investigators is another hurdle. The expertise required to conduct trials is highly specialized, and demand often exceeds supply. This can lead to delays, as securing the right investigators is crucial for the integrity and success of a trial.
Moreover, the efficient operation of 'EHR-sourced' trials, which utilize patient data from electronic health records, is still being refined. A demonstration project cited in Trials (2023) 24:566 illustrated the technical, governance, and operational support necessary from a central coordinating center to effectively manage these types of trials.
Patient recruitment is a further issue, with reports indicating that up to 85% of clinical trials do not meet recruitment goals, and up to 80% are delayed due to these challenges. Patients in rural areas or those with rare diseases may face significant logistical barriers to participation, as highlighted by the example of a patient in rural Pennsylvania needing to travel to Turkey for a trial. This not only impacts the patients but also the overall trial timelines and costs.
In addition, the structure of clinical trials has been traditionally geared towards large research institutions in urban settings, potentially excluding those in rural communities. Modern technology now allows for more decentralized trials, yet regulations have yet to fully adapt to these possibilities.
Overall, the goal is to facilitate effective and inclusive clinical trials that can lead to new treatments. The insights and experiences of professionals like Etienne Nichols, with expertise in medical devices and clinical trial systems, are invaluable in overcoming these challenges. The industry continues to seek innovative solutions to streamline clinical trial site identification and enhance the efficiency and inclusivity of clinical research.
Case Study: Successful Strategies for Optimizing Site Identification
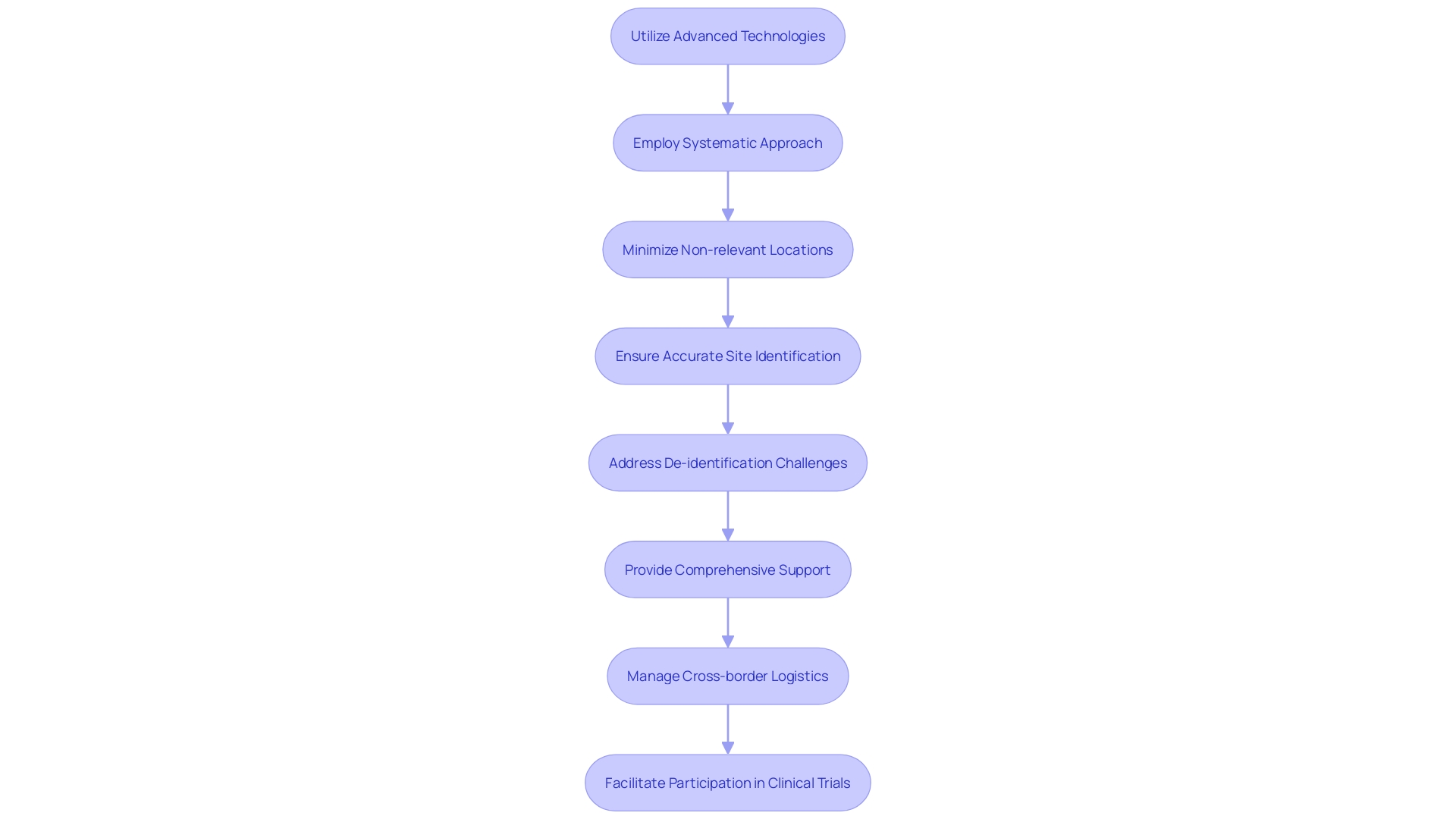
Adopting a sophisticated site identification strategy is essential for the success of clinical trials. A leading research organization demonstrated this by utilizing advanced technologies and a systematic approach, which streamlined their site selection process significantly. They achieved this by employing a methodology that ensured the accurate identification of relevant sites while minimizing the inclusion of non-relevant locations.
