Introduction
In the dynamic landscape of medical device development, understanding the regulatory environment is paramount for innovators seeking to navigate the complexities of approval processes. In the Dominican Republic, the Ministry of Public Health (MISPAS) plays a critical role in overseeing these regulations, particularly through Law No. 42-01, which outlines comprehensive requirements for device registration and market authorization.
With an impressive approval rate of 85% in the past year, MISPAS has demonstrated a commitment to fostering innovation while ensuring patient safety. This article delves into the intricate interplay of regulatory frameworks, clinical trials, and post-market surveillance that shape the pathway for medical devices, highlighting the essential steps that researchers and manufacturers must undertake to achieve successful outcomes in a competitive and rapidly evolving field.
Navigating the Regulatory Landscape for Medical Device Approval in the Dominican Republic
In the Dominican Republic, pivotal studies for medical device approval are primarily managed by the Ministry of Public Health (MISPAS) within the regulatory framework for health equipment approval. For clinical researchers and sponsors, a thorough understanding of key regulations, particularly Law No. 42-01 on Health Products, is essential.
This legislation outlines the requirements for the registration and market approval of health-related products, including the pivotal studies for medical device approval in the Dominican Republic, detailing the necessary documentation and evaluation process. With an impressive approval rate of 85% for health equipment under MISPAS in the past year, the process demonstrates a level of efficiency that is beneficial for pivotal studies for medical device approval in the Dominican Republic. Dr. Maria Gonzalez, a renowned expert in medical equipment regulations, emphasizes, 'Law No. 42-01 has significantly streamlined the approval process, making it more accessible for innovators in the healthcare sector.'
Moreover, the National Health Research Ethics Committee is tasked with supervising pivotal studies for medical device approval in the Dominican Republic, ensuring that all investigations adhere to established ethical standards and safeguard patient rights. The experimental arrangement involves acquiring ethics committee consent and securing import permits for research instruments, which are essential stages in the approval process.
A recent case analysis on the authorization of a cardiac instrument demonstrated that pivotal studies for medical device approval in the Dominican Republic, along with strict compliance with MISPAS regulations, not only enabled a smoother approval process but also improved patient safety outcomes. Acquaintance with these regulatory frameworks, along with extensive clinical research management services—including feasibility assessments, site selection, compliance evaluations, setup, import permits, project oversight, and thorough reporting on research status and adverse events—allows clinical researchers to maneuver through the approval process efficiently, thus enhancing the chances of favorable results in crucial investigations.

Key Clinical Studies and Ethical Considerations in Medical Device Approval
Crucial studies aimed at obtaining medical equipment approval in the Dominican Republic primarily depend on pivotal studies for medical device approval Dominican Republic, which are broadly acknowledged as the gold standard in clinical research. These experiments must be meticulously designed to convincingly demonstrate both the safety and efficacy of the device under investigation. Notably, if 20 independent subgroups of a frequentist study are each tested at a Type I error level of 5%, the chance of at least one falsely significant result can be as high as 64%.
This statistic highlights the significance of thorough research design in reducing bias and guaranteeing valid results.
In the context of clinical evaluations, bioaccess® provides extensive services customized to simplify the process, including:
- Feasibility assessments
- Site selection
- Compliance reviews
- Setup
- Import permits
- Project management
- Reporting
With over 20 years of expertise in managing various investigations—such as Early-Feasibility Investigations (EFI), First-In-Human Investigations (FIH), Pilot Investigations, and Pivotal Studies for Medical Device Approval Dominican Republic, as well as Post-Market Clinical Follow-Up Investigations (PMCF)—bioaccess® is well-equipped to navigate the complexities of clinical research in Latin America, utilizing a customized approach to meet the unique needs of each investigation.
Ethical considerations play a critical role in this process; researchers must prioritize elements such as informed consent and patient confidentiality throughout the investigation. It is essential that all participants receive comprehensive information regarding the nature, benefits, and risks associated with the research prior to giving their consent. Moreover, strict adherence to Good Clinical Practice (GCP) guidelines is crucial, as these standards ensure that clinical trials are conducted in a manner that is both ethically sound and scientifically robust.
This adherence not only safeguards the integrity of the research but also upholds the rights of participants, thereby fostering trust in the clinical research process.
An example of a hierarchical model can be utilized to combine success probabilities from earlier investigations with a new investigation, assuming exchangeability at different levels. This approach provides valuable information about the success probability in the current research while acknowledging differences between patient groups. Recognizing the biases and assumptions that can affect RCT outcomes, such as the constant background traits and the limitations linked to treatment effects, is essential for designing effective research that yields reliable results.
