Overview
The article focuses on the growth of medical trials in Latin America, highlighting the region's diverse patient demographics and improved healthcare infrastructure as key drivers of this trend. It supports this by detailing the increasing investment in research, favorable regulatory changes, and the potential for cost-effective studies, while also addressing the challenges that must be overcome to fully realize this growth potential.
Introduction
Latin America is rapidly emerging as a pivotal player in the global clinical trials landscape, characterized by its diverse patient populations and evolving healthcare infrastructure. As the region captures an increasing share of the clinical trials matching software market, countries like Brazil, Mexico, and Argentina are leading the charge with a multitude of trials across various therapeutic areas. This growth is not just a reflection of the region’s demographic advantages but also a response to the burgeoning demand for innovative treatments, particularly in a climate where investment in clinical research is skyrocketing.
However, navigating this promising terrain is not without its challenges, as researchers face:
- Regulatory complexities
- Cultural differences
- Infrastructure gaps
The interplay of these factors shapes the future of clinical trials in Latin America, making it essential to explore both the opportunities and obstacles that define this dynamic environment.
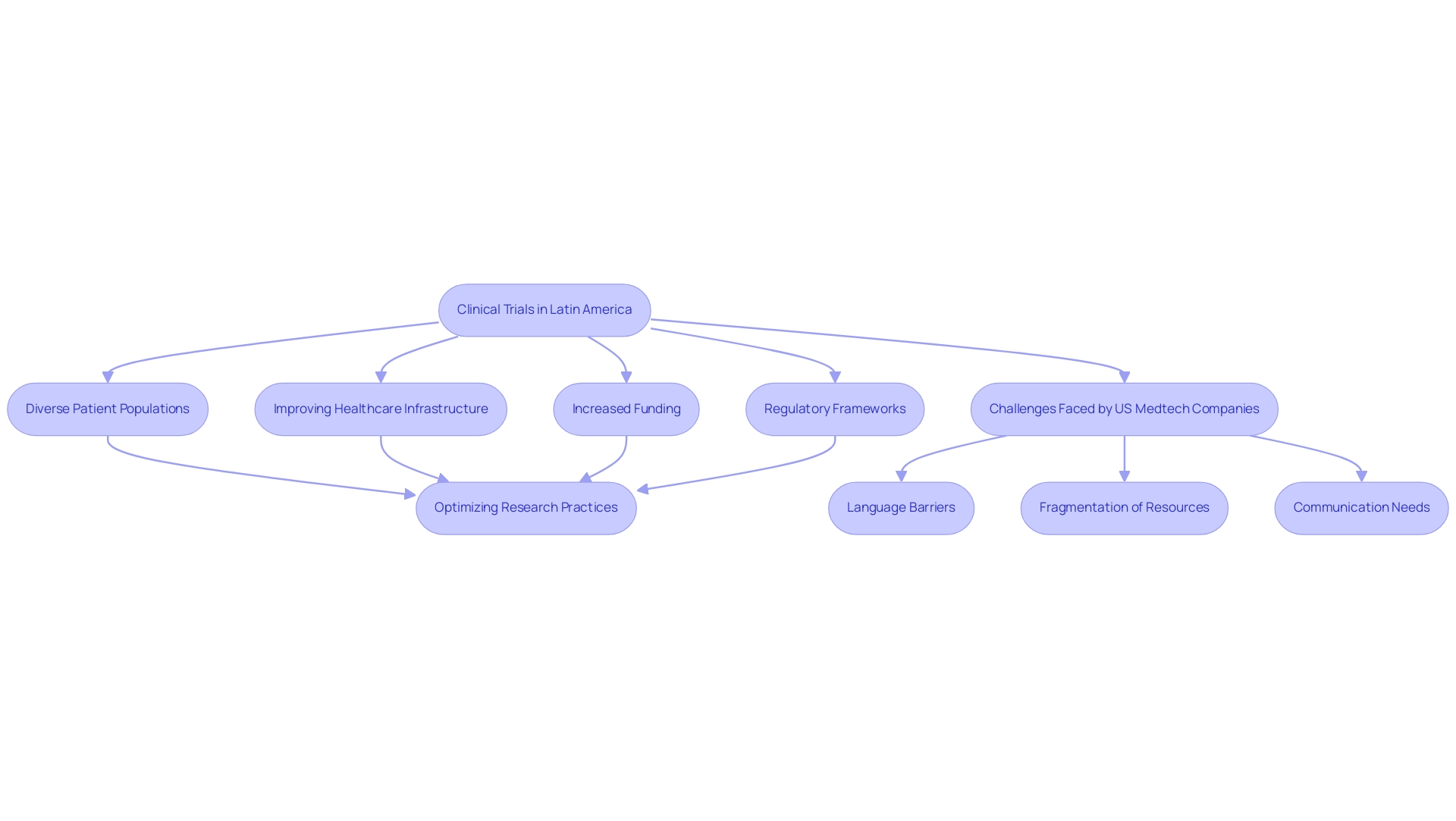
Overview of Clinical Trials in Latin America
Latin America has solidly positioned itself as an essential participant in the global research landscape, with the medical trial growth in Latin America being propelled by its varied patient demographics and swiftly improving healthcare infrastructure. In 2023, the area accounted for 3.5% of the worldwide research matching software market, indicating strong growth potential. Nations like Brazil, Mexico, and Argentina are at the forefront of the medical trial growth in Latin America, hosting numerous studies across various therapeutic areas.
The region's large pediatric population indicates a growing elderly demographic and a burgeoning new drug market, which could attract further investment. Significantly, funding in the research sector has increased from $3-4 million to over $50 million each year in the Andean Region, especially in Peru, Colombia, and Chile, emphasizing the area's attractiveness to both domestic and foreign sponsors. This growing interest is supported by favorable regulatory frameworks, such as the pending legislation in Brazil (PL 7082/2017), aimed at improving research practices and streamlining regulatory approval processes.