This precision was crucial in de-identifying data for research publication, much like the challenges faced in the de-identification of unstructured data in educational research. In the latter case, the absence of structured labels such as 'Name' or 'Address' commonly found in structured data made the process complex, but the organization's methodical strategy proved successful in overcoming such hurdles.
The implications of effective site identification extend beyond operational efficiency. For example, consider a patient with a rare disease in rural Pennsylvania who is presented with a life-saving clinical trial opportunity in Turkey. The success of this clinical trial not only depends on identifying the patient as a suitable candidate but also on the seamless coordination of cross-border logistics.
This includes visa procurement, translation of documents, and travel arrangements. The organization's adept handling of site identification and patient recruitment mirrors the comprehensive support required for such complex scenarios, emphasizing the multifaceted challenges in clinical research.
Clinical trials, like those using electronic health records (EHR) to gather patient data, underscore the necessity for robust site infrastructure. A demonstration project highlighted in 'Trials (2023) 24:566' reveals the potential of EHR-sourced trials and the pivotal role of a central coordinating center in managing the technical, governance, and operational facets of these trials. This initiative is a testament to the ongoing evolution of clinical trial methodologies and the importance of adapting to contemporary clinical settings.
The organization's strategy and resulting outcomes contribute significantly to the broader landscape of clinical research, which is foundational in advancing medical knowledge and improving human health. The meticulous design and execution of clinical trials are instrumental in bridging the gap between laboratory discoveries and practical applications, a process often fraught with challenges, including patient recruitment and retention. Thus, the organization's successful site identification strategy not only enhanced their operational capabilities but also served as an integral part of the larger endeavor to transform healthcare practices through clinical research.
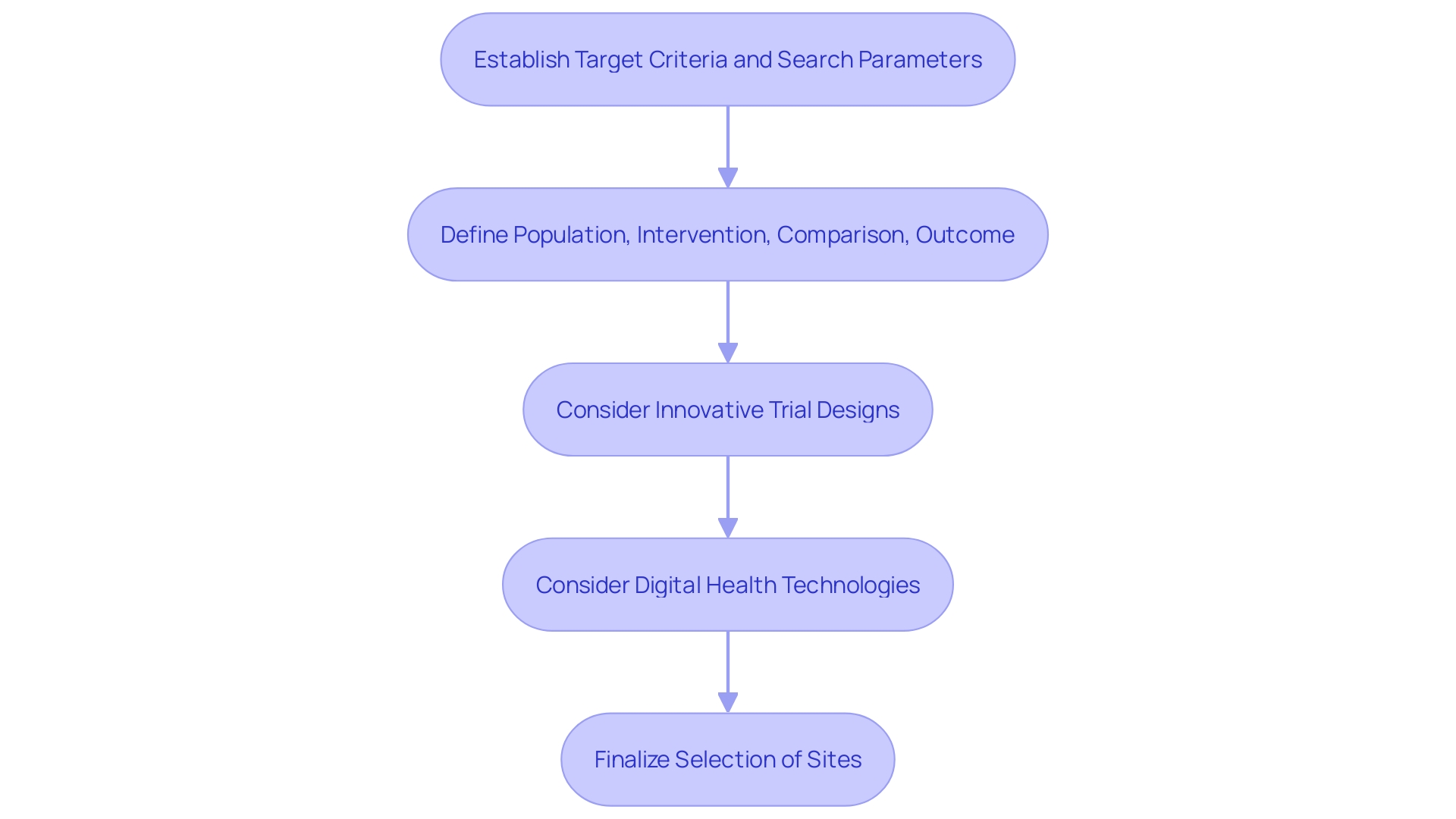
Step 1: Defining Target Criteria and Search Intent
To streamline the identification of suitable clinical trial sites, it is paramount to first establish explicit target criteria and search parameters. This entails pinpointing the particular patient demographic, geographical regions, and therapeutic domains pertinent to the study. A well-defined set of criteria ensures that researchers can concentrate on sites with the highest probability of fulfilling the study's needs.
