Introduction
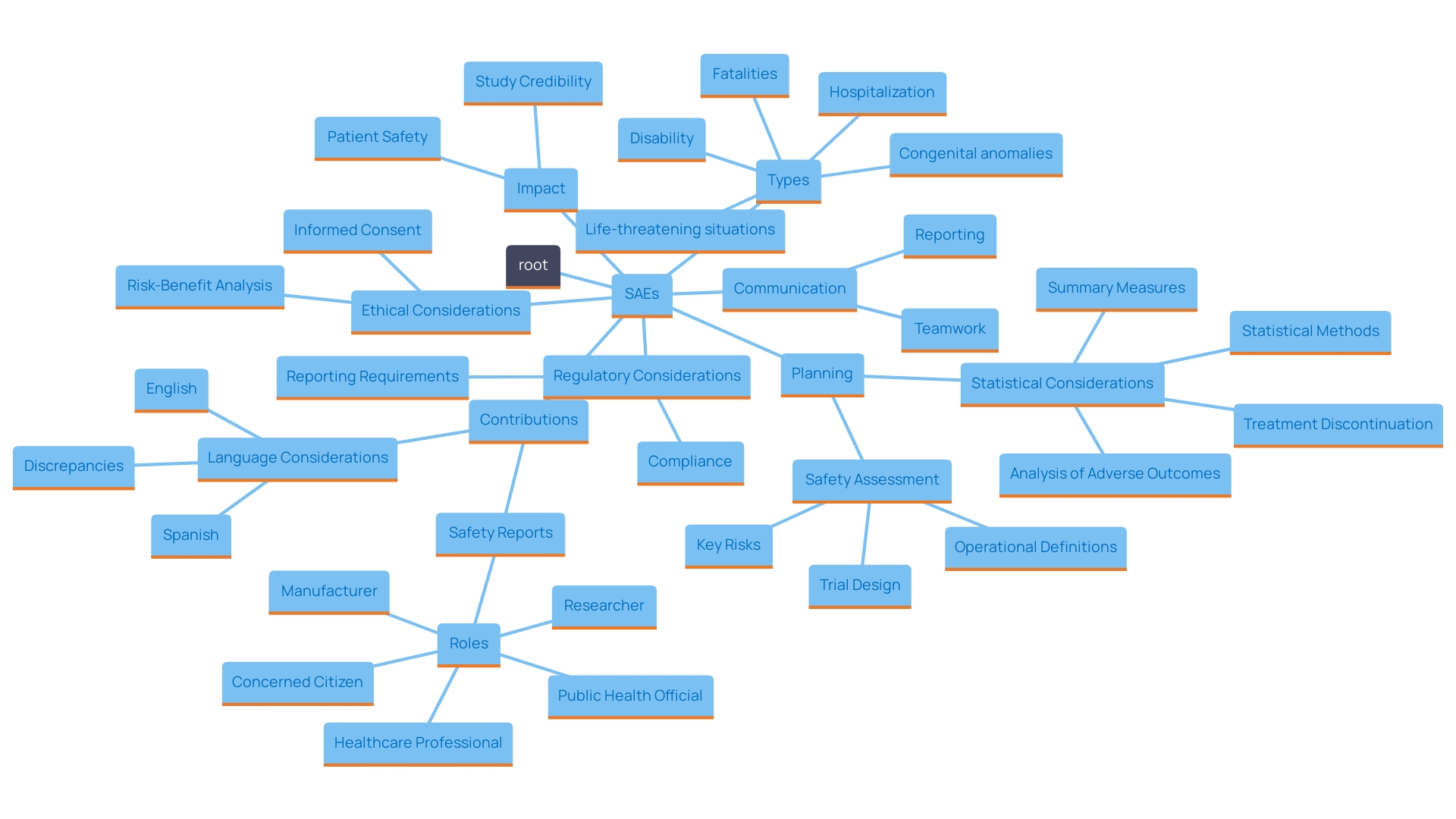
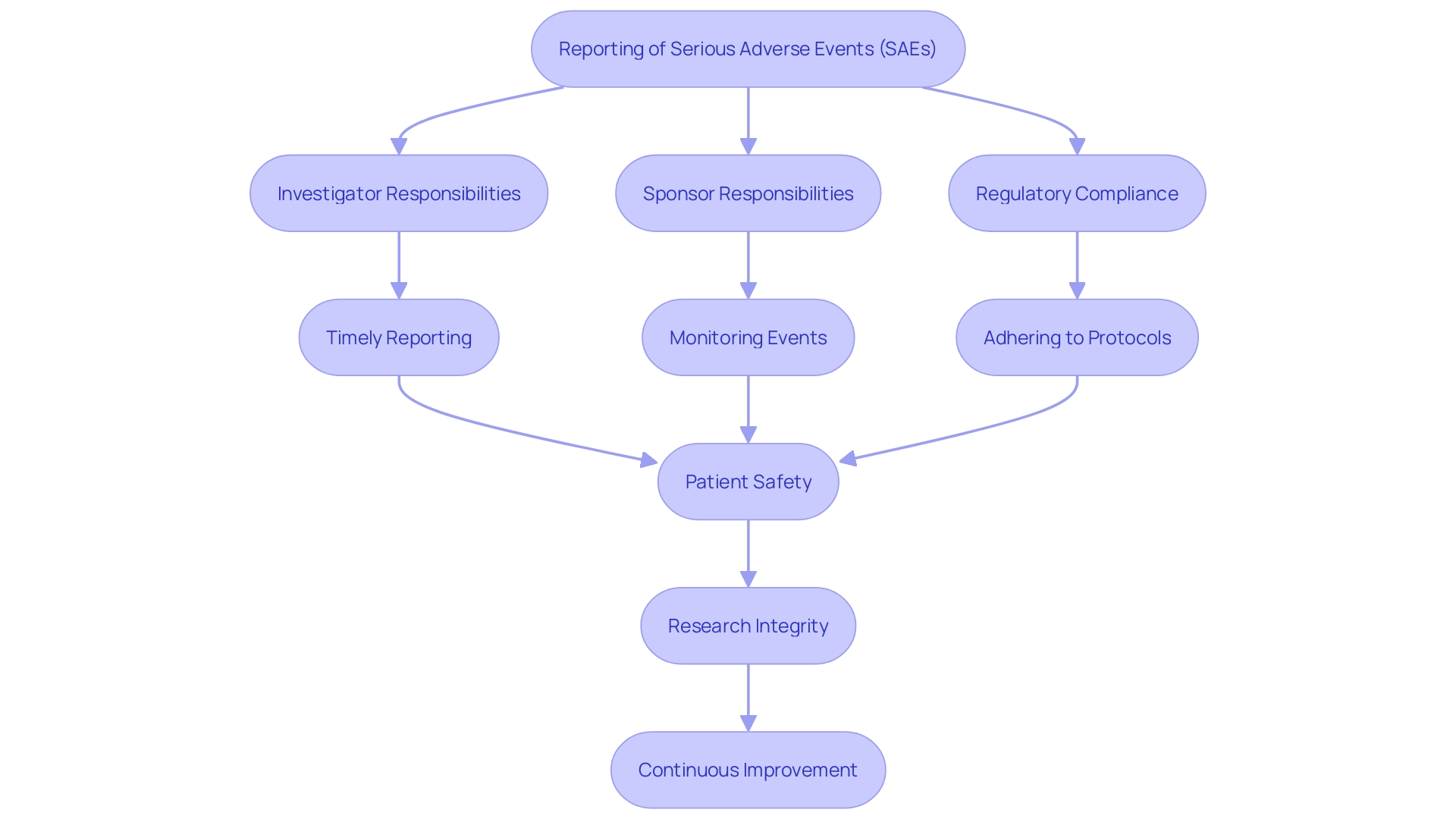
The landscape of clinical research is increasingly focused on ensuring patient safety, with Serious Adverse Events (SAEs) standing at the forefront of this endeavor. These significant occurrences, which can include life-threatening situations, hospitalizations, and even fatalities, necessitate rigorous monitoring and reporting to maintain the integrity of clinical trials. As regulatory bodies like the FDA and EMA outline detailed guidelines for SAE identification and documentation, it becomes imperative to understand the multifaceted role of investigators and sponsors in this process.
