Introduction
Clinical trials play a crucial role in the development and approval of medical devices. Just like the process for new drug approval, medical devices must undergo rigorous evaluations to ensure their efficacy and safety.
This article explores the purpose of clinical trials, the different phases involved, key considerations for conducting trials, regulatory requirements, and best practices. Understanding these aspects is essential for navigating the complex landscape of medical device development and ensuring successful implementation in the market.
Understanding the Purpose of Clinical Trials
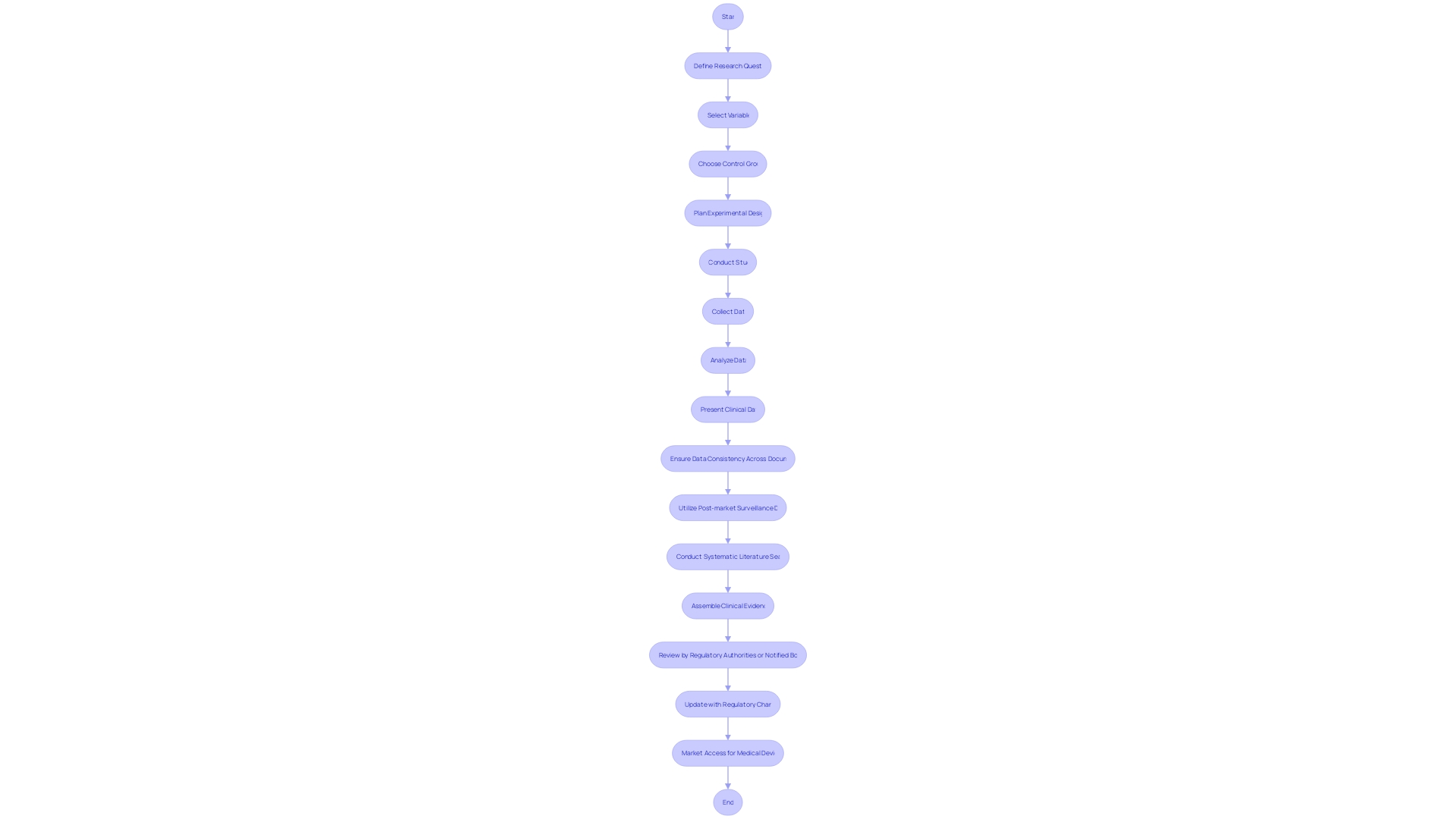
The journey of developing machine learning/artificial intelligence medical devices (Names) shares similarities with the arduous path of new drug approval, where both must initially be refined in a laboratory setting before undergoing stringent efficacy and safety evaluations. To secure regulatory blessings, researchers must meticulously design their studies around a precise research question, determining the independent variables to manipulate and the dependent variables to measure.