For example, evidence from a demonstration project described in Trials (2023) 24:566 illustrates the value of using electronic health records (EHR) to enhance data quality and operational efficiency in multi-center pharmaceutical trials. Such precise targeting not only aids in the effective utilization of existing trial sites and infrastructure but also propels the practical application of EHRs in modern clinical trial contexts.
The process mirrors the approach of expert problem solvers who prioritize understanding the issue at hand before considering potential solutions. As such, the formation of a research question is critical, with a focus on creating a question that is both focused and answerable. To develop a focused research question, it is essential to clearly define the population, intervention or exposure, comparison, and outcome of interest.
For instance, understanding the exposure factor, like smoking, and its association with a specific outcome, such as lung cancer, can greatly influence the study design and site selection.
Moreover, as the clinical research landscape evolves with innovative trial designs and digital health technologies, integrating lessons learned from diverse fields can be beneficial. The C3TI initiative, as mentioned by Bugin, aims to share knowledge across various trial types, emphasizing the importance of adaptability and context in clinical research. Such innovative approaches, including the use of real-world evidence and efforts to increase participation from underserved populations, can inform the criteria for site selection.
In summary, the initial step in optimizing clinical trial site identification is to meticulously articulate the target criteria and search intent. This lays the groundwork for a focused and effective search, ensuring that selected sites are equipped to meet the specific requirements of the study and embrace contemporary innovations in clinical research design.
Step 2: Conducting Thorough Keyword and Site Research
Identifying the ideal clinical trial sites and investigators starts with a meticulous approach to keyword and site research. It's essential to use relevant keywords and search terms tailored to the specific patient populations and disease areas of interest. Advanced database searches, patient registries, and robust online platforms can reveal invaluable insights into a site's capacities, historical performance, and demographic reach.
