Introduction
Clinical endpoints play a vital role in medical research, providing essential outcomes to evaluate the impact of treatments and interventions on patients. These endpoints, such as primary, secondary, composite, and safety outcomes, are meticulously measured and recorded to answer specific research questions. Primary endpoints directly address the main question of the study, while secondary endpoints offer additional insights.
Well-defined endpoints are crucial in ensuring the integrity of clinical trials and enhancing patient care. In this article, we will explore the definition and importance of clinical endpoints, the different types of endpoints, the characteristics of effective endpoints, and the process of choosing primary endpoints in clinical trials. Through this informative and professional tone, we will delve into the significance of clinical endpoints in medical research and their impact on patient outcomes.
Definition and Importance of Clinical Endpoints
Clinical outcomes represent the important results monitored in medical studies to evaluate the effect of a treatment or intervention on patients. These measures, which include primary, secondary, composite, and safety outcomes, are meticulously measured, monitored, and recorded to answer specific research questions or aims. The differentiation among these types of outcomes is crucial: primary goals directly tackle the main question of the study, while secondary and other goals offer additional insights into the intervention's effects.
A recent example of the significance of clearly defined objectives is the NOSTONE study, which examined the role of thiazide diuretics in the prevention of kidney stones. In spite of the null findings of the experiment, subsequent analysis indicated potential issues like statistical power, patient selection, and medication adherence as causes for the result. In the same way, the OCEANIC-AF test was praised for its thorough examination of a new medication through carefully planned objectives that aimed to minimize prejudice and concentrated on important results such as survival and stroke rates.
The interpretation of clinical examination results can be challenging, as demonstrated by a study concerning atrial fibrillation and stroke. This study challenged the conventional notion that strokes were closely associated with irregular heart rhythms, highlighting the importance of accurate and appropriate endpoints.
