Overview
Strategies for success in clinical trial innovation for devices involve adopting advanced methodologies such as:
- Adaptive study designs
- Leveraging artificial intelligence
- Fostering collaboration among stakeholders
These approaches not only enhance efficiency but also significantly improve participant engagement. The article emphasizes that by streamlining research processes, these strategies lead to better recruitment and retention rates. Ultimately, this results in improved outcomes and expedited market access for medical devices, underscoring the critical importance of innovation in the Medtech landscape.
Introduction
In the rapidly evolving MedTech landscape, clinical trial innovation emerges as a beacon of hope for enhancing the development and approval of medical devices. As the industry confronts unique challenges distinct from pharmaceuticals, the adoption of cutting-edge methodologies and collaborative strategies becomes imperative.
Advancements such as adaptive trial designs and the integration of artificial intelligence are not only increasing the efficiency of clinical trials but also making them more patient-centric. This article explores the transformative trends shaping clinical trials, emphasizing the critical importance of collaboration, diversity, and the strategic use of real-world evidence.
These elements are essential for navigating the complexities of medical device research and ensuring successful outcomes for both patients and healthcare providers.
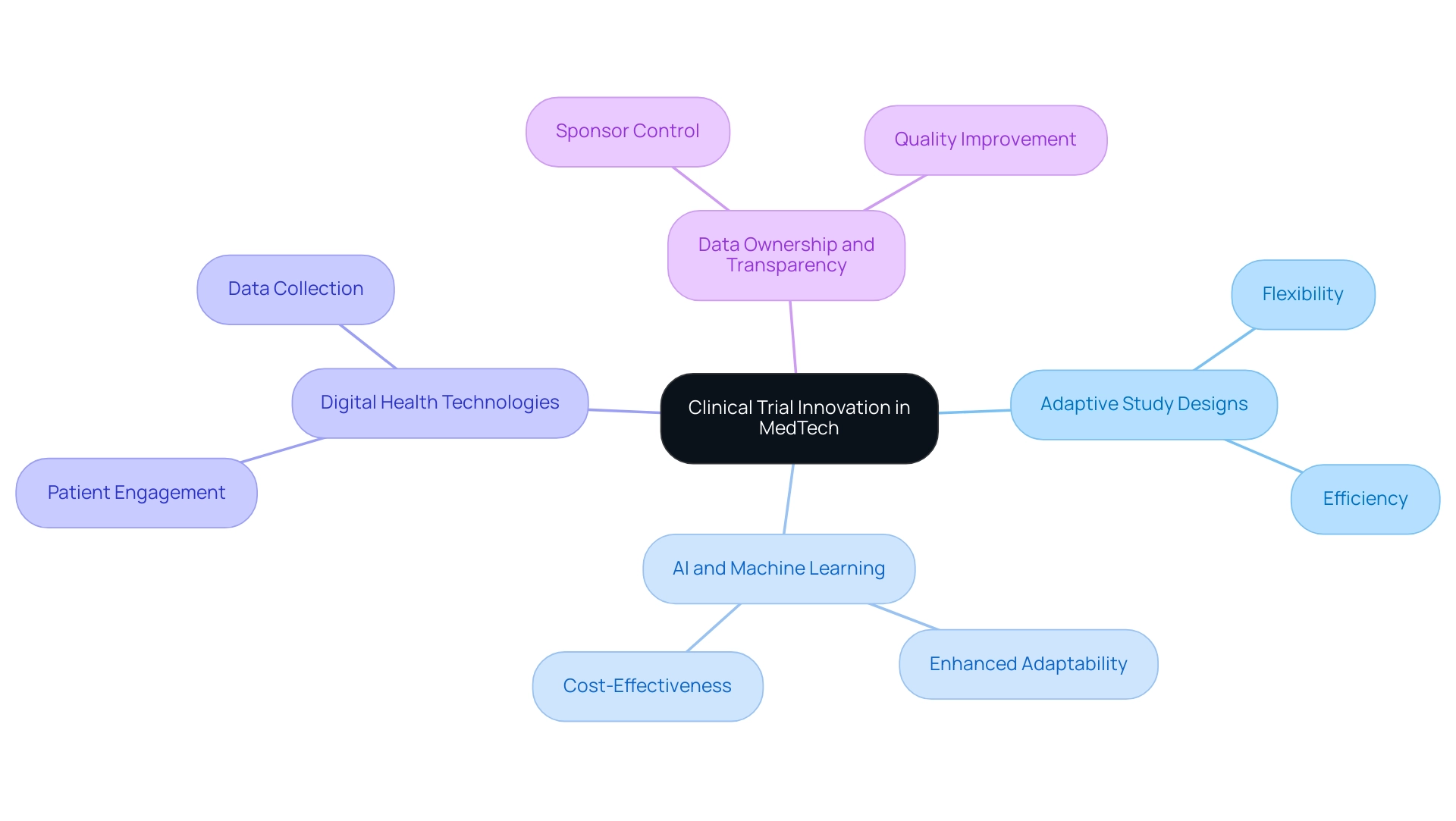
Understanding Clinical Trial Innovation in MedTech
Innovation in the MedTech sector is fundamentally driven by advancements in clinical trial methodologies for devices. This involves the adoption of cutting-edge strategies and technologies that significantly enhance the design and execution of research studies. Such innovation is crucial for tackling the unique challenges associated with medical devices, underscoring the importance of clinical trial innovation, which often navigates different regulatory frameworks compared to pharmaceuticals.
One of the most notable advancements is the implementation of adaptive study designs, which allow for modifications to the study protocol based on interim results. This flexibility not only accelerates the development timeline but also enhances the likelihood of successful outcomes. Recent trends reveal that inter-trial intervals have decreased to an average of 17 months, a substantial improvement from the peak of 32 months recorded in 2022.
This reduction highlights the increasing efficiency of research processes, primarily driven by innovations such as adaptive study designs and the integration of AI and machine learning. These advancements improve the adaptability, agility, and cost-effectiveness of research. Furthermore, the introduction of digital health technologies and decentralized studies is revolutionizing clinical trial innovation for devices, transforming the research landscape. These approaches enhance patient engagement and data collection, making studies more efficient and patient-centric.
As Max Baumann, Head of Execution, notes, there is a persistent emphasis on refining development pathways to ensure that medical endpoints not only facilitate regulatory approval but also prepare products for market success.
