Introduction
The International Classification of Functioning, Disability, and Health (ICF) is a vital tool in the healthcare and clinical trials field. Developed by the World Health Organization, the ICF offers a universal language and structure for documenting health and health-related states. It goes beyond simply cataloging ailments and evaluates the broader impact of health conditions on an individual's daily life, assessing their functional capabilities and societal involvement.
In contrast to the International Statistical Classification of Diseases and Related Health Problems (ICD), the ICF complements it by contextualizing the consequences of health conditions on individuals' lives. Together, these classification systems provide a holistic view of health, enhancing our understanding of health trends and enabling better healthcare delivery tailored to the diverse needs of patients. In this article, we will explore the origin and development of the ICF, its components, its application in healthcare, its role in clinical trials, and the benefits it brings to both fields.
What is ICF?
The International Classification of Functioning, Disability, and Health (ICF) is an integral part of the healthcare and clinical trials lexicon. Created by the World Health Organization, the ICF offers a global language and framework for the documentation of well-being and conditions related to well-being. Its purpose extends beyond documenting ailments; it evaluates the wider impact of medical conditions on an individual's daily life, assessing their functional capabilities and societal involvement. This comprehensive approach to well-being reflects the complex interplay of various factors, including genetic makeup, environmental influences, and personal experiences, which collectively shape an individual's well-being.