Selecting a suitable control group is paramount to establishing the validity of the study, which often involves a comparison between the treatment group and a placebo group. The study design is critical in minimizing potential biases and confounding factors, necessitating a comprehensive plan that details the investigation type, endpoints, variables, device information, subject selection criteria, and strategies for bias reduction, such as randomization.
A coherent presentation and thorough analysis of clinical data are indispensable, as inconsistencies can lead to a disconnect between the drawn conclusions and the actual data. Post-market surveillance data, which provides insights from both similar and the company's own products, must be analyzed with equal rigor to ensure continuous improvement and compliance. Furthermore, medical device manufacturers must navigate the complex landscape where the FDA's safety and effectiveness assessments do not always align with the data requirements of payors, leading to potential delays or denials in coverage and reimbursement post-approval. This regulatory environment underscores the importance of not only technological innovation but also the strategic planning and execution required for successful medical device implementation.
Phases of Clinical Trials
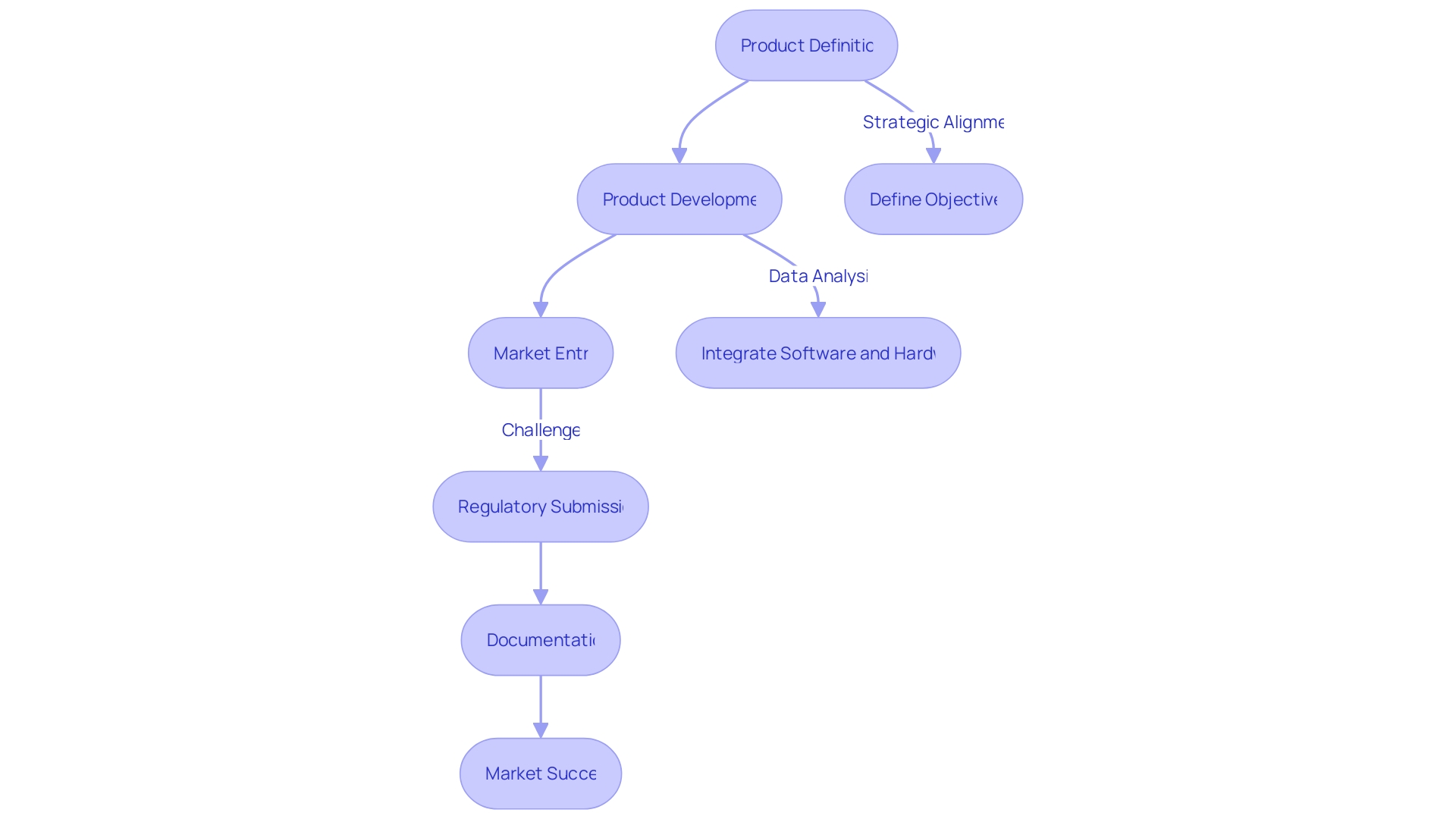
The journey from concept to commercialization for medical devices is meticulously structured into distinct phases, each with its own set of objectives and challenges. Phase One, often termed Product Development, is a crucial step where the groundwork for future success is laid.
It's the stage where the device's purpose is crisply defined—be it achieving commercial success, creating a clinical device, or securing the next round of funding. The clarity of this goal is paramount as Phase One typically requires a significant increase in resources and cost compared to Phase Zero, which focuses on Product Definition.
Strategic alignment during this phase is essential to formulate a plan that is precise and targeted, avoiding the pitfalls of overambition or conflicting objectives. Indeed, the path for machine learning/artificial intelligence medical devices (Names) mirrors the rigorous process of new drug development, with both requiring extensive lab development followed by detailed testing for efficacy and safety.