In this context, bioaccess® stands out with its comprehensive research management services, including:
- Early-Feasibility Studies (EFS)
- First-In-Human Studies (FIH)
- Pilot Studies
- Pivotal Studies
- Post-Market Medical Follow-Up Studies (PMCF)
With over 20 years of expertise in MedTech, bioaccess® is well-equipped to navigate the complexities of trials in Latin America, ensuring that research is conducted efficiently and effectively.
Recent guidelines have also shifted the focus towards enhanced data ownership and transparency among sponsors. This trend encourages sponsors to assume greater control over their data management, resulting in improved study quality and outcomes for patients. By insourcing data management, sponsors can mitigate risks and alleviate burdens on research sites, ultimately bolstering the integrity of the research process.
This shift is particularly significant as it aligns with the broader trend of leveraging technology to enhance research methodologies.
As we approach 2025, the MedTech sector is poised to continue embracing these innovative research designs and techniques, particularly with an emphasis on clinical trial innovation for devices. The importance of flexible experimental frameworks cannot be overstated, as they provide the essential adaptability for clinical trial innovation for devices, addressing the complexities of medical device evaluations and ensuring that advancements in technology yield tangible benefits for individuals and healthcare practitioners alike.
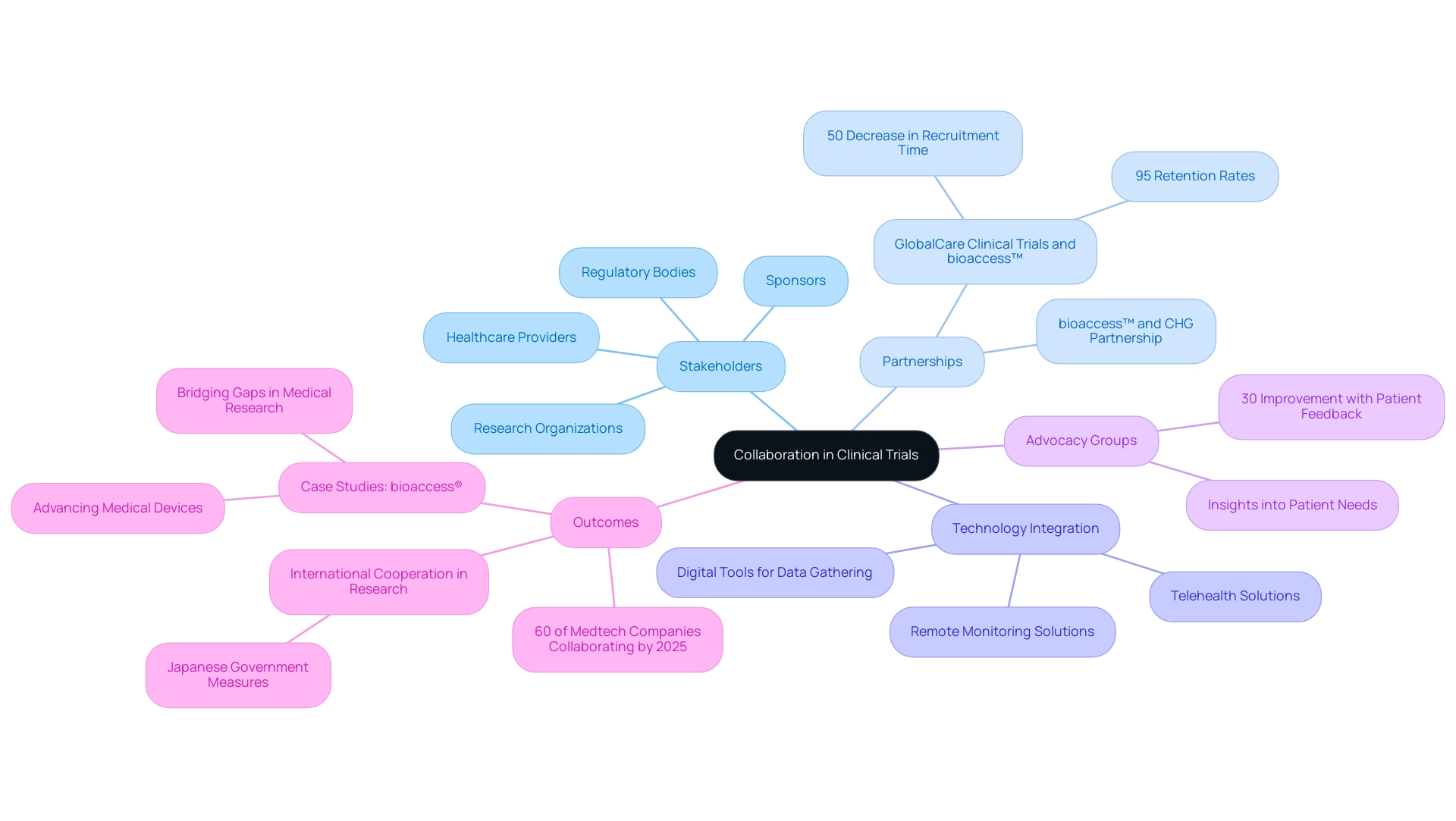
The Role of Collaboration in Advancing Clinical Trials
Cooperation among various stakeholders—including sponsors, research organizations, regulatory bodies, and healthcare providers—is crucial for the success of studies in the Medtech sector. Successful teamwork promotes better research designs, boosts participant recruitment, and simplifies regulatory procedures, ultimately speeding up the journey to market for groundbreaking medical devices.
A significant instance of this collaboration is the partnership between bioaccess™ and Caribbean Health Group (CHG), which aims to establish Barranquilla as a premier location for research studies in Latin America. This initiative, backed by Colombia's Minister of Health, has the potential to transform the region's medical research landscape. Moreover, GlobalCare Clinical Trials' partnership with bioaccess™ has resulted in improvements in ambulatory services in Colombia, achieving over a 50% decrease in recruitment time and remarkable 95% retention rates.
Engaging with advocacy groups is especially advantageous, as these organizations provide essential insights into needs and preferences. This involvement can greatly guide study design, ensuring that research is more aligned with what individuals seek, which in turn can lead to enhanced participant retention. For instance, a recent analysis indicated that studies incorporating patient feedback saw a 30% improvement in recruitment rates, underscoring the influence of advocacy groups on research success.