This article delves into the definition, criteria, and reporting requirements for SAEs, emphasizing the ongoing need for transparency and collaboration among all stakeholders involved in clinical trials. By addressing these critical elements, the discussion aims to highlight the importance of safeguarding patient welfare while advancing medical knowledge through rigorous research practices.
Definition of Serious Adverse Events (SAEs)
Serious Adverse Events include various important medical incidents that present a direct risk to patient well-being. These events include fatalities, life-threatening situations, hospitalizations or extended hospital stays, persistent disabilities, and congenital anomalies. The consequences of serious adverse events in research studies are significant, affecting both the safety of participants and the credibility of the study's results.
Serious Adverse Events are not merely statistical anomalies; they represent critical moments that necessitate immediate scrutiny and often lead to further investigation. The ethical, legal, and social dimensions surrounding these events are complex, as they can impact public perception of clinical research and regulatory practices. For instance, a study's integrity can be compromised if Sales are not adequately reported or analyzed. Transparency in trial protocols and statistical analysis plans is essential to ensure that all stakeholders, including healthcare professionals and regulatory bodies, have access to comprehensive data regarding these events.
Recent developments highlight the evolving landscape in risk monitoring. For example, the FDA has emphasized the importance of clear communication regarding drug side effects in direct-to-consumer advertisements. This reflects a broader commitment to safeguarding public health by ensuring that the major side effects of medications are presented in an understandable manner. The FDA's role in regulating and overseeing the protection of drugs and biological products is pivotal, as it provides the necessary framework to address potential risks associated with SAEs.