However, as highlighted by Gotuzzo from Universidad Peruana Cayetano Heredia, addressing linguistic, cultural, and socio-economic barriers remains essential for optimizing patient protection and enhancing the overall quality of research trials. Furthermore, US Medtech companies face specific challenges in this landscape, including:
- Language barriers
- Fragmentation of resources
- The need for effective communication with American hospitals
Cooperation between Medtech firms and prominent CROss like bioaccess® is crucial in addressing these challenges, enabling expedited study results, and ultimately connecting innovation with implementation.
This dynamic landscape not only highlights the significance of diverse patient populations but also underscores the medical trial growth in Latin America as a promising frontier for innovative medical research.
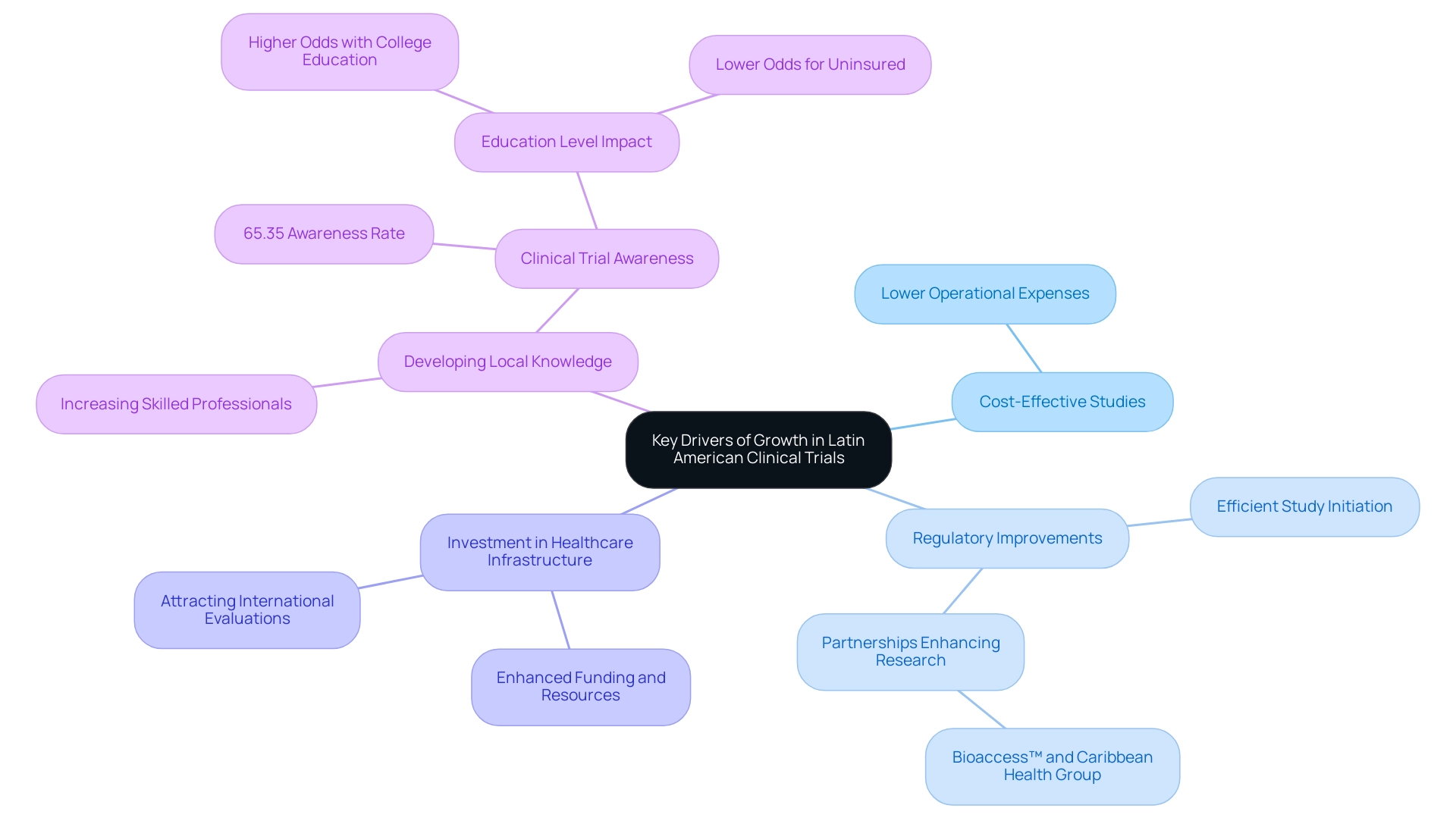
Key Drivers of Growth in Latin American Clinical Trials
Several crucial factors drive the medical trial growth in Latin America, including the region's diverse patient populations, which boast a rich tapestry of genetic backgrounds essential for studying a wide array of diseases and their responses to treatments. Significantly, a recent study discovered that among 79 respondents with a history of cancer, the majority showed no substantial differences in their willingness to engage in studies based on race or ethnicity. This emphasizes the potential for inclusive representation in studies.
However, as Singh points out, "there are many studies that have shown that there seems to be negative biases against African Americans and Latinos in receiving access to care, and that may extend into biases against involving them in research as well."
- Cost-Effective Studies: The medical trial growth in Latin America results in significantly lower operational expenses than both North America and Europe, making it an appealing location for sponsors aiming to maximize their budgets.
- Regulatory Improvements: The region has witnessed progress in regulatory frameworks, enabling more efficient initiation and execution of research studies, which is pivotal for the medical trial growth in Latin America, as evidenced by the partnership between bioaccess™ and Caribbean Health Group announced on March 29, 2019, in Miami, FL, to enhance research opportunities in Barranquilla, supported by Colombia's Minister of Health.
