Introduction
A well-planned and comprehensive clinical trial budget is crucial for successfully managing the financial demands of a trial. It involves projecting costs related to various aspects of the trial, such as procedures, participant recruitment, data analysis, regulatory compliance, and site management. Accurate budgeting is not only about tracking expenses but also about resource management and ensuring that trials are completed within financial constraints.
With the increasing complexity of clinical research and the challenges faced by healthcare professionals, a meticulously constructed budget becomes a vital tool for efficient trial execution. In this article, we will explore the key components of a clinical trial budget, the steps to develop one, strategies to maximize efficiency, common pitfalls in budgeting, and best practices for budget management. By understanding the importance of budgeting and implementing effective strategies, stakeholders can navigate the financial landscape of clinical trials and support sustainable research efforts.
What is a Clinical Trial Budget?
- A comprehensive clinical trial budget is essential to navigate the complexities of a trial's financial demands. It encompasses projected costs related to procedures, participant recruitment, data analysis, compliance with regulatory standards, site management, and ancillary expenses that may arise. Such meticulous budgeting is not just about tracking expenses – it's integral to resource management and to ensuring that trials are completed without exceeding financial constraints.
For instance, bearing in mind the experiences of Chris, a seasoned biomedical engineer who has managed pivotal studies for Class III devices, the allocation of resources to critical phases such as PMA studies or post-market registries can significantly drive the success of clinical research.
Similarly, the budget must account for potential logistical hurdles for participants, as highlighted in a scenario involving a Pennsylvania patient with a rare disease participating in a trial abroad. The trial budgeting process should therefore include provisions for travel, documentation, and other unforeseen costs associated with international research activities, ensuring inclusivity of participation for patients regardless of geographical barriers.
Moreover, with the WHO-AIMS providing data-driven insights for mental health systems in countries like Egypt, the value of a well-constructed budget becomes clear. The 2% government spending on mental health and the treatment uptakes make a strong case for a thorough understanding of country-specific healthcare economics when planning trial finances.
In the fast-paced world of clinical research where trials can extend over several years, as noted by McKinsey's analysis showing an increase in the average trial duration between 2011-2015 and 2016-2021, the role of a well-planned budget is critical. Particularly as the industry faces an 80 percent rate of clinical trials not finishing on time, and the new pressures brought on by legislation such as the US Inflation Reduction Act, which urges companies to be first-to-market while simultaneously managing drug prices.
However, current modeling of clinical trial involvement, such as the CMS's assessment based on Relative Value Units in the US, highlights the financial challenges faced by physicians in prioritizing clinical research. Combined with the global turnover of healthcare staff, these factors underscore the importance of ensuring that the clinical trial budget effectively reflects the full spectrum of operational costs to support sustainable research efforts.
Key Components of a Clinical Trial Budget
Crafting a meticulous budget is paramount for the execution of clinical trials, encompassing a spectrum of costs that are imperative to the operational success of the study. To encompass the multifaceted nature of trials, a comprehensive budget should account for:
- The remuneration of principal and ancillary investigators that play pivotal roles throughout the study.
- Compensation for the study staff which includes coordinators, research nurses, and ancillary personnel.
- Resources allocated to patient recruitment efforts are critical, covering the advertising, screening, and informed consent procedures to curate an eligible participant pool.
- Reliable and secure data management infrastructure, featuring costs for state-of-the-art electronic data capture systems, data entry personnel, quality checks, and data repositories.
- The acquisition, safekeeping, and handling expenses related to the investigational product, whether it be a novel pharmaceutical or a medical device.
- Monies disbursed to trial sites which facilitate the study, inclusive of initiation, ongoing monitoring, and eventual close-out activities.
- The overarching institutional fees which address the administrative, infrastructure, and regulatory adherence required by participating entities.
- Regulatory compliance costs pertain to ethical review processes, national regulatory approvals, and any ensuing inspections.
- Funding designated for the critical statistical analysis of the data procured during the trial.
- A provision for miscellaneous expenses which cannot be foreseen but could include travel, training, and material production for the trial.
