Introduction
The development and market adoption of machine learning/artificial intelligence medical devices (MAMDs) present unique challenges in the healthcare industry. In addition to navigating regulatory compliance and entrenched medical practices, MAMD makers must also address the limitations on insurance coverage for digital therapeutics. The integration of reimbursement considerations and cross-departmental collaborations can lead to significant time and cost savings.
Clinical trial design plays a crucial role in catering to the evidentiary needs of regulatory agencies and payers, while also balancing innovation and access demands. The pricing strategy of medical devices is influenced by various factors, including therapeutic area, development costs, and competitive scenarios. Medical devices face diverse levels of regulatory oversight in different regions, requiring manufacturers to carefully navigate the approval procedures and demonstrate the medical necessity of their products.
In Latin America, the cost dynamics of conducting post-market clinical studies for medical devices are shaped by complex factors such as the device's complexity, regulatory requirements, pricing strategies, and the economic climate within each country. Strategizing marketing tactics in clinical trials is essential for precise targeting, cost-efficiency, and maintaining trial integrity. A data-driven approach, combined with Voice of the Customer research, can help in developing medical devices that resonate with patients and healthcare professionals.
A successful case study in Latin America highlights the importance of selecting key target markets, establishing strategic partnerships, utilizing digital platforms for patient recruitment, and staying informed about international regulatory trends. By considering these factors and implementing effective strategies, medical device companies can achieve cost management while conducting clinical trials in complex and regulated environments.
Background and Context
Success in the development of machine learning/artificial intelligence medical devices (Names) mirrors the stringent process of new drug market introduction, from initial development to extensive safety and efficacy testing, followed by market adoption by physicians and costs establishment by payers. Despite sharing common hurdles with novel pharmaceuticals, such as the high stakes of commercial viability, MAMD makers must navigate unique challenges such as entrenched medical practices and consumer behaviors, preexisting financial interactions, and the nontrivial barriers of regulatory compliance which strive to sustain market safety and effectiveness.
The healthcare space, accustomed to evolution, is also witnessing the transformative potential of digital therapeutics—software-based treatments for diseases deployable via mobiles, virtual reality, and sensors. Highlighted for their role in managing chronic and neurological conditions, evidence has surfaced showing their capacity to decrease patient expenses. Yet, the novelty of digital therapeutics and the current limitations regarding insurance cover impede their widespread clinical employment.
At the 2024 MedExec Women Conference, the pivotal question posited was identifying strategies to accumulate requisite evidence for regulatory and reimbursement pathways with efficiency. Early integration of reimbursement considerations and cross-departmental collaborations can yield significant time and monetary savings. This multi-disciplinary approach necessitates a shared fluency in real-world evidence and reimbursement language across R&D, QA, and Health Economics, among others.
The accumulating experience with regulatory agencies reveals a pressing demand for evidence to substantiate the medical necessity of new devices. Clinical trial design, therefore, must cater to these evidentiary needs from inception, contemplating payer perspectives alongside regulatory compliance. The FDA, under its public health aegis, underscores the indispensability of well-crafted research in endorsing safe and effective products, signaling a continual effort to align federal research protections with ethical regulations and enhance the clinical study landscape.
Current market dynamics, influenced by diverse factors—from therapeutic area to development costs and competitive scenarios—dictate the selling price of medical devices. The pricing strategy, including discounts and rebates, often reflects internal company policies, inventory considerations, and volume-based negotiations, particularly within large healthcare settings.
In the intricate regulatory web, medical devices face a spectrum of oversight levels, both in the US and Europe. The FDA distinguishes devices into three risk-based classes, necessitating different degrees of regulatory scrutiny, with the highest-risk devices, such as pacemakers, subjected to the most stringent approval procedures. The need for credible evidence is balanced against innovation and access demands in an ecosystem where timely advancements in medical devices can profoundly affect patient outcomes and healthcare efficiency.
Factors Influencing Costs
The cost dynamics of conducting post-market clinical follow-up studies for medical devices in Latin America are multifaceted and reflective of the diverse economic climates within the region. While the complexity of the medical device itself and its intended use are pivotal to cost calculations—where sophisticated devices necessitate expansive sample sizes and extended study periods, thereby increasing expenses—the landscape of regulatory requirements can also steer financial planning off course. Distinct countries showcase a variance in their regulatory frameworks, which impacts overall costs of trials.
