Introduction
The integration of technology in clinical trials for medical devices is revolutionizing the field of medical research and product development. With advancements such as real-time data collection, remote patient monitoring, and sophisticated algorithms, the efficiency and effectiveness of clinical trials are being enhanced. These technological innovations not only streamline the trial process but also pave the way for faster and more reliable outcomes.
Furthermore, regulatory bodies like the FDA and EMA are recognizing the importance of technology in improving data accuracy and patient safety. As the industry continues to evolve, it is crucial to leverage these advancements to achieve smarter and patient-centered drug development. In this article, we will explore the key trends in clinical trial evolution, the impact of artificial intelligence and machine learning, the integration of real-world evidence, and the rise of precision medicine and personalized therapies.
Additionally, we will discuss the need for regulatory flexibility and the future directions of clinical trials in the ever-changing landscape of medical technology.
The Role of Technology in Shaping Clinical Trials
The field of medical device experiments is experiencing a noteworthy change, prompted by the fusion of digital health and MedTech advancements. With the arrival of real-time data collection, remote patient monitoring, and improved patient engagement tools, there is a noticeable shift towards streamlining the clinical experimentation process. These advancements not only improve the efficiency and effectiveness of legal proceedings but also pave the way for swifter, more reliable outcomes.
The development of sophisticated algorithms, such as the Hierarchical Interaction Network (HINT) by the lab of computer scientist Jimeng Sun at the University of Illinois Urbana-Champaign, exemplifies this shift. HINT, and its subsequent iteration, SPOT (Sequential Predictive Modelling of Clinical Trial Outcome), leverage predictive analytics to forecast study success, thereby informing potential modifications to study designs or therapeutic strategies. These tools emphasize the potential of technology to optimize methodologies for testing new drugs, a significant consideration given the increasing complexity and cost of the drug development process over time, as highlighted by Eroom's law.
The regulatory landscape, with entities like the FDA in the US and EMA in Europe, underscores the categorization and oversight of healthcare instruments based on their associated risks. Technologies that aid the trial process, like wearable tools and electronic health records, are crucial in improving data accuracy and patient safety. This is crucial in the context of high-risk class three healthcare instruments, which constitute a small but crucial segment of FDA-regulated tools, requiring rigorous approval procedures.
