Introduction
Pivotal trials play a vital role in advancing medical science by evaluating the efficacy and safety of novel medical interventions. These meticulously designed studies provide high-quality evidence that informs regulatory decisions and clinical guidelines. The importance of pivotal trials is underscored by their rigorous peer-review process and their ability to shape medical practice.
Strategic choices in titling, abstract writing, and keyword selection optimize the impact and dissemination of pivotal trial findings. Adherence to stringent authorship criteria ensures accountability and proper attribution of contributions. While pivotal trials are indispensable for generating actionable knowledge, they are just one component of a patient's care continuum.
It is crucial to understand the distinction between trial standardization and individualized clinical care to effectively apply trial findings in practice. In this article, we will explore the design and conduct of pivotal trials, the challenges they face, ethical considerations, their impact on regulatory approval, their relationship with real-world evidence, and their role in advancing medical knowledge.
The Role of Pivotal Trials in Clinical Research
Pivotal studies are integral to advancing medical science, particularly in evaluating the efficacy and safety of novel medical interventions. These studies are meticulously designed to follow up on promising preliminary data, culminating in high-quality evidence that informs regulatory decisions and clinical guidelines. Distinguished by their range, pivotal experiments often include numerous centers and demand a collective endeavor from various stakeholders to guarantee the integrity and validity of the research. The significance of these experiments is emphasized by the thorough peer-review process they undergo before being published, a testament to their crucial role in shaping medical practice.
To maximize the influence and spread of pivotal study findings, strategic decisions in titling, abstract writing, and keyword selection are crucial. This approach enhances the accessibility and searchability of the research, increasing its visibility and usage in practice. Furthermore, the adherence to stringent authorship criteria, as outlined by the International Committee of Medical Journal Editors (ICMJE), ensures accountability and proper attribution of contributions.
The field of clinical experiments is also characterized by developing approaches, as demonstrated by recent investigations into non-inferiority experiments. These experiments aim not only to establish a new treatment as a viable alternative but also to highlight additional benefits that may make it preferable over existing options. The comprehensive design, including the careful setting of non-inferiority margins and selection of secondary outcomes, leads to robust analyses and well-founded conclusions.
However, the journey from trial to treatment is not without its challenges. A recent collaboration with Consilium Scientific highlighted the variable quality of evidence that influences healthcare decision-making. The study found cases where the quality of life information was below standard, and the evidence used did not sufficiently represent the population or treatment methods. This requires a continuous endeavor to generate and depend on top-notch medical information, both before and after the market, to genuinely benefit individuals.
As we progress, it is essential to acknowledge that while pivotal experiments are necessary for producing actionable information, they are just one element of a person's care continuum. As beautifully expressed in a quote from clinicaltrials.gov, experiments are research endeavors to evaluate interventions' effects on humans. Still, they cannot always claim to offer the best management for every patient scenario. The differentiation between standardization of experiments and personalized healthcare is crucial in comprehending and implementing research findings in practical settings.
In celebrating the contributions of statisticians to medicine, as highlighted in the 40th anniversary of Statistics in Medicine, we reflect on the pivotal role of biostatistical sciences in the development of medical research. The ongoing dialogue among experts and the publication of methodological advancements reinforce the significance of statistics in the rigorous evaluation and interpretation of medical research.
In conclusion, pivotal experiments are cornerstone research efforts that, through scientific rigor and transparency, help shape the future of patient care. Their findings, when effectively communicated and thoroughly vetted, hold immense potential to guide medical decisions and improve health outcomes.
Design and Conduct of Pivotal Trials
Significant experiments are vital in the field of clinical research, requiring careful planning to maintain the highest scientific criteria. These experiments are frequently extensive undertakings, enlisting numerous participants who are randomly sorted into different groups. For instance, the experimental group may receive the novel treatment being tested, while the control group might receive a placebo or the standard care. The experiment's blueprint, known as the protocol, meticulously details the study's goals, who can participate, the treatments to be administered, and the outcomes being measured.
A characteristic of these experiments is the double-blind structure—neither the participants nor the investigators know which group is receiving the new treatment, which helps to eliminate bias. The statistical rigor of these trials is echoed by Professor Emeritus of Biostatistics at the University of Washington, who highlights the complexity of designs like the stepped-wedge, where clusters are randomized and each receives the treatment at different intervals. This design demands precise definitions of what is being measured and considers the magnitude of effect for adequate power.