Furthermore, risk analysis is a dynamic area that necessitates continuous learning and teamwork among different experts, including statisticians, medical writers, and research investigators. Ongoing education is essential for accurately analyzing risk information, particularly regarding combined research study evaluations. As the environment of medical research changes, so too must the methods of monitoring and addressing serious adverse events, ensuring that patient safety remains the foremost priority.
Criteria for Identifying SAEs
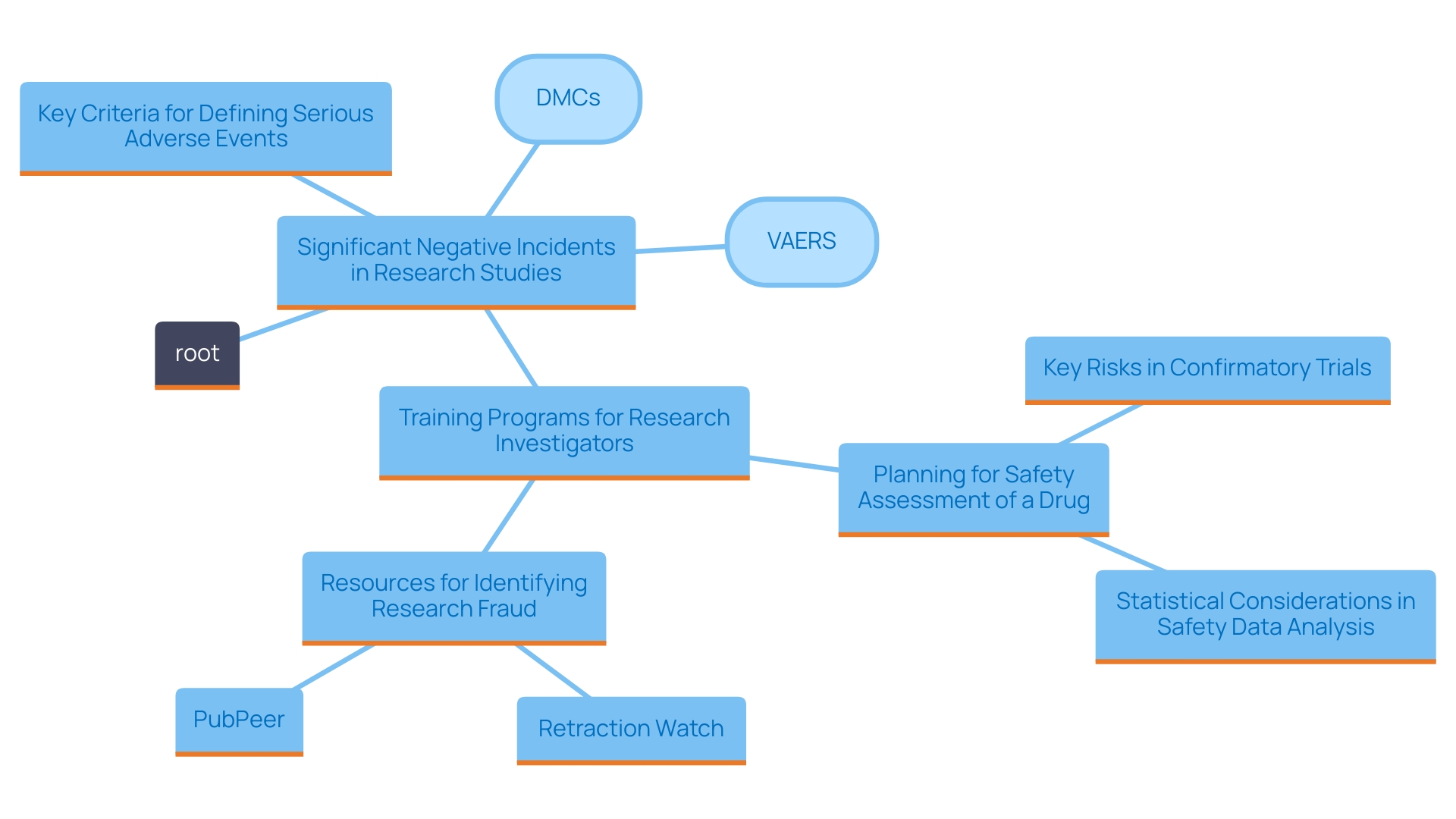
Significant negative incidents are crucial events that must be carefully recognized and documented during research studies. Key criteria for defining serious adverse events include the severity of the event, its relationship to the study treatment, and the resulting outcomes. Specifically, events that necessitate hospitalization, are life-threatening, or are unexpected yet serious must be documented. A comprehensive assessment of the patient's medical history, together with a thorough examination of the research protocol, is essential for the precise identification of SAEs.
The FDA emphasizes the importance of monitoring these events in their guidelines, particularly through the establishment of Data Monitoring Committees (DMCs). These committees play a crucial role in trial oversight, ensuring that concerns are addressed promptly. As stated by the FDA, promoting innovation in medical product development requires not only the evaluation of effectiveness but also a thorough review of risk profiles during trials.
Data from the Vaccine Adverse Event Reporting System (VAERS) demonstrate the system's effectiveness in identifying concerns related to vaccines, underscoring the importance of vigilance in monitoring Sales. According to recent reports, "Vaccines are a cornerstone of modern medicine, preventing debilitating diseases and saving countless lives," which emphasizes the importance of continuous risk assessments in medical environments.
Additionally, a research investigator training program seeks to provide all parties—industry experts, scholars, and regulators—with the understanding needed to recognize risk issues efficiently during product development. 'This initiative is vital as it focuses on particular groups engaged in biomedical research, guaranteeing that protection stays at the forefront of medical studies.'.
Key Elements of SAE Reporting
