Introduction
The 1572 Form is a critical document in the field of clinical research, serving as an agreement between investigators and sponsors to uphold study protocols and prioritize participant welfare. It reflects the commitment to ethical conduct and data integrity, ensuring that research findings are valid and reliable. This article explores the purpose and importance of the 1572 Form, when and who needs to complete it, the information required, completion and submission guidelines, updating and revising the form, the responsibilities of investigators, consequences of non-compliance, and special considerations for foreign clinical studies.
By understanding the significance of the 1572 Form, researchers can conduct clinical trials responsibly and with integrity, advancing medical science while prioritizing participant safety.
Purpose and Importance of the 1572 Form
The 1572 Form is integral to the clinical research process, embodying the agreement between the principal investigator and sponsor to uphold study protocols, regulatory demands, and the safeguarding of participant welfare. This form is a testament to an investigator's pledge to conduct the study ethically, ensuring the rights, safety, and well-being of all participants are prioritized. It also reflects the investigator's commitment to maintaining the integrity and credibility of the data collected.
Case studies highlight the transformative impact of clinical research, with participants like Barbara discovering life-saving health information as a result of trial involvement. This underscores the importance of rigorous adherence to ethical and regulatory standards, as delineated in the 1572 Form, to safeguard participants and the validity of research findings.
In the evolving landscape of clinical research, recent initiatives like 'The New Normal' portal have successfully recruited healthy participants by raising awareness and facilitating access to research opportunities. The success of such platforms exemplifies the need for effective communication and ethical considerations in participant recruitment, as stated in the 1572 Form.
The ethical perspective is crucial, with reimbursement and compensation being recognized as essential for treating participants fairly. The Declaration of Helsinki, a cornerstone of medical research ethics, underscores that participants should be treated no differently from others who contribute to public good, such as first responders, who are compensated for their service.
Daniel J. Herron emphasizes patient-centricity in clinical trials, advocating for the inclusion of diverse populations to ensure a wide range of perspectives and needs are considered. This aligns with the commitment to participant welfare that the 1572 Form requires.
Emerging technologies in clinical research are also enhancing patient monitoring and safety. Initiatives like iTraXS aim to prevent pressure injuries and assist with vital sign monitoring, offering a glimpse into the advancements that are being integrated into clinical trials, further emphasizing the importance of the 1572 Form in ensuring that such innovations adhere to the highest standards.
In conclusion, the 1572 Form is not merely a procedural requirement but a critical document that reinforces the ethical and regulatory framework essential for conducting clinical research responsibly and with integrity.
When to Complete and Sign the 1572 Form
Before any clinical trial activities commence, it is imperative for investigators to complete and sign the Form 1572. This critical step typically occurs in the trial's start-up phase, following the review and approval of the protocol and other associated documents. The act of signing this form is more than a mere formality; it represents the investigator's commitment to adhere to the study's protocol and abide by stringent regulatory standards.
Clinical trials are the backbone of medical advancements and are meticulously designed to evaluate new treatments, interventions, and technologies. For instance, phase one trials primarily focus on safety with a small cohort of volunteers, while phase two trials expand to assess both efficacy and safety among a larger group, including patients with the relevant condition. The culmination of these efforts is to deliver treatments that are not only safe but also more effective or with fewer adverse effects compared to existing options.
Innovative technologies are playing a significant role in streamlining the clinical trial process. Advances such as the HINT algorithm and SPOT system, developed at the University of Illinois Urbana-Champaign, leverage predictive modeling to potentially improve trial success rates and inform design decisions. These tools exemplify the increasing influence of artificial intelligence in drug development, as highlighted in discussions at industry conferences and podcasts featuring experts like Google's Scott Penberthy.
Moreover, the accessibility of clinical trial information has greatly improved over the past decade. Online services, in collaboration with organizations like EmergingMed, now offer user-friendly tools to help patients find relevant trials by filtering through various criteria, such as disease stage and location. However, participants must be cognizant of the additional costs that may be incurred, such as travel expenses and time away from work, even though the treatment under trial itself is provided at no extra cost.