Highlighting the gravity of timely and on-point budgeting, insights from a McKinsey analysis show an increase from 41 to 44 months in the average duration of Phase 3 trials between two five-year periods, 2011-2015 and 2016-2021, reiterating that around 80% of clinical trials fall behind their initial timelines. With an ever-increasing herd mentality pushing biopharma companies towards the same high-potential mechanisms of action, the race to market intensifies, with the pioneer often reaping outsized successes.
Pointedly, the United States represents a primary clinical trial location, playing host to over 83% of global Phase 3 industry-sponsored trials, despite the challenges that incentive models pose for physicians participating in clinical research. Given these complexities, as well as the high turnover among clinical trial personnel, the budget becomes a reflection of the overall project plan, telling its story numerically and allowing stakeholders an articulate view of both the what and why behind each cost.
In essence, a well-crafted clinical trial budget not only lays bare the financial groundwork of a trial but is also a narrative tool that educates stakeholders on the nuanced fabric of clinical research—a fabric woven from the threads of essential medical investigation, the pursuit of healing, and the relentless quest to push the boundaries of current medical knowledge.
Steps to Develop a Clinical Trial Budget
To orchestrate a financial plan for a clinical trial, it is critical to adopt a detailed approach that encapsulates all potential expenditures. Starting with a crystal-clear definition of research objectives, the desired outcomes of the study are illuminated, offering direction for subsequent budgetary considerations. It requires pinpointing the factors that predominantly influence costs, such as study site quantity, participant recruitment goals, and the intricacies of data accrual.
Accurate budgeting necessitates assembling and evaluating cost estimates for each component. This may entail dialogues with domain experts, examining analogous past studies, and collaborations with suppliers. The formation of a standardized budget framework ensures all financial aspects are consistently captured, enhancing comparability across various trials.
Precise cost attribution is crucial, demanding thorough allocation to the respective budget lines, which includes both overt and covert expenses. An iterative review process is essential, refining the budget as feedback from stakeholders is integrated and newly surfaced data is incorporated.
The culmination of these efforts is a comprehensive budget that must be presented for approval. This rigorous process is underscored by a guiding principle: the primary concern is to pinpoint the core research questions, the answering of which will dictate the methodology and ultimately, the allocation of funds.
For example, the use of the WHO-AIMS in Egypt enabled a strategic alignment of information-based mental health plans, illustrating the importance of systematic data collection for efficient budgeting and planning. Chris, by leveraging his biomedical engineering background in clinical study management, demonstrates the necessity of expertise in the development of a sound budgetary plan. Furthermore, current trends suggest an increased need for prudent budgeting.
With clinical trial durations expanding and regulatory shifts influencing market dynamics, such as the US Inflation Reduction Act's impact on drug pricing, the stakes for accurate and efficient budgetary planning are higher than ever.
Real-world insights reveal that the ever-evolving landscape of clinical research demands a proactive and informed budgeting strategy. With 80 percent of clinical trials not concluding on time and surging research into prevalent mechanisms of action, the competition for market primacy is intense, accentuating the need for strategic financial planning. Equally, the acknowledgement of the clinical workforce crisis highlights the complexity of the ecosystem and the necessity for a budget reflective of all stakeholders' requirements.
Ultimately, the goal is the formulation of a budget that is as thorough and accurate as possible, encapsulating a complete financial depiction and ensuring the successful execution of the clinical trial.
Maximizing Efficiency in Clinical Trials
Efficiency in managing resources is a central concern for clinical trial companies as they navigate the intricate process of drug development. To optimize operations, a multidimensional approach is needed, incorporating both technological advances and strategic partnerships.
To enhance trial procedures, embracing electronic data capture systems and utilizing telemedicine for patient interactions can significantly streamline processes. This not only reduces costs but also shortens timelines, which is critical in an industry where the duration of Phase 3 trials has risen from an average of 41 months to 44 months, and Phase 2 trials from 37 to 41 months over recent years.
Consolidating services, such as centralizing testing at select laboratories, not only mitigates duplicated efforts but also elevates data uniformity and quality, which can lead to better trial outcomes. Moreover, collaboration with well-established investigator networks offers access to pre-existing infrastructure and patient pools, expediting the recruitment phase and reducing administrative overhead.