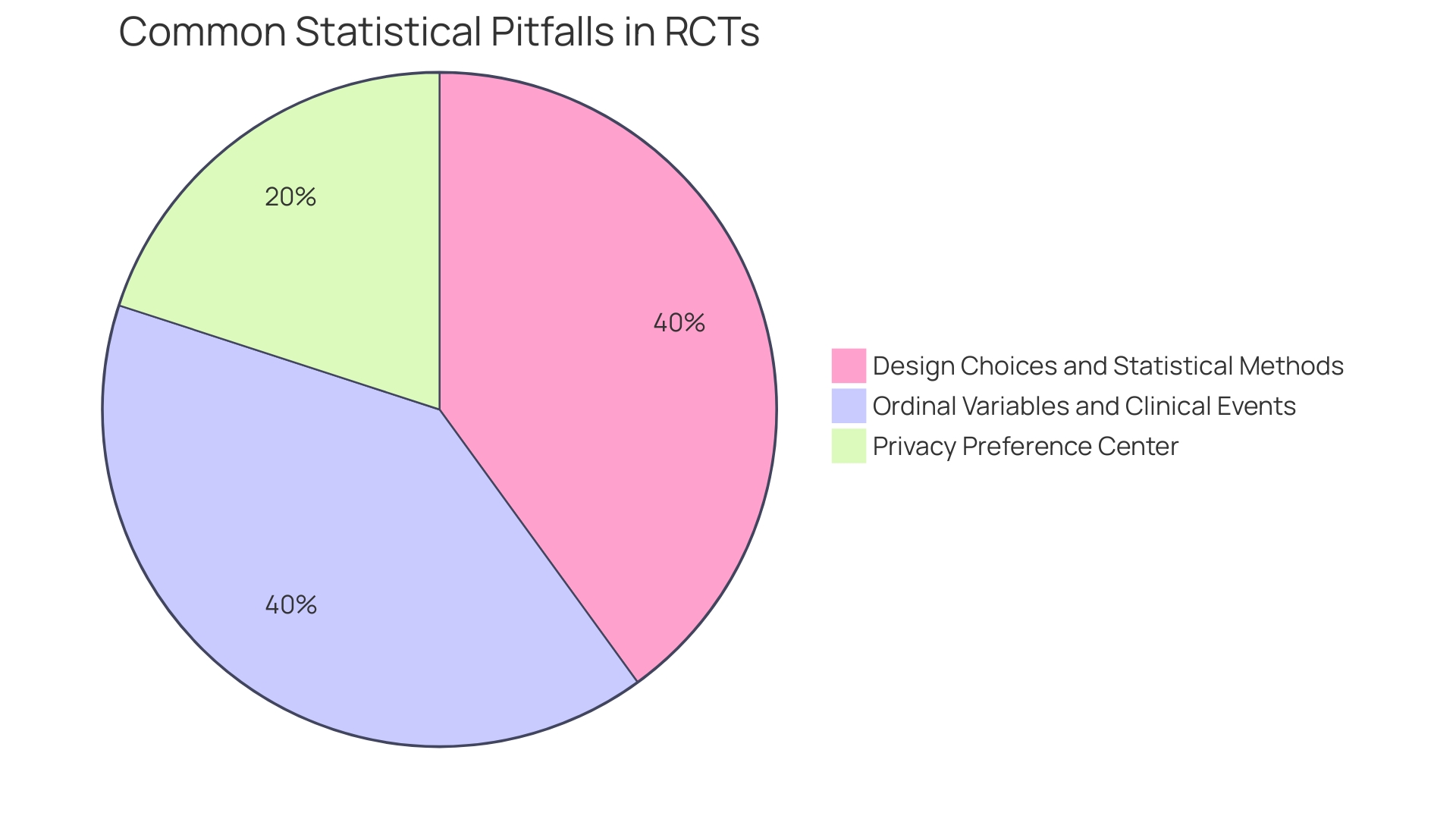
Given the increasing complexity of trials, healthcare professionals may find it challenging to interpret intricate data displays, like survival curves and forest plots. Research indicates that even healthcare providers may not always accurately interpret these complex types of data displays.
Enhancing the design of medical experiments and promoting diversity among participants are crucial measures for equitable and effective medical investigations. WHO has recently offered recommendations to facilitate trials, highlighting the disparities between high-income countries and low- and middle-income countries in terms of trial participation and benefits.
At the core of medical investigation are the patients who willingly take part, often enduring invasive tests and potential side effects. As Osipenko, a leader of a non-profit dedicated to improving the quality of medical studies, notes, these participants are motivated by the hope that their contributions will benefit future generations. Their experiences underscore the profound personal impact of clinical trials and the importance of ensuring that these trials are designed and conducted with the utmost integrity and regard for patient welfare.
Types of Clinical Endpoints
In medical research, the final outcome measures play a crucial role in determining the impact of various interventions on health outcomes. Primary goals are at the forefront of this process, serving as the main outcomes that reflect the direct effects of the interventions on patients. They are selected for their significance in addressing the clinical question posed by the study and their ability to yield definitive answers about the intervention's efficacy.
Secondary outcomes enhance primary goals by offering extra perspectives. They delve into a broader spectrum of the intervention's effects, enriching our understanding of its implications on patient health. These outcomes, while not the primary focus, are instrumental in painting a more complete picture of the intervention's impact.
Surrogate markers, while useful, must be approached with caution. They serve as substitutes for real outcomes and are considered valuable for their predictive abilities regarding the benefits of an intervention. However, the dependence on surrogate indicators necessitates careful consideration, as they may not always align perfectly with the actual clinical results.