Case studies underscore the challenges faced by patients when trial locations are distant or international, such as the logistical hurdles for a rural Pennsylvania patient considering a trial in Turkey. These real-world examples highlight the need to understand and select accessible and capable sites.
Furthermore, the significance of this research phase is echoed by industry experts like Etienne Nichols, who stress the importance of framing the research question correctly to guide methodology. This approach ensures that the clinical trial addresses focused and answerable questions, a cornerstone in the realm of medical research.
Clinical trial efficiency, including patient recruitment and retention, remains a pivotal concern. Statistics show a staggering 80% of clinical trials do not complete on time, often due to insufficient patient enrollment. This has considerable financial repercussions for sponsors and highlights the importance of selecting the right sites that can meet enrollment targets and support patient retention.
Incorporating real-time data and insights, such as those from Citeline, can aid in the assessment of rare diseases and the development of preclinical candidates. By leveraging cutting-edge tools and methodologies, such as 'digital twins' proposed by Karen Willcox, researchers can forecast and plan clinical trials with greater precision.
As clinical trial companies endeavor to connect treatments with patients efficiently, it's imperative that they employ comprehensive keyword and site research to operationalize study goals, particularly in the context of EHR-sourced trials. This strategic approach not only enhances the potential for successful outcomes but also aligns with the evolving needs of the healthcare industry.
Step 3: Evaluating Site Feasibility and Suitability
The meticulous evaluation of clinical trial sites is a cornerstone of successful clinical research. These sites must have the appropriate infrastructure, including access to efficient electronic health record (EHR) systems that can facilitate pragmatic clinical trials. A study highlighted in Trials (2023) 24:566 demonstrates the complexities associated with EHR-sourced trials, emphasizing the need for a robust operational framework to fully leverage these digital systems.
It is imperative to ascertain not only the site's capacity to handle the trial but also its staff's expertise in managing the integration of EHR data with traditional trial methods.
In addition to technical considerations, the potential for patient recruitment remains a critical factor. As illustrated by a case where a patient in rural Pennsylvania with an ultra-rare disease was presented with the opportunity to participate in a trial in Turkey, logistical hurdles can be significant. Such scenarios underscore the importance of evaluating the site's ability to navigate cross-border regulatory and logistical challenges, ensuring patients can participate without undue burden.
Furthermore, the alignment with regulatory requirements cannot be overstated. With the FDA issuing draft guidance on the operation of data monitoring committees (DMC), it is clear that governance and compliance are under intense scrutiny. The evolving landscape, as evidenced by the UK's clinical trial space gearing up for a revamp amid political promises to improve healthcare systems, signifies that sites must be agile and compliant with international standards.
Ultimately, the suitability of a site is multifaceted, encompassing technical capabilities, governance, patient accessibility, and a proven track record in managing clinical trials. The goal is to ensure that each site can contribute to the overarching mission of enhancing patient outcomes, as echoed by industry voices emphasizing the importance of embedding research within clinical practice for the benefit of patients, workforce, and the healthcare system at large.