The leverage of technology is another pillar that cannot be overlooked. Automation of routine tasks through advanced software can yield more accurate data and foster improved communication between team members. Integrating wearables, electronic diaries, and decentralized methods into data acquisition allows the collection of multi-faceted data, which artificial intelligence can then transform into actionable insights.
Investment into staff training is paramount; a workforce well-versed in trial protocols operates with greater efficiency and precision, mitigating errors and ensuring regulatory adherence. Additionally, a continuous quality improvement process enables the constant refining of trial procedures, fostering a cycle of enhancement that can result in sustained efficiency and reduced expenditure over time.
These strategies are reinforced by a shift towards greater patient involvement in trials, as demonstrated by the MHRA's pilot program emphasizing patient feedback in early stages of medicine development. Furthermore, with the initiative to streamline applications and attract more international trials to the UK, the necessity for efficient resource management has never been more pronounced. Each decision in trial design has a ripple effect, and optimizing these choices based on robust data can dramatically impact the success rate of a study.
Applying a thoughtful data strategy from the onset ensures quality insights guide drug development in a patient and safety-centric manner.
Cost-Effectiveness Strategies
Achieving cost-effectiveness in clinical trial management is not just a desirable goal but a critical one, as it enables the judicious use of limited resources while maintaining high standards of scientific rigor and patient care. To refine the financial stewardship of clinical trials, consider the following strategies:
- Resource Prioritization: Assign resources with precision, focusing on aspects of the trial that promise the most substantial scientific returns and clinical benefits. Concentrating efforts on pivotal interventions improves both economic efficiency and trial outcomes.
- Evidence-Informed Decision-Making: Ground treatment choices and diagnostic tests in a robust evidence base to avoid the unnecessary costs tied to experimental practices. This measured approach aligns with the principles of Health Technology Assessment, which balances cost against safety and efficacy in healthcare delivery.
- Strategic Contracting and Pricing: Engage in thorough negotiations with vendors and suppliers, and opt for long-term contracts where advantageous. This leverages the power of comparison and negotiation to achieve favorable terms, which can significantly reduce overall expenditures.
- Expenditure Monitoring and Control: Implement stringent budget oversight systems to keep a vigilant eye on spending. Comparing expenditure with allocated budgets regularly can bring to light any inconsistencies, allowing for timely correction and preventing overruns.
- Diversification of Funding Sources: Explore supplemental funding through grants, partnerships, or collaborations. Tapping into external financial support can alleviate budget constraints and broaden the scope of available resources for the trial.
- Evaluation of Innovations: Keep abreast of technological advancements that could potentially cut costs without compromising the integrity of trial data or patient safety. An example includes the development of novel, cost-effective MRI technologies that widen access to important diagnostic tools.
The paramountcy of each step cannot be overstated; focusing on cost and value simultaneously guides healthcare towards more beneficial and sustainable practices. As emphasized in a recently published analysis, cost-effectiveness should not be an afterthought but a fundamental criterion in patient care strategies, affecting decisions from the patient's journey to a trial across continents to the adoption of new medical technologies. With this mindful approach, clinical trials can achieve a balance between fiscal responsibility and exemplary scientific conduct.
