Introduction
The Importance of Post-Market Clinical Follow-Up Studies
Post-market clinical follow-up (PMCF) studies play a crucial role in evaluating the real-world application of medical devices. While devices undergo rigorous evaluation for FDA approval, their full performance spectrum is often only realized when used by a broader patient population in various clinical settings.
PMCF studies monitor and document adverse reactions or device malfunctions, ensuring patient safety. They also provide crucial data for coverage decisions and help bridge the informational gap between regulatory requirements. This article delves into the types of PMCF studies, the role of clinical evaluations in device safety, best practices for conducting these studies, challenges and limitations, and future directions and trends in Latin America.
The Importance of Post-Market Clinical Follow-Up Studies
The necessity of post-market clinical follow-up (PMCF) studies extends beyond initial approval processes to tackle real-world application issues. For instance, while devices undergo rigorous evaluation for FDA approval, the full spectrum of a device's performance is often only realized when it is used by a broader patient population in various clinical settings.
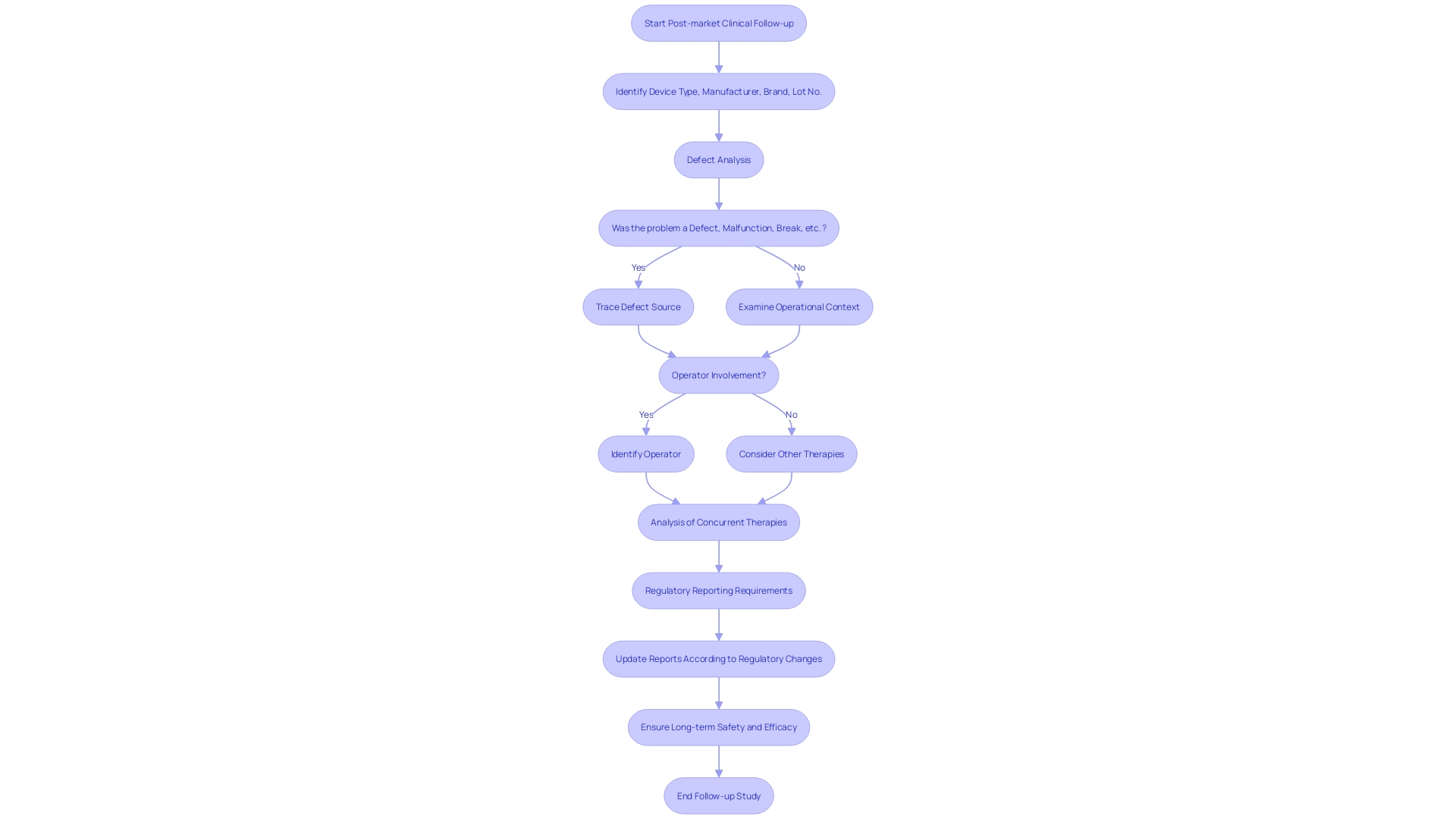
PMCF studies serve as a pivotal mechanism for monitoring and documenting any unanticipated adverse reactions or device malfunctions that could compromise patient safety. These studies are instrumental in updating device-specific information such as type, manufacturer details, brand, and lot numbers, enabling healthcare professionals to swiftly trace and address any product-related complications.