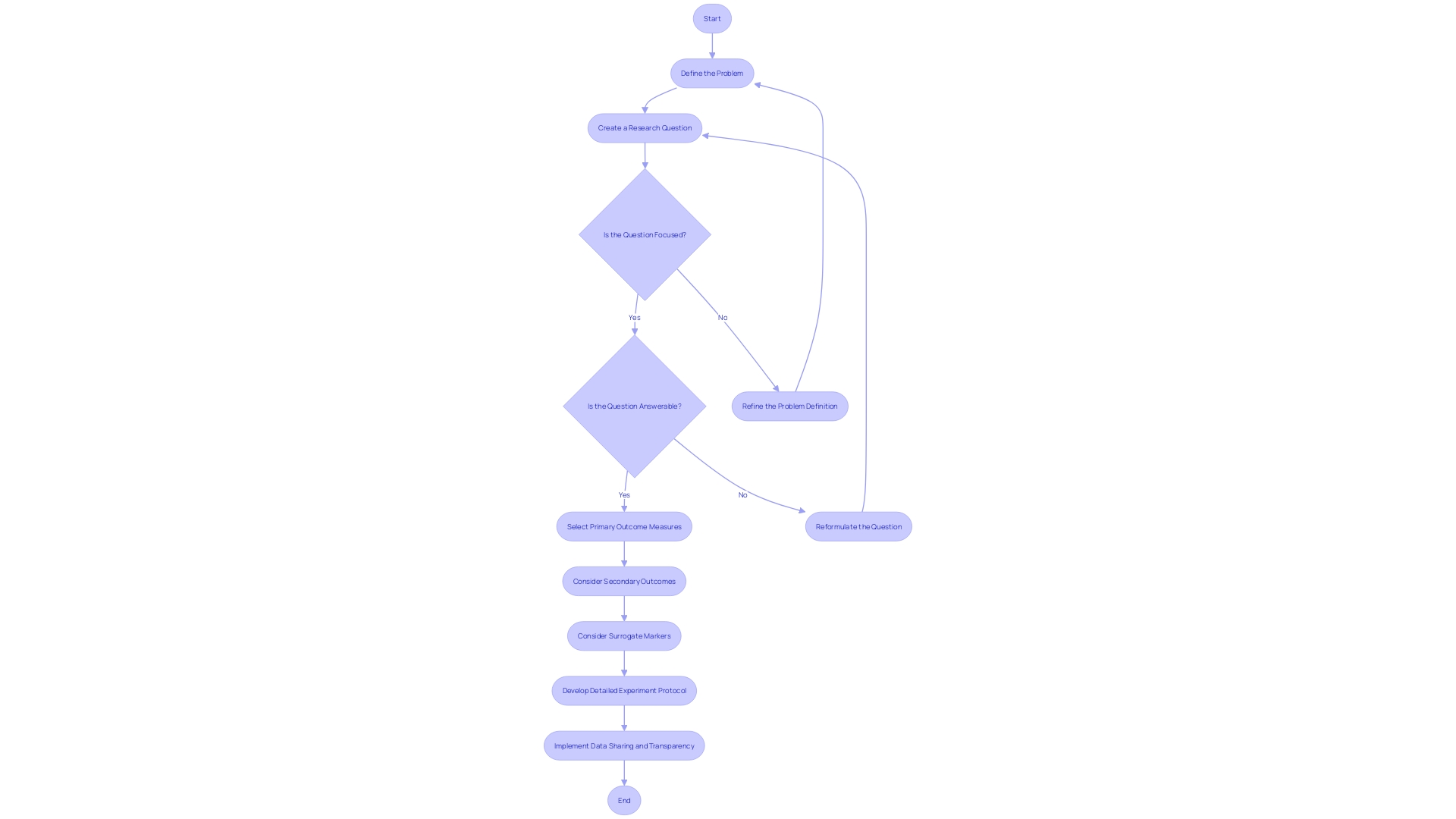
The choice of suitable terminations is a subtle procedure that requires a strong inquiry. As experts recommend, creating a concentrated and answerable question is crucial, and it directs the methodology, including the selection of endpoints. This careful approach guarantees that the results measured are not only significant but also helpful in addressing the central query.
Furthermore, the openness in medical experiments is crucial. The existence of detailed experiment protocols and statistical analysis plans enhances the reproducibility and trustworthiness of the study, yet trials sponsored by the industry often fall short in this aspect. The commitment to data sharing and transparency remains a key issue in the sphere of trials, which is essential for advancing medical knowledge and improving patient care.
Characteristics of Effective Clinical Endpoints
Dependable clinical outcomes are crucial for the success of medical research, influencing both the validity and impact of the findings. These points of measurement, which assess the outcomes of interventions, must be significant, directly linked to the study's hypothesis and the intervention being investigated. They are the cornerstone of patient-centered care, as they gauge the outcomes that matter most to patients and healthcare professionals. The accuracy of these points is equally crucial; they must precisely reflect the intended outcomes. Methods to ensure validity include comparisons with gold standard measures, which serve as benchmarks for evaluation.
