Introduction
Clinical trials play a crucial role in evaluating the effectiveness of new treatments and interventions. Central to these trials are the primary endpoints, which serve as the key outcomes that the study aims to assess. The selection of these endpoints is not only essential for the success of the trial but also for the validity and reliability of its findings.
In this article, we will explore the importance of endpoint selection in clinical trials, the characteristics of effective endpoints, the different types of endpoints, commonly used endpoints, the challenges in selecting primary endpoints, statistical considerations in endpoint selection, and a case study highlighting successful endpoint selection in practice. By understanding the intricacies of endpoint selection, we can enhance our understanding of clinical trials and contribute to the advancement of medical research and patient care.
Importance of Endpoint Selection in Clinical Trials
Within the domain of clinical research, the identification of key outcomes is a crucial determination that affects the integrity of the study and its findings regarding the novel therapies or interventions being examined. These primary endpoints serve as the central outcomes that the study is set up to assess. Their careful selection is not only a marker of a trial's success but also a safeguard for the validity and reliability of its findings. To address the complexities of such a selection, a stepwise process has been formulated. This includes defining a causal question, choosing appropriate information, evaluating precision, planning robustness assessments, and conducting inferential analyses. The process underscores the importance of avoiding bias, especially in non-interventional studies that hinge on real-world healthcare data. Tools like ROBINS-I and GRACE checklist aid in bias evaluation, while RECORD-PE and Start-RWE enhance transparency in reporting. Similarly, the HARPER protocol template fosters clear communication of study parameters and is endorsed by regulators for non-interventional study designs. These measures are essential in improving the methodological rigor of experiments, thus strengthening the evidence generated for healthcare interventions.
Characteristics of Effective Endpoints
When it comes to clinical experiments, the choice of main and additional outcomes is a decision of utmost significance. These termination points must not only align with the scientific goals of the research but also need to be measurable and responsive enough to identify the effects of the intervention under examination. Aligning endpoints with the goals of the trial also requires a profound understanding of the information and methodologies at hand. Equal Randomisation (ER) and Thompson Sampling (TS) are two of the methods used to assign treatments to patients, with ER being straightforward and TS aligning the likelihood of receiving a treatment with its potency. Furthermore, the integration of insights from various digital sources, such as connected devices and electronic diaries, has emphasized the value of patient-centered drug development. This extensive range of information sources requires a comprehensive strategy to guarantee the integrity and quality of the collected information. Ensuring that endpoints are clinically relevant, measurable, and interpretable is not a task taken lightly, as it involves meticulous planning and expert knowledge to anticipate and address potential issues in data management and oversight. The challenges emphasized by the World Health Organization, from inadequate experiment design to restricted participant diversity, highlight the continuous need for improvement in the field. With less than 5% of experiments involving pregnant women and only 13% including children, there is an apparent gap in inclusivity that must be addressed. Clinical experiments must aim to be cost-effective, provide the best treatment to as many as possible, and be likely to yield accurate results. Balancing these aims is a delicate act, but one that is essential for the advancement of medical research and the betterment of public health worldwide.
Types of Endpoints: Direct, Surrogate, and Composite
In clinical trials, comprehending the range of terminations is vital for propelling advancements in medical treatments. Primary results are the most significant consequences that closely match the research question or goal, offering a clear response to the study's hypothesis. Secondary results, although not the primary emphasis, provide corroborating evidence and may encompass supplementary perspectives such as subgroup analysis. Composite measures are particularly beneficial as they amalgamate multiple single outcomes into a more comprehensive measure, allowing for a broader assessment of treatment effects.
For example, Pfizer's clinical trial for the potential cachexia treatment, ponsegromab, demonstrates the utilization of composite outcomes. Patients with cachexia, a severe wasting condition in cancer, saw improvements in body weight, muscle mass, quality of life, and physical function. This holistic view, afforded by composite endpoints, is essential for conditions like cachexia where multiple factors influence patient health.