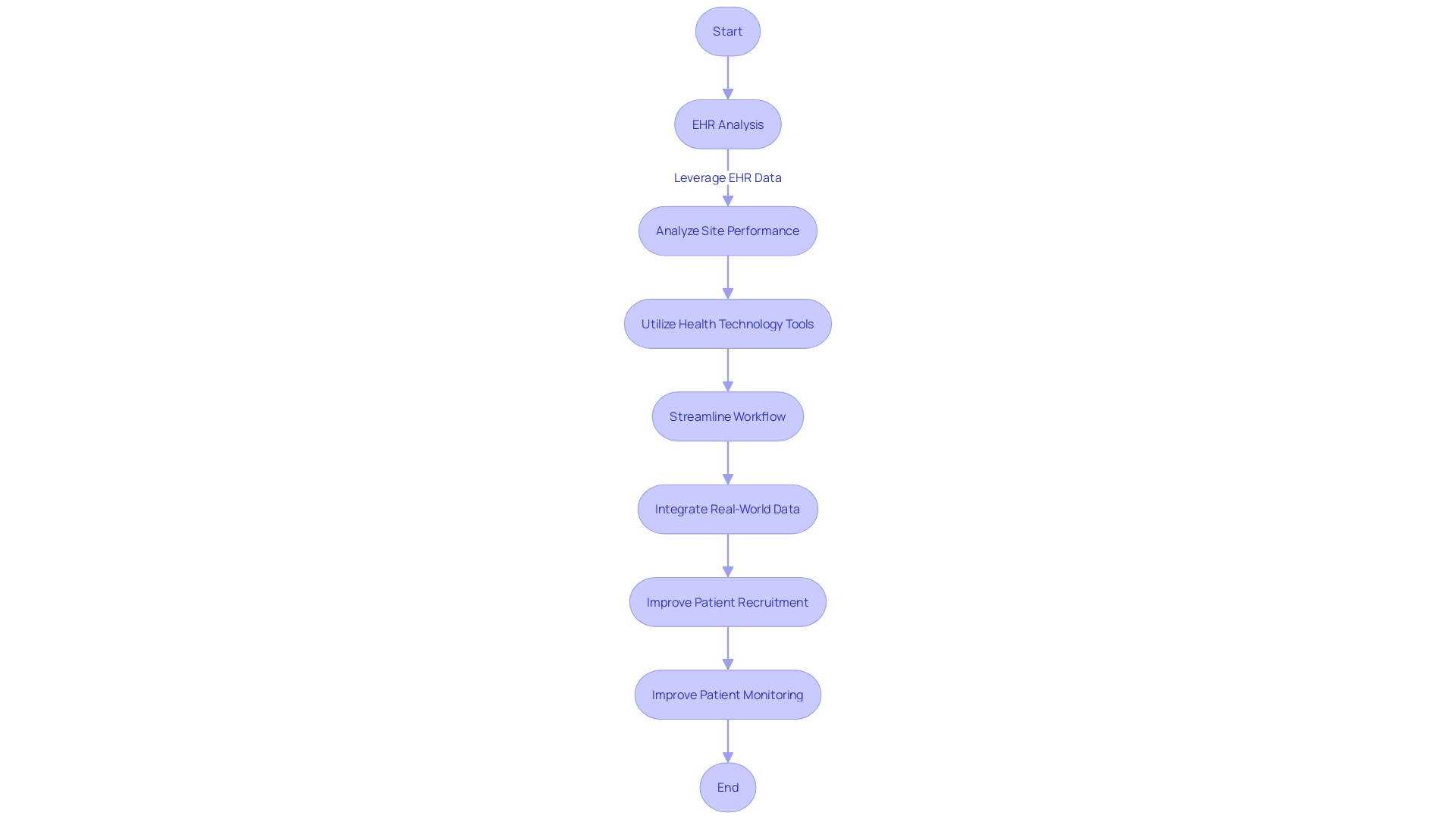
Step 4: Implementing Effective Site Selection Tools and Technologies
The integration of advanced software platforms and data analytics is revolutionizing the site identification process for clinical trials. By leveraging electronic health records (EHRs) and other digital health data, researchers can gain a comprehensive understanding of site performance, including patient enrollment rates and compliance with regulatory standards. These insights are essential for conducting EHR-sourced trials, which rely on existing trial sites and infrastructure to meet study goals effectively.
For instance, a demonstration project utilizing EHR data to support a multi-center pharmaceutical trial showcased how a central coordinating center can facilitate technical, governance, and operational aspects, enhancing the overall efficiency of site selection.
With the advent of health technology, tools like brain-computer interfaces and 'mouthpad' tongue-controlled interfaces are not only transforming patient interaction with medical devices but also opening new avenues for patient recruitment and monitoring. Such innovations are pivotal in ensuring that clinical trials are inclusive of diverse patient populations, thus improving the generalizability of research findings and minimizing health inequalities.
However, the clinical trial landscape faces challenges due to the proliferation of disparate technological solutions, with some research sites managing over 20 systems daily. This complexity can lead to staff burnout and reduced site capacity, prolonging research timelines. To combat this, a concerted effort to streamline the clinical trial workflow through a unified data strategy is crucial.
This approach involves the integration of data from connected devices, wearables, and AI-driven methodologies to glean richer insights and inform drug development.
Moreover, the use of real-world data (RWD) is gaining traction, as emphasized by health authorities like the FDA, to optimize clinical trial design and site activation. According to Flatiron Health's research, the quality of RWD hinges on its relevance and reliability in informing scientific inferences. Therefore, a strategic application of RWD can lead to more effective patient-centered clinical trials and potentially serve as an external control arm in research settings.