The importance of compliance with Good Clinical Practice (GCP) and the current Good Manufacturing Practices (cGMP) cannot be overstated, as it ensures the integrity and quality of the trials. Public databases like ClinicalTrials. Gov have become instrumental in fostering transparency by mandating the registration and publishing of clinical trial results, thereby enabling the sharing of knowledge, including that of unsuccessful trials, which is crucial for the progression of medical research.
Who Needs to Complete the 1572 Form
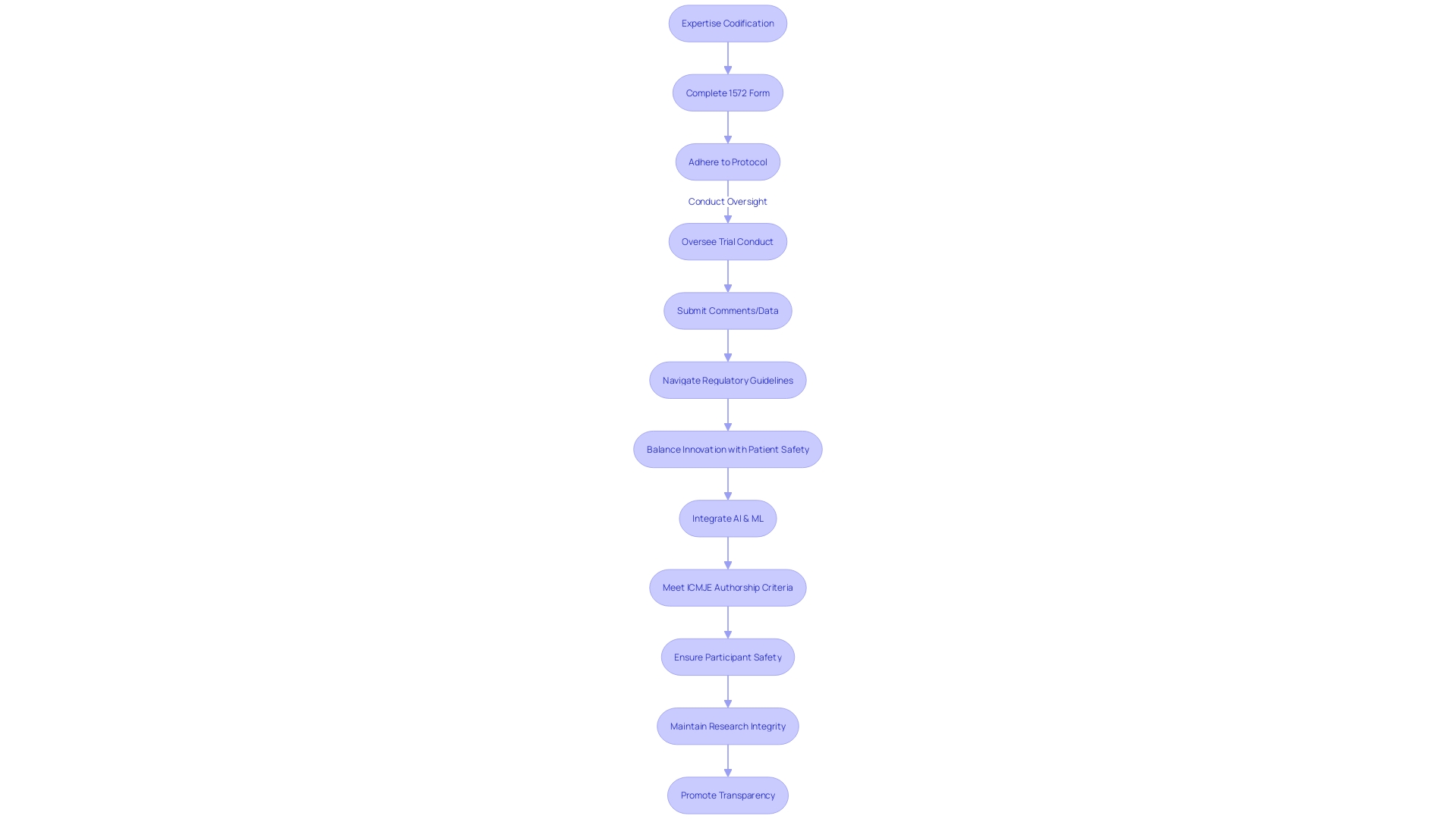
The principal investigator (PI) plays a critical role in clinical trials, and their expertise is codified through the completion of the 1572 Form. This document is not only a testament to the Pi's qualifications and experience but also serves as an agreement to adhere to the trial's protocol and oversee its proper conduct. In multicenter studies, each investigator is often required to submit a separate 1572 Form, thereby taking on the responsibility for the segment of the study conducted at their location.