Furthermore, companies like Cardiawave are making progress in research funding and regulatory preparation, demonstrated by their Series B financing round aimed at enabling marketing in Europe and supporting studies in the US. The Biden administration's comprehensive rules on AI regulation and ongoing discussions in the European Parliament about the AI Act highlight the evolving governance of technology, with a focus on ethical, legal, and social implications, as well as market and intellectual property factors.
In summary, it is clear that the incorporation of technology in experiments for healthcare equipment is not only improving the productivity and success of these experiments but also transforming the general method to healthcare investigation and product advancement. As the industry moves forward, it is crucial to leverage these technological advancements to achieve smarter, patient-centered drug development, with a strategic emphasis on data management and insight extraction.
Key Trends in Clinical Trial Evolution
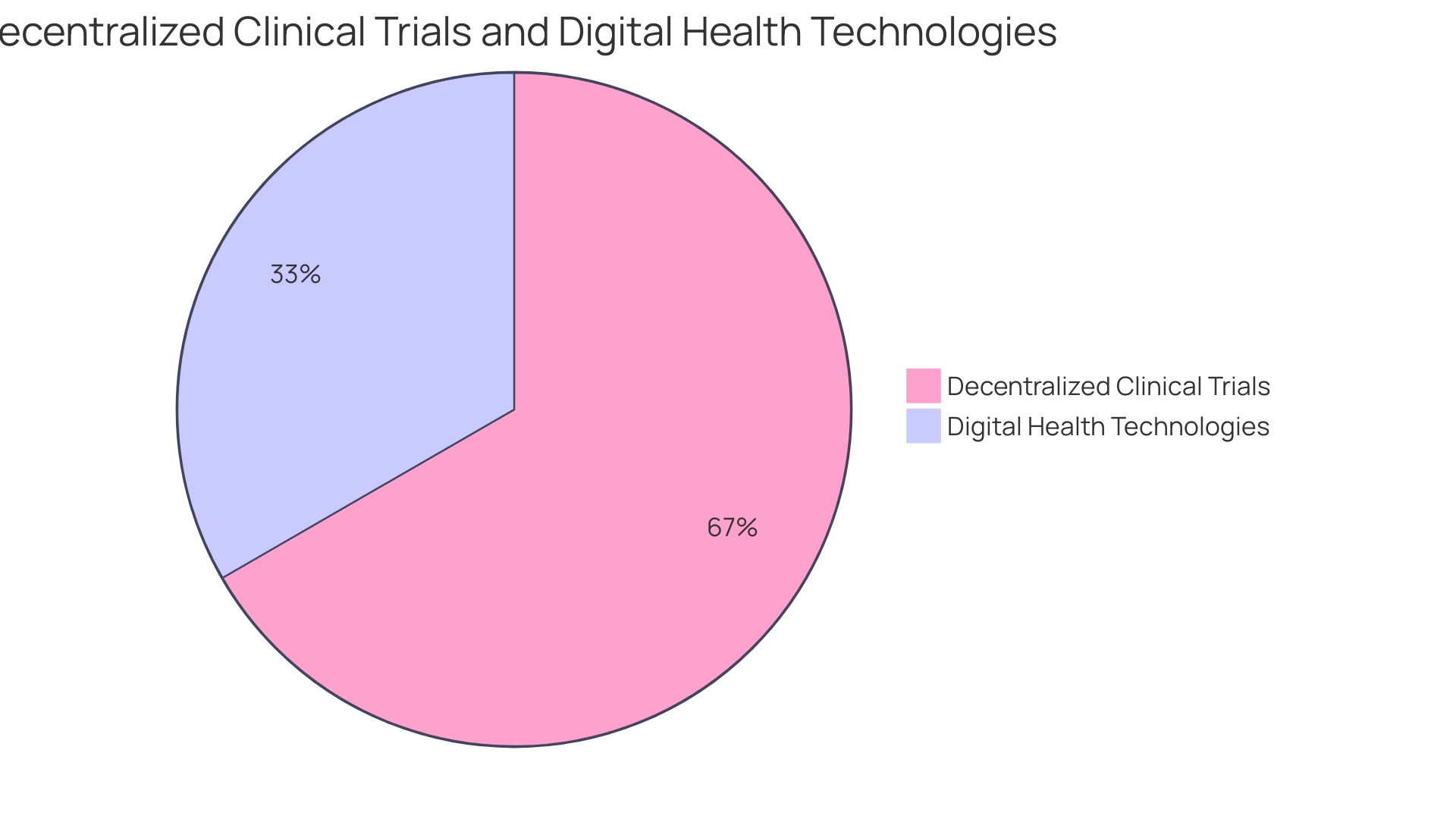
Decentralized research studies (DCTs) are transforming the landscape of medical device research by bringing study activities closer to participants' lives. These experiments utilize digital health technologies (DHTs) like activity trackers, glucose monitors, blood pressure monitors, and spirometers to gather data remotely. The versatility of carrying out some or all experiment activities outside customary research locations, including participants' homes or local healthcare facilities, is a feature of DCTs that is especially revolutionary. The use of DHTs in DCTs not only facilitates a more inclusive participant pool by simplifying access for a diverse group of participants but also aligns with the rising trend of digital therapeutics in managing chronic and neurological diseases. Despite their potential, DCTs face challenges like regulatory uncertainty and the need for standardization. Nonetheless, the sector is poised for substantial growth, with the market expected to expand at a compound annual growth rate of 30.1% through 2026. This expansion highlights the sector's dedication to improving patient availability and prioritizing diversity in medical studies, as echoed by executives at important industry events.
The Impact of Artificial Intelligence and Machine Learning
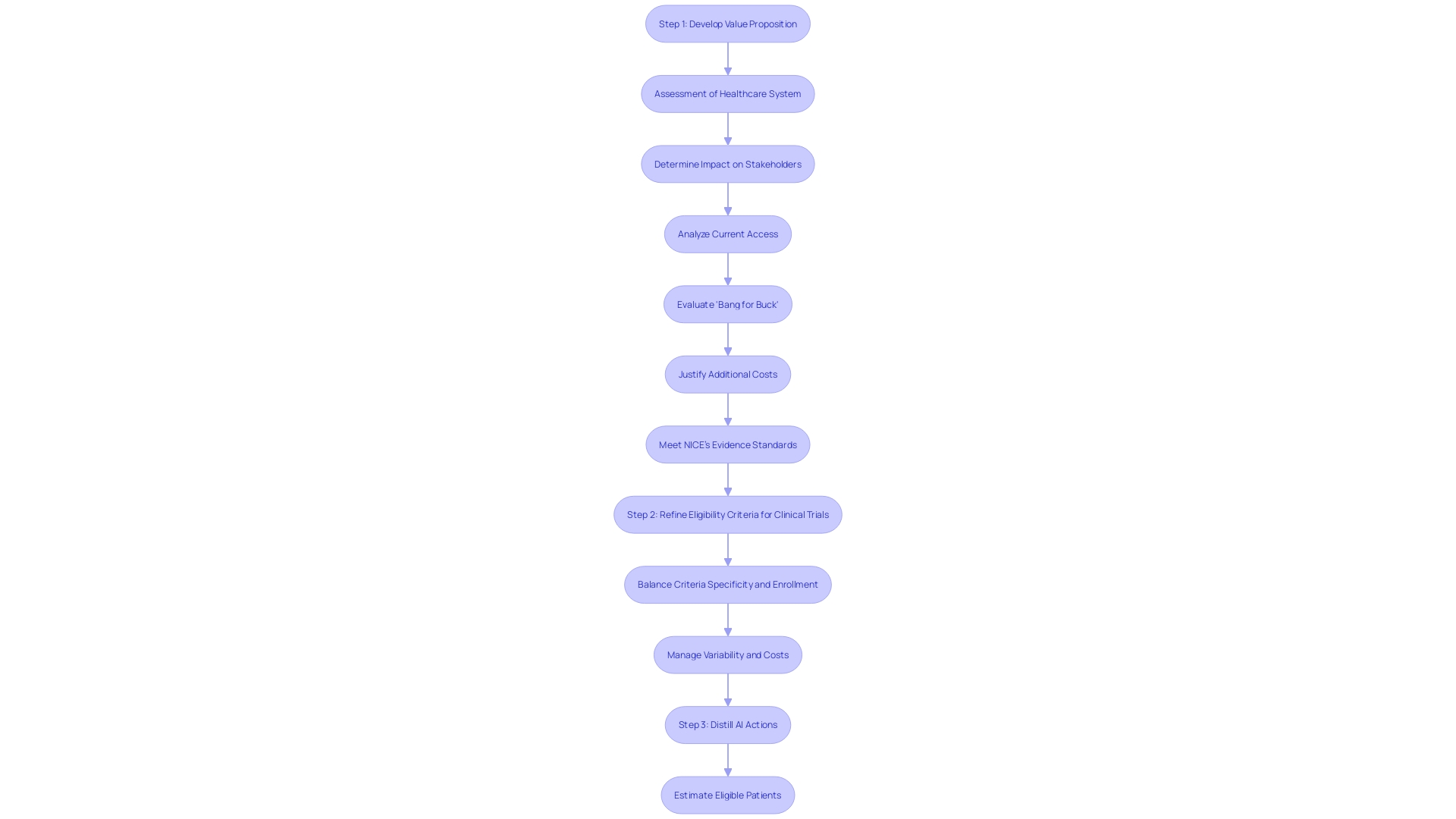