Furthermore, collaborations with technology firms are becoming increasingly essential. These partnerships enable the integration of digital tools that improve data gathering and analysis, resulting in more efficient experiments. As the landscape of medical research evolves, the incorporation of innovative technologies—such as remote monitoring and telehealth solutions—has proven to streamline processes and enhance data accuracy.
The trend towards collaboration is further supported by statistics indicating that by 2025, over 60% of Medtech companies are expected to engage in collaborative studies, reflecting a shift towards more integrated approaches in research. Moreover, the Japanese government's recent actions to permit Japanese locations to be part of global multi-center Phase III studies without prior Phase I Japanese participant data underscore the increasing trend of international cooperation in medical research.
Upcoming events related to infectious disease studies, occurring at Sands Expo & Convention Centre in Singapore and in Milan, Italy from March 17-19, 2025, further highlight the ongoing significance of collaboration in the sector.
Successful case studies, such as those involving bioaccess®, demonstrate how strategic alliances can bridge gaps in medical research, particularly in areas like Latin America, where the potential for conducting studies is extensive yet underutilized. Dushyanth Surakanti, Founder & CEO of Sparta Biomedical, shared his positive experience with bioaccess® during its initial human study in Colombia, highlighting the effectiveness of these collaborations. By utilizing these partnerships, stakeholders can improve the overall efficiency and effectiveness of research studies, ultimately benefiting the advancement of medical devices through clinical trial innovation and enhancing patient outcomes.
As Emma Mitchell aptly noted, 'A larger team doesn't always lead to better performance,' highlighting the importance of strategic collaboration over mere size in achieving success in clinical research.
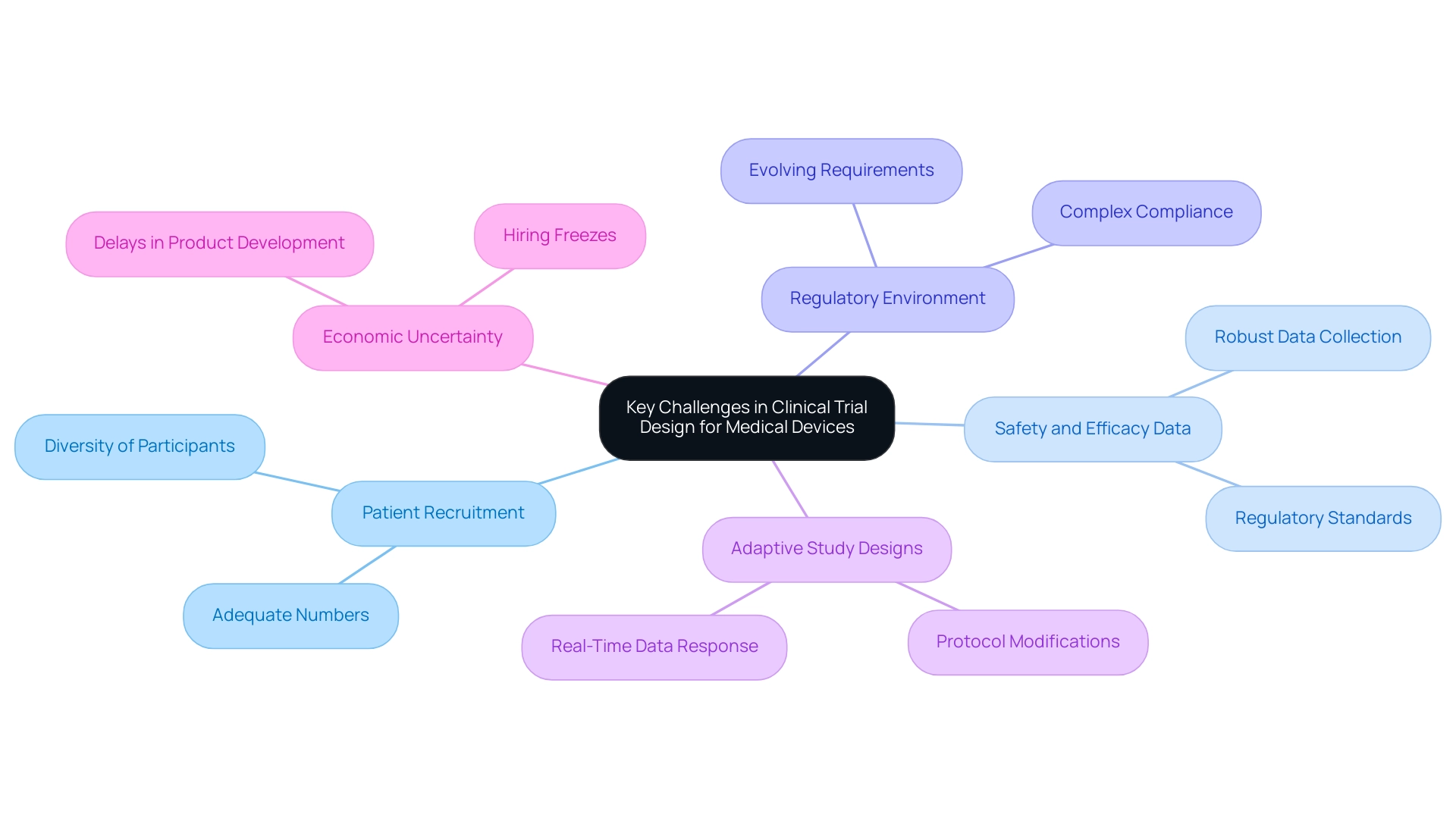
Key Challenges in Clinical Trial Design for Medical Devices
The design of clinical studies for medical devices demands clinical trial innovation, enabling devices to navigate a landscape rife with unique challenges that differ from those faced in pharmaceutical studies. As we approach 2025, the regulatory environment is anticipated to grow increasingly complex, necessitating a comprehensive understanding of evolving requirements. Key challenges include:
- Ensuring adequate patient recruitment, which is critical for the success of any study.
- Addressing the need for robust safety and efficacy data that meets regulatory standards.