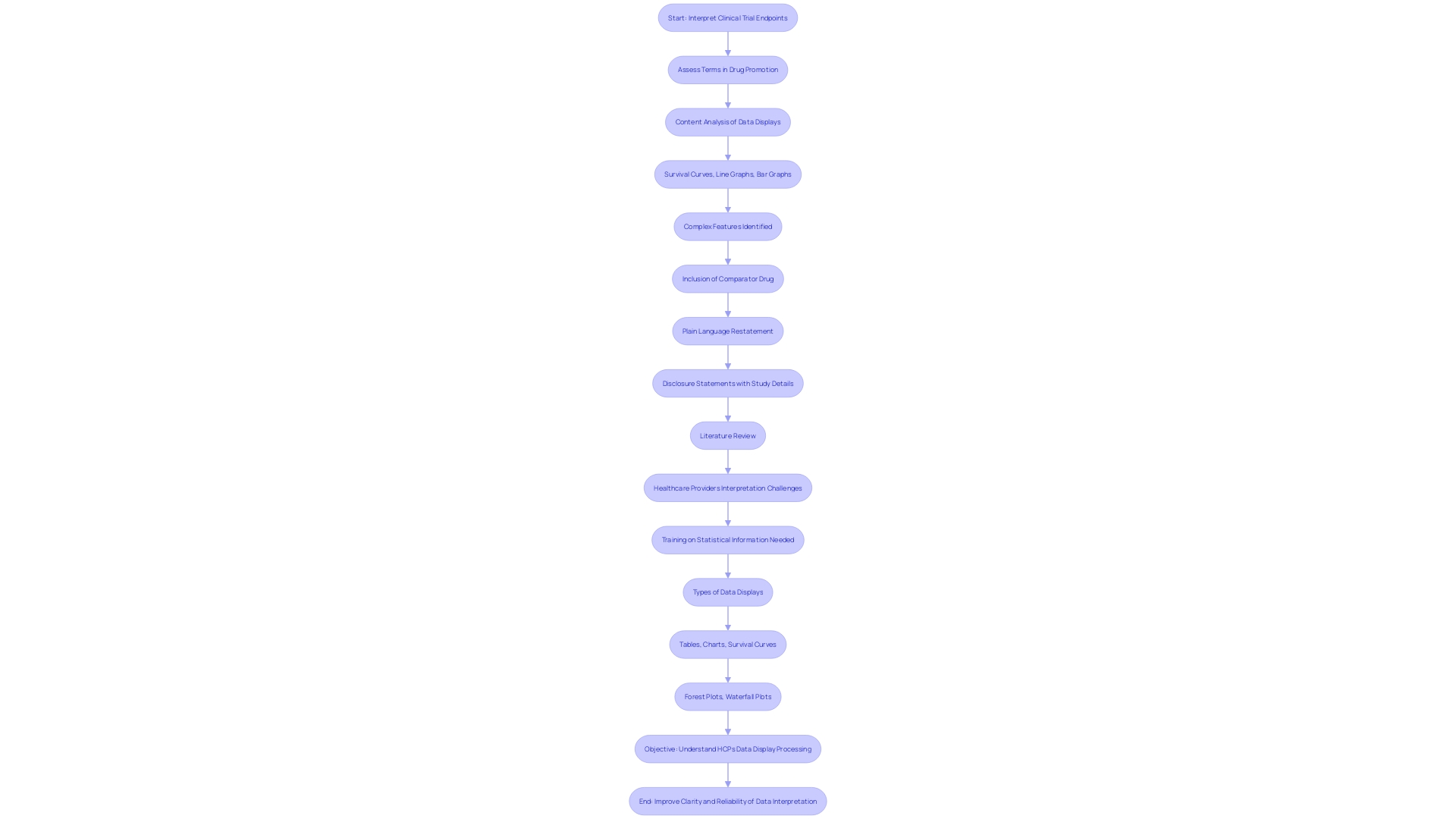
However, clinicians and researchers must navigate the complexity of information interpretation, as healthcare providers often encounter intricate statistical information, such as survival curves and bar graphs. Research indicates that numerous healthcare practitioners face challenges with intricate information presentations, emphasizing the importance of clarity in showcasing clinical testing results. This is particularly relevant as industry leaders like Pfizer set standards for quality and safety, emphasizing the importance of reliable data interpretation to improve patient outcomes.
Comprehending these various types of endpoints—and interpreting them accurately—is more than an academic exercise; it is a responsibility to the patients who stand to benefit from the advancements these studies bring about.