The industry is witnessing a shift towards patient-centered drug development, leveraging information from connected devices and advanced AI-driven methodologies. This extensive range of information, spanning from lab results to patient-reported outcomes, can offer deeper insights and identify trends to steer more informed drug development decisions. However, it requires a proactive data strategy, clearly defined prior to the experiment's beginning, to manage this data effectively.
Furthermore, the worldwide scenario of clinical experiments encounters obstacles such as inadequate design and limited participant diversity, frequently resulting in discrepancies between high-income and lower-income areas. In 2022, the amount of experiments in high-income countries slightly exceeded those in low- and middle-income countries, with less than 5% of experiments involving pregnant women and only 13% including children. Efforts to enhance country-led research and integrate experiments into routine services are crucial for fair, effective interventions.
In summary, carrying out a crucial study is a intricate, multi-faceted process with significant ethical and scientific implications. From the initial design to participant recruitment and data analysis, every step must be carefully considered to ensure the integrity and success of the experiment.
Challenges in Pivotal Trials
Key clinical experiments are crucial for progressing medical understanding and improving healthcare, but they face notable obstacles, especially with regards to participant diversity and recruitment. Representativeness in demographics, such as age, ethnicity, and socioeconomic status, is crucial for the generalizability of trial outcomes. For instance, older individuals, who frequently require hospital care and typically present with multiple health conditions, are markedly underrepresented in research studies. The busy and demanding environment of hospital settings presents difficulties in enrolling these individuals, particularly when urgent medical care is needed. Researchers must be persistent, revisiting patients multiple times if necessary, and often engage with patients' family members, who may need to consent on behalf of those unable to do so due to cognitive impairments like dementia.
Ensuring the integrity of experiment data and managing potential biases are pivotal to maintaining the quality of research. Bias can arise from non-representative sample populations, leading to skewed results and potentially contributing to health inequities. The intricacy of conducting these experiments is further emphasized by the need to manage logistical concerns, such as the distribution and costs associated with investigational products, as well as maintaining compliance with regulatory standards. As the medical community continues to learn from past public health emergencies, such as the COVID-19 pandemic, the significance of adaptive and resilient experimental designs has become increasingly apparent. These designs are necessary to mitigate the impacts of unforeseen disruptions and to ensure the safety and efficacy evaluations remain robust despite protocol deviations or statistical challenges. Clinical experiments, therefore, are not just about assessing new treatments; they are also about embracing methodological rigor and ethical considerations to ensure that the findings can truly inform patient care and medical practice.
Ethical Considerations in Pivotal Trials
The integrity of crucial experiments is essentially based on ethical considerations, which act as a guiding compass in both their design and implementation. A central tenet of this ethical framework is the safeguarding of participant rights and welfare, which demands rigorous adherence to the principles of informed consent, voluntary participation, and the safeguarding of personal data. The administration of these experiments often involves a cooperative endeavor, with autonomous ethics committees or institutional review boards carefully scrutinizing protocols to guarantee ethical integrity and regulatory adherence.
Current trends highlight the significance of inclusivity and diversity in medical experiments. Data from 2022 shows a difference, with 27,133 experiments carried out in high-income countries compared to 24,791 in low- and middle-income countries, emphasizing a global imbalance. This gap highlights the requirement for fair and comprehensive research practices that guarantee results are relevant to a wider population, encompassing marginalized communities like expectant mothers and minors, who are involved in less than 5% and 13% of research studies correspondingly.
Moreover, ethical perspectives are evolving, with a growing focus on fair treatment of participants. It is increasingly recognized that participants should not bear the cost of contributing to public health advancements. As such, fair compensation for research-related expenses, time, and potential risks is advocated, drawing parallels to the compensation models for public servants like firefighters.
The Declaration of Helsinki, a cornerstone document in medical research ethics, is currently under review, signaling an opportunity to address long-standing ethical concerns and align more closely with the principles of participant best interest. In addition, innovative designs such as Thompson Sampling are being explored, which customize treatment assignment to the likelihood of a treatment being the most beneficial, demonstrating a shift from traditional methods towards more participant-centric approaches.
The drive for openness in medical experiments is also gathering pace, with anticipation for public access to experiment protocols and information. Nevertheless, there is variation in the commitments to openness, and the exchange of unprocessed information remains an aspect with space for enhancement, as demonstrated by the reality that industry-sponsored experiments are not uniformly subjected to external analysis.
Overall, ethical considerations in crucial experiments are not fixed; they are constantly changing with the technological, social, and regulatory environments, influencing the future of clinical research with a focus on fairness, inclusiveness, and transparency.