The iterative nature of medical device development often calls for clinical trial innovation through adaptive study designs, which allow researchers to modify protocols based on preliminary findings. This flexibility is essential for responding to real-time data, ultimately enhancing relevance and effectiveness. For instance, bioaccess® leverages over 20 years of experience in overseeing Early-Feasibility Studies (EFS), First-In-Human Studies (FIH), Pilot Studies, Pivotal Studies, and Post-Market Clinical Follow-Up Studies (PMCF) to ensure successful research outcomes across Latin America.
By streamlining processes and enhancing site experiences, bioaccess® addresses challenges that impact care, thereby improving overall study efficiency and outcomes.
Moreover, economic uncertainty has led to hiring freezes and delays in product development among larger medical device companies, further complicating the landscape. As Joseph Tucker from Enveric emphasizes, defining and measuring suitable outcomes in clinical studies is crucial, especially in groundbreaking fields such as psychedelics, where conventional metrics may not apply. Vivienne van der Walle, Founder and Medical Director, underscores that "anything that takes away time from patients is a pain point for a site, and anyone who resolves that is helping patient care."
In this context, understanding the regulatory requirements for medical device studies in 2025 is paramount. Companies must remain informed about the latest developments and adapt their strategies accordingly to navigate these challenges effectively. Furthermore, in 2025, we anticipate a broader acceptance of human cells and tissues for drug discovery and development, which could further influence study designs.
By adopting innovative study designs and focusing on patient-centric approaches, bioaccess® can continue to propel the medical technology sector forward through clinical trial innovation for devices, ensuring that new devices reach the market efficiently and safely.
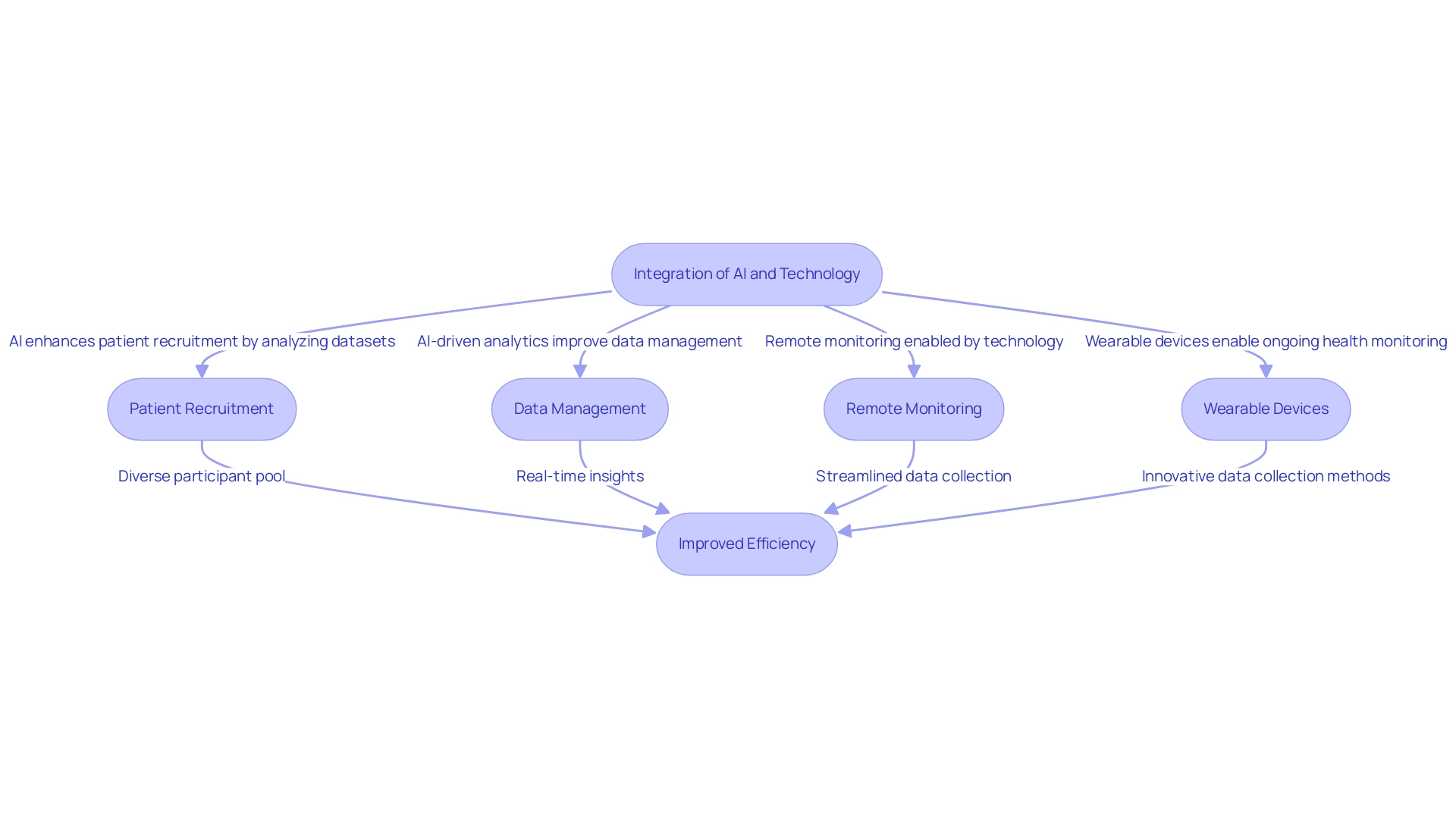
Leveraging AI and Technology for Enhanced Trial Efficiency
The integration of artificial intelligence (AI) and advanced technologies is fundamentally transforming the landscape of clinical trial innovation for devices and study execution. By 2025, the use of AI is expected to significantly enhance patient recruitment through the efficient analysis of extensive datasets, identifying suitable candidates with precision. This capability streamlines the recruitment process and ensures a more diverse participant pool, which is crucial for the generalizability of study results.
AI-driven analytics further enhance research studies by improving data management and monitoring. These tools provide real-time insights into study progress and participant safety, enabling researchers to make informed decisions promptly. For instance, the implementation of electronic patient-reported outcomes (ePROs) has been shown to enhance data collection rigor, supporting the development of effective therapies.
The case study titled 'Measuring Outcomes' highlights the significance of Pros and biomarker identification in medical studies, emphasizing how advancements in electronic Pros can enhance therapeutic assessment. Moreover, organizational change is necessary to fully capture AI's potential for clinical trial innovation for devices, enabling faster delivery of treatments to patients. As Kevin Webster, a partner in the Bay Area office, observes, "Gen AI is set to revolutionize medical studies, particularly through clinical trial innovation for devices, by making processes such as documentation creation, protocol design, and performance monitoring more time and cost effective."
