Introduction
Clinical indications play a vital role in radiology documentation, guiding radiologists in selecting imaging techniques and interpreting results. Efficient workflow management is crucial, and standardized clinical indications can streamline reporting and enhance patient care. Technologies like Sectra's enterprise imaging solution and AI-driven tools offer promising returns on investment, improving operational efficiency.
However, misconceptions in clinical indication documentation can lead to subpar information. Collaborative efforts, precise and compliant records, and efficient documentation processes are key to rectifying these misconceptions. Documenting clinical indications with precision, considering the audience, and incorporating evidence-based practice are essential principles.
The use of specific language, especially in diverse and multilingual landscapes, is crucial for inclusive patient care. The role of ICD-10-CM codes in clinical indications is significant for standardized classification, reimbursement processes, and quality reporting. Real-world case studies highlight strategies for effective clinical indication documentation.
Radiologists and healthcare providers can optimize the process by fostering collaboration, ongoing education, and leveraging advanced technology solutions like AI. Implementing best practices enhances the quality of clinical indication documentation, leading to accurate diagnosis, effective patient care, and financial well-being of healthcare institutions.
Importance of Clinical Indications in Radiology Documentation
In radiology documentation, indications are of utmost importance, serving as the compass that directs radiologists' attention to pertinent areas or conditions. These indications inform the selection of imaging techniques and are pivotal in the interpretation of results. With the vast array of imaging modalities, from X-rays to MRIs and CT scans, radiologists are tasked with deciphering a diverse spectrum of medical data daily. Efficient workflow management becomes essential, particularly in the face of varying rules, data inputs, and the need for data standardization across different facilities. Implementing standardized indications can alleviate workflow impediments, streamline reporting, and enhance IT management, ultimately fostering better patient care.
The advent of innovative technologies such as Sectra's enterprise imaging solution underscores the importance of collaboration and efficiency in radiology workflows. These technologies are instrumental in managing the surge in imaging volumes and offer promising returns on investment (ROI) by improving operational efficiency and diagnostic accuracy. Comprehensive ROI analyses emphasize the tangible and intangible benefits of such investments, including increased revenue, cost savings, and improved staff satisfaction, which contribute to reduced burnout among radiologists. Comprehending and proficiently conveying indications can greatly influence these outcomes, showcasing the wider strategic value they hold within the healthcare system.