- Investment in Healthcare Infrastructure: Investment in healthcare infrastructure is vital as enhanced funding and resources in healthcare systems strengthen the ability to perform high-quality studies, which is essential for the medical trial growth in Latin America and attracting international evaluations.
- Developing Local Knowledge: An increasing pool of skilled professionals is vital for the medical trial growth in Latin America, enhancing the region's capacity to manage complex studies effectively. Furthermore, a study showed that among 2956 participants, 1932 (65.35%) reported knowing something about trials, suggesting that education levels can affect awareness and involvement.
Furthermore, partnerships like that of GlobalCare Clinical Trials with bioaccess™ have led to over a 50% reduction in recruitment time and achieved 95% retention rates, showcasing the efficiency gains possible in this landscape. Thus, the continuous enhancements in regional expertise and infrastructure, together with bioaccess®'s dedication to information security—utilizing appropriate measures to avert loss and unauthorized modification of data—are encouraging for the medical trial growth in Latin America.
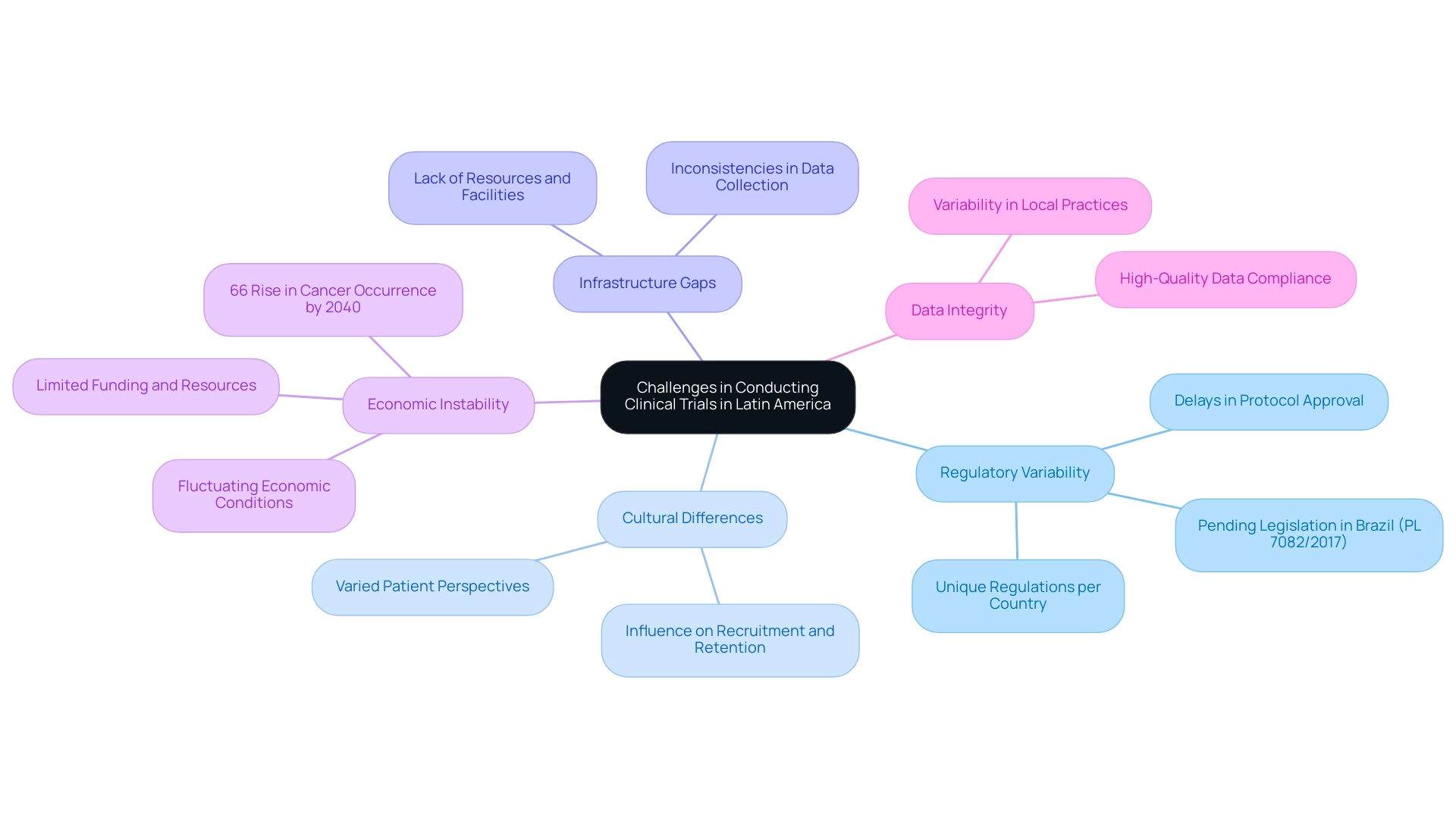
Challenges in Conducting Clinical Trials in Latin America
While Latin America offers an abundance of possibilities for medical investigations, the medical trial growth in Latin America is challenged by various substantial obstacles that can impede the success of studies. One prominent issue is Regulatory Variability. Each nation has its unique set of regulations, complicating the implementation of multi-country studies and often resulting in delays in protocol approval.
For example, pending legislation in Brazil (PL 7082/2017) aims to simplify these processes, with Mirella Nardo mentioning that it could signify a significant enhancement, necessitating various good practice regulations for trials, including a maximum duration to obtain regulatory approval for a study protocol.
Another challenge is Cultural Differences. Varied patient perspectives and convictions about healthcare and research can significantly influence recruitment and retention rates in medical studies. Understanding these cultural nuances is vital for designing studies that resonate with local populations.