Alongside these technological advancements, bioaccess provides extensive research management services encompassing feasibility studies, site selection, compliance assessments, setup, import permits, project oversight, and reporting. These services are crucial for ensuring that clinical trial innovation for devices is conducted efficiently and in accordance with regulatory requirements, ultimately aiding in the successful development of medical devices.
Wearable devices and telehealth platforms are also pivotal in enabling remote monitoring, streamlining data collection from participants and encouraging ongoing engagement throughout the study. The emergence of wearable technology in research studies exemplifies clinical trial innovation for devices, resulting in innovative methods for data collection that allow ongoing health monitoring and provide a wealth of real-time information to guide study results.
As the sector progresses, the acceptance of fundamental outcome sets across diverse research designs is expected to become standard practice, further improving the quality and comparability of medical research. By 2025, research sponsors are anticipated to adhere to a fundamental outcome framework, emphasizing the importance of clinical trial innovation for devices, as it incorporates technology into medical evaluations, enhances efficiency, and aligns with the evolving expectations of research sponsors and regulatory organizations.
Moreover, the influence of Medtech research extends beyond the studies themselves, contributing to local economies through job creation, economic growth, and healthcare enhancement. The merging of AI and wearable technology is poised to drive clinical trial innovation for devices, transforming research methodologies and enhancing their efficiency and responsiveness to the needs of both researchers and participants. Furthermore, events concerning infectious disease research trends and insights, set for March 17-19, 2025, in Milan, Italy, underscore the continuous evolution and emphasis within the industry.
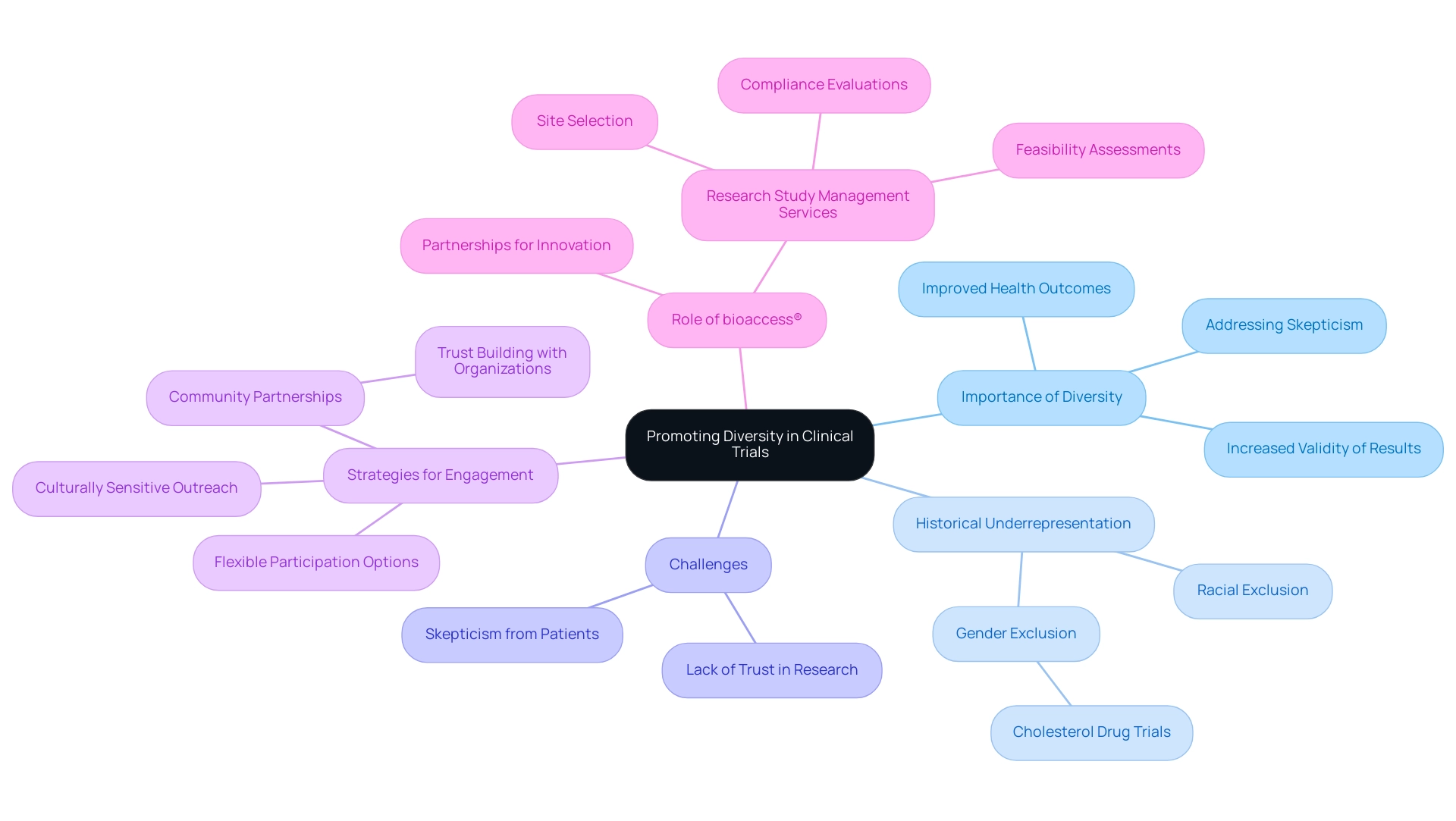
Promoting Diversity in Clinical Trials: A Path to Better Outcomes
Variety in research studies is essential for guaranteeing that medical devices are both safe and effective for all groups. Historically, certain demographic groups have been underrepresented in clinical research, resulting in significant gaps in understanding how various populations respond to treatments. For instance, initial trials for cholesterol-lowering medications predominantly involved male participants, raising concerns about their efficacy in women and other demographics.
This lack of representation has not only led to skepticism among individuals but has also underscored the necessity for inclusive research practices. As observed by Matthew Herper, "Scientists have concentrated on the issue of diversity in research studies both because lacking a varied population can lead to skepticism from patients who could benefit from medicines and because some drugs do function differently in individuals of different backgrounds."