Common Misconceptions in Clinical Indication Documentation
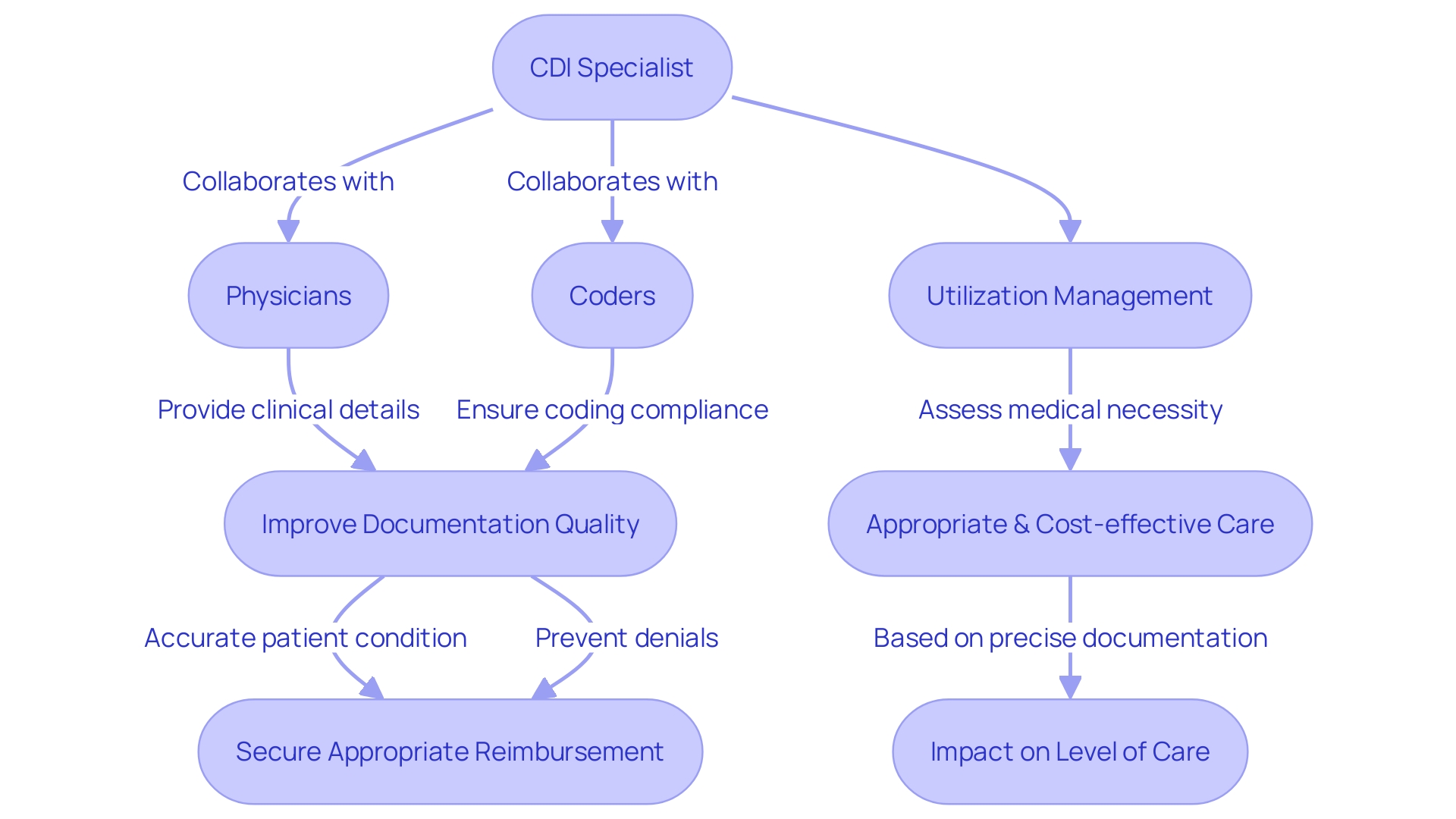
To improve the quality and effectiveness of indication records, it is crucial to correct common misunderstandings that often result in subpar information. Clinical Documentation Improvement (CDI) specialists play a pivotal role in this process by working collaboratively with physicians and coders to create detailed, precise, and compliant records. These experts endeavor to guarantee that the records accurately depict the patient's condition, the level of care given, and the complexity of the case, which is vital for preventing rejections and securing appropriate reimbursement. Meanwhile, utilization management assesses the appropriateness and medical necessity of care services, decisions that are deeply rooted in the accuracy of the documentation.
For instance, Advocate Health, a leader in clinical innovation and outcomes, employs nearly 150,000 team members, including CDI specialists, who face the daunting task of translating complex medical information into clear and comprehensive summaries. This challenge is not unique to large medical organizations. At Summer Health, for instance, medical visit notes have traditionally been a source of frustration, consuming over half of medical care providers' time on administrative tasks and contributing to physician burnout. This highlights the significance of effective documentation processes that save time and alleviate the burden on providers.
According to the 2022 practice brief, which provides updated guidance from its 2019 predecessor, the query process is integral to various healthcare initiatives. This includes reimbursement, data stewardship, collection, quality measures, and prevention of denials. The brief emphasizes the requirement for utilizing indicators and evidence from the health record to support queries and ensure compliance, regardless of whether they are generated by AI technology or other computer-assisted tools.
Moreover, research on medical intervention suitability, which includes thorough approaches like analyzing literature, consulting experts, and abstracting medical records, additionally emphasize the importance of precise record-keeping. These methods, often including meta-analyses, are crucial for determining the appropriateness of indications, which can number in the hundreds for a single intervention.
In summary, through comprehending and tackling the misunderstandings surrounding indication documentation, and by implementing strong CDI processes, providers can enhance documentation quality and outcomes.