Ultimately, the goal is to harness technology to not only streamline site identification but also to create a more patient-centric, efficient, and inclusive clinical trial ecosystem. Tools like ResearchMatch further this ambition by bridging the gap between potential participants and researchers, thereby improving access to clinical trials and contributing to advancements in medical knowledge and patient care.
Step 5: Ensuring Compliance with Regulatory Standards
In the realm of clinical trial site identification, adherence to regulatory standards is not just a mandate, it is integral for the integrity and success of a study. It is essential for researchers and clinical trial companies to ensure that sites are compliant with ethical guidelines, patient safety protocols, and Good Clinical Practice (GCP) standards. The rigorous landscape of clinical trials requires sites to uphold a commitment to quality and safety, as exemplified by Good Manufacturing Practice (GMP) guidelines, which encompass aspects such as facility cleanliness, equipment verification, and employee training.
The significance of compliance is highlighted in the context of innovation, where the use of artificial intelligence (AI) and machine learning (ML) is under intense scrutiny by regulatory bodies. Recent guidelines from the FDA and the European Medicines Agency (EMA) suggest a risk-based approach to AI, demanding transparency and advocating for pre-planned change control plans to maintain compliance.
Additionally, the environmental impact of clinical trials is under increasing examination. As part of the industry's commitment to sustainability, innovative approaches are being pioneered to minimize the carbon footprint of clinical trials. This includes the implementation of tools like the Carbon Emission Index, which enables trial teams to evaluate and optimize the GHG emissions associated with their studies, ensuring that environmental considerations are integrated from the trial design phase.
The importance of compliance extends to inclusivity as well. The recent FDA guidance on diversity in clinical trials urges sponsors to factor in site locations and community-based care to facilitate the participation of diverse populations. This is critical for ensuring that trial outcomes are relevant and applicable to the broader patient population.
In summary, maintaining regulatory compliance is a multifaceted endeavor that encompasses ethical conduct, patient safety, innovation, environmental stewardship, and inclusivity. It is a foundational aspect of clinical research that ensures the validity and applicability of study results, ultimately contributing to the advancement of patient care and medical knowledge.
Results and Outcomes: Success Metrics and Case Study Findings
Optimizing site identification is a pivotal component in the successful execution of clinical trials. A recent case study in the realm of electronic health record (EHR)-sourced trials has shed light on the significance of carefully selecting trial sites and infrastructure to support study goals effectively. The case study examined the use of EHR data to supplement information gathered for a multi-center pharmaceutical industry outcomes trial.
A central coordinating center played a crucial role in aiding sites through technical, governance, and operational challenges.
The demonstration project highlighted in this case study provides invaluable insights into the operational considerations crucial for site selection, including assessing the feasibility and capabilities of potential sites, and determining the most suitable data extraction strategies. The study also scrutinized site performance, data transfer protocols, and quality review processes. By addressing these elements, the case study was able to identify key operational hurdles and develop best practices for site identification in EHR-sourced trials.
One of the key findings was the importance of a centralized coordinating center in supporting site participation and facilitating the technical aspects of EHR data integration. This support was essential in overcoming the uncertainty that often hampers the operationalization of study goals in clinical trial settings. The study's success metrics, which included data quality and site performance, demonstrated the positive outcomes of the strategic approach to site identification.
These metrics underscore the potential for optimizing trial efficiency and data integrity through well-chosen sites and robust supporting infrastructure.
As clinical trials continue to evolve with the integration of digital data sources, such as wearables and electronic diaries, the need for strategic site identification and a comprehensive data strategy becomes increasingly important. The ability to manage data flow and extract meaningful insights from vast amounts of clinical data relies on the thoughtful alignment of trial sites and the technologies they employ. The lessons learned from this case study are instrumental in guiding future clinical trials towards more successful and efficient outcomes.
Best Practices and Recommendations for Future Trials
To enhance the efficiency and efficacy of clinical trials, embracing technological advancements and data-driven strategies is essential. For instance, the utilization of electronic health records (EHRs) can significantly streamline the process. As demonstrated in a recent project, EHR data was effectively used to complement information collected for a multi-center trial, highlighting the potential to optimize existing trial sites and infrastructure for study goals.
This pragmatic approach underscores the importance of a robust data strategy prior to protocol design, emphasizing the need for meticulous planning in data collection from both traditional and digital sources.