To promote diversity, researchers must adopt targeted recruitment strategies that actively engage underrepresented communities. Effective approaches include:
- Forming partnerships with community organizations that have established trust within these populations
- Implementing culturally sensitive outreach efforts
- Offering flexible participation options that cater to diverse needs
For instance, utilizing local health fairs or community events can enhance visibility and encourage participation from groups that may otherwise feel excluded from research.
The significance of variety in medical studies cannot be emphasized enough, particularly in 2025, as the healthcare community increasingly acknowledges that treatments may have different effects based on demographic factors. Statistics suggest that varied research studies produce more extensive data, representing real-world experiences and ultimately resulting in improved health outcomes. By promoting diversity, health studies can not only improve the validity of their results but also ensure that clinical trial innovation for devices addresses the needs of all patients, paving the way for innovations that genuinely benefit society.
bioaccess®, boasting more than 20 years of expertise in the Medtech sector, plays a crucial role in connecting innovative medtech firms with opportunities for carrying out research projects in Latin America. Through comprehensive research study management services—including feasibility assessments, site selection, compliance evaluations, study setup, import permits, project management, and reporting—bioaccess® is committed to promoting diversity and innovation in research. Moreover, the partnership between bioaccess® and Caribbean Health Group seeks to establish Barranquilla as a prominent location for medical studies in Latin America, backed by Colombia's Minister of Health, improving the environment for medical research in the area.
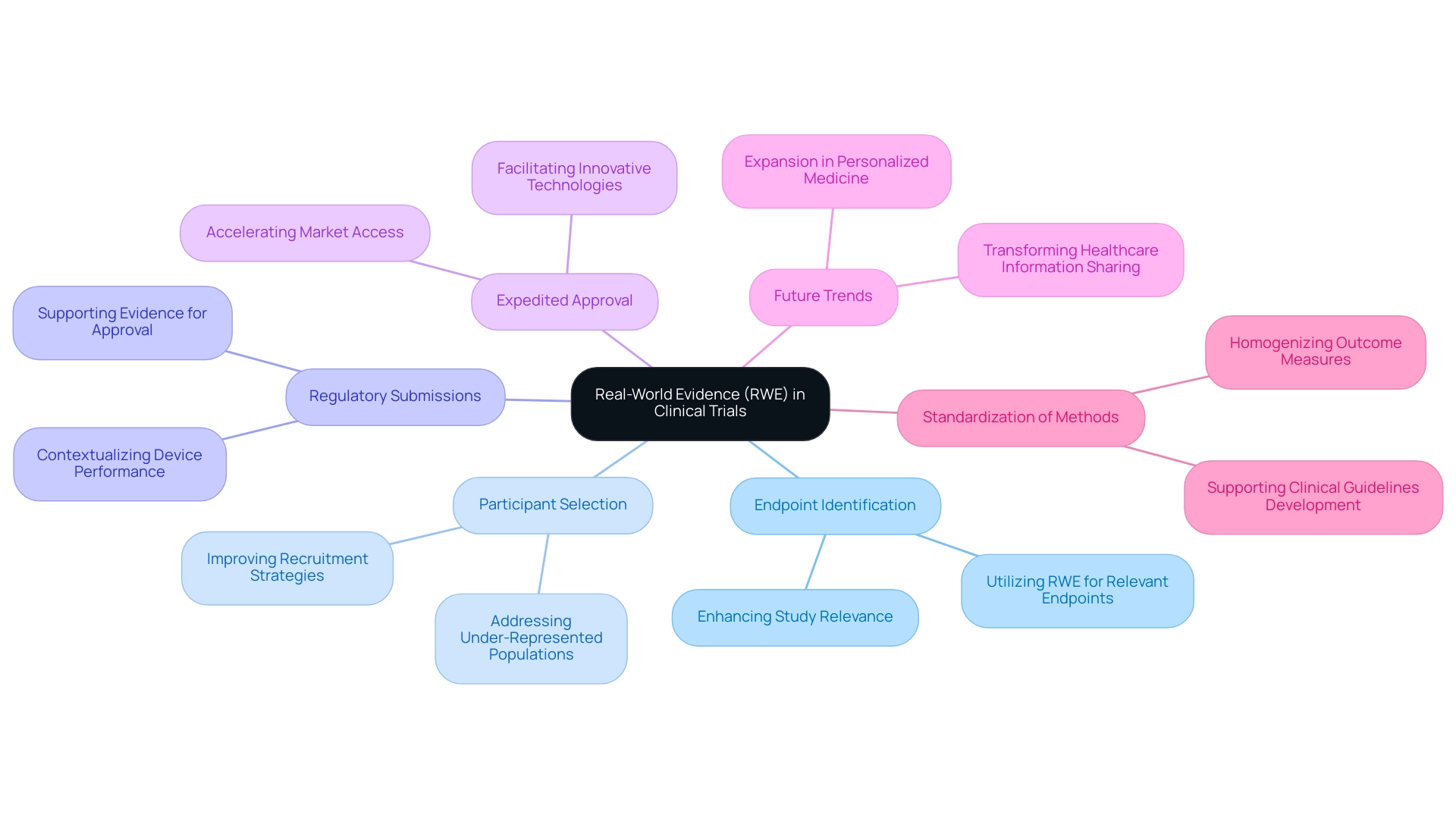
Utilizing Real-World Evidence to Inform Clinical Trial Design
Real-world evidence (RWE) is increasingly recognized as a pivotal asset in the design of medical device studies. By utilizing information obtained from regular medical practice, researchers can uncover essential insights into individual demographics, treatment trends, and outcomes, thereby enhancing the significance and applicability of studies. The incorporation of RWE into clinical trial innovation for devices not only aids in identifying appropriate endpoints but also improves participant selection, ultimately enhancing the feasibility and efficiency of research.
Moreover, RWE plays a crucial role in supporting regulatory submissions by providing additional context and evidence regarding a device's performance in real-world environments. This approach can significantly expedite the approval process for innovative medical technologies through clinical trial innovation for devices, facilitating quicker market access. As the landscape of medical research evolves, the utilization of RWE is expected to expand, particularly in tailoring medical treatments to meet individual patient needs and addressing under-represented populations in research.