Commercial viability remains a high bar for both, and it's crucial that technological innovation does not eclipse the fundamental requirements for successful market implementation. Moreover, the process of clinical trial participation has evolved.
A decade ago, finding a clinical trial was a daunting task, often limited to searching through the National Institute of Health's website. Today, the landscape has changed with online services simplifying the search for trials by disease stage, location, and other factors. These advancements, however, also bring to light the complexities of trial participation, such as managing travel logistics for international studies, understanding language barriers, and the financial implications of travel and potential lost work time. As we consider the multi-faceted approach to medical device development, it's clear that a strategic, well-informed, and meticulously planned process is key to navigating the challenging terrain from ideation to market entry. The alignment of objectives, detailed data analysis, and the integration of software and hardware components are all critical components in the success of new medical device launches.
Phase 1: Pilot Stage
The initiation of Phase 1 clinical trials marks a pivotal moment in medical device development, where a new device is first introduced to human subjects. Often involving a select group of participants, these trials are essential for evaluating the safety profile of the device and establishing the parameters for its use.
The scope of Phase 1 encompasses the meticulous analysis of the device's interaction with the human body, monitoring for any potential adverse effects or complications that may arise. A well-defined objective for Phase 1 is paramount, as echoed by industry experts, who stress the importance of clarity in the trial's purpose—be it achieving commercial viability, clinical application, or securing subsequent funding.
This phase demands a substantial increase in resources compared to the preliminary Phase Zero, with heightened costs underscoring the need for precise planning. As part of this process, researchers must present a comprehensive investigation plan, detailing the type of study, its rationale, endpoints, and the variables involved.