In contrast to the ICF's emphasis on functionality, the International Statistical Classification of Diseases and Related Problems (ICD), specifically the latest ICD-11 version effective from January 2022, serves as a global data standard for recording and analyzing disease and mortality data. While the ICD is pivotal for producing standardized health statistics, guiding diagnoses, and supporting management of medical conditions, the ICF complements it by contextualizing the consequences of medical conditions on individuals' lives. Collectively, these categorization systems provide a comprehensive perspective on well-being, improving our comprehension of well-being patterns and facilitating superior medical provision customized to the varied requirements of individuals.
Origin and Development of ICF
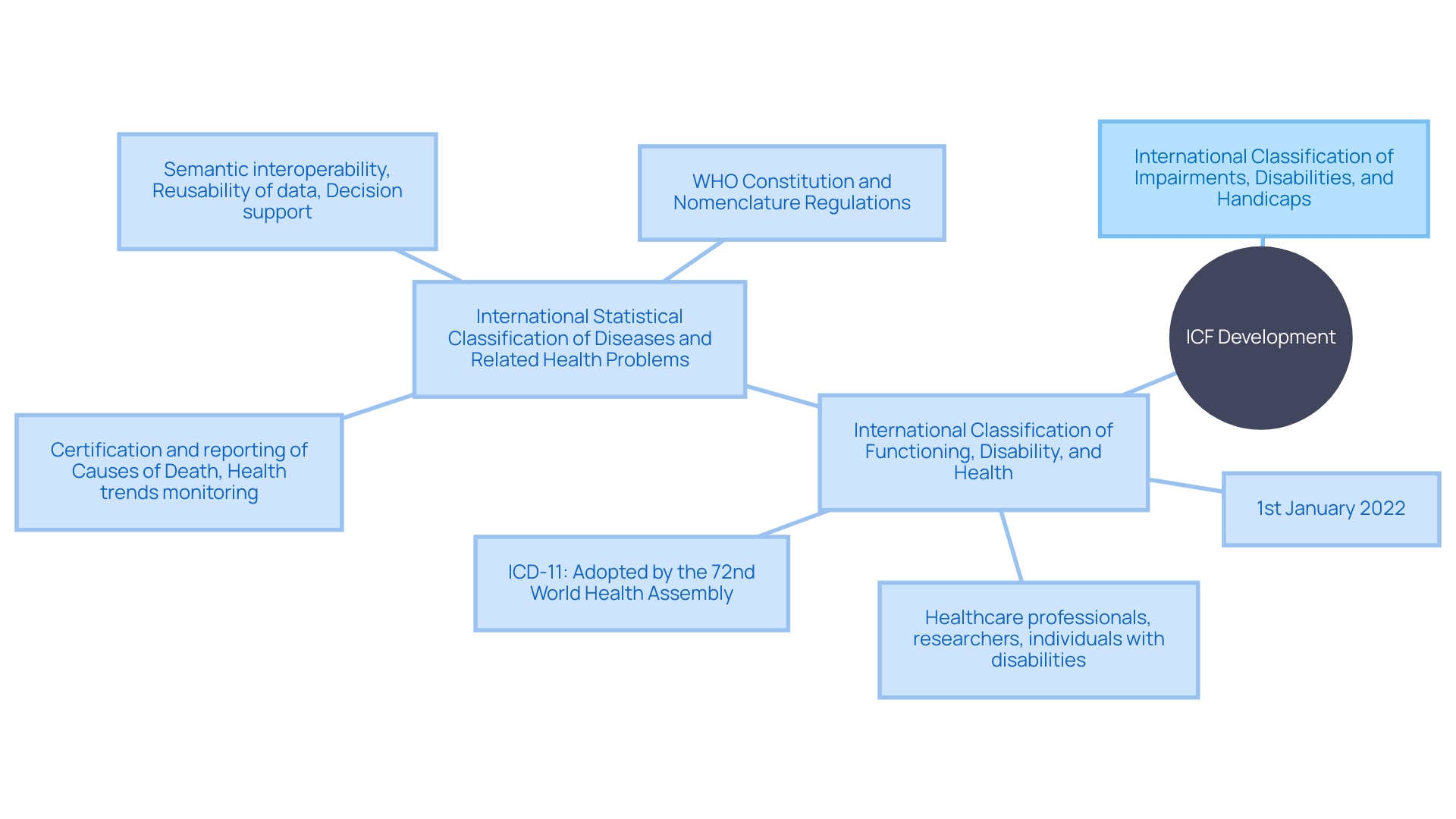
The inception of the International Classification of Functioning, Disability, and Health (ICF) in the early 2000s marked a significant evolution from the previous International Classification of Impairments, Disabilities, and Handicaps (ICIDH). With an aim to adopt a more integrated and comprehensive framework for classification, the ICF was cultivated through rigorous research and the concerted efforts of a diverse group of experts. This group encompassed healthcare professionals, researchers, and individuals with firsthand experience of disability. They worked together to build a tool that would improve the comprehension and monitoring of well-being and disability at both individual and population levels. The ICF's development mirrors the meticulous process undertaken for the International Statistical Classification of Diseases and Related Problems (ICD), a global standard for recording and statistics, which has been foundational in providing consistent and comparable data for over a century. The ICF, similar to the latest ICD-11, aims to facilitate the systematic recording, analysis, and interpretation of information, transcending language and cultural barriers to achieve a universal standard. This aligns with the World Organization's mandate for a complete data standard, ensuring interoperability and utility across various domains, from clinical decision support to resource allocation.