Key Principles for Documenting Clinical Indications
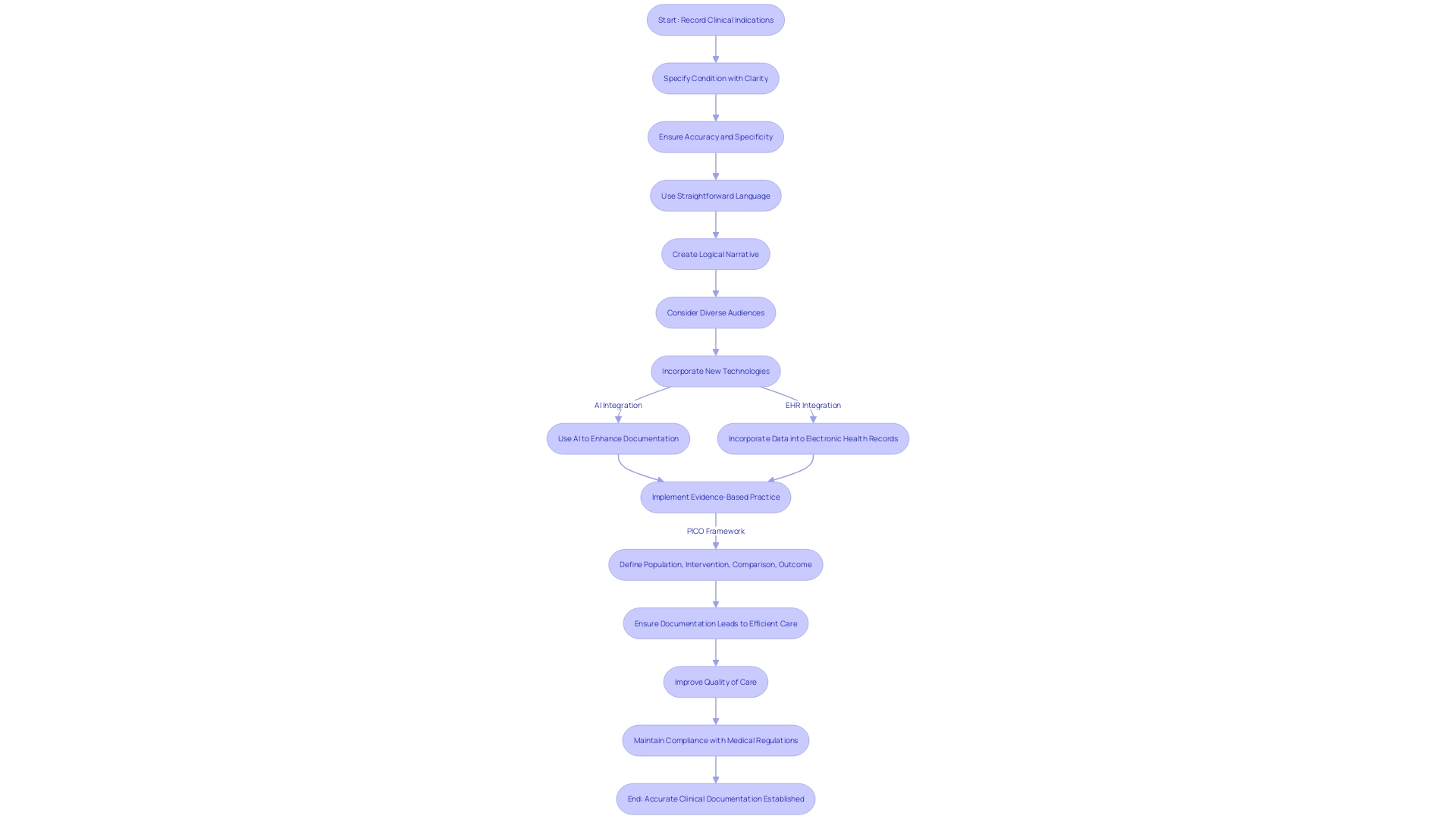
Recording clinical indications with accuracy is vital for facilitating communication among healthcare professionals and delivering the highest level of care. To ensure that these indications fully capture the individual's condition and the intent behind the examination or treatment, it is critical to emphasize specificity, accuracy, and clarity. One must consider the audience, which may include individuals beyond the medical community, such as clients or non-native English speakers. Employing straightforward language and keeping the narrative logical and sequential can significantly enhance the comprehensibility of medical summaries.
Case studies, such as the one involving Summer Health, emphasize the necessity for enhancing medical record-keeping. By converting complex medical shorthand into easily digestible summaries, the burden of administrative tasks can be reduced, leading to better patient care and reducing provider burnout. Such efforts align with the objectives established by the 21st Century Cures Act, highlighting prompt access to clinical records and advocating for patient-centered record-keeping procedures.
In addition, new technologies are changing the landscape of medical documentation. For example, Amazon Web Services has utilized AI to craft content that not only engages the audience but also adheres to accuracy standards, thereby streamlining the content creation process. Similarly, medical organizations are utilizing tools that seamlessly integrate into electronic health records (EHRs), improving the functionality and user experience for providers.