By analyzing disease incidence and prevalence data, one can pinpoint key target markets and cherry-pick a representative subset of locales to navigate the VoC research meaningfully despite the inherent subtleties among nations. The cost elements are further compounded by the pricing strategies of manufacturers, the sale location, and the technology lifecycle stage of the device. For instance, companies like Beckman Coulter tailor discounts for their wares centered on strategic, inventory, and sales considerations, which can sway the ultimate pricing, particularly in regions or institutions poised to negotiate based on volume.
Furthermore, the burgeoning emergence of Low-and Middle-Income Countries (LMICs), especially the BRICS nations (Brazil, Russia, India, China, and South Africa), introduces novel opportunities within rapidly expanding economies and an increasingly middle-class demographic demanding superior healthcare services. It is crucial to study the market valuation and trends through comprehensive analysis, as offered by industry intelligence firms like GlobalData, ensuring an informed decision-making process that accounts for the endemic intricacies of the target region. Collaborative endeavors between regulatory agencies and industry agents, expedited by agencies such as the COVID-19 pandemic, prioritize the approval of devices serving unmet medical needs, with shared aspirations to harness the growth trajectory of places like Brazil, despite its current medical equipment industry challenges that include technological integration and export limitations.
Marketing Strategies for Clinical Trials
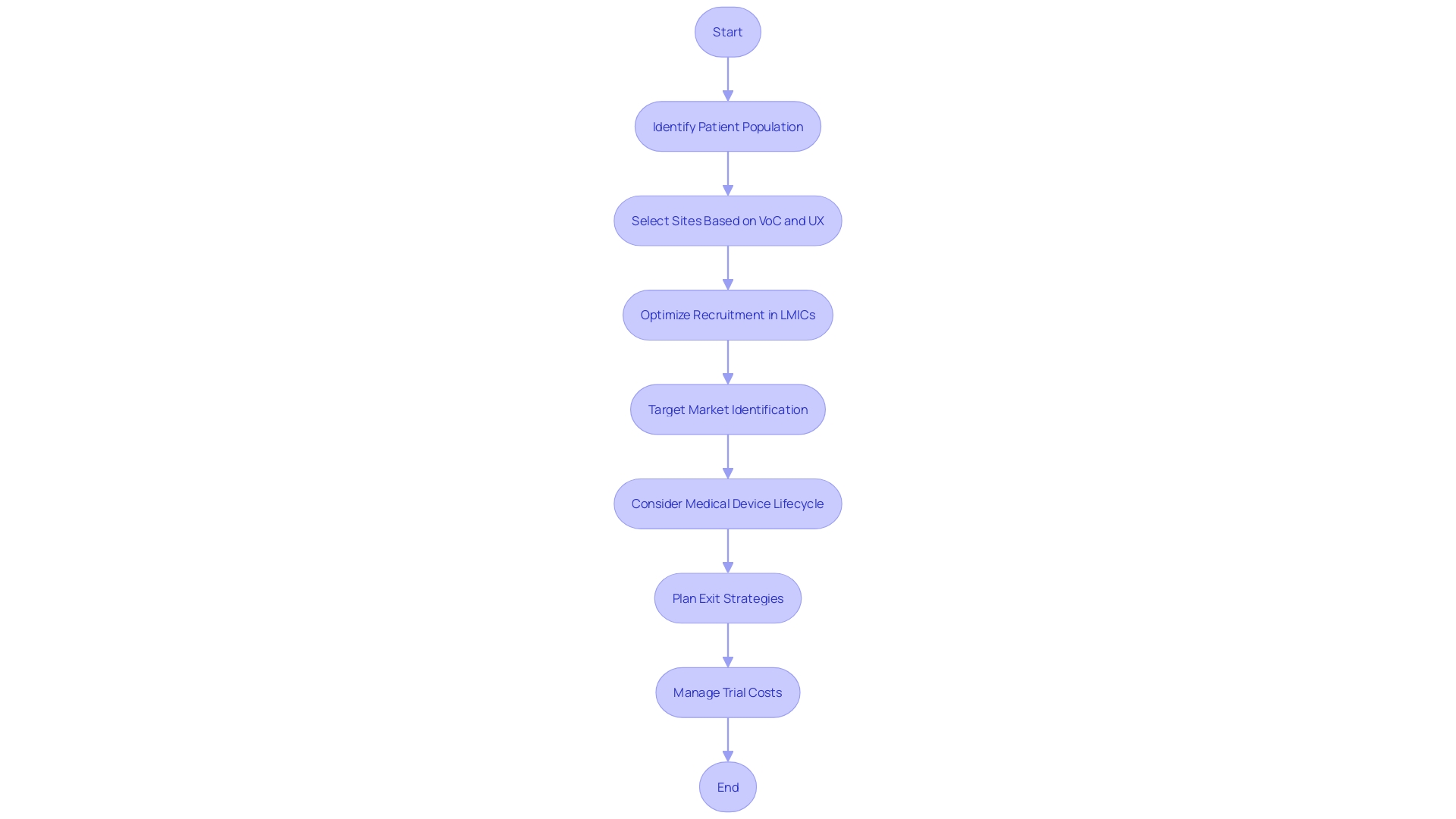
Strategizing the deployment of marketing tactics in clinical trials for medical devices is imperative, not only to ensure precise targeting of the intended patient demographics but also to achieve the requisite balance between cost-efficiency and the trial's overarching integrity. A data-driven approach to patient population identification, underpinned by disease incidence and prevalence figures, lays a foundation for judicious site selection. Enhanced by insightful Voice of the Customer (VoC) research and through the intelligent application of UX design principles, companies can develop medical devices that resonate with both patients and healthcare professionals, thereby reducing superfluous training and customer service costs.