The case analysis titled "Future of Real-World Data in Personalized Medicine" underscores this anticipated expansion, emphasizing the role of RWD and RWE in informing policymaking and health system planning. Additionally, democratizing access to medical knowledge through RWE could transform healthcare information sharing and utilization, paving the way for advancements in personalized medicine. As noted by Peng Lu, chief medical officer of Dutch biotech Pharvaris, "Standardizing the application of specific results and outcome metrics for trials will aid in the development of treatment guidelines and future indirect comparisons among interventions." This highlights the significance of standardized methods in medical research.
bioaccess® provides extensive management services for studies, including pilot studies, first-in-human studies, early-feasibility studies, pivotal studies, and post-market follow-up studies. By bridging the gap between innovative medtech firms and research opportunities in Latin America, bioaccess® aligns with the industry's requirements and showcases the transformative potential of RWE in the context of clinical trial innovation for devices.
Strategies for Effective Recruitment and Retention in Trials
Effective recruitment and retention strategies are essential for the success of clinical trial innovation for devices, particularly in the rapidly evolving landscape of medical devices. To optimize recruitment efforts, researchers must craft clear and compelling messaging that articulates the benefits of participation, ensuring potential subjects understand the value they bring to the study. By 2025, utilizing digital platforms for recruitment has become indispensable in the age of technology, facilitating broader outreach and engagement with diverse populations.
This method not only enhances visibility but also aids in identifying appropriate candidates through focused strategies. As emphasized by Michael Young, 'utilizing data analytics can assist in targeting specific demographics, thus increasing the likelihood of discovering suitable candidates for assessments.'
Once participants are enrolled, maintaining their engagement is crucial for retention. Regular communication is vital; it fosters trust and keeps participants informed about the trial's progress. Personalized support significantly enhances the participant experience, addressing individual needs and concerns.
Additionally, providing incentives for continued participation can motivate subjects to remain engaged throughout the research. Creating a sense of community among participants can further strengthen loyalty and encourage ongoing involvement. Case studies have demonstrated that patient-centered recruitment strategies, which focus on participant needs and preferences, lead to higher enrollment rates. For instance, the partnership between bioaccess® and Caribbean Health Group aims to establish Barranquilla as a premier location for medical studies in Latin America, supported by Colombia's Minister of Health.
This initiative seeks to improve research services and enhance recruitment and retention outcomes. Moreover, bioaccess® offers comprehensive services for research studies, including protocol creation, data delivery, and site services, all of which assist in effective recruitment and retention strategies. As the medical research environment continues to evolve, implementing clinical trial innovation for devices will be crucial for advancing medical devices and ensuring successful study execution.

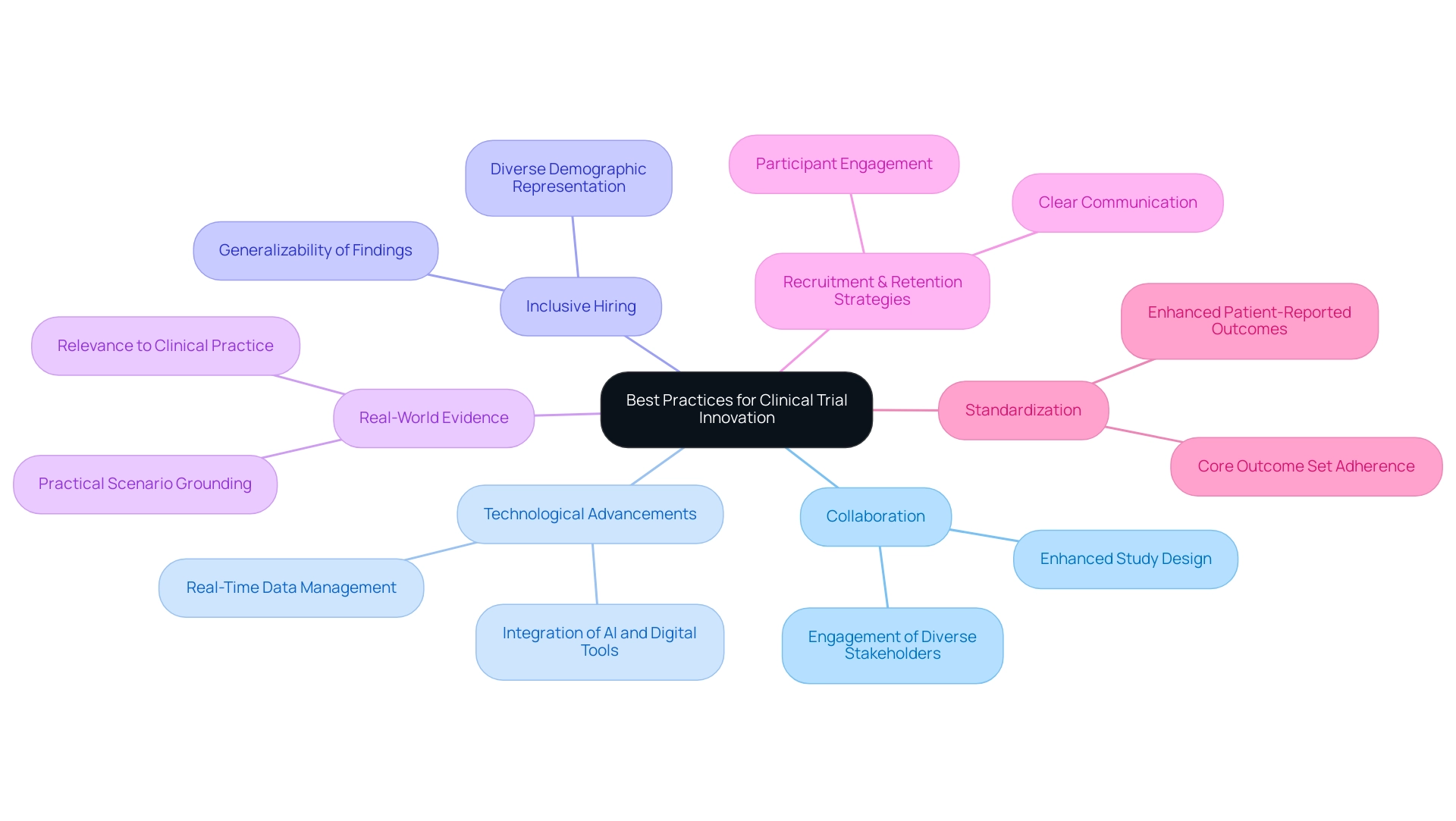
Best Practices for Successful Clinical Trial Innovation
To achieve success in clinical trial innovation for devices, stakeholders must adopt several best practices that are increasingly relevant in 2025. First, fostering collaboration among diverse stakeholders—including researchers, regulatory bodies, and patient advocacy groups—can significantly enhance study design and execution. This collaborative method not only streamlines processes but also enriches the experience with varied perspectives, ultimately leading to more robust outcomes.