Incorporating evidence-based practice (EBP) is also crucial. It is a systematic method to determine the optimal course of action by taking into account current research, expertise, and individual preferences. By implementing evidence-based practice and utilizing models such as the Johns Hopkins PET process, providers can develop stronger indications based on the PICO framework.
To sum up, thoroughly documented indications are the foundation of efficient care, improvement in quality, and adherence to medical regulations. By implementing transparent, succinct, and person-focused record-keeping methods, healthcare providers can attain improved results, promote individual involvement, and guarantee a more streamlined healthcare system.
Avoiding Ambiguity: The Use of Specific Language
Understanding and accuracy in indication documentation are crucial, especially in diverse and multilingual environments like Southern Nevada, where more than a third of the population communicates in a language other than English. The accurate and specific portrayal of clinical indications is not merely a matter of regulatory compliance, but a crucial component of inclusive care.
The intricacy of conveying medical information to a diverse audience necessitates that medical professionals avoid ambiguous language. For instance, terms such as "prevent" versus "help prevent" have significantly different connotations and implications for patient understanding and expectations. Likewise, medical providers themselves may encounter difficulties in interpreting intricate data displays in prescription drug advertisements, which underscores the importance of simplicity and clarity in communication.
Effective documentation should incorporate the use of concrete terms and the repetition of key points, as advised by experts. Graphics and simplified visual aids can also play a vital role in bridging communication gaps, particularly among populations with varying levels of health literacy or language proficiency.
In addition, the ethical deployment of AI in healthcare reinforces the importance of transparency and accountability in communications. As AI becomes integrated into medical affairs and communications, adherence to core principles, such as privacy, confidentiality, inclusivity, and respect, is essential to ensure that the technology serves to enhance, rather than complicate, the understanding of clinical indications.
Ultimately, the objective is to guarantee that all individuals, regardless of their background or disability, have access to clear, accurate, and relevant information about their treatment choices. This not only aligns with the legal and ethical standards set forth by industry guidance but also with the intrinsic values of medical practice, advocating for an informed and empowered individual community.
Understanding the Role of ICD-10-CM Codes in Clinical Indications
The International Statistical Classification of Diseases and Related Health Problems (ICD), especially the 10th edition, Modification (ICD-10-CM), is crucial in streamlining documentation through a standardized system for classifying health conditions and diagnoses. This intricate coding structure not only enhances the precision and efficiency of medical summaries but also plays a pivotal role in optimizing reimbursement processes and quality reporting. The selection of accurate ICD-10-CM codes directly influences data analysis, impacting health services research and public health reporting. For example, the vast database from the Medical Information Mart for Intensive Care III, which catalogs data on over 60,000 critical care individuals, relies on ICD codes to facilitate secondary data analysis that informs epidemiological studies and health service evaluations. Moreover, the adoption of ICD-10-CM codes is essential to the advancement of decision support systems and the utilization of natural language processing in medical settings. With the recent finalization of Medicare payment rates by the Centers for Medicare & Medicaid Services (CMS) for 2024, which will affect thousands of hospitals and surgical centers, the accuracy of ICD-10-CM coding acquires even greater significance as it ensures compliance with evolving policies aimed at advancing health equity and patient-centered care. Furthermore, the adoption of ICD-11, which became effective in January 2022, underscores the ongoing evolution of these standards, promising enhanced data interoperability and the facilitation of global health research independent of language and cultural barriers. As such, it is incumbent upon healthcare providers to meticulously select and apply ICD-10-CM codes to maintain the integrity of health data and ultimately support the overarching goals of patient safety, quality improvement, and equitable healthcare delivery.
Case Studies: Effective Clinical Indication Documentation
To improve the efficiency of medication record, it is essential to take into account real-life situations and the methods used to tackle their intricacies. For example, Cardinal Health's collaboration with a client for an investigational drug application reveals the significance of developing a detailed regulatory starting material strategy. This collaboration facilitated timely and robust Investigational New Drug (IND) submissions, highlighting the significance of strategic planning in documentation for medical trials.
Furthermore, case studies, like the one demonstrating how diuretic therapy enhanced hepatic, portal, and intrarenal waveforms, offer important insights into the outcomes of interventions. Notably, this case emphasizes the sequential improvement of these waveforms and the potential delay in intrarenal venous waveform recovery due to factors like renal interstitial edema. Another case emphasizes the dynamic nature of the portal vein waveform and its response to fluid management procedures, providing valuable information for practice.