In optimizing recruitment strategies, an understanding of the unique ecosystems within different Low- and Middle-Income Countries (LMICs) becomes crucial, as the diversity of these markets impacts both accessibility and the final pricing strategies of medical devices. An emphasis on the product's key target markets, identified through well-orchestrated VoC research, culminates in more representative and strategically selected trial sites. Such precision marketing, when executed with a comprehensive appreciation of the medical device's lifecycle and potential exit strategies like acquisitions and partnerships, supports the proficient advancement of a medical device from concept to a successful market entry while concurrently managing and often reducing trial costs.
Case Study: Successful Cost Management
A medical device company executed a cost-effective clinical trial in Latin America, addressing a common challenge of balancing quality research with financial constraints. They did this by initially identifying key target markets through data on disease incidence and prevalence, ultimately selecting a few representative locations to streamline their efforts. Furthermore, the company established strategic partnerships with local healthcare entities to capitalize on existing infrastructure and know-how, optimizing the trial process and cost containment.
To mitigate costs further, they took an innovative approach to patient recruitment by utilizing digital platforms and social media. This not only expanded their reach but also led to better retention rates. Learning from examples where certain regions like Japan or China necessitate local clinical data, the strategy also sidestepped potential expenses associated with fulfilling diverse regulatory demands across different countries.
The result: a well-conducted trial that maintained regulatory compliance without excessive spending.
Moreover, insights from the case revealed how keeping abreast with international regulatory trends—such as MHRA's recent move to expedite approval for low-risk trials—can benefit future clinical operations. These findings underline the importance of strategic planning and the use of digital tools in conducting cost-effective post-market clinical follow-up studies in dynamically regulated environments like Latin America.
Conclusion
In conclusion, the development and market adoption of machine learning/artificial intelligence medical devices (MAMDs) in the healthcare industry pose unique challenges. Navigating regulatory compliance and insurance coverage limitations requires integrating reimbursement considerations and fostering cross-departmental collaboration, leading to time and cost savings.
Clinical trial design plays a crucial role in meeting evidentiary needs while balancing innovation and access demands. Pricing strategies are influenced by factors such as therapeutic area, development costs, and competitive scenarios. Manufacturers face varying levels of regulatory oversight in different regions and must navigate approval procedures accordingly.
In Latin America, conducting post-market clinical studies for medical devices entails complex cost dynamics shaped by device complexity, regulatory requirements, pricing strategies, and economic climates. Analyzing disease data helps identify key target markets, promoting precise targeting and cost-efficiency. Staying informed about international regulatory trends is crucial.
Effective marketing strategies are essential for target precision, cost-efficiency, and maintaining trial integrity. A data-driven approach, combined with Voice of the Customer research, ensures the development of resonating medical devices. Careful site selection and utilizing digital platforms for patient recruitment enhance effectiveness and reduce costs.
A successful case study in Latin America underscores the importance of selecting key target markets, establishing strategic partnerships, utilizing digital platforms for patient recruitment, and staying informed about international regulatory trends. By considering these factors and implementing effective strategies, medical device companies can achieve cost management while conducting clinical trials in complex environments.
To summarize, addressing the challenges of MAMD development and market adoption involves integrating reimbursement considerations, collaborating across departments, designing clinical trials carefully, and strategizing marketing tactics. By doing so, medical device companies can achieve cost management and success in demanding environments.