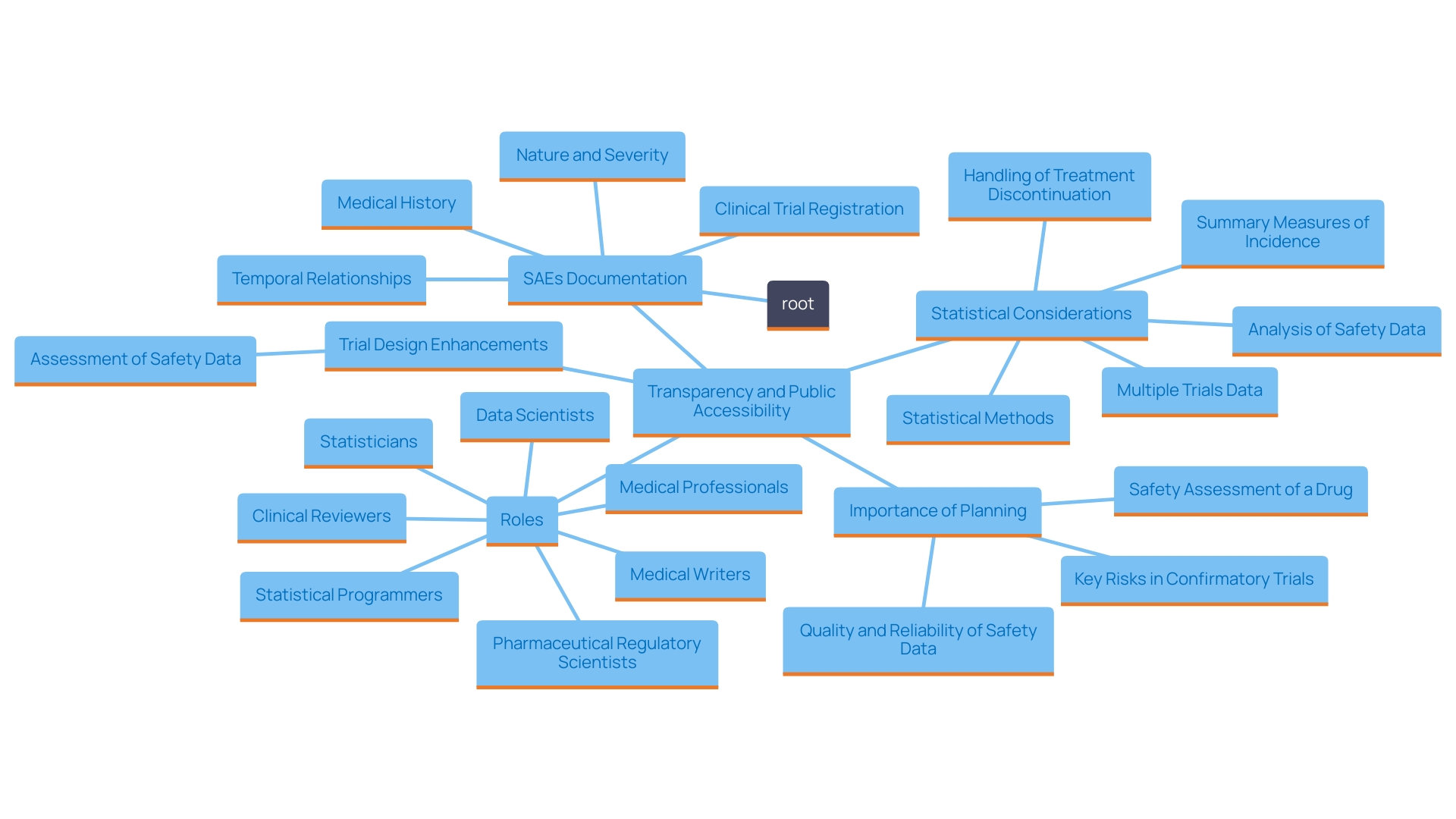
The documentation of Serious Adverse Events (SAEs) is a vital part of medical research, including various crucial aspects that guarantee the integrity and protection of medical studies. A comprehensive description of the event must be provided, detailing the nature and severity of the SAE, as well as its timing in relation to the study intervention. This temporal relationship is vital for determining causality and assessing any potential risks that may arise from the intervention.
Moreover, incorporating relevant medical history into the SAE report is crucial. This background information allows for a more informed analysis of the event, facilitating a better understanding of individual patient risks and responses. Accurate and thorough reporting not only aids in the assessment of patient safety but also ensures that all stakeholders, including regulatory authorities and ethics committees, are kept informed of any significant risks associated with the research.
Recent trends highlight a growing emphasis on openness in medical studies. While many influential studies are now registered in clinical research databases like ClinicalTrials.gov, the level of detail provided often varies significantly. A mere registration does not guarantee the availability of comprehensive experimental protocols or statistical analysis plans, which are essential for fostering transparency and reproducibility in research outcomes. Such gaps can hinder the ability of researchers and regulatory bodies to fully assess the implications of SAEs.
A significant statistic from recent analysis shows that the dedication to openness among companies conducting research studies remains inconsistent. This highlights the importance of enhanced methods regarding the public accessibility of study information, which is crucial for maintaining ongoing patient well-being and trust in the research process.
As stated by industry professionals, "Examination of the warning signs you should observe in research design, implementation, and presentation of outcomes" is crucial for protecting patient well-being. This proactive approach not only enhances the quality of studies but also helps mitigate potential adverse events before they escalate into serious issues.