Information about the device, any comparators, and the selection criteria for subjects are also crucial elements to be included. To ensure the integrity of the data collected, strategies to minimize bias, such as randomization, are implemented. The clinical procedures and diagnostic methods employed during the investigation must be described, highlighting any deviations from standard clinical practice. Furthermore, the management of clinical data, including post-market surveillance, requires rigorous analysis to maintain consistency across various documents such as the clinical evaluation plan, clinical evaluation report, and risk management files. This alignment in data collection and analysis strategies is essential for drawing accurate conclusions from the study.
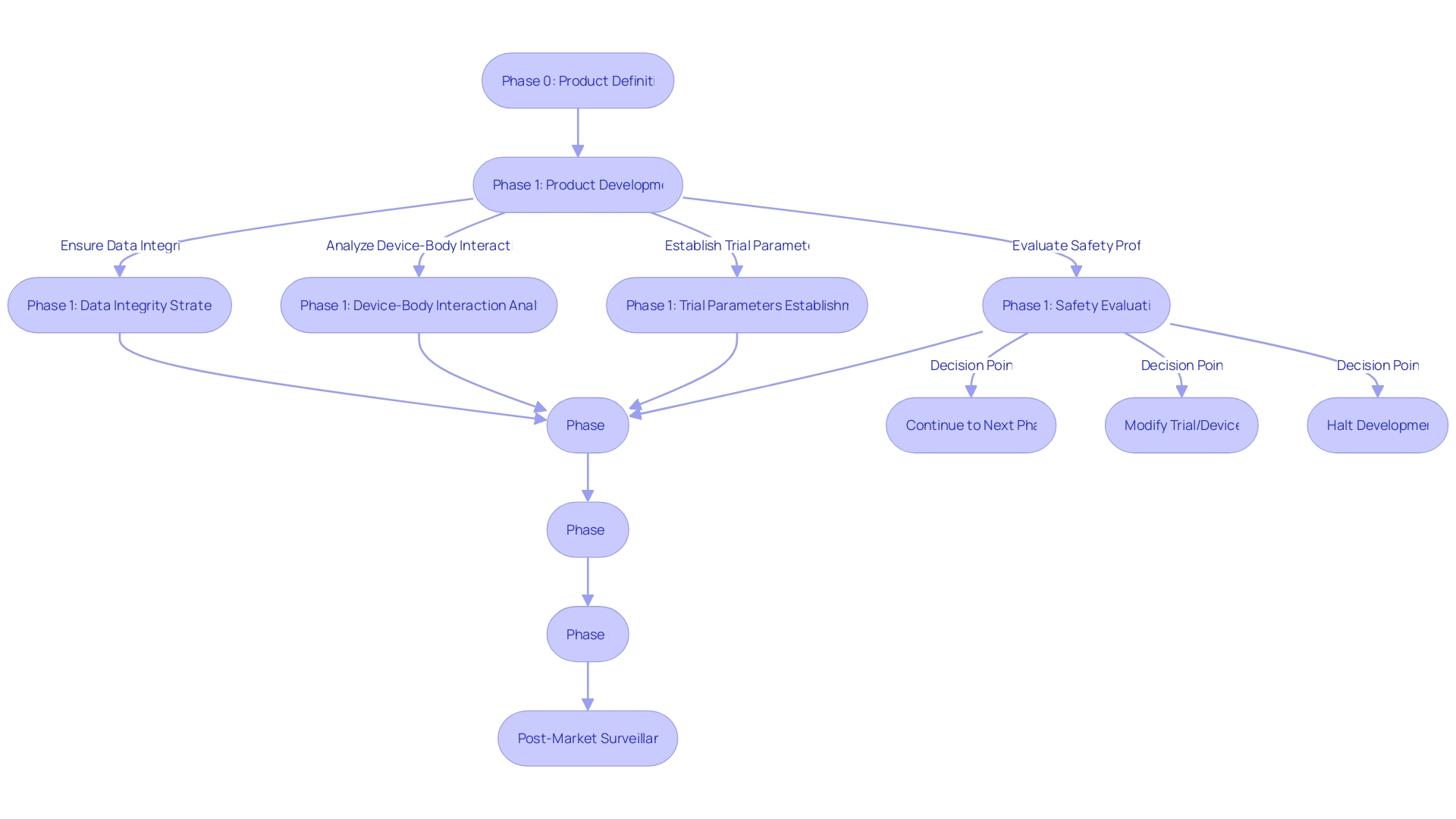
Phase 2: Pivotal Stage
During Phase 2 clinical trials for medical devices, the scale broadens to encompass patients who suffer from the condition targeted by the device. The primary aim at this stage is to acquire robust data regarding the safety and efficacy of the device, while concurrently monitoring for any adverse outcomes or hazards that could arise.