Moreover, PMCF studies provide crucial data for coverage decisions by payors. Manufacturers must navigate these requirements and often find that data required by entities like the Centers for Medicare & Medicaid Services (CMS) can differ significantly from that required by the FDA. Hence, comprehensive PMCF data is vital for bridging this informational gap and facilitating timely coverage and usage determinations. Through diligent postmarket reporting of adverse events and product problems, including the specifics of device operation and possible influences of concurrent therapies, the clinical research community contributes to a robust safety surveillance that maximizes patient protection and informs ongoing device utilization in clinical practice.
Types of Post-Market Clinical Follow-Up Studies
To ensure the ongoing safety and efficacy of medical devices post-market, a variety of clinical follow-up studies can be initiated. Prospective cohort studies are essential in this; they track a patient group over a given time to gauge device performance and safety. Complementarily, retrospective studies delve into historical patient records to draw long-term outcomes.
Additionally, registry studies are instrumental; they leverage patient data collated in device-specific registries to yield insights into safety and efficacy over extensive periods. Finally, post-approval studies, frequently mandated by regulatory bodies, are imperative for real-world monitoring of approved devices. Understanding device classification is crucial as it influences both risk assessment and the study selection—be it 510(k), PMA, or De Novo pathways.
Furthermore, when incidents arise, detailed information regarding device type, manufacturer, issues encountered, and context of device operation must be meticulously documented. Such postmarket reporting can reveal adverse events or operational errors, which are informative for subsequent clinical follow-ups. The FDA's pivotal role in assessing device safety pre-market contrasts with post-market considerations by payers and providers, often relying on additional post-approval data to inform crucial decisions on coverage and usage.
The Role of Clinical Evaluations in Device Safety
Post-market clinical follow-up studies are an essential component of monitoring medical devices after they have entered the market. These studies offer a structured approach to evaluate the long-term safety and efficacy of devices, ensuring that any emerging risks or complications are identified and addressed.
Through careful analysis of data regarding the device type, manufacturer, brand name, and specific lot numbers, researchers can trace and assess issues such as defects, malfunctions, or breaks. Furthermore, it is critical to consider the operational context during the time of any adverse events, including who was handling the device and other concurrent therapies that might have influenced patient outcomes.
With the rapid advancement in medical device technology, it is more important than ever to maintain rigorous post-market oversight. Regulatory authorities continue to heighten requirements to align with such innovations, demanding diligent reporting of adverse events, use errors, and product problems to protect public health. These regulatory updates shape an ever-changing landscape that industry stakeholders must navigate to not only comply with safety standards but also to stay competitive in the fast-paced medical device sector.