Engaging qualified PIs is paramount, as highlighted by a case where a participant, Barbara, found out about a potentially life-threatening heart condition through her involvement in a clinical study. This discovery, facilitated by the research team's recruitment efforts on The New Normal—a platform designed to connect individuals with health research opportunities—demonstrates the unforeseen benefits of clinical trials.
In the context of ensuring the integrity of the trial and safeguarding confidential information, PIs must navigate the submission of comments and data with meticulous care. This process is subject to public transparency, as outlined by the FDA, where submitted comments are accessible in the docket without redaction, emphasizing the need for discretion regarding sensitive data.
Moreover, the landscape of clinical research is evolving with the advent of artificial intelligence (AI), as discussed in the Bioworld Insider Podcast. Ai's potential to hasten the drug development process and revolutionize clinical trials signifies a future where PIs may oversee more technologically advanced and efficient studies.
In terms of manuscript preparation, the individuals who accept direct responsibility for the content should meet the criteria for authorship as per the International Committee of Medical Journal Editors (ICMJE) guidelines. This ensures that contributions are properly acknowledged, and the integrity of authorship is maintained.
The clinical trial environment is complex and ever-changing, with industry involvement and transparency in trials being a significant focus. Industry-sponsored trials often lack public access to detailed protocols and statistical analysis plans, a gap that calls for increased transparency to enhance research reproducibility and trust.
In summary, the PI's role encapsulated by the 1572 Form is foundational to the success and integrity of clinical trials, with responsibilities extending from ensuring participant safety to maintaining rigorous adherence to research protocols and ethical standards.
Information Required on the 1572 Form
The 1572 Form stands as a pivotal document in clinical research, outlining an investigator's qualifications like their medical licensure, educational background, training, and experiential credentials. It further delineates the specifics of the study site, encompassing the location, available facilities, and resources at hand. This form also plays a critical role in maintaining transparency by requiring the disclosure of any financial interests or affiliations that might pose a conflict of interest, ensuring the integrity of the study.
When considering the involvement in clinical research, the process extends beyond form-filling. Real-life stories illustrate the profound impact participation can have on individuals. For instance, Barbara's participation in a research study, which she discovered through an online matching portal, not only facilitated her learning about her health but indeed proved life-saving when a heart condition was detected. This underscores the vital importance of patient-awareness and informed decision-making in clinical trials.
Moreover, the digital age has brought about innovative solutions like AI-driven platforms that assist in matching patients with appropriate trials, streamlining the recruitment process while maintaining privacy and consent through careful handling of medical records. Such technology, combined with the knowledge and guidance from healthcare providers, enhances the efficiency and effectiveness of the trial matching process.
In the realm of drug development, exhaustive details are required to guarantee the drug product's quality and safety. From the ingredients used to the manufacturing processes and packaging procedures, every aspect is meticulously documented. This includes stringent specifications for components, in-process controls, analytical procedures, and stability data to ensure the drug product's identity, strength, quality, purity, potency, and bioavailability.
The importance of hypothesis generation and testing is another cornerstone of clinical research, as it provides the foundation upon which studies are built and grants are awarded. The research surrounding statin use and its purported long-term effects on cancer risk exemplifies the need for a hypothesis-driven approach that is transparent and reproducible, with data analyses that are accessible for scrutiny.
Finally, the issue of transparency in clinical research remains a pressing concern. With variable commitments from companies and a need for public access to protocols and statistical plans, there is a push for full disclosure of trial information. This movement is not only about transparency but also about enabling broader access to raw data, fostering a research environment that prioritizes openness and collaboration for the advancement of medical science.