Infrastructure Gaps also pose a significant barrier. Certain regions lack the necessary resources and facilities to support the demands of complex studies, which can lead to inconsistencies in data collection and patient management.
Furthermore, Economic Instability can severely impact the feasibility of research trials. Fluctuating economic conditions can limit funding and resource availability, making it difficult to sustain ongoing research initiatives. This is especially pertinent as forecasts suggest a staggering 66% rise in cancer occurrence in Central and South America and the Caribbean by 2040, with over 2.4 million new cases anticipated, which underscores the urgent requirement for effective research studies and highlights the necessity for medical trial growth in Latin America.
Lastly, concerns about Data Integrity are paramount. Ensuring high-quality data that complies with international standards is crucial; however, the variability in local practices and regulations can complicate this effort. Studies like 'Cancer Burden in Central and South America' and 'Liver Cancer as a Public Health Priority' highlight the critical need for targeted public health interventions to address risk factors and improve early diagnosis.
Tackling these challenges is crucial for advancing the field of healthcare in Latin America and fostering medical trial growth in Latin America to improve patient outcomes throughout the region. At the forefront of these efforts, bioaccess® stands as a prominent contract organization, facilitating medical device evaluations with a focus on innovation and regulatory excellence. Their comprehensive services encompass feasibility studies, site selection, compliance reviews, experiment setup, project management, and reporting processes, ensuring that studies are conducted efficiently and effectively.
Moreover, Katherine Ruiz, a specialist in Regulatory Affairs for medical devices and in vitro diagnostics in Colombia, plays a crucial role in navigating the complex regulatory landscape, offering invaluable insights that boost the success of research initiatives.
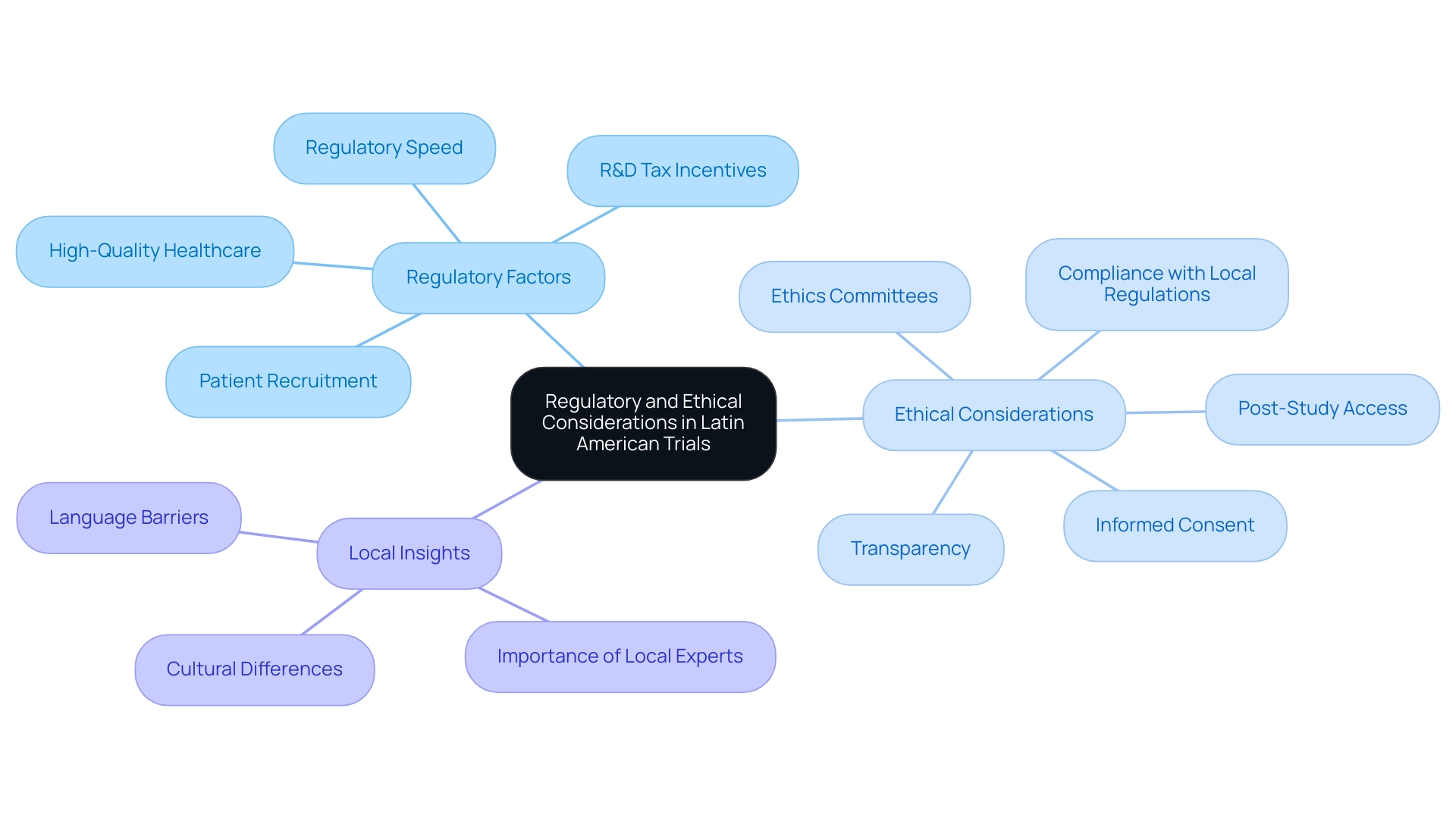
Regulatory and Ethical Considerations in Latin American Trials
In Central America, regulatory authorities play an essential role in ensuring that clinical studies adhere to established ethical and operational guidelines, with a significant emphasis on Colombia as a top choice for first-in-human (FIH) clinical studies. Notably, 83% of studies in Latin America and the Caribbean reflect the medical trial growth in Latin America, as they are industry-sponsored, which significantly influences regulatory practices and ethical considerations. Colombia stands out for several competitive advantages, particularly in the context of medical trial growth in Latin America, as clinical studies in Colombia can save over 30% compared to similar studies in North America or Western Europe.