The Impact of Pivotal Trials on Regulatory Approval
Significant experiments serve as the basis upon which regulatory bodies, such as the Food and Drug Administration (FDA) in the US and the Medicines and Healthcare products Regulatory Agency (MHRA) in the UK, evaluate the safety and efficacy of medical interventions. The thoroughness and results of these experiments are crucial, as they can determine whether a new treatment receives approval or requires further investigation. For example, the MHRA, which oversees medicine regulation in the UK, emphasizes a pragmatic approach to assessments and offers guidance to applicants to streamline the Clinical Trial Authorisation process.
FDA regulatory compliance is complex and multifaceted, impacting both the cost and timeline of drug development. The agency's role extends to ensuring that all medications, including innovative drugs that provide new treatment options, meet stringent standards before reaching the public. The Center for Drug Evaluation and Research (CDER) plays an integral role in this process, which can span from 12 to 15 years, depending on the thoroughness of the research development and the final approval process.
In recent times, the FDA has expanded its guidance to encompass public health emergencies, reflecting on lessons learned from the COVID-19 pandemic. This includes addressing logistical concerns and adopting a risk-based approach to monitoring clinical research sites and participants. The FDA's adaptable measures during the pandemic emphasized the necessity for flexibility in study management, while guaranteeing the integrity and dependability of study results.
The FDA's approval process is supported by the expertise of an independent group of physicians and scientists who meticulously evaluate each medication's safety, effectiveness, and labeling. The power of the evidence, both from the primary study and any subsequent confirmatory examinations, is essential. The amount of confirmatory evidence required is relative to the robustness of the initial trial's findings, a principle that holds particular importance for rare disease drug development.
Each year, CDER approves a range of new molecular entities and therapeutic biological products, some of which introduce unprecedented treatments to clinical practice. These approvals are based on a comprehensive understanding of the science behind product creation, the diseases they are intended to treat, and rigorous testing and manufacturing standards. The endorsement of these products not only promotes healthcare but also offers individuals with new therapy choices, contributing to the overall improvement of public health.
Pivotal Trials and Real-World Evidence (RWE)
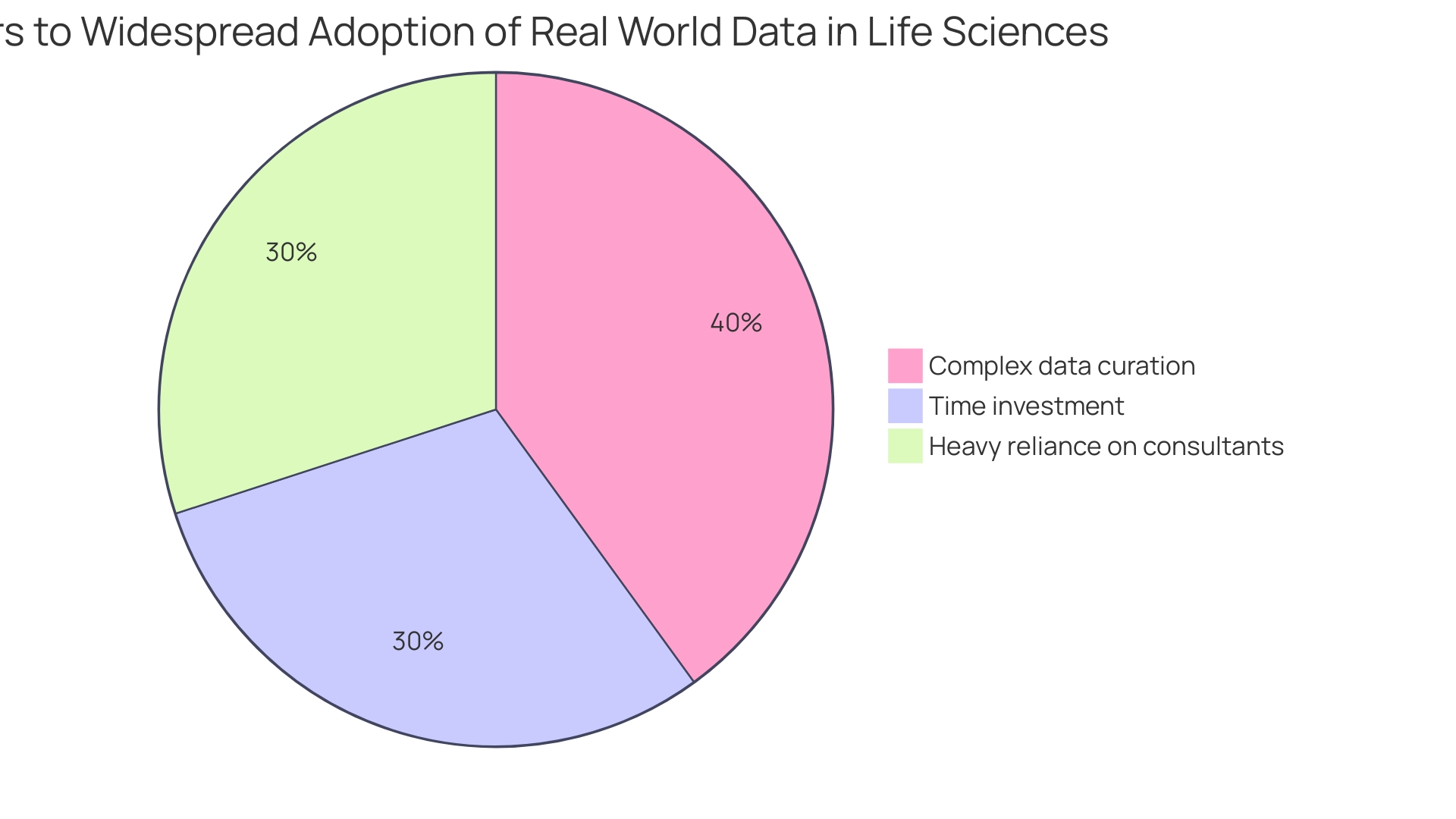
Essential tests are crucial in evaluating the safety and effectiveness of medical interventions in controlled settings, yet their range is frequently restricted to particular circumstances and individual characteristics. The emergence of Real-World Evidence (RWE) studies has been crucial in connecting the gap between controlled experimentation environments and the intricacies of everyday clinical practice. These studies build on the results of important experiments by examining the efficacy and safety of interventions across a broader range of individuals and different real-life situations. Recent efforts, like the FDA's RWE Program, highlight the significance of efficient procedures in randomized controlled experiments (RCTs), which can be incorporated into regular