Completion and Submission Guidelines
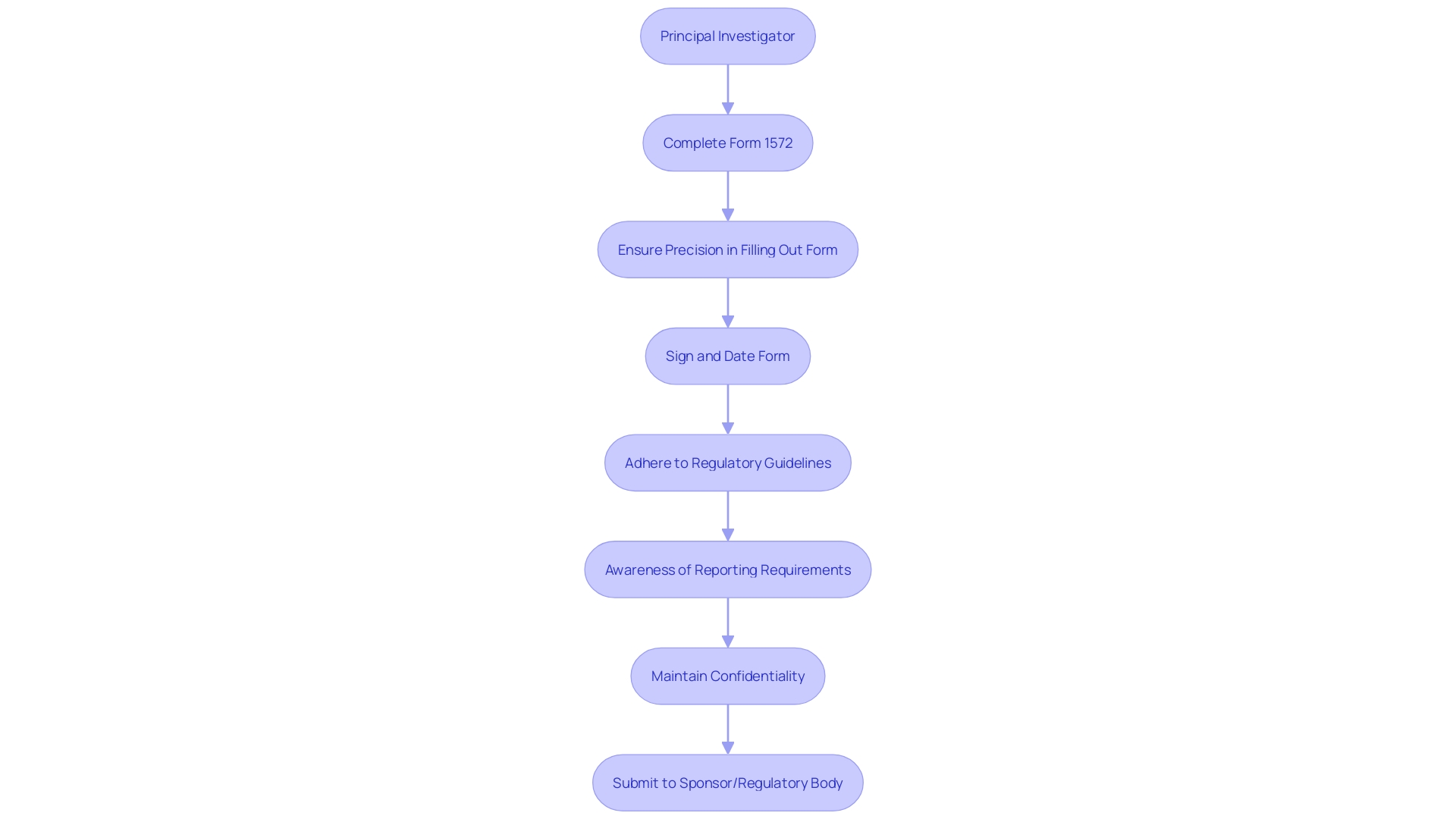
Accurate and thorough completion of the Form 1572 is a cornerstone requirement for clinical research, as it serves as a critical document that outlines the responsibilities of the principal investigator and the framework of the study. Investigators are required to complete the form with precision, ensuring that it is filled in using legible handwriting or typing to avoid misinterpretation and to facilitate review. The form must be signed and dated by the investigator to attest to the accuracy of the information provided and to signal readiness to comply with the associated regulatory, ethical, and study-specific obligations.