The Role of Investigators and Sponsors in SAE Reporting
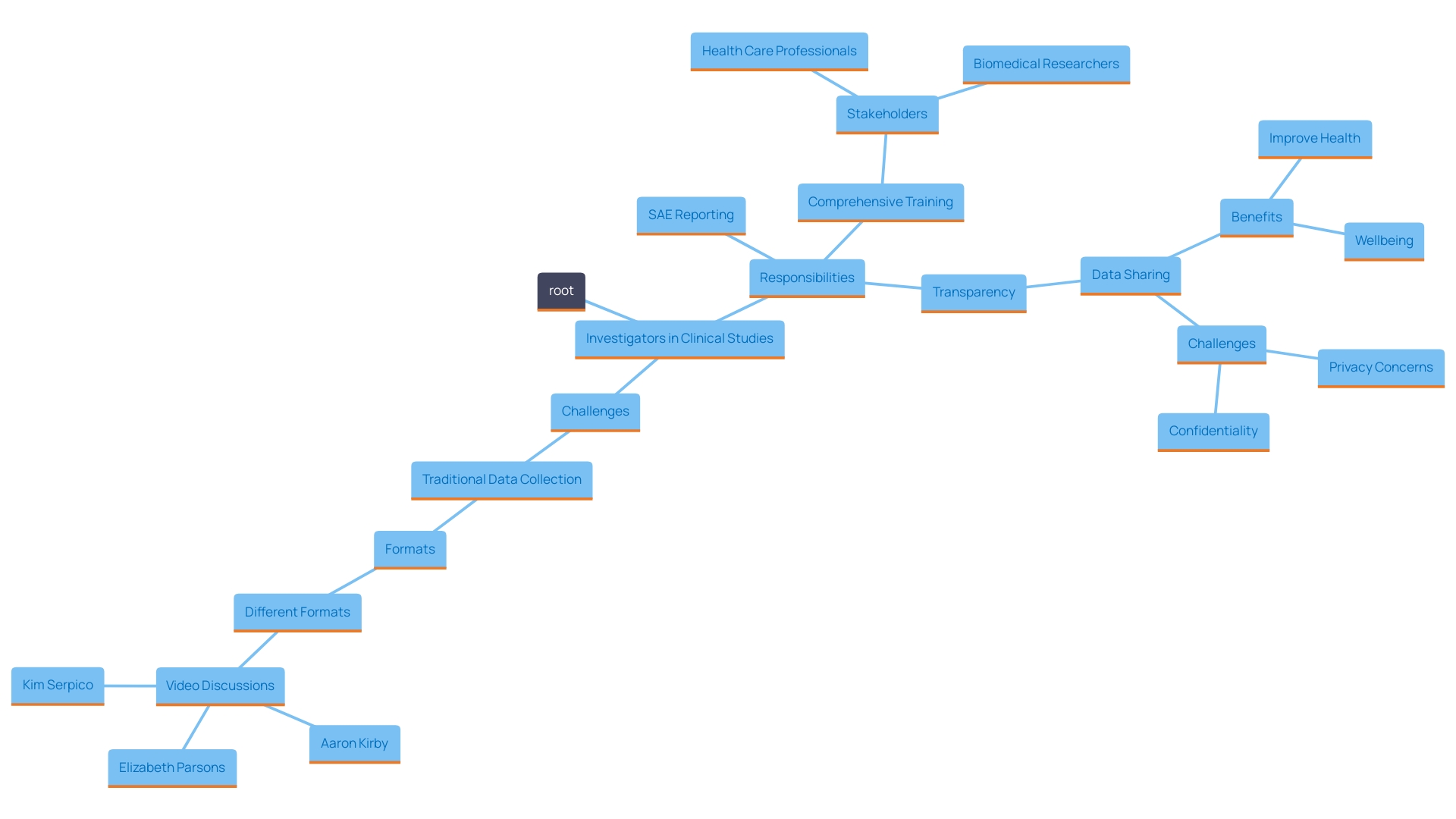
Investigators occupy a crucial role in the detection and documentation of Serious Adverse Events (SAEs) during clinical studies, acting as the primary protectors of patient well-being. Their responsibilities involve vigilant observation of participants throughout the study duration, ensuring that any adverse events are documented and reported promptly in adherence to regulatory guidelines.