healthcare. This approach facilitates the inclusion of broader patient populations, enhancing the generalizability of the research findings. For instance, the DAPA-MI study utilized clinical registry information within an RCT framework to evaluate a marketed product's efficacy, showcasing a novel method in registrational clinical trial design. Moreover, RWE has proven its regulatory value through instances like the expansion of Ibrance's label to treat male breast cancer, a decision underpinned by real-world evidence illustrating a consistent safety profile across genders. Recognizing the variety of Resources, the FDA emphasizes their potential for regulatory processes, provided the information is accurate, complete, and systematically collected. However, the application of RWE is not without challenges; data privacy, access issues, and the depth and quality of data sources are among the concerns that need to be addressed. Efforts are being made to standardize research objectives and study designs globally to ensure that RWE meets the quality and relevance standards required for regulatory decision-making.
Advancing Medical Knowledge through Pivotal Trials
Critical studies are central to clinical research, influencing the domain of medical treatment and care for individuals. These studies are instrumental in refining our understanding of diseases and evaluating the efficacy of new treatments. The results of significant experiments can transform healthcare practices by establishing new benchmarks for care, updating existing treatment protocols, and setting innovative care standards. Healthcare providers heavily depend on the robust data from these experiments to make informed, evidence-based decisions for patient care.
Furthermore, crucial experiments occupy a prominent position not just in the healthcare field but also in the wider framework of technology governance. They are examined through multifaceted lenses including ethical, legal, and social implications, while addressing the challenges and successes in governance across sectors. Case studies often underscore these aspects with real-world examples, delineating the trajectory of technology and its impacts over time.
Recent discussions, like those at the first JAMA Summit, emphasize the need to bridge the gap between experiments and everyday practice. According to Gregory Curfman, executive editor for JAMA, and Derek Angus of the University of Pittsburgh School of Medicine, the disconnection between the design of randomized experiments (RCTs) and the complexity of medical practice contributes to inefficiencies and limited applicability of experiment results. They advocate for the incorporation of experiments into medical environments to enhance significance and influence.
In a time period where experiments are progressively important, obstacles in openness and information exchange continue to exist. Although signing up on platforms like ClinicalTrials. Gov is frequent for influential studies, comprehensive study protocols and statistical analysis plans are not universally accessible, impeding reproducibility. Efforts to improve information exchange have been suggested, but the execution remains inconsistent.
Moreover, trials supported by the industry often restrict analysis to within the sponsoring organization, limiting broader scrutiny. This practice contrasts with the views of experts like Margaret MacDougall, a senior lecturer in medical statistics, who advocates for open access to research and data to foster innovation and learning.