Once finalized, the original signed Form 1572 must be submitted to the sponsor or the appropriate regulatory body, such as the FDA. This is a standard procedure that aligns with the regulatory expectations for initiating clinical trials. Submissions should adhere to the guidelines provided by the regulatory authorities or the study sponsor, which often detail the manner and format of submission, including any electronic submission portals or specific address information for paper submissions.
It is crucial for investigators to be aware of the evolving landscape of clinical trial reporting and regulatory compliance. For example, the recent draft guidance issued by the FDA on the use of real-world evidence in medical device regulation indicates a shift towards integrating more diverse data sources into regulatory decision-making. Additionally, the modernization of platforms like ClinicalTrials. Gov reflects ongoing changes in trial reporting requirements, emphasizing the importance of keeping abreast of current policies and ensuring that submitted information meets the latest standards.
As clinical research continues to advance and incorporate new regulatory frameworks, investigators must remain vigilant in their submissions and mindful of the confidentiality of the information they handle. In the public domain, such as when providing comments to the FDA, individuals must take care not to disclose sensitive personal or proprietary information, as these submissions become part of the public record.
In summary, completing and submitting the Form 1572 with diligence is more than a procedural task; it is an essential component of ethical research conduct and regulatory adherence. It requires an understanding of current guidelines and a commitment to maintaining the integrity of the research process.
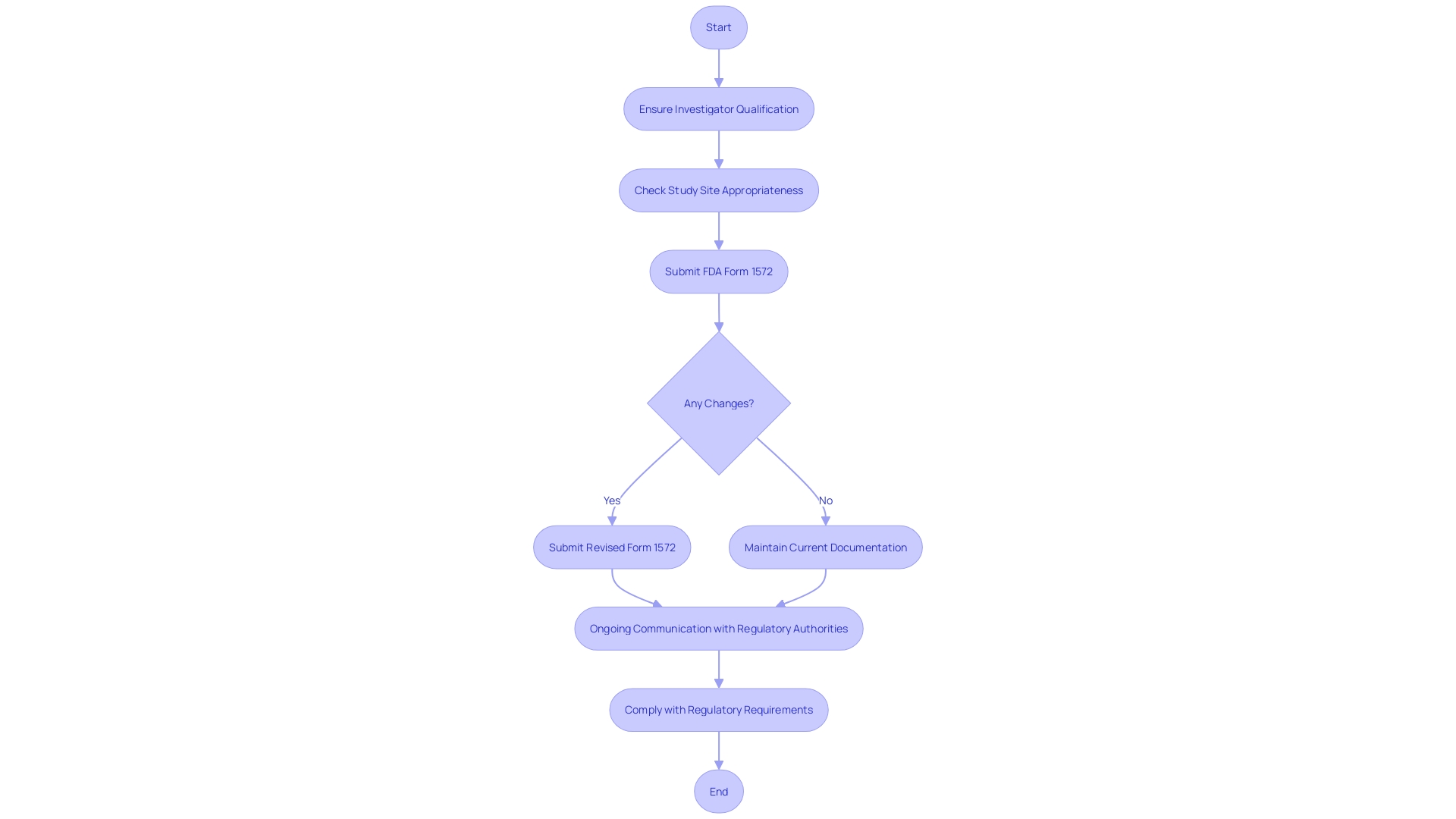
Updating and Revising the 1572 Form
Maintaining the integrity of clinical trial documentation is essential, particularly when it comes to the FDA Form 1572. This form acts as a critical piece of the regulatory framework, ensuring that investigators conducting the trials are qualified, and that the study sites are appropriate. Should there be any alterations in the details initially provided—be it a shift in the investigator's qualifications or a modification of the study site—it is