Embracing technological advancements is another critical strategy. The integration of artificial intelligence and digital health tools can optimize data management and improve operational efficiency. These technologies enable real-time data gathering and analysis, permitting faster modifications to protocols as necessary.
Variety in hiring initiatives is crucial to guarantee that study outcomes are relevant to a wide range of individuals. By prioritizing inclusivity, researchers can gather data that reflects the experiences of various demographic groups, enhancing the generalizability of findings.
Utilizing real-world evidence is also essential in informing study design. This approach helps to ground clinical research in practical scenarios, making the findings more relevant to everyday clinical practice and patient care.
Moreover, implementing effective recruitment and retention strategies is crucial for maintaining participant engagement throughout the study. Engaging participants through clear communication and support can lead to higher retention rates, which is essential for the integrity of the research.
In 2025, study sponsors are expected to adhere to a core outcome set across different study designs, highlighting the significance of standardization in medical research. Moreover, progress in assessing health study results, especially through enhanced patient-reported outcomes and biomarker identification, is anticipated to improve the evaluation of new therapies.
As Max Baumann notes, "We expect continued focus on optimizing the development journeys of assets to achieve not only an approval-enabling endpoint but to qualify for commercial success." This focus is essential in an increasingly crowded healthcare market. By following these best practices, researchers can significantly improve the efficiency and effectiveness of medical studies, ultimately resulting in better patient outcomes.
Moreover, bioaccess's extensive management services for studies—including feasibility analyses, site selection, compliance assessments, setup, import permits, project oversight, reporting on significant and minor adverse events, and review and feedback on research documents—play a crucial role in advancing successful research initiatives. Additionally, many biotechnology companies are conducting early phase clinical trials in Australia to leverage its regulatory advantages, highlighting the geographical considerations in clinical trial innovation for devices and the potential for job creation and economic growth in local economies.
Conclusion
The evolving landscape of clinical trials in the MedTech sector is characterized by significant innovation and collaboration, essential for addressing the unique challenges inherent in medical device research. The adoption of adaptive trial designs and the integration of artificial intelligence streamline processes, enhance patient engagement, and ultimately lead to more efficient and effective studies. Moreover, collaboration among stakeholders—sponsors, CROs, and patient advocacy groups—proves vital for successful trial execution and improved patient outcomes.
Promoting diversity in clinical trials emerges as a critical aspect that warrants attention. By ensuring trials are inclusive and representative of various demographics, researchers can generate comprehensive data that accurately reflects real-world patient experiences. This focus on diversity not only enhances the validity of findings but also fosters trust among patients, many of whom remain skeptical of treatments lacking representation in clinical research.
As the industry looks toward 2025, leveraging real-world evidence and employing effective recruitment and retention strategies will continue to shape the future of clinical trials. By utilizing innovative technologies and adhering to best practices, stakeholders can adeptly navigate the complexities of medical device research, ensuring advancements in technology translate into tangible benefits for patients and healthcare providers alike. The commitment to innovation, collaboration, and diversity will ultimately drive the success of clinical trials, paving the way for groundbreaking medical devices that enhance health outcomes on a global scale.
Frequently Asked Questions
What drives innovation in the MedTech sector?
Innovation in the MedTech sector is primarily driven by advancements in clinical trial methodologies for devices, including the adoption of cutting-edge strategies and technologies that enhance research study design and execution.
What are adaptive study designs in clinical trials?
Adaptive study designs are methodologies that allow for modifications to the study protocol based on interim results, which accelerates development timelines and increases the likelihood of successful outcomes.
How have inter-trial intervals changed recently?
Inter-trial intervals have decreased to an average of 17 months, down from a peak of 32 months recorded in 2022, indicating improved efficiency in research processes.
What role do AI and machine learning play in clinical trials?
AI and machine learning enhance the adaptability, agility, and cost-effectiveness of research, contributing to the overall innovation in clinical trial methodologies.
How are digital health technologies impacting clinical trials?
The introduction of digital health technologies and decentralized studies is revolutionizing clinical trial innovation, improving patient engagement and data collection, making studies more efficient and patient-centric.
What services does bioaccess® offer in the MedTech sector?
Bioaccess® provides comprehensive research management services, including Early-Feasibility Studies (EFS), First-In-Human Studies (FIH), Pilot Studies, Pivotal Studies, and Post-Market Medical Follow-Up Studies (PMCF).
What is the significance of data ownership and transparency in clinical trials?
Enhanced data ownership and transparency among sponsors encourages better control over data management, leading to improved study quality and outcomes for patients.
Why is cooperation among stakeholders important in MedTech studies?
Cooperation among sponsors, research organizations, regulatory bodies, and healthcare providers promotes better research designs, boosts participant recruitment, and simplifies regulatory procedures, speeding up the market journey for medical devices.
Can you provide an example of successful collaboration in the MedTech sector?
An example is the partnership between bioaccess™ and Caribbean Health Group (CHG), which aims to establish Barranquilla as a premier research location in Latin America, supported by Colombia's Minister of Health.
How do advocacy groups contribute to clinical trials?
Advocacy groups provide insights into patient needs and preferences, guiding study design and improving participant recruitment and retention rates.
What is the trend regarding collaborative studies in MedTech?
By 2025, over 60% of MedTech companies are expected to engage in collaborative studies, reflecting a shift towards integrated approaches in research.
What upcoming events highlight the significance of collaboration in clinical trials?
Upcoming events related to infectious disease studies will be held at Sands Expo & Convention Centre in Singapore and in Milan, Italy from March 17-19, 2025, emphasizing ongoing collaboration in the sector.
How do strategic alliances enhance medical research efficiency?
Strategic alliances, such as those involving bioaccess®, can bridge gaps in medical research, particularly in underutilized areas like Latin America, improving overall research study efficiency and effectiveness.