On the administrative side, the weight of medical record-keeping is illustrated by the situation at Summer Health, where pediatricians are faced with translating complex medical observations into comprehensive visit summaries. This task, consuming over half of medical care providers' time, leads to delays and potential frustration for both providers and parents. The implementation of the 21st Century Cures Act has mandated rapid, online access to medical records, thereby necessitating a patient-centered approach to documentation that avoids bias and promotes clear communication.
The American Health Information Management Association (AHIMA) underscores the importance of ensuring that health information professionals are equipped to manage these challenges effectively. With over 67,000 members, AHIMA emphasizes the role of accurate and accessible health information.
Furthermore, the current shortfall in the research workforce, with an alarming ratio of available positions to experienced candidates, underscores the urgency to address these systemic issues. The projected increase in demand for research coordinators by 9.9% between 2016 and 2026, coupled with a high resignation rate among tenured research professionals (CRPS), emphasizes the need for a distinct professional identity and support for the research workforce.
In summary, by examining these various case studies and the broader industry context, medical professionals can gain a comprehensive understanding of the challenges and strategies related to clinical indication record-keeping, ultimately leading to improved outcomes for individuals and streamlined processes in the healthcare sector.
Best Practices for Radiologists and Healthcare Providers
In the ever-changing realm of radiology, top-notch indication record keeping is crucial for precise diagnosis and efficient patient care. Radiologists and providers can enhance the process of recording by following proven methods, such as promoting multidisciplinary cooperation, sustaining continuous learning and development, and utilizing cutting-edge technology solutions.
Joint efforts between different medical fields are crucial to establish a complete understanding of indications. This method not just enhances the lucidity of records but also guarantees that all medical professionals are in agreement regarding the individual's state and the reasoning for the selected diagnostic techniques.
Continuous education and training are the bedrock of maintaining proficiency in the ever-evolving medical field. Radiology reading groups and imaging centers that handle a plethora of imaging types from X-rays to MRIs must navigate the complexities of diverse medical imaging data. Standardizing data and workflows helps radiologists overcome reporting challenges, which is why ongoing training is crucial in keeping staff abreast of best practices and the latest technological developments.
The use of technology plays a vital role in improving the quality of indication recording. Advanced solutions like Enlitic's ENDEX can significantly improve efficiency and accuracy in radiology diagnostics. For instance, dual-energy X-ray technology has shown promise in improving soft tissue visualization while reducing radiation exposure, as reported in a study at Grand River Hospital. Technologies that can deliver bedside imaging solutions in critical care settings are essential, as they provide high-quality images and assist in timely interventions.
Moreover, the integration of artificial intelligence and machine learning technologies can alleviate some of the cognitive burdens faced by radiologists. Tools like PowerScribe Smart Impression are already demonstrating efficiency gains across health systems by speeding up interpretation times. Such technologies not only contribute to increased revenue and cost savings but also play a role in enhancing employee satisfaction and reducing the risk of burnout among radiologists, as evidenced by the reduction of reading times and increased confidence in diagnostic accuracy.
Overall, by implementing these best practices, healthcare providers can significantly enhance the quality of clinical indication documentation, which in turn, improves patient care outcomes and contributes to the financial well-being of healthcare institutions.
Conclusion
In conclusion, clinical indications are crucial in radiology documentation, guiding radiologists in selecting imaging techniques and interpreting results. Standardized clinical indications can streamline reporting and enhance patient care, leading to improved operational efficiency and diagnostic accuracy. Collaborative efforts, precise and compliant records, and efficient documentation processes are key to rectifying misconceptions and improving the quality of clinical indication documentation.
Documenting clinical indications with precision, considering the audience, and incorporating evidence-based practice are essential principles. Using specific language, especially in diverse and multilingual landscapes, is crucial for inclusive patient care. The role of ICD-10-CM codes in clinical indications is significant for standardized classification, reimbursement processes, and quality reporting.
Real-world case studies highlight strategies for effective clinical indication documentation.
Radiologists and healthcare providers can optimize the process by fostering collaboration, ongoing education, and leveraging advanced technology solutions like AI. Implementing best practices enhances the quality of clinical indication documentation, leading to accurate diagnosis, effective patient care, and financial well-being of healthcare institutions. By adhering to these principles and utilizing innovative technologies, healthcare providers can achieve better outcomes, enhance patient engagement, and ensure a more efficient healthcare system.