The development and implementation of machine learning/artificial intelligence devices (Names) follow a pathway akin to new drug commercialization, requiring lab development, exhaustive safety and efficacy testing, and the endorsements of healthcare professionals and insurers. Despite the allure of their technological prowess, the real measure of MAMD success hinges on their ability to meet high commercial standards, mirroring the stringent requirements faced by new pharmaceuticals. As discussed by a research team from the University of Illinois, the transformative potential of AI extends to the optimization of experiments, where algorithms like HINT and SPOT can forecast test outcomes and inform more strategic designs. Moreover, the Food and Drug Administration (FDA) underscores its commitment to public health by ensuring the integration of AI into healthcare products meets the highest standards of safety, efficacy, and security. The FDA's informational resources serve as a portal to understanding Ai's role in healthcare, thus shaping its future through responsible innovation. In areas such as the UK, where healthcare systems may impose higher evidence thresholds, the motivation for thorough examinations of AI products is even stronger, providing a glimpse into the diverse landscape of AI in medicine.
Real-World Evidence in Clinical Trials
The incorporation of Real-World Evidence (RWE) in the realm of medical investigations for medical instruments is a crucial advancement, utilizing data from real patient care to improve our comprehension of instrument performance. This change towards RWE is not simply a fad but a revolutionary movement in the domain, with experts like Chris, a biomedical engineer with 13 years' experience in Class III apparatus studies, leading the way. His work at Greenlight Guru exemplifies the industry's commitment to leveraging RWE for deeper insights.
The potential of RWE is evident, as it offers a comprehensive view of patient health by capturing data from various sources under real-world conditions, which differs significantly from controlled clinical trials. Embracing this approach allows for a nuanced understanding of patient responses and behaviors, and how these factors impact health outcomes. Moreover, it aids in monitoring therapy responses and identifying potential adverse events, ultimately enhancing R&D efficiencies and accelerating market readiness for new devices.
Regulatory bodies and decision-makers worldwide are recognizing the value of RWE, yet they face the challenge of standardizing diverse research objectives, study designs, and data methodologies. The European Commission, for instance, is prioritizing the European Health Data Space (EHDS) to address data quality, relevance, and interoperability issues. Nonetheless, the utilization of RWE in the EU is hindered by concerns around data privacy, access, fragmentation, and the depth and quality of data sources.
Economic modeling in healthcare is increasingly integrating RWE, thereby refining the precision and realism of these models. This integration is pivotal for evaluating the cost-effectiveness of healthcare decisions, guiding the industry towards more economically sustainable practices.