Commonly Used Endpoints in Clinical Trials
Endpoints in clinical experiments are crucial for assessing the efficacy of therapeutic interventions. They range from measuring overall patient survival and progression-free survival to response rates, quality of life, and the incidence of adverse events. These measures are chosen for their clinical significance and their capacity to reflect the impact of the treatment under study. In cardiology, for example, Major Adverse Cardiac Events (MACE) are used as a combined result to capture different cardiovascular consequences. In oncology trials, Progression-Free Survival (PFS) and Disease-Free Survival (DFS) are often used as substitutes for more conclusive measures such as overall survival or health-related quality of life.
The selection and reporting of endpoints require careful consideration. As mentioned in the management of multiple coronary lesions, where choices involve multiple stents versus coronary bypass surgery, the selected results must be consistently reported to provide clear insights into the effectiveness of interventions. In addition, it's essential to maintain consistency in reporting outcomes over time for comparability.
Clinical experiments may also utilize non-interventional studies, where treatments are not assigned according to a protocol but rather observed during routine medical practice. The FDA and EMA have differing definitions for these studies, highlighting the need for harmonization in regulations. For instance, the FDA does not require that there be no additional diagnostic or monitoring procedures, whereas the EMA does.
Furthermore, stakeholders such as Regeneron Pharmaceuticals have requested more explicit direction regarding non-interventional research, proposing the establishment of dependable information sources and verification methods to guarantee the quality of information. The National Organization for Rare Disorders (NORD) emphasized the importance of observational studies, especially for rare diseases, and advocated for more specific guidance.
Data quality and integrity are crucial in clinical trials, as highlighted by issues encountered with paper-based patient-reported measures (Proms). Research has indicated that 44% of patients using paper diaries either missed or ambiguously marked items, causing concerns about the quality of information. Electronic information capture methods have been suggested to improve the accuracy and dependability of clinical outcome assessments and alleviate the challenges linked to paper-based collection.
In summary, the meticulous choice and consistent documentation of outcomes, together with the implementation of digital data collection techniques, are critical in enhancing the comprehension of clinical experiments and, ultimately, healthcare for patients.
Challenges in Selecting Primary Endpoints
The intricacies of choosing main objectives for clinical experiments are multifaceted, encompassing a combination of rigorous scientific approaches and practical logistics. One must consider the ability to measure the final outcome reliably within the trial's timeline. The DAPA-MI study exemplifies this challenge. Initially, the primary endpoint was a composite of hospitalization for heart failure and cardiovascular death. However, the number of primary composite outcomes accrued was lower than anticipated, prompting reevaluation. The incorporation of real-world registry data with randomized experiment components in this study, a registry-based randomized controlled investigation (R-RCT), aimed to reconcile the need for reliable data with the practicalities of patient enrollment and cost considerations.
In oncology, the growing use of Patient-Reported Outcomes Measures (PROMs) reflects an understanding that survival metrics alone do not fully capture treatment impacts. Instruments like the NSCLC-SAQ for non-small cell lung cancer are increasingly employed to gauge multiple symptom dimensions, addressing the sometimes insufficiently quantitative survival endpoints.
Conversations among specialists, including those from health technology and regulatory agencies, highlight a modular approach to PRO administration in interventional experiments. This approach, while not addressing how subscales are selected, which is crucial, does focus on the methodological and statistical justification for modular implementation, aiming to enhance patient-centric drug development.
Globally, the difference in clinical study distribution between high-income and low- and middle-income countries demonstrates the need for more equitable research practices. 'WHO's recommendations and the FDA's commitment to harmonizing human subject protection regulations exemplify efforts to enhance experiment design and participant diversity.'.
Statistical considerations are equally paramount. Frequentist and Bayesian methodologies offer contrasting approaches to design and analysis, with the latter recommended for its flexibility in a dynamic research environment. The SPIRIT-Surrogate extension provides guidelines for reporting protocols using substitute goals, underscoring the importance of transparent and replicable methods for reliable conclusions.
Clinical experiments are essential for medical progress but encounter obstacles such as delays and high rates of failure to finish on schedule. With the average duration of Phase 3 trials increasing and the pressures of the Inflation Reduction Act, the necessity to optimize study design and endpoint selection has never been more crucial. As pointed out by McKinsey, the gathering in biopharma intensifies the race to be the first to market, emphasizing the significance of efficient conduct. Non-inferiority studies, which compare the effectiveness of a new treatment to an existing one, demonstrate the delicate balance between showing effectiveness and emphasizing additional advantages that could outweigh the risks. Transparency in objectives is essential to ensuring that new treatments with potential benefits are not overlooked simply because they do not meet conventional non-inferiority margins.