imperative that a revised Form 1572 is promptly submitted. This action is more than just a bureaucratic necessity; it is a cornerstone of ethical research practices, safeguarding participant well-being and upholding the quality and integrity of the clinical trial. Sponsors and investigators alike must be diligent in these updates, communicating any changes to the relevant regulatory authorities to ensure ongoing compliance.
Reflecting on the evolution of trial reporting laws and policies over the past quarter-century, we see that the requirements for study records, such as those on ClinicalTrials.gov, have adapted significantly. What was once optional or not collected may now be compulsory, underscoring the importance of contemporaneous record-keeping. For instance, the modernized ClinicalTrials.gov platform has been designed with the user in mind, providing clear displays of both submitted data and indicating what information was not furnished by study sponsors and investigators.
In the spirit of transparency, it is also critical to understand that any electronically submitted comments related to these study records will be made public. Researchers and participants must be cautious to exclude confidential personal or business information from these comments, as they will be posted as received. If confidential data needs to be submitted, one must adhere to the guidelines for written or paper submissions, which safeguard such sensitive information.
Moreover, recent guidance from the FDA emphasizes the significance of collecting data on race and ethnicity in clinical trials to identify population-specific responses to medical products. This nuanced approach allows for a deeper understanding of how intrinsic and extrinsic factors may influence drug efficacy and safety across diverse populations, enhancing the robustness of clinical research.
In the context of patient participation, it's important to remember the profound personal impact that clinical trials can have. As researchers like Gamertsfelder and Osipenko observe, participants often bear a heavy burden, enduring invasive tests and managing the uncertainties and side effects that come with novel treatments. Their commitment not only contributes to the advancement of medical science but also carries the hope of creating a better future for subsequent generations.