Best Practices for Conducting Post-Market Clinical Follow-Up Studies
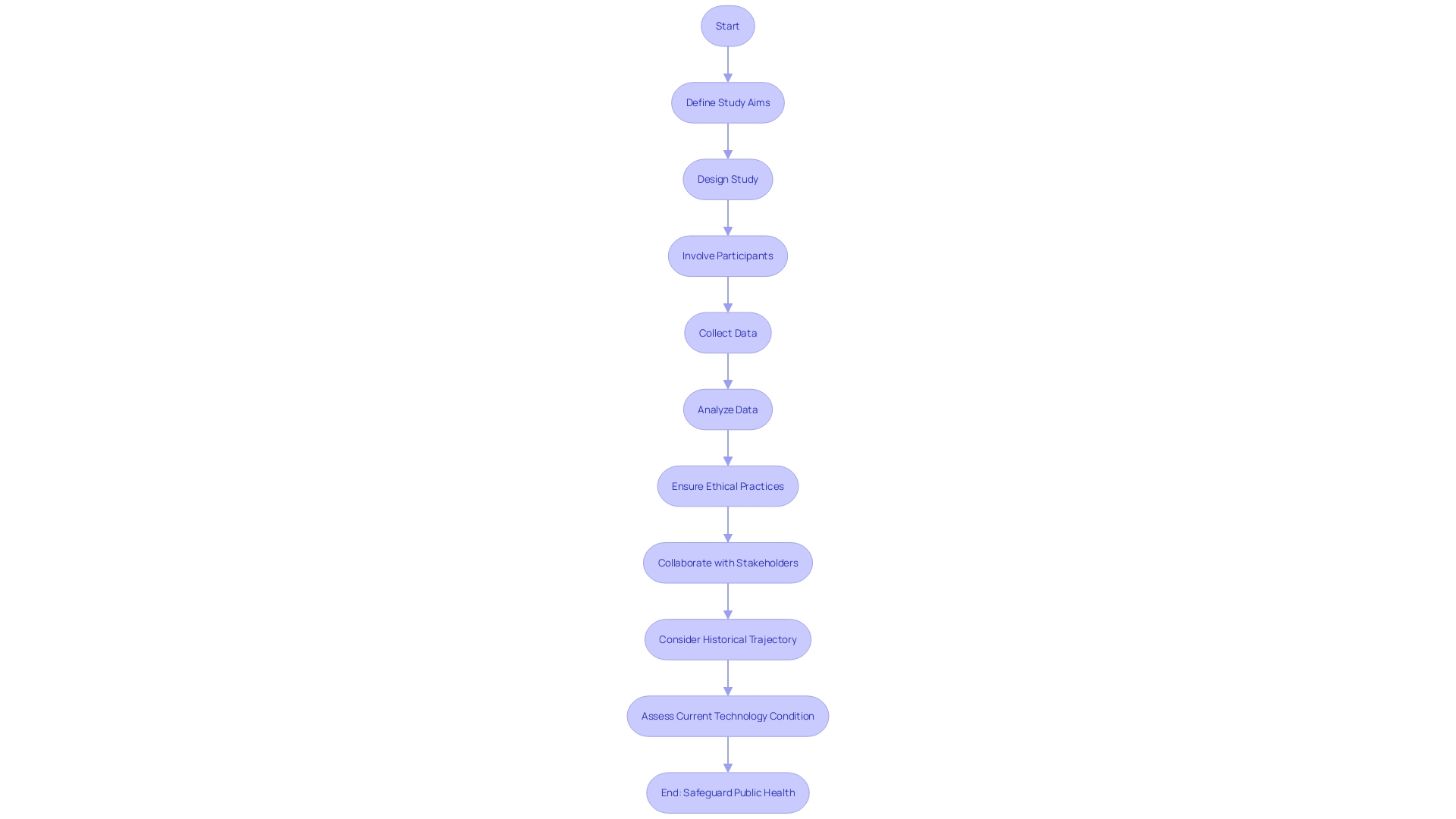
For efficacious post-market clinical follow-up studies in Latin America, a comprehensive approach is indispensable. Key elements include setting distinct study aims to scrutinize specific endpoints and results, coupled with an astute study configuration that mitigates biases or confounding variables, possibly through randomization, blinding, and well-matched control groups.
It is critical to involve an adequate number of participants to yield statistically significant outcomes, supported by stringent data collection and scrupulous analysis methodologies, ensuring findings are precise and trustworthy. Ethical practices must be upstanding, with informed consent from all participants and vigilant protection of their rights and welfare.
It is also crucial to fortify collaboration and dialogue among researchers, regulatory bodies, and other pertinent stakeholders to foster effective and timely sharing of results. The historical trajectory and present condition of technology should be taken into account to comprehend the overarching governance and ethical challenges, ensuring robust, adaptable frameworks that address market and intellectual property influences on the evolution of emerging medical technologies. This overarching multi-faceted strategy guarantees that post-market activities continue to support the safety and effectiveness of medical devices, thereby upholding public health standards and fostering trust in health systems.