Statistical Considerations in Endpoint Selection
Choosing the most suitable outcome measures in clinical studies is a procedure emphasized by thorough statistical analysis. Sample sizes are not arbitrary numbers; they are meticulously calculated to ensure that the study has adequate power to detect a significant effect of the treatment under investigation. The main goal, specifically, is a crucial factor of a study's statistical power, impacting the feasibility and significance of the experiment's results.
To contextualize this, consider a cross-over study design used in bioequivalence trials. Each participant receives both the test and reference drug in successive periods, allowing researchers to observe differences in pharmacokinetic responses. Through statistical models, such as the calculation of the geometric mean ratio from log-transformed information, we can infer bioequivalence between the two treatments.
Bayesian statistics have become increasingly relevant, providing a flexible approach to integrating prior data with current research, thus enhancing the decision-making process. This methodology has gained traction in regulatory submissions, offering valuable insights that traditional frequentist methods may not provide, especially in complex trial designs.
However, it's not just about choosing the right statistical tools; it's also about understanding what the numbers truly represent. Inferential statistics, for example, do not give us probabilities but rather allow us to estimate what might occur across a broader population based on our sample. This is akin to predicting election results based on a poll, where the margin of error gives us a range of potential outcomes, not a definitive answer.
In the spirit of continual advancement, the field of biostatistics celebrates its progress with discussions reflecting on the seminal work of Sir Austin Bradford Hill and the evolving role of statisticians in medicine. With 40 years of advancements, experts like Dr. Albert from the National Cancer Institute contribute to the development of novel methodologies that underpin the interpretation of clinical data.
The importance of robust statistical methods extends beyond the confines of high-income countries; it's a global imperative to ensure equitable access to safe and effective health interventions. According to the World Health Organization, enhancing research and incorporating clinical experiments into regular services can close the gap between countries, ultimately improving global health.
Case Study: Successful Endpoint Selection in Practice
The choice of key outcomes in clinical experiments is a crucial element in assessing novel therapies. Consider a recent study targeting a specific cancer type. The researchers designated overall survival as the main focus, highlighting its importance in clinical relevance and expecting the new drug to surpass standard treatments in this critical aspect. Their results showed a marked improvement in overall survival rates, subsequently leading to regulatory approval of the new medication. These results emphasize the strategic significance of selecting the most appropriate primary measures to assess the effectiveness of a treatment in clinical studies.
In the context of clinical experiments, it is important to acknowledge that while main results are the most vital focus, additional results also contribute to understanding the main result's significance. A thorough comprehension of these results is crucial for researchers to communicate the importance of their findings efficiently and guarantee that their work tackles the intended research question or study aim. Moreover, the evolving landscape of trial reporting underscores the importance of transparently presenting all measured outcomes, as demonstrated by the modernized ClinicalTrials. Gov website, which now enhances the visibility of study records and their associated data elements.
Conclusion
In conclusion, the selection of primary endpoints in clinical trials is crucial for the validity and reliability of the study's findings. It involves a stepwise process that includes defining a causal question, choosing appropriate data, evaluating precision, planning robustness assessments, and conducting inferential analyses. Effective endpoints must be scientifically relevant, quantifiable, sensitive enough to detect treatment impacts, and align with the goals of the trial.
Commonly used endpoints include overall survival, progression-free survival, response rates, quality of life, and adverse events.
However, challenges arise in selecting primary endpoints, such as limited participant diversity, statistical considerations, and the need for more equitable research practices. Statistical methods like Bayesian analysis play a vital role in endpoint selection. Ensuring clarity in presenting clinical trial outcomes is crucial for improving patient care.
A successful case study exemplifies the strategic importance of choosing relevant primary endpoints. The selection of overall survival as the primary endpoint led to marked improvements and subsequent regulatory approval of a new medication. Recognizing the role of secondary outcomes and transparently presenting all measured outcomes contribute to the understanding and significance of trial findings.
In summary, endpoint selection in clinical trials is a meticulous process that impacts the integrity and reliability of study findings. By understanding the complexities involved, we can enhance our understanding of clinical trials, improve trial design, and contribute to the advancement of medical research and patient care.