This phase is pivotal as it not only aids in enhancing the design and functionality of the device but also serves as a critical point in validating the device's clinical utility. Experts emphasize the significance of having a clear objective during the early phases of medical device development.
The focus may vary from achieving commercial viability to securing additional funding, necessitating a precise definition of goals as the scope of work and financial outlay escalate considerably from Phase Zero. It is crucial to ensure that these objectives are not only well-defined but also aligned to prevent conflicts that could derail the project.
A common hurdle encountered in this phase is the rigorous analysis and presentation of clinical data. The clarity and consistency of data narratives, as well as their alignment across various documentation, are essential to support the conclusions drawn from the trials.
Moreover, post-market surveillance data, which can provide invaluable insights, is often underleveraged in the evaluation process. This oversight can lead to discrepancies in data collection and analysis strategies that are central to demonstrating the device's safety and effectiveness to regulators and payers alike. The FDA's approval is a crucial milestone, but it does not guarantee immediate coverage or payment by healthcare providers and payors. The data submitted to the FDA might not fulfill the requirements of these entities, potentially leading to delays or denials in the device's adoption post-approval. It is, therefore, imperative for manufacturers to recognize that the approval process is just one part of a larger ecosystem involving various stakeholders, each with their own set of criteria and expectations.
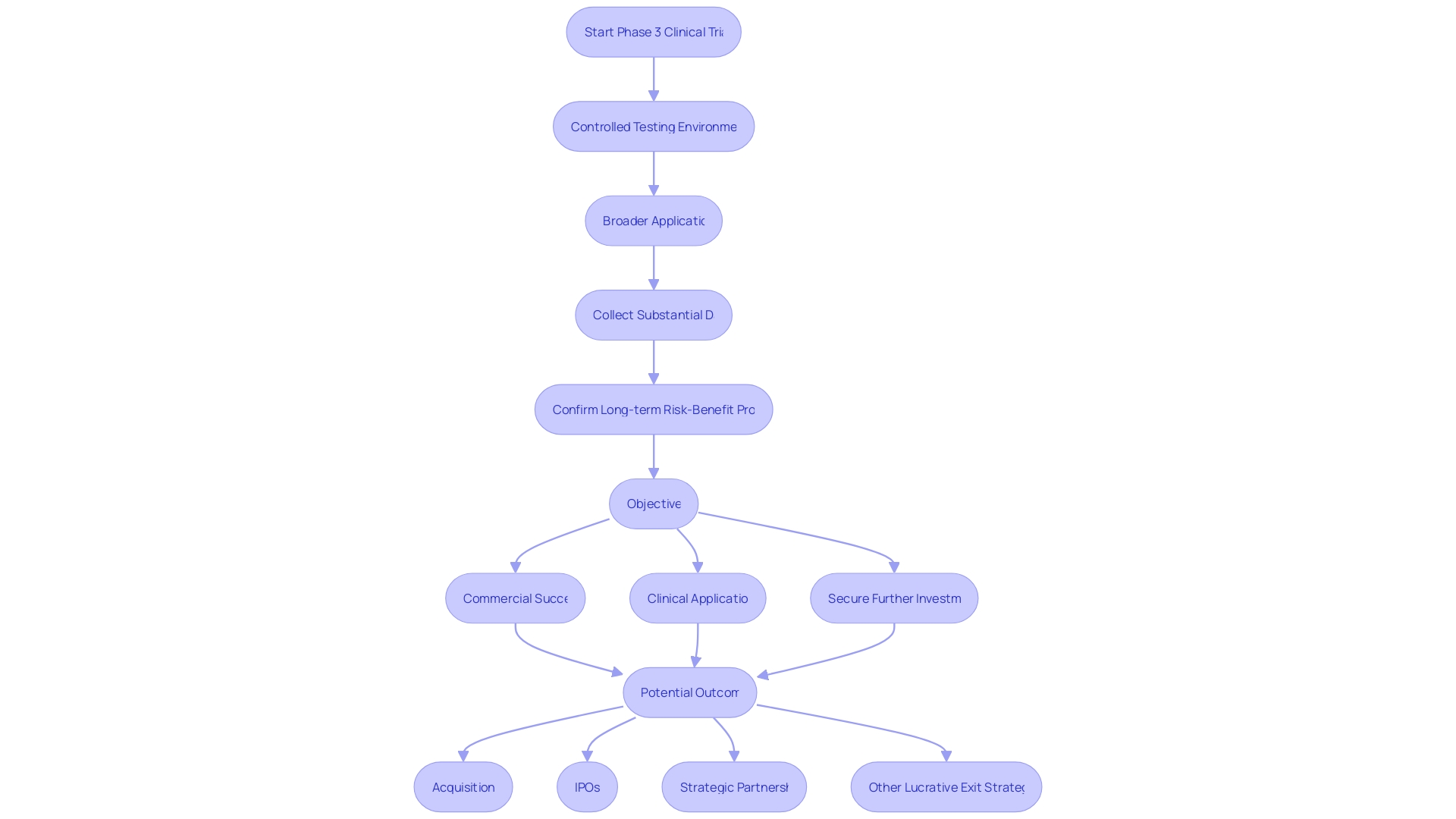
Phase 3: Post-market Stage
Phase 3 clinical trials represent a pivotal moment in medical device development, marking the transition from controlled testing environments to broader application within diverse patient populations. The primary focus of this stage is to amass substantial data on the device's efficacy, safety, and overall benefit, particularly in relation to existing therapeutic or diagnostic options. These trials are critical in confirming the long-term risk-benefit profile of the device, as well as in establishing definitive proof of its therapeutic value.
With the costs significantly higher than the initial phases of development, it's imperative that companies have a sharply defined objective, be it commercial success, clinical application, or securing further investment. This clear direction ensures that the expansion of effort in Phase 3 is meticulously planned, avoiding the pitfalls of overextension or conflicting goals. According to industry veterans, such strategic clarity, combined with traits like grit and perseverance, often characterizes the pathway to successful outcomes, whether through acquisitions, IPOs, strategic partnerships, or other lucrative exit strategies.