Challenges and Limitations of Post-Market Clinical Follow-Up Studies
Post-market clinical follow-up (PMCF) studies serve as a critical component in monitoring the long-term safety and efficacy of medical devices. However, ensuring compliance with study protocols and maintaining the integrity of the data can be quite challenging. For instance, variability in patient adherence to study protocols may introduce data inaccuracies.
Furthermore, patient attrition may lead to the loss of valuable follow-up information, introducing potential bias that could affect the reliability of study results. The extended duration required for PMCF studies also demands substantial resources to monitor device performance over time, which can prove both costly and labor-intensive. The applicability of PMCF findings poses another concern; results may not fully translate to the broader patient population due to possible underrepresentation of certain groups.
This is particularly critical when considering the diversity of patients and healthcare practices in Latin America. Moreover, the resources required to undertake these studies, regarding funding, personnel, and infrastructure, are often substantial, emphasizing the need for strategic planning and efficient resource management. To illustrate these complexities, consider the rigorous development and validation process for machine learning/artificial intelligence medical devices (Names), paralleling new drug market introductions, which mandate steadfast persuasiveness for both clinical adoption and insurance reimbursement.
This approach underscores the importance of not only technological innovation but also practical implementation strategies for PMCF studies. Clear documentation regarding device specifications and incident details, such as type, manufacturer, brand name, lot number, and whether the device was in operation during an adverse event, is imperative. Comprehensive reporting of such incidents aids in fine-tuning protocols and improving the relevance and quality of PMCF studies.
Future Directions and Emerging Trends
As the medical field strides forward, post-market clinical follow-up studies (PMCF) in Latin America play a crucial role in assuring device safety and effectiveness after they reach the market. Emerging trends in PMCF are shaping a future where technology and comprehensive analysis intertwine.
Real-world evidence is increasingly pivotal; it contributes crucial data on device performance in day-to-day healthcare settings, complementing controlled clinical trial data. With the surge in digital health technologies, tools such as wearable devices and health apps are redefining possibilities for data gathering and patient monitoring.
These technologies enable continuous, precise data collection, offering a richer, more granular view of device performance. Collaborative networks across stakeholders are crucial.
These alliances can foster data-sharing and collective expertise, bolstering PMCF studies. By cultivating such partnerships, researchers can navigate ethical, legal, and social issues more effectively, shaping the governance of emerging technologies.
Intellectual property and market incentives are also significant, influencing the trajectory of technology development. Furthermore, the integration of advanced data analytics, including machine learning, into PMCF studies sets the stage for discerning complex patterns within vast datasets, enhancing the speed and accuracy of post-market analysis. Recognizing the importance of patient involvement, the sector is moving towards more patient-centric approaches. Engaging patients in the study design and execution not only enhances participation and data integrity but also ultimately betters patient outcomes. Together, these advancements and trends indicate a proactive approach to PMCF, ensuring medical devices' ongoing safety and efficacy through vigilant, adaptive governance and stakeholder collaboration.
Conclusion
Post-market clinical follow-up (PMCF) studies are essential for evaluating the real-world performance and safety of medical devices. These studies monitor adverse reactions, document device malfunctions, and ensure patient safety.
PMCF studies provide crucial data for coverage decisions, bridge regulatory requirements, and contribute to a robust safety surveillance system. Different types of PMCF studies, including cohort studies, retrospective studies, registry studies, and post-approval studies, offer unique insights into device safety and efficacy.
Clear documentation of device information during adverse events is crucial. To conduct successful PMCF studies in Latin America, a comprehensive approach is necessary.
This includes clear study aims, mitigating biases, involving an adequate number of participants, and ensuring ethical practices. Collaboration among researchers, regulatory bodies, and stakeholders is crucial.
PMCF studies face challenges such as protocol compliance, data integrity, patient adherence, patient attrition, and resource requirements. Strategic planning, efficient resource management, and clear documentation are necessary. Looking towards the future, PMCF studies will benefit from real-world evidence, digital health technologies, collaborative networks, advanced data analytics, and patient-centric approaches. In conclusion, PMCF studies play a vital role in evaluating the real-world performance and safety of medical devices. They provide crucial data, bridge regulatory requirements, and contribute to patient safety. Adherence to best practices, addressing challenges, and embracing emerging trends will enhance the effectiveness of PMCF studies in Latin America and uphold public health standards.