As we keep observing the rise of sophisticated analytics and digital tools in medicine, experts and stakeholders, including those from Medical Device News Magazine's readership, can expect a more efficient and knowledgeable experiment environment that not only fulfills but surpasses current healthcare demands. The use of RWE is poised to redefine the standard of care, providing a robust foundation for medical device development and assessment.
Precision Medicine and Personalized Therapies
The experimental examination landscape is experiencing a paradigm shift with the integration of precision medicine and individualized therapies, which address the distinct genetic composition, environmental factors, and lifestyle choices of individual patients. This evolution mirrors the automotive industry's concept of "your mileage may vary" (YMMV), acknowledging the variability of standardized test results when applied to individual experiences. Similarly, in clinical trials, the traditional randomized clinical trial (RCT) model, which produces average effects, is being enhanced by personalized approaches that consider each patient's unique profile, moving away from a one-size-fits-all treatment model.
The advent of potent new antitussives for conditions like chronic cough, which affects up to 33% of the population in Europe and the U.S., illustrates the need for tailored therapies. These therapies can potentially alleviate the substantial economic impact on healthcare systems and improve patient quality of life. Healthcare equipment plays a crucial role in this transition, with governing organizations like the FDA in the United States and the EMA in Europe classifying tools according to their potential risks and simplifying the authorization procedures for those that target unaddressed healthcare requirements.
The FDA evaluates medical devices for safety and effectiveness, but coverage decisions by payors can delay patient access to approved devices. The requirement for effectiveness and swiftness in the development of medical studies has never been more crucial, as up to 80% of assessments do not finish on schedule, and the competition to release in the market is intensified by competitive pressures and legislative changes like the US Inflation Reduction Act.
In cancer care, for instance, wearable monitoring technologies provide real-time, personalized data, revolutionizing patient management and treatment efficacy. These advancements highlight the transformation of healthcare delivery and clinical research, as proven by the trends in new drug launches, clinical investigation starts, and R&D funding, which continue to demonstrate the industry's dedication to innovation and patient-centric care.
Regulatory Flexibility and Future Directions
With the rapid evolution of digital health and healthcare technology, regulatory bodies like the FDA recognize the imperative for adaptable regulatory frameworks. These are essential for integrating innovative trial designs and technologies while upholding the paramount importance of patient safety and device effectiveness. The FDA has emphasized the importance of effective, well-designed research in its public health mission, recognizing that strong studies and reliable data are fundamental to informed decision-making regarding medical products. Efforts are underway to streamline clinical research by aligning FDA's human subject protection regulations with the HHS Common Rule, thereby enhancing research efficiency and participant safeguards.
Medical equipment manufacturers, navigating a landscape of traditional practices and regulatory hurdles, often mirror strategies of disruptive innovators like Uber and Lyft—pioneering new business models to create market demand and navigate regulatory processes. This method, while possibly expediting innovation, raises concerns about the rapid implementation of new treatments or technology without enough evidence. The FDA's dedication to evidence generation for product safety and effectiveness is a testament to balancing innovation with patient protection.
The agency's role extends to evaluating the safety and effectiveness of equipment for medical purposes, with subsequent coverage and usage decisions falling to payors and healthcare providers. The data required by these parties may differ from that submitted to the FDA, potentially resulting in coverage delays or denials post-approval. Since the range of devices in the healthcare field spans from low-risk class one to high-risk class three, with the latter necessitating more thorough regulatory examination, the implications for patient access and the adoption of medical technologies become increasingly complex.
In this dynamic environment, the future of clinical trials is shaped by a collaborative effort among the FDA, researchers, and industry stakeholders to ensure that the introduction of novel medical devices into the healthcare system is both safe and effective, reflecting a commitment to advancing medical innovation responsibly.
Conclusion
In conclusion, the integration of technology in clinical trials for medical devices is revolutionizing medical research and product development. Real-time data collection, remote patient monitoring, and sophisticated algorithms are enhancing trial efficiency and reliability. Regulatory bodies like the FDA and EMA recognize the importance of technology in improving data accuracy and patient safety.
Key trends include decentralized clinical trials (DCTs) using digital health technologies for remote data collection. Artificial intelligence and machine learning optimize trial outcomes and inform strategic designs. Real-world evidence (RWE) enhances understanding of device performance through data from actual patient care.
Precision medicine and personalized therapies address individual patient characteristics, reshaping the landscape. Regulatory flexibility is crucial in adapting to the rapid evolution of digital health and medical technology.
To achieve smarter and patient-centered drug development, leveraging these advancements is essential. Collaboration among regulatory bodies, researchers, and industry stakeholders is crucial for the safe and effective introduction of novel medical devices. Embracing technology, data management, and insight extraction will drive innovation and improve patient outcomes in medical research and product development.