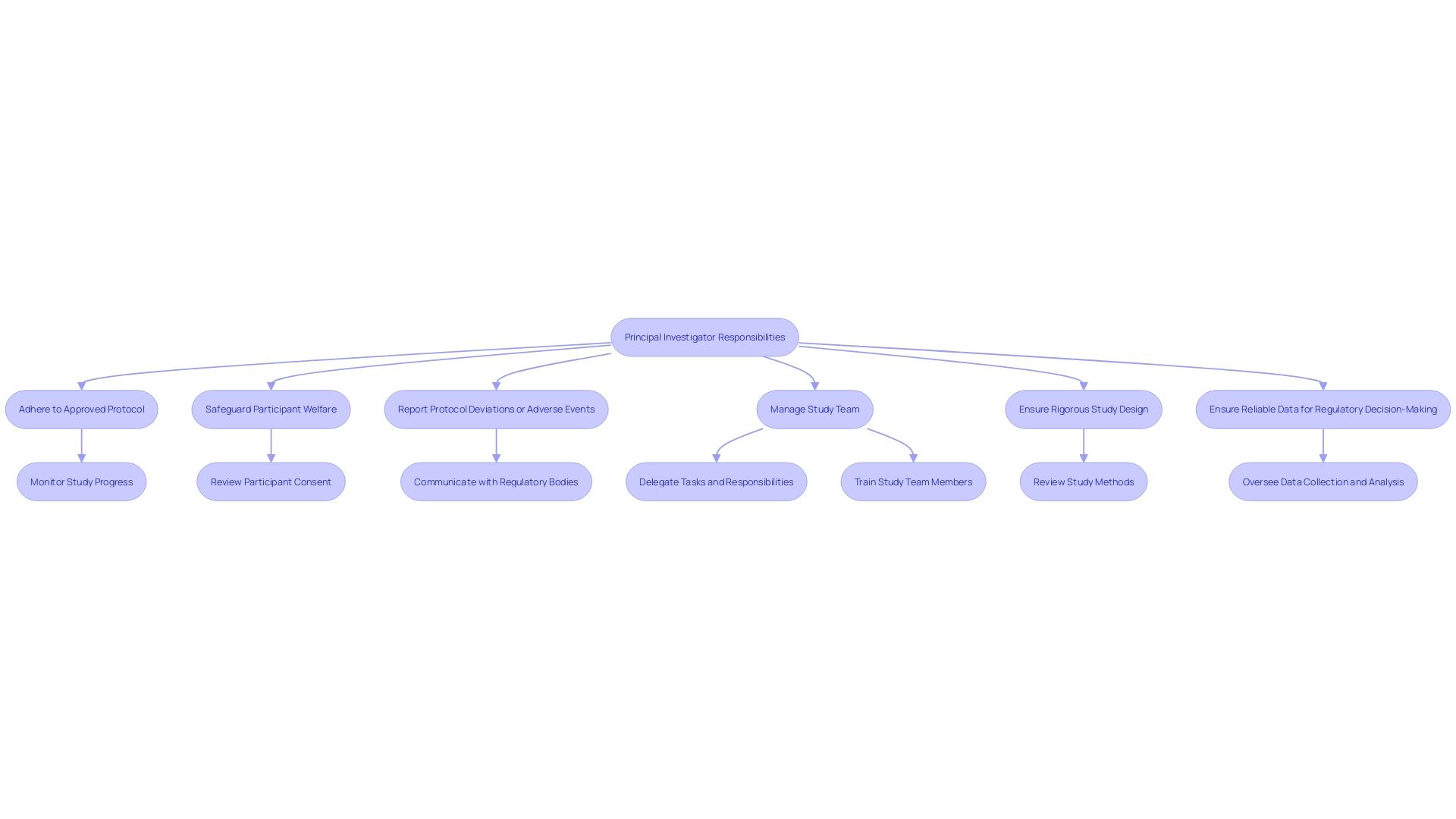
Responsibilities of the Investigator
The 1572 Form represents a cornerstone of clinical research, delineating the investigator's multi-faceted role in safeguarding participant welfare and ensuring study integrity. The principal investigator, often a seasoned healthcare professional, is mandated to conduct the study in strict adherence to the approved protocol. This includes upholding regulatory obligations, ensuring the rights and welfare of participants—particularly vulnerable populations—and maintaining precise records. The investigator must promptly report any protocol deviations or adverse events, a critical aspect underscored by recent FDA and EMA initiatives aimed at enhancing clinical trial transparency and participant safety.
Moreover, the investigator's responsibility extends to the management of the study team, ensuring that their training and qualifications align with the study's specific needs. This oversight is vital for addressing the nuanced safety concerns in the development of medical products, as highlighted in targeted clinical investigator training programs. These programs focus on the complexities of drug and biological product development, emphasizing the need for practical understanding and competency among all stakeholders, including healthcare workers and researchers.
The FDA's ongoing efforts to harmonize human subject protection regulations with the HHS Common Rule further accentuate the importance of rigorous study design and reliable data in informing regulatory decision-making. As such, investigators are crucial in facilitating well-designed research studies that can lead to medical advances, balancing the need for transparency with the protection of sensitive information. In this context, the role of the 1572 Form transcends administrative compliance, embodying the ethical and operational blueprint for conducting clinical trials that safeguard participant rights and foster medical innovation.