As highlighted by experts, these biases include:
- The unique time period assessment bias
- The average treatment effects limitation
- The preconditions that must be fully met assumption
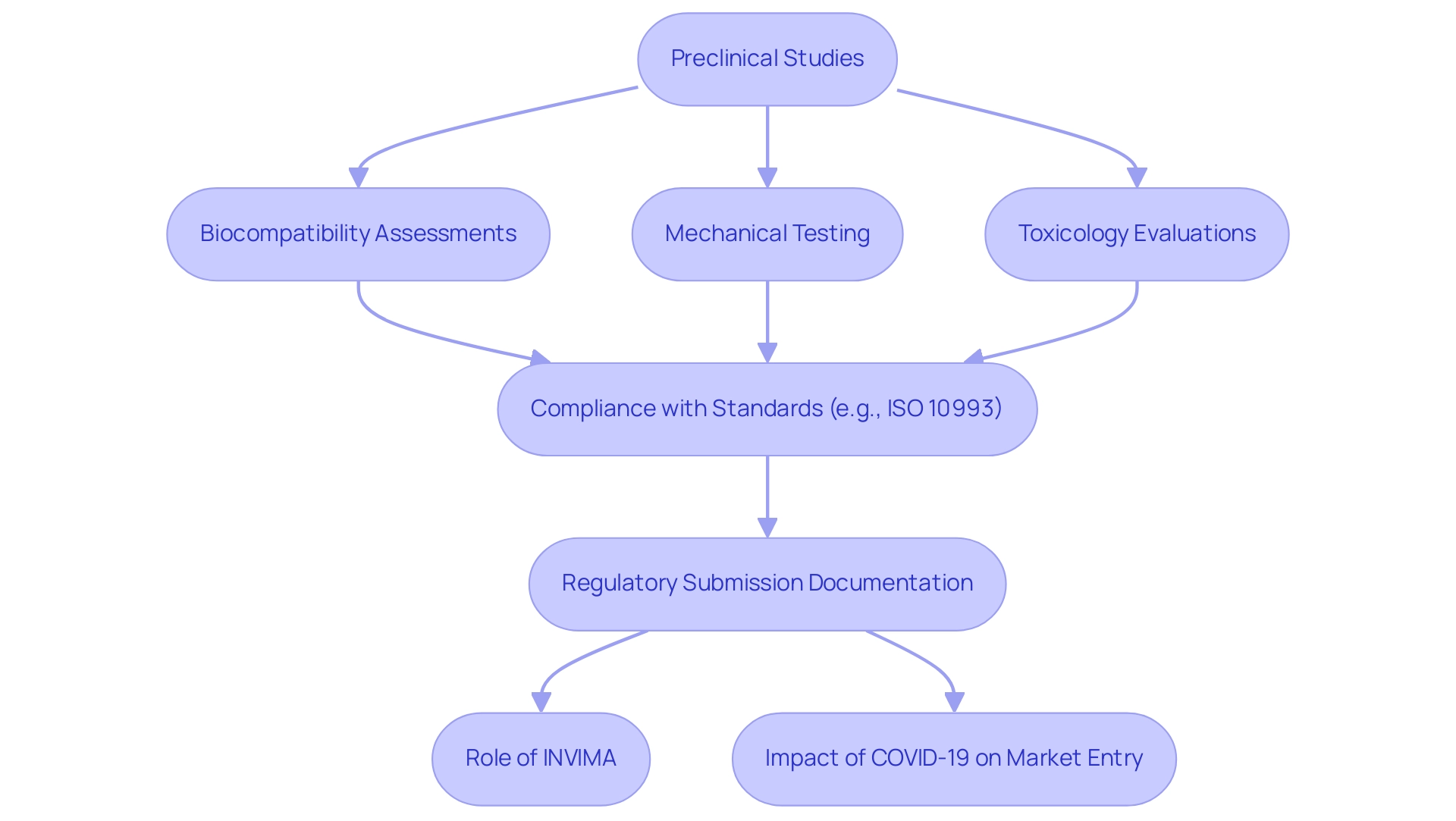
Importance of Preclinical Studies in Medical Device Development
Preclinical investigations act as a foundational phase in the development of medical devices, employing both laboratory and animal testing to assess safety and efficacy. These investigations are crucial in identifying potential risks and establishing suitable dosage parameters prior to human trials. Notably, the chance of at least one falsely significant result can be as high as 64% if 20 independent subgroups are each tested at a Type I error level of 5%, underscoring the necessity for rigorous testing and data integrity in preclinical research.