Key Considerations for Medical Device Clinical Trials
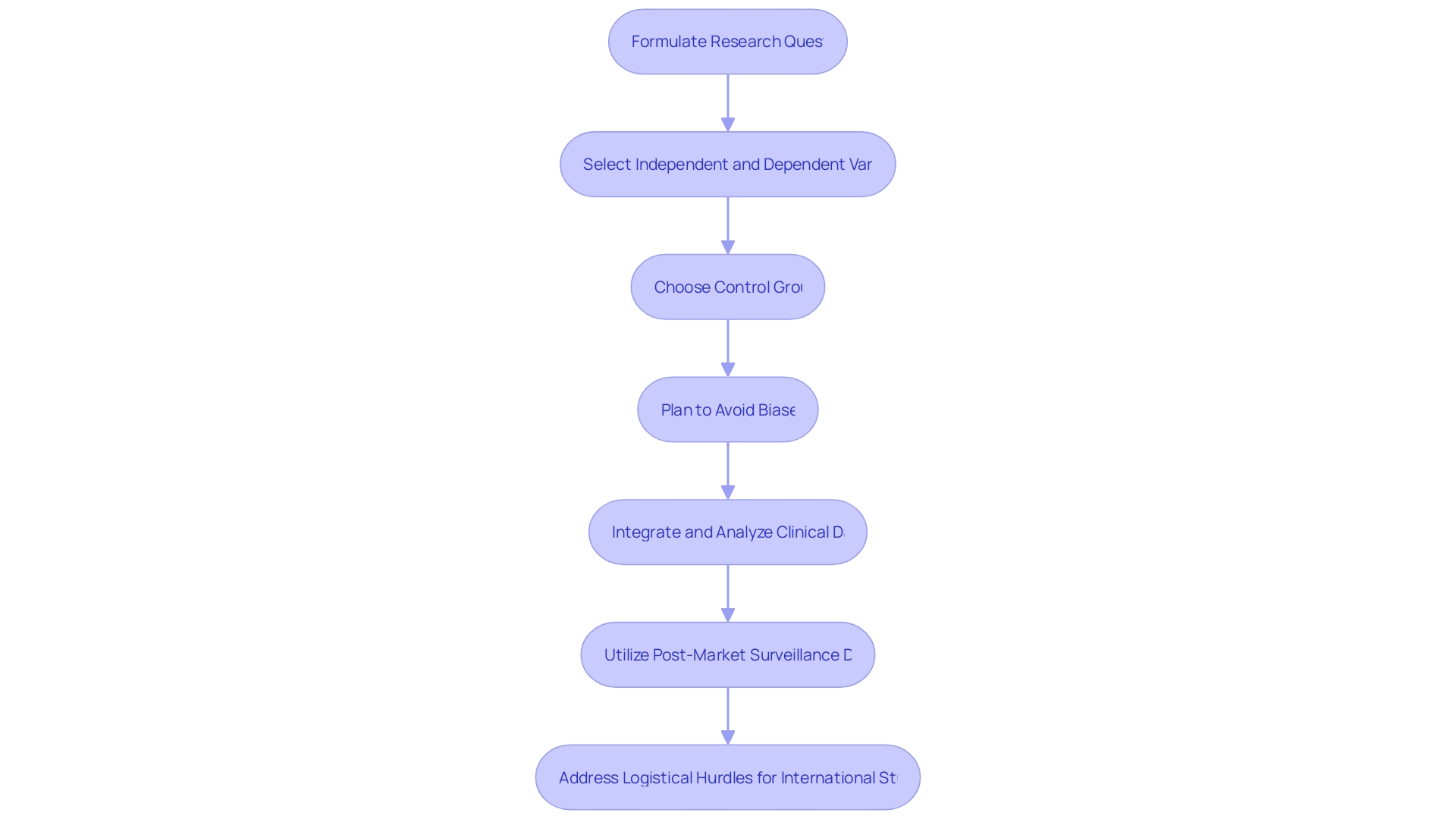
Embarking on the clinical trial journey for medical device research necessitates a strategic approach, beginning with a solid research question that guides the study's design. The research question sets the stage for selecting relevant independent variables to manipulate and dependent variables to measure.
The choice of a control group is pivotal in distinguishing the treatment effects from other influences, enabling researchers to draw credible conclusions. This process requires meticulous planning to avoid biases and confounding factors that could compromise the study's integrity.
In the realm of medical device development, the integration and analysis of clinical data are of paramount importance. It is essential to maintain a consistent and detailed narrative across all documents, including clinical evaluation plans, reports, and risk management files.
Discrepancies in data presentation can lead to an incongruous interpretation of results. Furthermore, the utilization of post-market surveillance data is often overlooked, yet it is crucial for a comprehensive evaluation of medical devices.
This data, encompassing both similar and proprietary products, demands rigorous scrutiny akin to primary data. Navigating the complexities of medical device trials extends beyond the research parameters. For instance, patients faced with participating in international studies must grapple with the logistical hurdles of cross-border travel, language barriers, and documentation, which can be overwhelming. Such scenarios underscore the need for clarity in the early phases of device development. Clear objectives for Phase One, whether aiming for commercial success, clinical application, or securing further funding, are vital. This clarity ensures that the expansion of effort and resources during this phase is well-directed and not diluted by conflicting goals.