Consequences of Non-Compliance
The integrity of clinical research is paramount, and adherence to the 1572 Form is a cornerstone of maintaining this integrity. This form is not just a bureaucratic requirement; it is a binding document that outlines the responsibilities of the investigator to ensure the safety, rights, and well-being of participants. Non-adherence to its stipulations can profoundly affect the course of a study, its participants, and the field of research at large.
In recent years, cases like that of Nancy Olivieri, who faced legal threats for prioritizing patient safety over the interests of a drug company, underline the ethical dilemmas and potential consequences when compliance is at stake. Olivieri's commitment to transparency and participant safety, despite the risks to her own career, embodies the ethical standards that the 1572 Form seeks to uphold.
Recent studies, such as one published in the journal Facets, highlight the prevalence of non-compliance in reporting clinical trial results, with only 59% of trials registered before participant enrollment and a staggering 32% never reporting results. These statistics serve as a stark reminder of the need for stringent adherence to clinical trial protocols and the ethical considerations encapsulated in the 1572 Form.
Moreover, with the World Medical Association currently revising the Declaration of Helsinki—a document considered the ethical bedrock of medical research—there is an opportunity to address the inconsistencies and reinforce the importance of ethics in clinical trials. As the clinical research landscape evolves, the role of the 1572 Form remains central, ensuring that clinical trials are conducted with the highest standards of safety, efficacy, and ethical integrity. Failure to comply can result in severe regulatory sanctions, legal implications, and damage to the credibility of the research, potentially leading to suspension or termination of the study and disciplinary actions against the investigator.
The lessons learned from these cases and studies underscore the critical nature of compliance and the need for investigators to rigorously adhere to the requirements outlined in the 1572 Form to safeguard the trust and safety of research participants and the reputation of the clinical research community.
Special Considerations for Foreign Clinical Studies
As international clinical trials become increasingly prevalent, it's crucial to navigate the complexities of using the 1572 Form outside of the United States. Investigators must adapt to the diverse regulatory landscapes unique to each country. This includes not only being attentive to local regulations and guidelines but also addressing potential cultural, linguistic, or logistical challenges that could influence the form's accurate completion and submission. Proactive collaboration with in-country experts and regulatory bodies is essential to ensure adherence to all pertinent requirements. It is also vital to consider the public nature of electronic submissions, as outlined by the FDA, and to protect any confidential information by following the proper procedures for written/paper submissions when necessary. With countries like Japan, China, and Hong Kong necessitating local clinical trial data, and others like the UK accelerating approval processes, staying informed of global regulatory changes and opportunities is necessary for efficient and compliant international clinical research. This ensures not only the integrity of the trial but also the safety and efficacy of the medical advancements it seeks to achieve.
Conclusion
The 1572 Form is a critical document in clinical research, ensuring ethical conduct, data integrity, and participant welfare. It must be completed and signed by investigators before starting any trial activities, emphasizing adherence to protocols and regulatory standards. The form plays a vital role in maintaining transparency, facilitating participant recruitment, and ensuring compliance with Good Clinical Practice (GCP) and Good Manufacturing Practices (cGMP).
Investigators are responsible for accurately completing and submitting the form, showcasing their qualifications and agreeing to oversee the study's conduct. They must stay updated on evolving reporting requirements and regulatory changes to ensure compliance. Updating and revising the form when necessary is essential for maintaining the integrity of clinical trial documentation.
Investigators have extensive responsibilities, including participant safety, regulatory obligations, and record-keeping. Non-compliance with the form can lead to severe consequences, such as regulatory sanctions and damage to research credibility. Special considerations arise when conducting foreign clinical studies, requiring collaboration with in-country experts and adherence to diverse regulatory landscapes.
In conclusion, the 1572 Form is a critical document that upholds the ethical and regulatory framework of clinical research. Adherence to its requirements ensures participant safety, research integrity, and contributes to the advancement of medical science. Investigators must prioritize accurate completion, stay informed about regulatory changes, and maintain transparency throughout the research process.