Moreover, the inclusion of patient voices in the earliest phases of new medicine development, as seen in the MHRA's pilot program, reflects the industry's shift towards patient-centered drug development. The integration of feedback from connected devices, wearables, and electronic diaries allows for a more comprehensive understanding of patient behaviors and trends. However, to convert the vast amounts of data into actionable insights, it is crucial to establish a clear data strategy that addresses data management expectations, risk mitigation through data collection, and the impact on site operations.
The critical role of these strategies is further reinforced by recent guidelines, such as those outlined in the FDORA, which dictate the submission of diverse and inclusive data analysis plans (DAPs) to regulatory authorities like the FDA. These plans should detail enrollment goals, the rationale behind them, and the metrics for success, particularly in multinational studies, ensuring that diverse patient populations are adequately represented.
In summary, clinical trial companies should consider integrating these best practices to refine site identification processes: leveraging EHRs, involving patients early in the drug development process, and ensuring comprehensive data strategies are in place. Such practices not only facilitate better trial outcomes but also pave the way for more inclusive and patient-centric research efforts.
References and Further Reading
A broadening of understanding in clinical trial site identification is critical for the advancement and success of research. Publications like Raman et al. in Trials (2023) 24:566, licensed under a Creative Commons Attribution 4.0 International License, delve into the challenges and strategies for utilizing electronic health records (EHR) in trials.
Their work highlights the practical use of EHRs to enhance data quality in multi-center pharmaceutical industry outcomes trials, emphasizing the need for robust site infrastructure to operationalize study goals.
Experts like Etienne Nichols, a medical device guru, and Karen Willcox with her work on "digital twins" provide insights into the technological advancements shaping clinical trial designs, underscoring the importance of understanding complex systems. Similarly, the FDA's recent discussions on decentralized clinical trials (DCTs) illuminate the current obstacles faced in oncology care and research, as noted in Bugin's comments on the importance of sharing innovative trial methodologies across various disciplines.
The field is also witnessing a data-driven transformation, as highlighted by the creation of the FDA's Compass Repository—an initiative to connect users to clinical trial innovation information swiftly. This database represents an effort to streamline workflows and reduce administrative burdens, enabling broader participation in clinical trials.
Furthermore, the narrative of a patient with an ultra-rare disease considering participation in an international clinical trial illustrates the logistical challenges and underscores the need for localizing trial participation to reduce barriers. This is supported by the observation that many oncologists lack comprehensive knowledge of the clinical trial landscape, which could hinder patient access to experimental treatments.
In conclusion, the landscape of clinical trial site identification and operation is evolving rapidly, driven by technological advancements, regulatory innovations, and a push for more inclusive and patient-centric approaches. For those seeking to delve deeper into this subject, a wealth of resources are available, each contributing valuable insights and guiding principles for the future of clinical research.
Conclusion
In conclusion, clinical trial site identification is crucial for successful and efficient studies. Selecting the right sites is essential for recruiting eligible participants and gathering reliable data. Integration of electronic health records (EHR) data presents challenges and opportunities for improved data quality and operational efficiency.
Strategic site selection and management are vital in overcoming recruitment and retention hurdles. Challenges include limited access to diverse patient populations and competition for qualified investigators. Leveraging community presence and utilizing centralized coordinating centers can address these challenges.
Effective site identification strategies streamline the process. Advanced technologies and a systematic approach accurately identify relevant sites, ensuring data de-identification and seamless logistics coordination. Successful outcomes bridge the gap between laboratory discoveries and practical applications.
Defining target criteria and conducting thorough keyword and site research optimize site identification. Real-time data and insights inform assessments of capacities, performance, and demographic reach. Evaluating site feasibility and suitability considers technical capabilities, patient recruitment potential, and regulatory compliance.
Implementing effective site selection tools and technologies revolutionizes the process, enabling comprehensive understanding and operational efficiency. Adhering to regulatory standards ensures integrity and success. Compliance with ethical guidelines, patient safety protocols, and Good Clinical Practice (GCP) is crucial.
Successful outcomes and case study findings highlight the importance of strategic site identification. Integration of EHRs and digital health data enhances site performance and data quality. Leveraging technology and data-driven strategies makes clinical trials more patient-centric, efficient, and inclusive.
In conclusion, clinical trial site identification is a complex process. Embracing advancements, refining processes, and maintaining regulatory compliance optimize trials for better patient outcomes and advancement of medical knowledge.