Among the key components of these studies are:
- Biocompatibility assessments
- Mechanical testing
- Toxicology evaluations
The results of biocompatibility testing are particularly vital, as they must comply with international standards, such as ISO 10993, which regulates the biological assessment of healthcare instruments. In Colombia, regulatory oversight is provided by INVIMA (Instituto Nacional de Vigilancia de Medicamentos y Alimentos), a Level 4 health authority recognized by the Pan American Health Organization and the World Health Organization.
INVIMA is responsible for ensuring that healthcare equipment meets safety and efficacy standards, monitoring and controlling such equipment, and suggesting technical standards for their manufacturing and marketing. This reinforces the importance of compliance during preclinical testing, as researchers must ensure that their preclinical data is comprehensive and compliant. This not only substantiates the safety profile of the equipment but also constitutes a vital part of the regulatory submission documentation.
Katherine Ruiz, a specialist in regulatory matters for healthcare products, emphasizes the importance of effectively navigating INVIMA's requirements to attain successful market entry. The impact of the COVID-19 pandemic on drug development has further highlighted the importance of rapid response in preclinical studies, illustrating how timely assessments can facilitate swift market entry during public health emergencies. Additionally, as noted by the Congressional Budget Office, private spending on pharmaceutical R&D and the approval of new drugs have both increased markedly in recent years, emphasizing the financial implications of thorough preclinical testing.
By prioritizing rigorous preclinical testing, developers can significantly enhance their chances of successful regulatory approval and market entry.
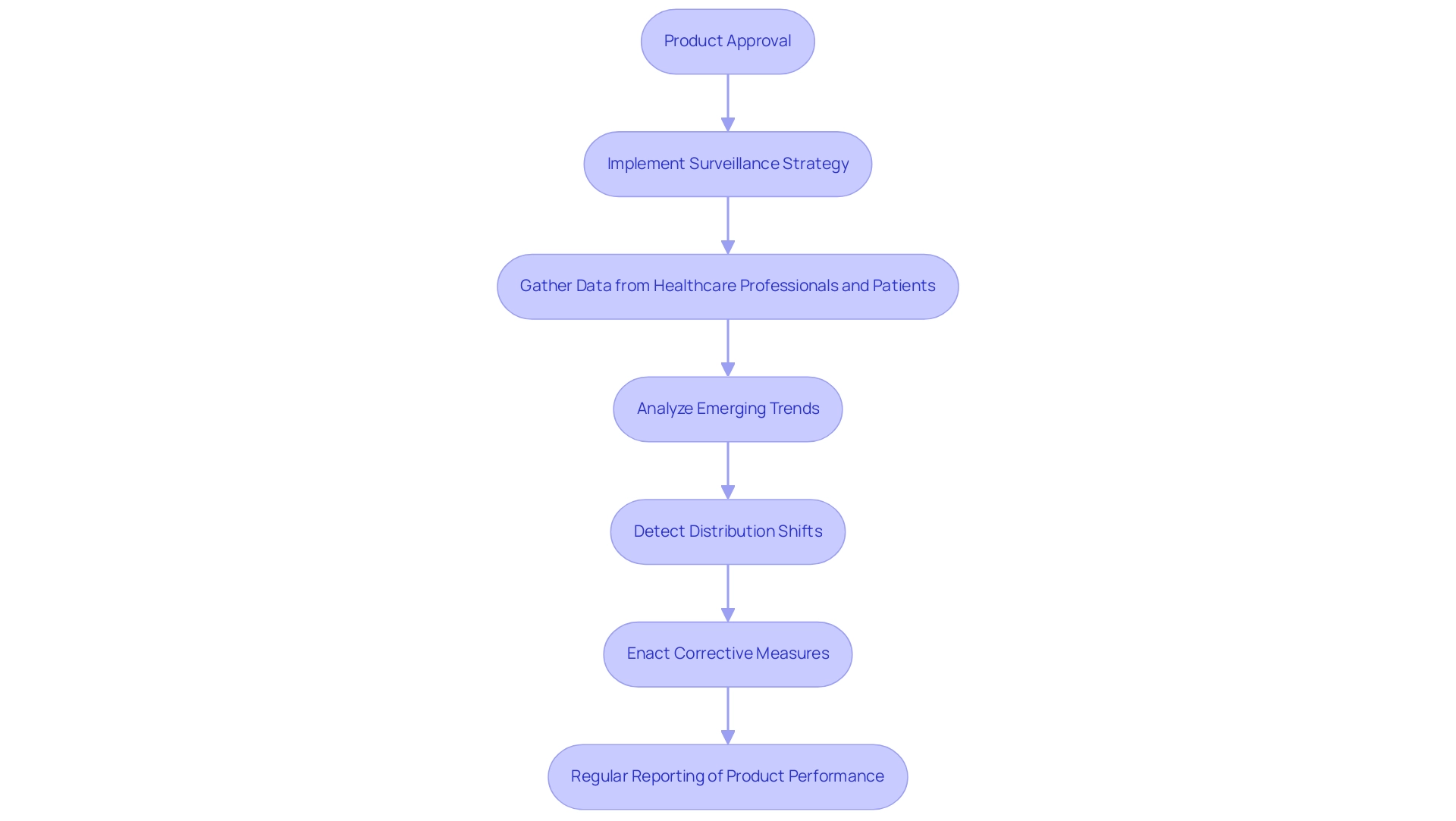
Post-Market Surveillance and Reporting Obligations
Following the approval of a healthcare product, manufacturers must implement a comprehensive post-market surveillance strategy to monitor its performance and document any adverse events, as mandated by INVIMA, the Colombia National Food and Drug Surveillance Institute. Established in 1992, INVIMA plays a crucial role in overseeing the marketing and manufacturing of health products, ensuring compliance with local regulations. This surveillance process entails gathering data from healthcare professionals and patients, analyzing emerging trends, and enacting corrective measures when necessary.
'INVIMA's Directorate for Health Products and other Technologies is particularly accountable for overseeing and regulating health equipment, monitoring pre- and post-market initiatives, and recommending technical standards for production, promotion, and quality assurance of products. As a Level 4 health authority acknowledged by the Pan American Health Organization/World Health Organization, INVIMA's regulations necessitate regular reporting on product performance, which encompasses any safety incidents that arise. In 2024, post-market surveillance statistics indicate an increasing emphasis on accurate adverse event reporting, highlighting the critical need for manufacturers to establish a rigorous surveillance plan that complies with INVIMA's standards while prioritizing patient safety.