- Regulatory Speed: The total review time for IRB/EC and INVIMA approvals is between 90-120 days, facilitating rapid trial initiation.
- High-Quality Healthcare: The World Health Organization ranks Colombia's healthcare system as #22 globally, while local hospitals are recognized among the best in Latin America.
- Patient Recruitment: With a population exceeding 50 million and 95% covered by universal healthcare, Colombia offers robust patient recruitment potential.
- R&D Tax Incentives: Investments in inquiry and innovation can yield significant tax deductions and credits, further encouraging clinical studies.
The subsequent key factors are essential to the success of these assessments, especially in the context of medical trial growth in Latin America:
- Informed Consent: It is crucial that investigators guarantee participants fully understand the study's nature and purpose, offering voluntary consent as a cornerstone of ethical practices.
- Ethics Committees: Independent ethics committees are responsible for reviewing and approving studies, acting as protectors of participant welfare and rights throughout the research process.
- Compliance with Local Regulations: Considering the varied legal environments throughout the region, following the particular regulations of each nation is crucial for preserving the integrity of research.
- Transparency: Effective communication with all stakeholders fosters trust and ensures the integrity of the study, particularly in a context where cultural differences can enhance patient-physician relationships, potentially improving participation rates.
- Post-Study Access: Ethical considerations must include the availability of treatment for participants after the study, a commitment that should be factored into the design.
Moreover, language variations complicate research studies in South America, which is significant in the context of medical trial growth in Latin America, requiring precise translation of regulatory and patient documents to maintain ethical treatment and informed consent. Addressing linguistic and cultural differences can mitigate delays in ethics committee approvals and enhance patient understanding and rights. The seasonal prevalence of diseases like pneumonia and flu at different times in the southern hemisphere also positions America as ideal for infectious disease studies.
As Sandra Grosworsel Schefler, Managing Director in Brazil, aptly states, 'It pays to listen to these regional experts for the best possible outcome of a Latin American study.' This perspective highlights the necessity of integrating local insights into the regulatory and ethical considerations of medical trial growth in Latin America that involves patients. Moreover, our extensive research management services encompass feasibility studies, site selection, compliance evaluations, setup, import permits, project oversight, and reporting to guarantee a smooth process.
Specialists such as Ana Criado and Katherine Ruiz play essential roles in navigating the regulatory environment, offering invaluable advice that improves the success of research studies in Colombia.
Best Practices for Successful Clinical Trials in Latin America
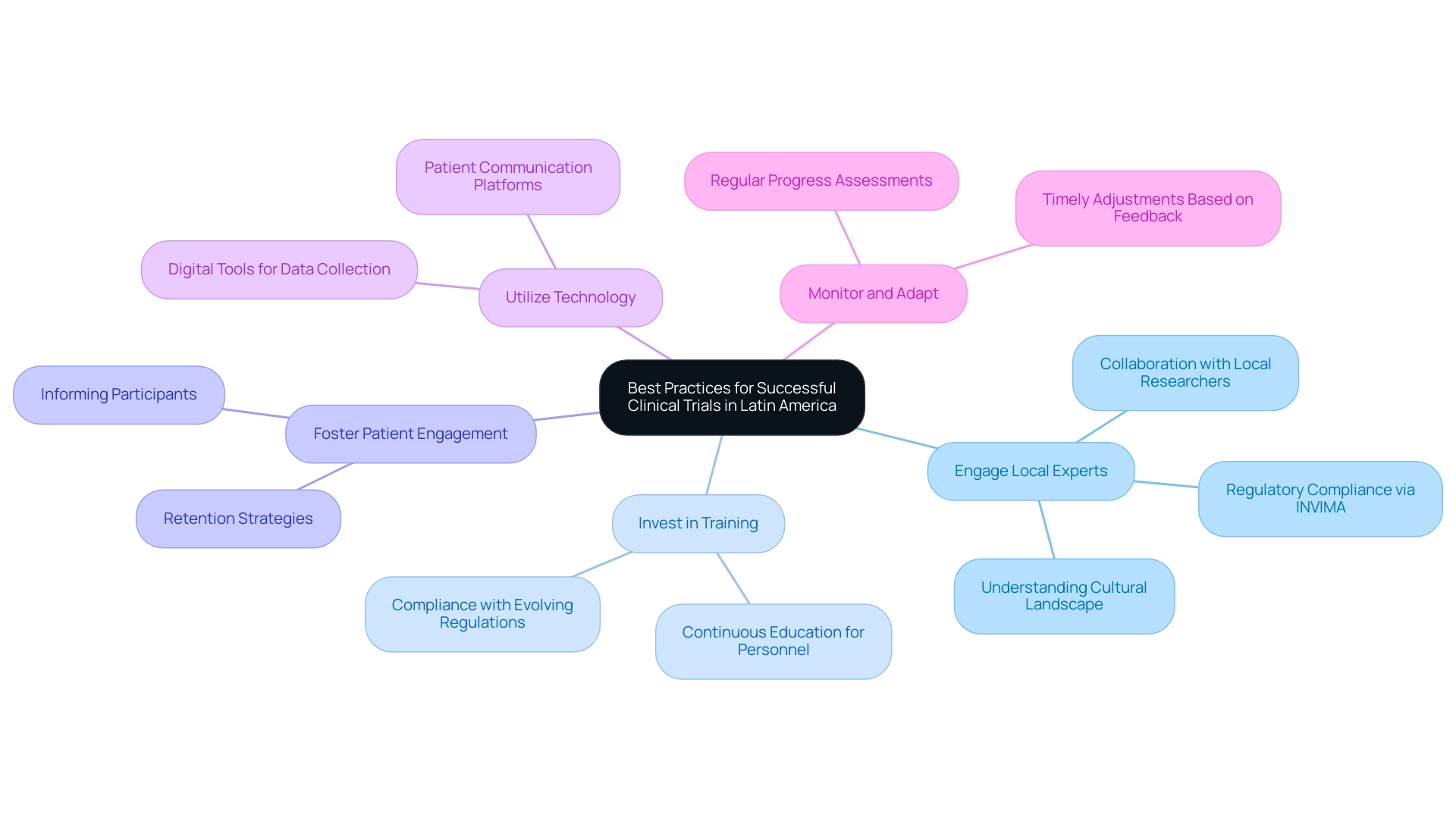
To enhance the success of clinical studies and support medical trial growth in Latin America, several best practices should be prioritized:
- Engage Local Experts: Collaborating with local researchers is essential, as they possess a deep understanding of the cultural and regulatory landscape, which can significantly influence study outcomes. This is particularly vital in the context of Colombia, where the National Food and Drug Surveillance Institute (INVIMA) serves as a Level 4 health authority, overseeing medical device regulations and ensuring compliance.