Common Pitfalls in Clinical Trial Budgeting
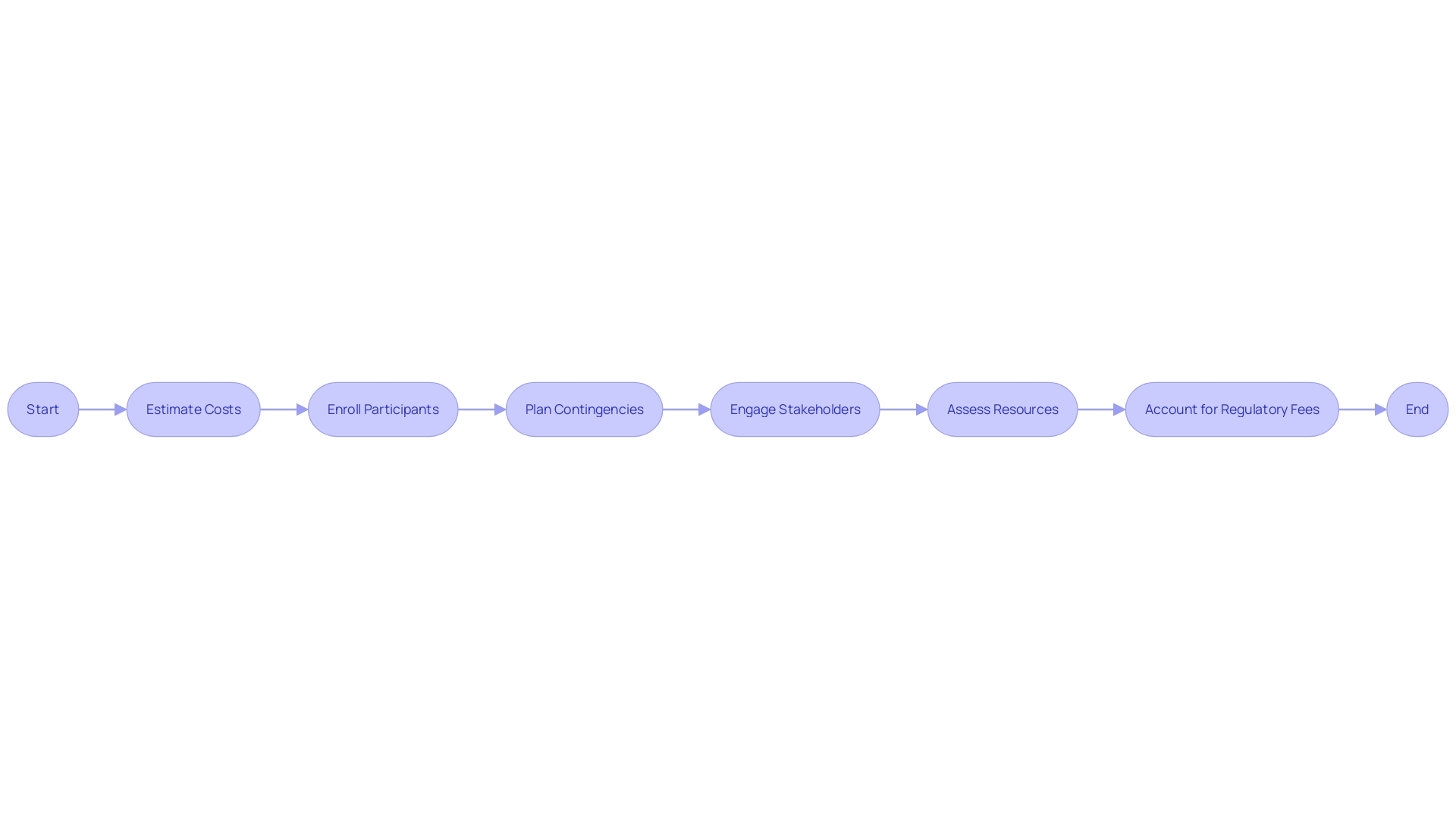
Building a rigorous clinical trial budget is an intricate process, where precision and foresight are essential to prevent missteps. Key considerations to improve the accuracy and efficiency of clinical trial budgets include meticulous cost estimation, having realistic participant enrollment figures based on empirical data, establishing a contingency fund for unexpected changes, engaging stakeholders for comprehensive planning, assessing resource availability, and fully accounting for regulatory fees.
Precise cost calculations guard against shortfalls by incorporating all necessary elements and planning for the unpredictable, as clinical trials may take longer and consume more resources than initially projected. For example, clinical trial durations have increased over recent years, necessitating a more robust budgeting strategy. Realistic enrollment projections are crucial, with sophisticated methods like Thompson Sampling enabling the assignment of treatments in a manner that corresponds with their likelihood of being beneficial.
Furthermore, maintaining an open line of communication with key players such as investigators and financial personnel ensures alignment with the trial's practical requirements and promotes a more accurate resource allocation. Additionally, recognizing the importance of compliance costs and the implications of recent legislation such as the US Inflation Reduction Act helps navigate the financial landscape of drug development efficiently. Employing such strategic planning and foresight enhances the capacity of clinical trials to innovate healthcare, mirroring efforts like the pioneering low-cost MRI by CTSI grantee Efraín Torres, whose technology is set to extend medical care access to broader populations.