To facilitate this, it is imperative that sponsors equip investigators with comprehensive training in SAE reporting procedures. This includes access to necessary resources and tools that streamline the documentation process. The partnership between researchers and backers is essential; it promotes openness and bolsters adherence to set safety guidelines, ultimately improving the integrity of the study.
A significant issue is that the data gathering techniques used in medical studies can be labor-intensive, frequently leading to gaps in the information collected. For instance, traditional data collection systems may overlook valuable insights from real-world sources or fail to capture important contextual factors such as social determinants of health. These limitations can affect the overall understanding of a participant's health and the long-term implications of the interventions being tested.
Furthermore, while numerous studies are registered in platforms like ClinicalTrials.gov, the extent of information provided can differ greatly. Openness in medical research necessitates not only registration but also the accessibility of complete study protocols, statistical analysis plans, and, ideally, raw data. This is crucial for reproducibility and for fostering trust in the results produced.
As the field evolves, the emphasis on data sharing continues to grow. Regulatory organizations are progressively advocating for better access to research data, in accordance with efforts focused on improving the clarity and reproducibility of research results. This environment highlights the need for continuous training and support for investigators, who are crucial in navigating the complexities of SAE reporting and ensuring patient protection.
Regulatory Requirements for SAE Reporting
Regulatory bodies, such as the FDA and EMA, have established extensive protocols for the documentation of Serious Adverse Events (SAEs) during research studies. These guidelines are essential for ensuring patient well-being and upholding the integrity of the research process. They specify detailed timelines for reporting incidents, outline the required content of reports, and delineate the responsibilities of both investigators and sponsors.
For example, if an event represents a divergence from set good manufacturing practices or presents an unforeseen situation that could affect the integrity or efficacy of a product, it must be reported without delay—typically within 45 calendar days of becoming aware of the event. This prompt reporting is vital for mitigating risks associated with research trials.
The necessity of compliance with these regulatory requirements is underscored by the evolving landscape of medical product development. As regulatory entities adjust to progressions, like the emergence of Software as a Medical Device (SaMD), the need for thorough assessments becomes even more evident. The most recent recommendations from global regulatory bodies support a risk-oriented method, highlighting openness and responsibility in research involving health.
Additionally, research studies contribute greatly to the progression of medical understanding by thoroughly evaluating new therapies to assess their reliability and efficacy. With three distinct phases—where phase one primarily assesses safety among a small group of healthy volunteers and subsequent phases evaluate efficacy and safety among larger populations—the structured approach ensures that only well-vetted products reach the market.
Overall, adherence to these regulatory guidelines not only safeguards patient welfare but also enhances the credibility of the research outcomes, thus fostering trust among stakeholders in the clinical trial ecosystem.
Conclusion
The significance of Serious Adverse Events (SAEs) in clinical research cannot be overstated, as they directly impact patient safety and the integrity of trial outcomes. SAEs encompass a variety of critical medical incidents, including life-threatening situations and hospitalizations, which necessitate immediate and thorough reporting. Understanding the definition and criteria for identifying these events is essential for all stakeholders involved in clinical trials.
A rigorous approach to monitoring and documenting SAEs is vital to uphold the ethical standards of clinical research.
The role of investigators and sponsors is central to the effective management of SAEs. Investigators are tasked with vigilant monitoring and prompt reporting, while sponsors must provide the necessary training and resources to facilitate this process. This collaboration is crucial for ensuring compliance with regulatory guidelines and enhancing the transparency of clinical trials.
The ongoing evolution of data collection methods and regulatory requirements further emphasizes the need for improved practices in SAE reporting.
Regulatory agencies, such as the FDA and EMA, have established comprehensive guidelines that govern the reporting of SAEs. Compliance with these regulations is paramount for safeguarding patient welfare and maintaining the credibility of clinical research. By adhering to these requirements, stakeholders not only protect participants but also contribute to the advancement of medical knowledge through rigorous evaluation of new treatments.
In conclusion, the commitment to transparency, collaboration, and adherence to regulatory standards is essential for fostering a safe and effective clinical research environment. Continuous education and proactive measures in SAE management will ultimately enhance patient safety and the reliability of clinical trial outcomes, ensuring that the progress of medical science is both ethical and trustworthy.