- Invest in Training: Continuous education for research personnel not only enhances study execution but also ensures compliance with evolving regulations.
- Foster Patient Engagement: Implementing effective strategies to keep participants informed and engaged throughout the study process is crucial for retention and data integrity.
- Utilize Technology: Leveraging digital tools for data collection and patient communication can enhance efficiency and streamline operations, facilitating better project management and monitoring.
- Monitor and Adapt: Regularly assessing the progress of the study allows for timely adjustments based on feedback and emerging data, ultimately improving its quality.
As emphasized by the Pan American Health Organization (PAHO), 'As part of the execution of the World Health Assembly’s resolution WHA 75.8, PAHO gathered over 50 attendees from various nations of the Americas in the workshop Strengthening experimental studies to provide high-quality evidence on health interventions, and to enhance study quality and coordination.' This highlights the dedication to improving the quality of studies in the region. Moreover, the creation of the Regional Forum of Research Regulators seeks to promote cooperation among research regulators, enhancing regulatory alignment and improving supervision, which is essential for the successful implementation of studies in the area.
Significantly, yearly funding in the healthcare investigation field in the Andean Region increased from $3-4 million to more than $50 million, which underscores the medical trial growth in Latin America and the rising significance of medical studies in South America. Julio Martinez-Clark, CEO of bioaccess, plays a vital role in fostering medical trial growth in Latin America by supporting over 100 Medtech companies in implementing successful trials. His emphasis on guiding startups and advocating for regional opportunities underscores the collaborative efforts required to enhance research in South America.
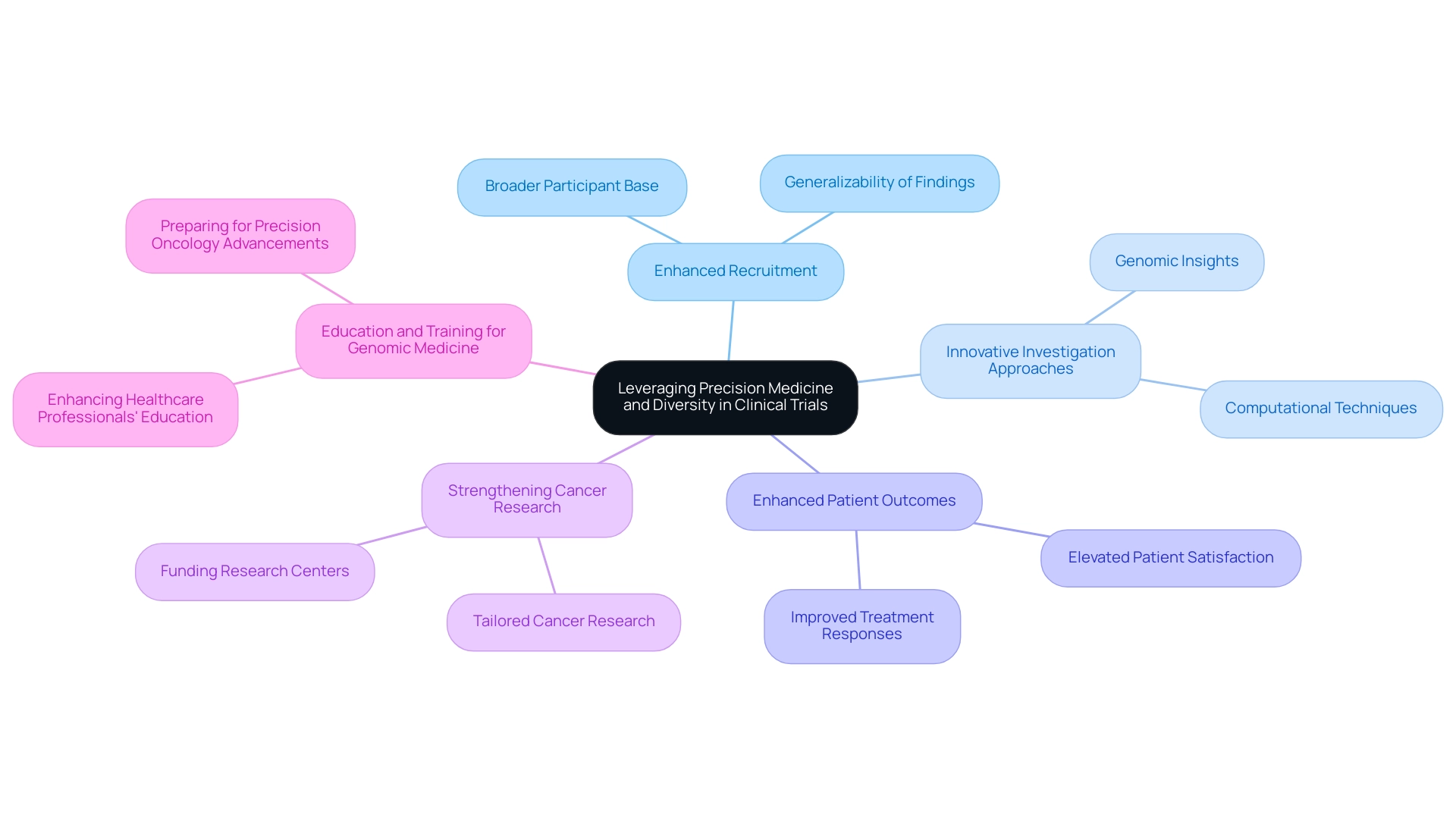
Leveraging Precision Medicine and Diversity in Clinical Trials
Precision medicine seeks to customize treatments based on individual characteristics, a goal that holds particular relevance in Latin America due to its rich ethnic diversity. Harnessing this diversity offers several key advantages, with medical trial growth in Latin America enabling a deeper understanding of genetic variations across various ethnic groups, which can significantly improve treatment efficacy.