Components of ICF
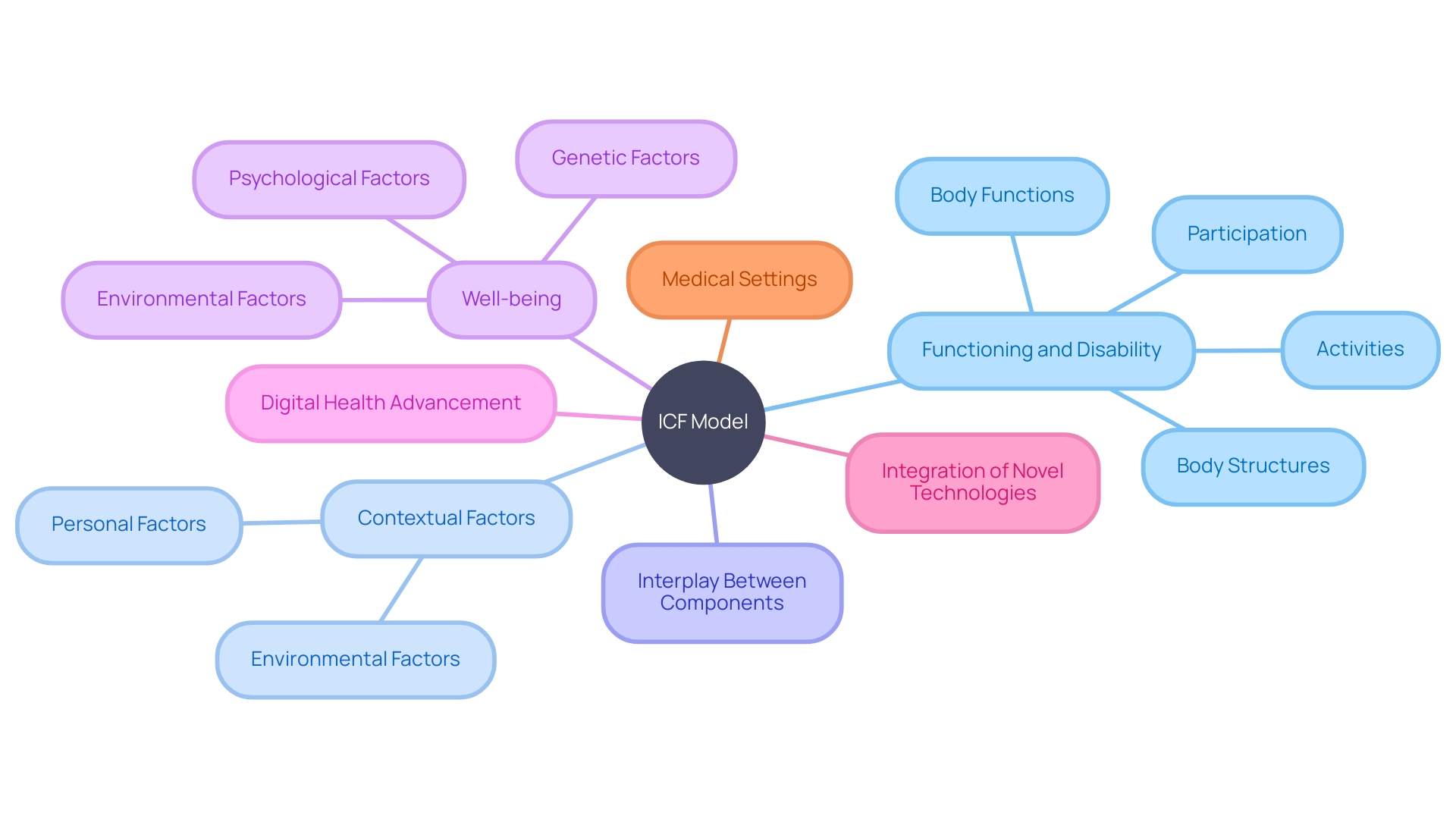
The International Classification of Functioning, Disability and Well-being (ICF) model is a dual-component system designed to capture an in-depth picture of an individual's physical and mental condition and its impact on day-to-day life. The first component, Functioning and Disability, encompasses Body Functions and Body Structures, as well as an individual's Activities and Participation. This aspect of the model provides insights into the physiological and anatomical components of various conditions, alongside the practical implications on a person's ability to engage in life situations.
The second component, Contextual Factors, is further divided into Environmental Factors and Personal Factors. These factors collectively account for the role of the physical, social, and attitudinal environment in which people live and conduct their lives. They serve as an integral part of the model, recognizing that disability and functioning do not exist in isolation but are influenced by a broader context. This approach mirrors the multi-faceted nature of well-being, as per statistics which highlight that well-being is not merely about the absence of disease but involves a complex interplay of genetic, psychological, and environmental factors.
Essentially, the ICF framework corresponds to the recognition that health outcomes and the effectiveness of interventions result from both individual traits and the support systems accessible, as highlighted by recent efforts in digital health advancement and the incorporation of novel technologies in medical settings.