Consistency in the measurement of medical outcomes is also crucial, necessitating them to be dependable and repeatable across numerous tests. Test-retest reliability studies are instrumental in confirming this aspect. Moreover, the sensitivity of medical outcomes is vital—they must be capable of detecting even the slightest, yet medically significant, changes caused by the intervention.
Practicality is another consideration, with feasibility playing a role in the selection of termination points. They should be measurable within the study's constraints, straightforward for both patients and researchers to assess, and must not place undue burden on either group.
Considering the recent study on Zilebesiran, which highlighted the medication's capacity to considerably lower blood pressure, the significance of choosing accurate and meaningful outcome measures has been emphasized. By concentrating on the production of angiotensinogen, a protein connected to blood pressure levels, investigators could establish distinct and influential outcomes pertinent to both patient results and the intervention's effectiveness.
The importance of strong medical outcomes goes beyond individual research studies. They form the foundation upon which treatment guidelines are established and influence decision-making processes, such as those conducted by the National Institute for Health and Care Excellence (NICE). Nevertheless, the reliability of evidence from medical experiments often faces examination. It has been observed that, at times, the evidence underpinning drug appraisals may be of poor quality or based on unsuitable comparators. This confirms the necessity for rigorous measures in the choice and verification of medical outcomes to guarantee that new therapies demonstrate genuine advantages for patients.
In an investigation landscape where the integrity of medical trials is paramount, the role of ultimate outcomes as a measure of research excellence cannot be overstated. The Canadian Institutes of Health Research (CIHR) emphasizes the importance of conducting studies that not only achieve scientific excellence but also result in tangible health benefits for all. Therefore, the selection and execution of medical outcomes are crucial in meeting these anticipations and in progressing the research environment as a complete.
Choosing Primary Endpoints
Choosing a main outcome in a clinical examination is a fundamental determination that can greatly impact the result of the study. The main goal must be clinically meaningful, reflecting a direct benefit to patient health. It should be a robust measure that can provide clear statistical power to detect the treatment effect. Sample size and statistical analysis plans are critical in this regard. Additionally, adherence to regulatory guidelines is imperative to ensure the trial's compliance with agencies like the FDA. Ethical considerations are equally important, prioritizing patient safety above all else.
The process of choosing a destination often starts not with a solution, but with a well-defined research question that is both focused and answerable. This approach enables researchers to clearly delineate the population, intervention, comparison, and outcome of interest. For example, in studies involving multiple coronary lesions, the discussion between the effectiveness of multiple stents versus coronary bypass surgery depends on consistent and meaningful selection of the final outcome.
Moreover, the utilization of surrogate markers necessitates thoughtful deliberation. According to the SPIRIT-Surrogate extension guidelines, surrogate measures should improve the transparency and replicability of methods, thus contributing to better patient care and more informed healthcare decisions. Protocols for reporting that use surrogate outcomes as main results should be thorough and transparent to have value.
In conclusion, the selection of a primary endpoint is not merely a procedural step but a crucial determinant of a trial's integrity and its potential impact on patient care and medical practices.
Conclusion
In conclusion, clinical endpoints are essential in medical research. Primary endpoints directly address the main question of the study, while secondary endpoints offer additional insights. Effective endpoints are relevant, valid, reliable, and practical.
The selection of a primary endpoint in a clinical trial is crucial. It should be clinically meaningful, robust, and ethically sound. By choosing appropriate endpoints, researchers can provide accurate and meaningful results that have a significant impact on medical practices and patient outcomes.
In summary, clinical endpoints play a vital role in ensuring the integrity of clinical trials and enhancing patient care. They provide essential outcomes to evaluate the impact of treatments on patients. By selecting and validating endpoints carefully, researchers can contribute to research excellence and improve medical practices.
Improve your clinical trials and enhance patient care with our expert services.