Statistics highlight these concerns, showing that experimentation durations have increased, with Phase 3 assessments now averaging 44 months. Delays are frequent, with almost 80 percent of experiments not completing on schedule. The need for speed in the development of medicines is increased by competitive pressures in the biopharma industry and legislative changes like the US Inflation Reduction Act, which could alter the strategic landscape for drug development and the race to market.
In conclusion, pivotal trials are the bedrock upon which modern medical practice is built. They not only provide the evidence needed for sound clinical decision-making but also reflect the complexities and evolving nature of healthcare governance and industry dynamics. It is through these rigorous studies that we can continue to advance patient care and uphold the integrity of medical science.
Case Study: Successful Pivotal Trials in Medical Research
Crucial experiments serve as a foundation in the progression of medical treatments, often deciding the destiny of new therapies. A remarkable instance is the groundbreaking immunotherapy medication for advanced melanoma, which underwent thorough testing in a pivotal examination. This comprehensive study not only enrolled a large cohort but also marked a significant leap in survival rates when benchmarked against existing therapies. The robust design and substantial outcomes propelled the drug towards regulatory sanction, introducing a revolutionary option for those grappling with advanced melanoma.
The significance of these trials is emphasized by their influence on future medical practices and care for individuals. For instance, the reliance on IV-magnesium in myocardial infarction patients was predicated on a collection of smaller studies that, when combined, indicated a remarkable 50% reduction in mortality. This highlights the transformative power that well-conducted medical research can have on treatment protocols.
However, ensuring the relevance and quality of medical evidence remains a critical challenge. Research has shown that the main evidence affecting decision-making frameworks can be of subpar quality, requiring the generation of strong data both before and after market introduction of medical interventions. It is not uncommon to find that evidence from medical experiments is weak or insufficient, often due to being the only evidence available. Even well-conducted trials with comprehensive evidence may falter if the comparators used are unsuitable for making informed decisions about the deployment of treatments.
As medical device news circulates among specialists and stakeholders, it becomes increasingly important that the evidence supporting these devices is rigorous and transparent. With approximately 200 million patients worldwide suffering from peripheral arterial disease (PAD), for example, the meticulous analysis of data from paclitaxel-coated devices has been crucial. This analysis, steered by independent physicians and scrutinized by the FDA, exemplifies the necessity of meticulous research governance and the ethical, legal, and social considerations it entails.
In the realm of medical research, each decision is a link in a chain that can have an exponential effect on subsequent outcomes. As such, the planning and execution of medical studies demand a strategic and thoughtful approach. Considering their extensive advisory background, professionals have observed that numerous companies could have gained advantages from more thorough planning in the creation and execution of their clinical experiments. This includes a close examination of the multitude of factors, such as market incentives and intellectual property, that shape the evolution of emerging technologies and their governance.
In summary, the statistical rigor, ethical considerations, and strategic governance are crucial to the success of pivotal experiments and the progress they bring in medical science. It is through this lens that pivotal trials, such as the one for the advanced melanoma immunotherapy drug, must be viewed—not only as a triumph in their own right but as a blueprint for future research endeavors.
Conclusion
In conclusion, pivotal trials are vital for advancing medical science by evaluating new interventions. They provide high-quality evidence that guides regulatory decisions and clinical guidelines. Strategic choices in titling, abstract writing, and keyword selection optimize the impact of pivotal trial findings, while stringent authorship criteria ensure accountability.
It is important to understand the distinction between trial standardization and individualized clinical care to effectively apply trial findings in practice. Pivotal trials are just one part of a patient's care continuum, and their design and conduct require meticulous planning and adherence to scientific standards.
Challenges faced by pivotal trials include participant diversity, data integrity, bias management, and logistical concerns. Ethical considerations play a fundamental role, with a focus on participant rights, inclusivity, and transparency. Regulatory bodies rely on pivotal trial outcomes to evaluate the safety and efficacy of medical interventions.
Real-world evidence studies complement pivotal trials by assessing interventions in diverse patient populations and real-life scenarios. However, challenges related to data privacy, access, and quality need to be addressed. Pivotal trials shape the landscape of medical treatment, refine our understanding of diseases, and revolutionize healthcare practices.
Successful pivotal trials have a transformative impact on medical treatments and patient care. Ensuring the relevance and quality of clinical evidence remains a critical challenge. Strategic planning and execution of clinical studies are essential for their success and the advancements they bring in medical science.
In conclusion, pivotal trials are essential for generating high-quality evidence, guiding regulatory decisions, and shaping medical practice. Through scientific rigor, ethical considerations, and strategic governance, these trials drive advancements in patient care and uphold the integrity of medical science.