- Enhanced Recruitment: By prioritizing diversity in research trials, researchers can contribute to the medical trial growth in Latin America by involving a broader participant base, which is essential for the generalizability of findings.
- Innovative Investigation Approaches: The combination of conventional medical studies with genomic insights and computational techniques promotes new exploration paths that can improve understanding.
- Enhanced Patient Outcomes: Tailoring interventions to meet the specific needs of diverse populations can lead to improved treatment responses, ultimately elevating patient satisfaction and overall health outcomes.
Recent discussions emphasize the need for strengthening and funding cancer research centers in South America to facilitate medical trial growth in Latin America, which is essential for enhancing cancer research tailored to the region's specific needs.
Furthermore, a literature review of articles published between 2000 and 2019 provides a historical perspective on the evolution of precision medicine in the region. As highlighted in the case study titled 'Education and Training for Genomic Medicine,' there is a pressing need to enhance the education of healthcare professionals regarding genomic medicine and computational methods for oncology. Improving training will help prepare healthcare workers for advancements in precision oncology, ultimately benefiting patient care.
Future Trends and Opportunities in Latin American Clinical Trials
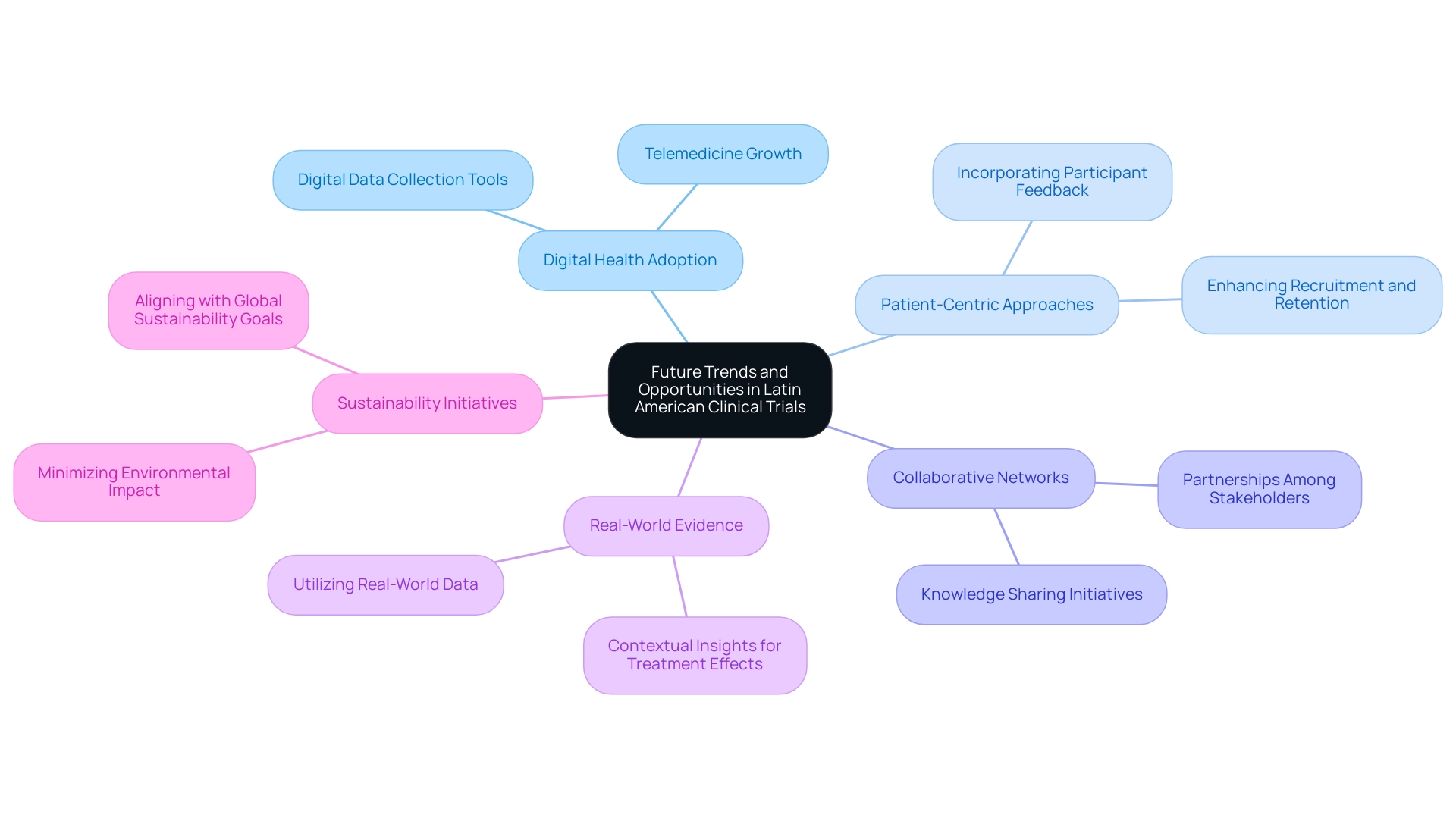
The future of clinical studies in Latin America appears increasingly promising, driven by medical trial growth in Latin America and several key trends set to shape the landscape:
-
Increased Adoption of Digital Health: The rise of telemedicine and digital data collection tools is anticipated to facilitate remote participation, enhancing accessibility and efficiency in clinical studies. This shift aligns with the growing demand for innovative solutions in healthcare delivery.