Regulatory Requirements and Compliance
Conducting clinical trials for medical devices within the regulatory frameworks of Latin America requires meticulous planning and adherence to detailed guidelines to ensure patient safety and the validity of data. Early engagement with regulatory authorities is paramount to facilitate a smooth approval process and market access for the device.
A comprehensive investigation plan should include the type of study, the rationale for selecting it, and clearly defined endpoints and variables. The plan must also detail information about the device, comparators used, subject selection criteria, the size and representativeness of the study population, and any considerations for vulnerable subjects.
Minimizing bias is a critical component, often addressed through randomization and thorough descriptions of clinical procedures and diagnostic methods. Sections 3.1 to 3.3 of MDCG 2024-3 provide a framework for presenting information about the device and the study.
This includes identifying the sponsor, investigators, study sites, and the manufacturer, along with outlining the roles, responsibilities, and qualifications of all study personnel. A thorough description of the investigational device, its intended purpose, patient populations, and indications for use is required under section 3.2.
Section 3.3 mandates that the submission includes a comprehensive analysis of the benefits and risks associated with the device and the investigation, including a benefit-risk ratio and the rationale behind it. As the medical device industry evolves with significant innovations, regulatory oversight must also adapt. According to industry experts, "The medical device industry has witnessed significant advancements and innovations in recent years, revolutionizing patient care and delivering a range of new treatment options. However, along with these breakthroughs comes the need for stringent regulatory oversight to ensure patient safety and product effectiveness." This underscores the importance of keeping abreast of regulatory updates to prevent delays in bringing advanced medical devices to the market.
Best Practices for Conducting Clinical Trials
The medical device industry operates under the principle that the rights, safety, dignity, and well-being of clinical trial subjects are paramount. This ethos is embodied in Article 62 of the EU MDR, which also emphasizes the necessity for sound, scientifically valid, and robust clinical data.
To this end, meticulous clinical data management is not merely a regulatory checkbox but a fundamental component of patient safety and the integrity of trial results. With approximately two million medical devices on the market, as per WHO estimates, the impact of these devices on human health is profound, further underscoring the critical nature of reliable data management.
In the pursuit of clinical excellence, a well-defined research question is the cornerstone of any controlled medical study. The research design must be rigorous, minimizing biases and confounding factors through careful selection of both independent and dependent variables, and the establishment of an appropriate control group.
Such precision in study design is echoed by seasoned epidemiologists who underscore the importance of preempting and addressing potential study design flaws. As highlighted by industry experts, decisions made in the early stages of clinical trials can have lasting ramifications.
Therefore, it is imperative to invest time and energy into ensuring that each decision is bulletproof, akin to reinforcing the links in a chain, to optimize outcomes for the timeframe relevant to the company. The clinical trial landscape is not without its challenges. MedTech companies, particularly those dealing with high-risk devices, must navigate the complexities of trial management and data handling to achieve their business objectives, including market entry and retention. According to our 2024 State of the MedTech Industry Benchmark Report, these clinical activities are among the top priorities for industry leaders. The ultimate goal is to ensure that clinical trials do not just take place, but that they yield high-quality information and reliable results that meet the rigorous standards of regulatory bodies.
Conclusion
In conclusion, clinical trials are essential for the development and approval of medical devices. These trials ensure device safety and effectiveness, similar to the process for new drugs.
Key considerations include solid research questions, careful variable selection, and thorough data analysis. Regulatory requirements and compliance are crucial for successful trials.
Best practices involve prioritizing patient safety, robust data management, and well-defined research questions. MedTech companies must navigate trial complexities to meet their business goals. Understanding these aspects is vital for successful medical device development. By following these guidelines, manufacturers can confidently navigate the complex landscape of clinical trials.