Best Practices for Budget Management
Streamlining financial management within clinical trial operations is pivotal for project success. Here are several strategic practices to enhance fiscal oversight and efficiency:
- Integration of Financial Expertise: Partnering with professionals specialized in finance and accounting is paramount. Such collaboration guarantees the precision and steadfastness of budget creation and adherence, with experts lending their acumen to identify possible fiscal hazards and optimize the allocation of resources.
- Real-Time Expenditure Tracking: Employing a sophisticated financial tracking mechanism is essential for capturing all trial-related expenditures as they occur. This facilitates immediate evaluation of spending in relation to the budget and enables quick adjustments when deviations are detected.
- Dynamic Budget Management: It’s imperative to perform continuous reassessment of the budget as the trial progresses to confirm that it remains current and accurate, adjusting as and when needed due to protocol modifications, enrollment shifts, or unexpected events.
- Transparent Communication with Stakeholders: Ensuring regular and transparent dialogue with all stakeholders about the fiscal health of the project is crucial. It is through this transparency that efficient collaboration on budget modifications can be fostered, should they become necessary.
- Variance Rationalization: It is vital to meticulously record and elucidate any significant discrepancies between the forecasted and actual expenditures. This practice not only reinforces fiscal accountability but also serves as a repository of financial intelligence for future budgeting endeavors.
- Retrospective Budget Analysis: Examining budgetary performance post-trial is a wise approach to discover areas for fiscal improvement. Drawing lessons from past trials and applying that knowledge to future budget planning is vital for the cultivation of fiscal prudence and effectiveness in subsequent projects.
In light of statistics revealing an increase in average clinical trial duration—rising from 41 to 44 months for Phase 3 trials, and 37 to 41 months for Phase 2 trials between 2011-2015 and 2016-2021—it's more crucial than ever to manage budgets effectively to mitigate delays. Moreover, with approximately 80% of clinical trials not finishing on time, enhanced budgeting strategies can contribute to improving the speed of clinical development, which is pivotal for biopharma companies in the race to be the first to market, especially given the competitive landscape accentuated by legislation such as the US Inflation Reduction Act.
Additionally, the poignant scenario of a rural Pennsylvania patient with a rare disease facing cross-border travel challenges for a clinical trial in Turkey underscores the complexity and logistical considerations that can impact clinical trial budgeting and management. These challenges must be skillfully navigated to optimize the integration and analysis of rich data insights from diverse sources such as wearables and electronic diaries, necessitating an intentional and well-defined data strategy from inception to the close of the trial.
Conclusion
In conclusion, a well-planned clinical trial budget is crucial for successfully managing the financial demands of a trial. It allows for accurate tracking of expenses, resource management, and ensuring trials are completed within financial constraints.
The key components of a clinical trial budget include investigator remuneration, staff compensation, patient recruitment, data management infrastructure, investigational product expenses, trial site costs, institutional fees, regulatory compliance costs, statistical analysis funding, and provisions for miscellaneous expenses.
To develop a clinical trial budget, a detailed approach is necessary, starting with clear research objectives and evaluating cost estimates for each component. Stakeholder feedback and newly surfaced data should be incorporated through an iterative review process.
Efficiency in clinical trials can be maximized through the adoption of technological advances, strategic partnerships, and patient involvement. Electronic data capture systems, telemedicine, centralizing testing, automation, staff training, and continuous quality improvement contribute to streamlined processes and resource optimization.
To achieve cost-effectiveness, resource prioritization, evidence-informed decision-making, strategic contracting, expenditure monitoring, diversification of funding sources, and evaluation of innovations are crucial strategies.
Avoiding common pitfalls in budgeting requires meticulous cost estimation, realistic enrollment projections, contingency funds, comprehensive planning, resource availability assessment, and accounting for regulatory fees.
Best practices for budget management involve integrating financial expertise, real-time expenditure tracking, dynamic budget management, transparent communication with stakeholders, variance rationalization, and retrospective budget analysis.
By implementing these strategies, stakeholders can navigate the financial landscape of clinical trials and support sustainable research efforts. With a well-planned budget and efficient resource management, stakeholders can ensure successful trial execution and contribute to the advancement of medical knowledge.