It is essential to note that shift detection methods have proven more effective with sample sizes of 300 or fewer, which is crucial for understanding the methodologies employed in post-market surveillance. As Berens, P. highlights, the effective identification of distribution shifts in healthcare AI algorithms is essential for ensuring equipment safety in the post-market phase. The main evaluation criteria for the shift detection methods include the shift detection rate, which measures the probability of correctly identifying a distribution shift, alongside the false positive rate.
Furthermore, recent case studies, such as 'Sensitivity to Subgroup Shift Strength,' illustrate that more pronounced shifts in performance correlate with higher detection rates of adverse events, emphasizing the necessity for ongoing vigilance and responsiveness in monitoring. Katherine Ruiz, a specialist in regulatory matters for health-related products and in vitro diagnostics in Colombia, highlights the significance of following these regulatory frameworks to guarantee safe and effective health products in the market.
The Role of Clinical Trials in Accelerating Medical Innovation
Pivotal studies for medical device approval in the Dominican Republic serve as a foundation in the medical equipment approval process, providing vital information that confirms a product's safety and effectiveness. These investigations are instrumental in identifying both potential risks and benefits, allowing researchers to make necessary refinements to the device. Through the execution of well-structured clinical studies, especially the pivotal studies for medical device approval in the Dominican Republic, facilitated by experienced teams such as bioaccess®, manufacturers can significantly reduce the time to market for innovative technologies, thereby enhancing patient care outcomes.
bioaccess® specializes in managing various types of studies, including:
- Early-Feasibility Studies (EFS)
- First-In-Human Studies (FIH)
- Pilot Studies
- Pivotal Studies for Medical Device Approval Dominican Republic
This ensures a comprehensive approach to clinical research. It is essential for all stakeholders—including manufacturers and regulatory agencies—to recognize the strategic importance of clinical studies. These experiments not only supply the scientific proof required for informed decision-making but also promote progress in healthcare tools that can result in better health outcomes.
The function of INVIMA as a Level 4 health authority, supervising regulations for health equipment in Colombia, emphasizes the significance of adherence and supervision in this process. Moreover, the continuous partnership between Greenlight Guru and bioaccess™ seeks to expedite Medtech advancements and clinical research in Latin America, illustrated by successful results such as PAVmed's first in-human study in Colombia. As highlighted in recent discussions, the global commitment to optimizing medical equipment regulations and assessments by institutions like WHO, CENETEC in Mexico, and CECMED in Cuba further advances health technology in diverse settings.