Application of ICF in Healthcare
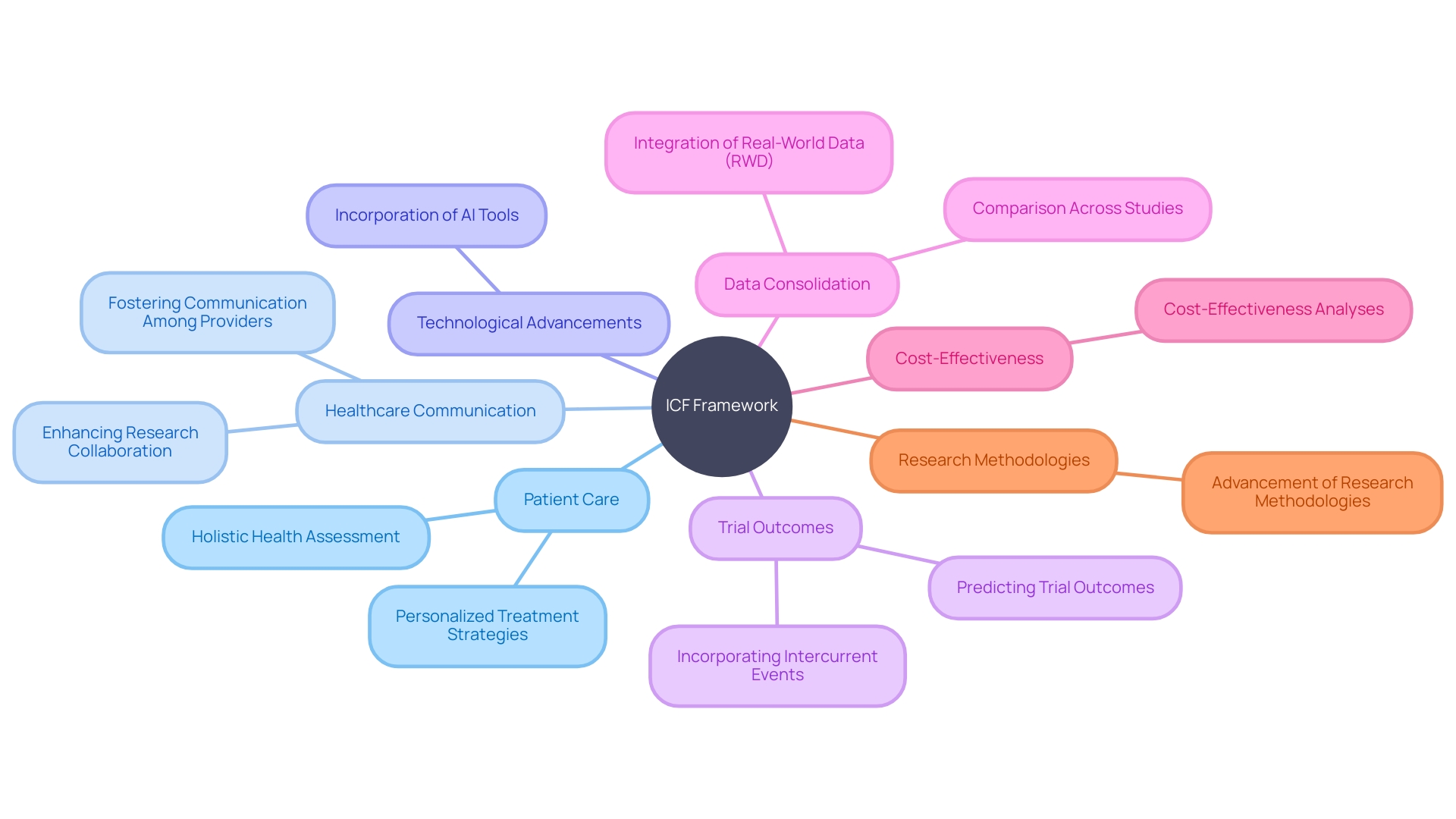
The implementation of the International Classification of Functioning, Disability and Health (ICF) has transformed the provision of medical services, providing a standardized framework to assess and record individual functioning and disability. Healthcare professionals utilize ICF to meticulously identify areas of patient concern, facilitating the creation of tailored intervention strategies. This fosters a holistic, person-centered treatment paradigm, prioritizing personal objectives and values. Concurrently, the integration of Medical 4.0 technologies, including big data and artificial intelligence, is reshaping the delivery of medical services, paving the way for more efficient, personalized services such as telemedicine and teledentistry. This digital transformation in the medical field supports a more nuanced application of ICF, enhancing the precision and personalization of patient care. As the medical sector keeps progressing, the combination of ICF's extensive evaluation tools with state-of-the-art digital medical solutions offers the potential to enhance the influence on patient results and medical efficiency.
ICF in Clinical Trials
The International Classification of Functioning, Disability, and Health (ICF) serves as a universal framework in trials to describe and measure health and disability levels. By employing the ICF, researchers gain the ability to convey the effects of healthcare interventions on an individual's functional status and societal involvement with precision. This shared language promotes the synthesis of research outcomes, enhancing the comparability of studies across various conditions and interventions. This is especially apparent in research on personalized medicine approaches, such as AI-driven predictions of individual drug responses in oncology, where outcomes are intricately related to patient-specific factors. For example, in precision oncology trials, matching scores based on drug sensitivity assays are utilized to correlate the alignment of prescribed treatments with AI recommendations, significantly impacting patient prognosis in conditions like B-cell lymphoma. Moreover, the ICF's comprehensive approach allows for the assessment of interventions through both the quality-adjusted life year (QALY) metric and the Equal Value of Life Years Gained (evLYG), providing a holistic view of the intervention's impact on life length and quality. The integration of patient and public involvement in trial design, as endorsed by international bodies, further emphasizes the importance of aligning research with patient-centered outcomes, ensuring that the findings resonate with the needs and experiences of those affected. Basically, ICF's role extends beyond measurement to inform decision-making and policy development, aligning with the FDA's initiatives to harmonize human subject protection regulations and enhance the efficiency of research.