-
Greater Focus on Patient-Centric Approaches: There is a notable shift toward prioritizing the patient experience, with researchers expected to incorporate participant feedback into study designs.
This approach not only enhances recruitment and retention but also guarantees that studies are more pertinent to patient needs.
-
Expansion of Collaborative Networks: Strengthening partnerships among academic institutions, industry stakeholders, and healthcare providers will be crucial in fostering innovation and knowledge sharing.
Collaborative efforts can enhance study feasibility and support the development of tailored interventions, particularly through comprehensive services such as feasibility studies, site selection, and compliance reviews.
-
Emphasis on Real-World Evidence: Utilizing real-world data to enhance conventional study findings will deepen the comprehension of treatment effects and enhance decision-making processes.
This method is particularly valuable in a region where diverse disease trends demand contextually relevant insights, further supported by effective project management and thorough reporting of study status, inventory, and adverse events.
-
Sustainability Initiatives: A growing emphasis on sustainable practices in research will aim to minimize environmental impact while maximizing patient benefit.
This trend reflects a broader commitment within the industry to align with global sustainability goals.
Remarkably, 30% of the population in South America is below 14 years old, establishing a substantial market for pediatric studies. As highlighted by industry expert Murray Aitken, the composite success rate for trial pipelines has experienced a positive shift, with success rates in Phase I increasing to 48% and Phase III to 66%, exceeding pre-pandemic averages.
This upward trajectory, alongside the region’s substantial pediatric population and rising incidence of chronic diseases such as gastric carcinoma and gallbladder cancer, positions Latin America as a vital hub for medical trial growth in Latin America, supported by international collaboration and innovation in Medtech.
Conclusion
The landscape of clinical trials in Latin America is marked by significant growth, driven by diverse patient populations, cost-effective research opportunities, and advancements in regulatory frameworks. Countries like Brazil, Mexico, and Argentina are leading the way, attracting investment and fostering innovative research that addresses both local and global health challenges. The region's unique demographics and evolving healthcare infrastructure create a promising environment for clinical research, particularly in therapeutic areas that require diverse representation.
However, this promising landscape is accompanied by notable challenges, including regulatory variability, cultural differences, and infrastructure gaps. These hurdles necessitate careful navigation to ensure successful trial outcomes. Researchers are encouraged to engage with local experts and invest in training to enhance the quality and efficiency of clinical trials. Additionally, fostering patient engagement and leveraging technology can significantly improve recruitment and retention rates.
Looking ahead, the future of clinical trials in Latin America appears bright, with trends such as increased adoption of digital health, a greater focus on patient-centric approaches, and an emphasis on real-world evidence set to shape the industry. The region's rich ethnic diversity, coupled with a commitment to sustainable practices, positions Latin America as a vital hub for innovative clinical research. As the sector continues to evolve, collaboration among stakeholders will be essential to harness the full potential of this dynamic landscape, ultimately leading to improved health outcomes for diverse populations and a stronger global clinical trials framework.
Frequently Asked Questions
What is the current status of medical trial growth in Latin America?
Latin America has become an essential participant in the global research landscape, accounting for 3.5% of the worldwide research matching software market in 2023, with significant growth potential driven by diverse patient demographics and improving healthcare infrastructure.
Which countries in Latin America are leading in medical trial growth?
Brazil, Mexico, and Argentina are at the forefront of medical trial growth in Latin America, hosting numerous studies across various therapeutic areas.
What factors contribute to the attractiveness of Latin America for medical trials?
Key factors include a large pediatric population, a growing elderly demographic, increased funding in the research sector, favorable regulatory frameworks, and cost-effective studies compared to North America and Europe.
How has funding in the research sector changed in the Andean Region?
Funding in the research sector has increased from $3-4 million to over $50 million each year, particularly in Peru, Colombia, and Chile, attracting both domestic and foreign sponsors.
What are some challenges faced by US Medtech companies in Latin America?
Challenges include language barriers, fragmentation of resources, and the need for effective communication with American hospitals.
Why is cooperation between Medtech firms and CROs important?
Cooperation is crucial for addressing challenges, enabling expedited study results, and connecting innovation with implementation in the medical trial landscape.
What role does diversity in patient populations play in medical trials in Latin America?
The diverse patient populations in Latin America, with rich genetic backgrounds, are essential for studying various diseases and their responses to treatments, promoting inclusive representation in studies.
What improvements have been made in regulatory frameworks in Latin America?
The region has seen progress in regulatory frameworks that facilitate more efficient initiation and execution of research studies, enhancing opportunities for medical trials.
How does investment in healthcare infrastructure impact medical trials?
Investment in healthcare infrastructure strengthens the ability to perform high-quality studies, which is vital for attracting international evaluations and supporting the growth of medical trials.
What is the significance of local knowledge and skilled professionals in medical trials?
An increasing pool of skilled professionals enhances the region's capacity to manage complex studies effectively, contributing to the overall growth of medical trials in Latin America.