Furthermore, the recent appeal for submissions of innovative health technologies for low-resource environments highlights the essential role of clinical studies in tackling global health issues. As mentioned by an anonymous commenter, 'Patients would tend to believe a study listed in the data bank indicates that the investigational device is promising,' which emphasizes the importance of transparency and credibility in clinical research. The processes involved in trial setup and management, including feasibility assessments, site selection, and compliance reviews, are crucial for ensuring successful outcomes and maintaining the integrity of the research.
Conclusion
The regulatory environment for medical device approval in the Dominican Republic is a multifaceted landscape shaped by the Ministry of Public Health (MISPAS) and its pivotal Law No. 42-01. This legislation not only streamlines the registration and market authorization process but also emphasizes the importance of rigorous clinical research, preclinical studies, and post-market surveillance. With an impressive approval rate of 85%, MISPAS demonstrates a commitment to fostering innovation while prioritizing patient safety.
Understanding the intricacies of clinical trials is essential for researchers and manufacturers alike. The emphasis on randomized controlled trials as the gold standard reflects the necessity for meticulous study design to ensure valid outcomes. Additionally, ethical considerations such as informed consent and adherence to Good Clinical Practice (GCP) guidelines are crucial for maintaining the integrity of the research and protecting participant rights. Preclinical studies lay the groundwork for safe and effective device development, while robust post-market surveillance ensures ongoing monitoring of device performance and patient safety.
Ultimately, the successful navigation of this regulatory framework not only enhances the likelihood of obtaining market authorization but also significantly contributes to advancements in medical technology that can improve health outcomes. As the landscape continues to evolve, maintaining compliance with established regulations and prioritizing ethical research practices will be paramount for innovators aiming to thrive in this competitive field. By embracing these principles, stakeholders can play a vital role in the future of medical devices, ensuring that innovations are both safe and effective for patients in need.
Frequently Asked Questions
What is the primary regulatory body for medical device approval in the Dominican Republic?
The primary regulatory body for medical device approval in the Dominican Republic is the Ministry of Public Health (MISPAS).
What legislation governs the registration and market approval of health-related products in the Dominican Republic?
Law No. 42-01 on Health Products governs the registration and market approval of health-related products in the Dominican Republic.
What is the approval rate for health equipment under MISPAS in the past year?
The approval rate for health equipment under MISPAS in the past year was 85%.
What role does the National Health Research Ethics Committee play in the approval process?
The National Health Research Ethics Committee supervises pivotal studies for medical device approval, ensuring adherence to ethical standards and safeguarding patient rights.
What are the key components involved in pivotal studies for medical device approval?
Key components include acquiring ethics committee consent, securing import permits for research instruments, and thorough documentation of the study process.
How does thorough research design impact the validity of clinical evaluations?
Thorough research design reduces bias and guarantees valid results, as highlighted by the statistic that the chance of at least one falsely significant result can be as high as 64% in certain study conditions.
What services does bioaccess® provide to facilitate clinical evaluations?
Bioaccess® provides services such as feasibility assessments, site selection, compliance reviews, setup, import permits, project management, and reporting.
What are some ethical considerations that researchers must prioritize during clinical investigations?
Researchers must prioritize informed consent and patient confidentiality, ensuring participants receive comprehensive information about the research's nature, benefits, and risks.
Why is adherence to Good Clinical Practice (GCP) guidelines important?
Adherence to GCP guidelines is crucial to ensure clinical trials are conducted ethically and scientifically robust, safeguarding the integrity of the research and the rights of participants.
What is the significance of preclinical investigations in the development of medical devices?
Preclinical investigations assess safety and efficacy through laboratory and animal testing, identifying potential risks and establishing suitable dosage parameters before human trials.
What are the responsibilities of INVIMA in Colombia regarding health products?
INVIMA oversees the marketing and manufacturing of health products, ensures compliance with local regulations, and monitors pre- and post-market initiatives.
What is required from manufacturers after the approval of a healthcare product?
Manufacturers must implement a comprehensive post-market surveillance strategy to monitor product performance and document any adverse events, as mandated by INVIMA.
How does the partnership between Greenlight Guru and bioaccess™ benefit Medtech advancements in Latin America?
The partnership seeks to expedite Medtech advancements and clinical research, leading to successful outcomes such as first-in-human studies.
What is the strategic importance of clinical studies in the medical device approval process?
Clinical studies provide the scientific proof necessary for informed decision-making and promote progress in healthcare tools, ultimately leading to better health outcomes.