Benefits of Using ICF in Healthcare and Clinical Trials
The application of the International Classification of Functioning, Disability and Health (ICF) in the domain of medical care and trials is crucial for improving patient care and progressing medical research. ICF's framework excels in fostering uniformity in communication among healthcare providers and researchers, which is paramount for collaborative efforts. For example, the use of artificial intelligence (AI) to analyze unstructured medical notes demonstrates the incorporation of technological advancements with ICF's standardized vocabulary, enhancing patient treatment plans and potentially prolonging life expectancies in conditions like uveal melanoma metastasis to the liver, for which research studies are a vital pathway due to the lack of FDA-approved therapies.
Moreover, ICF's holistic approach to health assessment recognizes the intricate interplay between biological and psychosocial factors, thereby ensuring that treatment strategies are not only personalized but also aligned with the individual's unique health profile. This methodology is supported by emerging AI tools like the HINT algorithm and SPOT system, which aid in predicting trial outcomes and refining trial designs to enhance efficacy.
Additionally, the integration of ICF in research enables the consolidation and comparison of data across studies, thereby facilitating the emergence of evidence-based practices. This is especially relevant when considering the utilization of quality-adjusted life years (QALYs) in cost-effectiveness analyses, which have become a cornerstone in evaluating the impact of medical interventions on patient outcomes.
The adoption of ICF is further underscored by the evolving landscape of real-world data (RWD) quality assessment, as highlighted by the FDA's encouragement of incorporating RWD for more representative trial designs. The discussion about data quality and the appropriate use of RWD for trials are crucial in shaping patient-centric research methodologies.
Essentially, the ICF framework is a driver for innovation in the medical field, optimizing patient-centered care and propelling the advancement of research methodologies that are both effective and adherent to regulatory standards. It plays a critical role in the curation of a more robust, efficient, and patient-focused healthcare system, ultimately contributing to the betterment of clinical outcomes.
Conclusion
In conclusion, the International Classification of Functioning, Disability, and Health (ICF) is a vital tool in healthcare and clinical trials. Developed by the World Health Organization, it provides a universal language and structure for documenting health and health-related states. The ICF goes beyond cataloging ailments and evaluates the broader impact of health conditions on daily life, assessing functional capabilities and societal involvement.
It complements the International Statistical Classification of Diseases and Related Health Problems (ICD), offering a holistic view of health and enhancing healthcare delivery tailored to diverse patient needs.
The ICF's origin and development involved collaboration among healthcare professionals, researchers, and individuals with firsthand experience of disability. It aims to facilitate the systematic recording, analysis, and interpretation of health information on a universal scale. The ICF model consists of two components: Functioning and Disability, which encompass Body Functions, Body Structures, Activities, and Participation; and Contextual Factors, which include Environmental Factors and Personal Factors.
This comprehensive framework recognizes the multi-faceted nature of health and the influence of a broader context on disability and functioning.
In healthcare, the ICF revolutionizes patient care by delivering a standardized framework to evaluate and document individual functioning and disability. Integration with Medical 4.0 technologies enhances the precision and personalization of patient care. In clinical trials, the ICF serves as a universal framework to describe and measure health and disability levels, promoting research outcome synthesis, comparability across studies, and assessment of interventions.
The benefits of using the ICF in healthcare and clinical trials are significant. It fosters uniformity in communication, supports personalized treatment strategies, enables data consolidation and comparison, and contributes to evidence-based practices. The integration of ICF in research methodologies aligns with the evolving landscape of real-world data quality assessment and patient-centric research.
Overall, the ICF is a catalyst for innovation in healthcare, optimizing patient-centered care, and propelling the development of effective research methodologies. Its comprehensive approach to health assessment plays a critical role in curating a robust, efficient, and patient-focused healthcare system, ultimately contributing to better clinical outcomes.




