Introduction
In clinical research, obtaining informed consent is a cornerstone of ethical practice, ensuring that participants are fully aware of what their involvement entails. This article delves into the critical components of informed consent, beginning with a thorough statement of the research's purpose, objectives, and duration. It emphasizes the importance of clear communication in helping participants understand the study's goals and their role in it.
The discussion extends to a detailed description of the procedures and experimental aspects involved in the research, outlining the necessity for transparency to facilitate participants' comprehension. A comprehensive overview of potential risks and discomforts is provided, highlighting the importance of disclosing both physical and psychological challenges participants might face.
The article also explores the benefits that participants might derive, both immediate and long-term, and underscores the significance of contributing to broader advancements in healthcare. Additionally, it covers the importance of disclosing alternative procedures or treatments available outside the study, ensuring participants can make informed choices.
Further sections address the confidentiality of participants' records, the provision for compensation and medical treatment in case of injury, and the fundamental principle of voluntary participation, including the right to withdraw from the study at any time. This holistic approach aims to foster trust, transparency, and ethical integrity in the conduct of clinical research.
Statement of Research, Purpose, and Duration
Informed consent must commence with a comprehensive overview of the study's purpose. This includes a detailed explanation of the project's objectives, the expected duration, and the procedures involved. Participants need to comprehend what the study aims to achieve and why their involvement is essential. The Declaration of Helsinki underscores this necessity, emphasizing respect for individuals and their right to self-determination. In alignment with this, the Belmont Report highlights the principles of respect for persons, beneficence, and justice, which guide ethical considerations in clinical trials.
Furthermore, the Multi-Regional Clinical Trials Center's updated guidance from 2022 stresses the inclusion of key information at the beginning of the consent process. This should encompass the research's purpose, potential risks and benefits, and the study's duration and procedures. The National Organization for Rare Disorders has praised initiatives to present consent in accessible formats, such as through videos, to ensure participants' understanding, regardless of language barriers or health literacy levels. By prioritizing clear communication, researchers can foster informed, voluntary participation.
Description of Procedures and Experimental Aspects
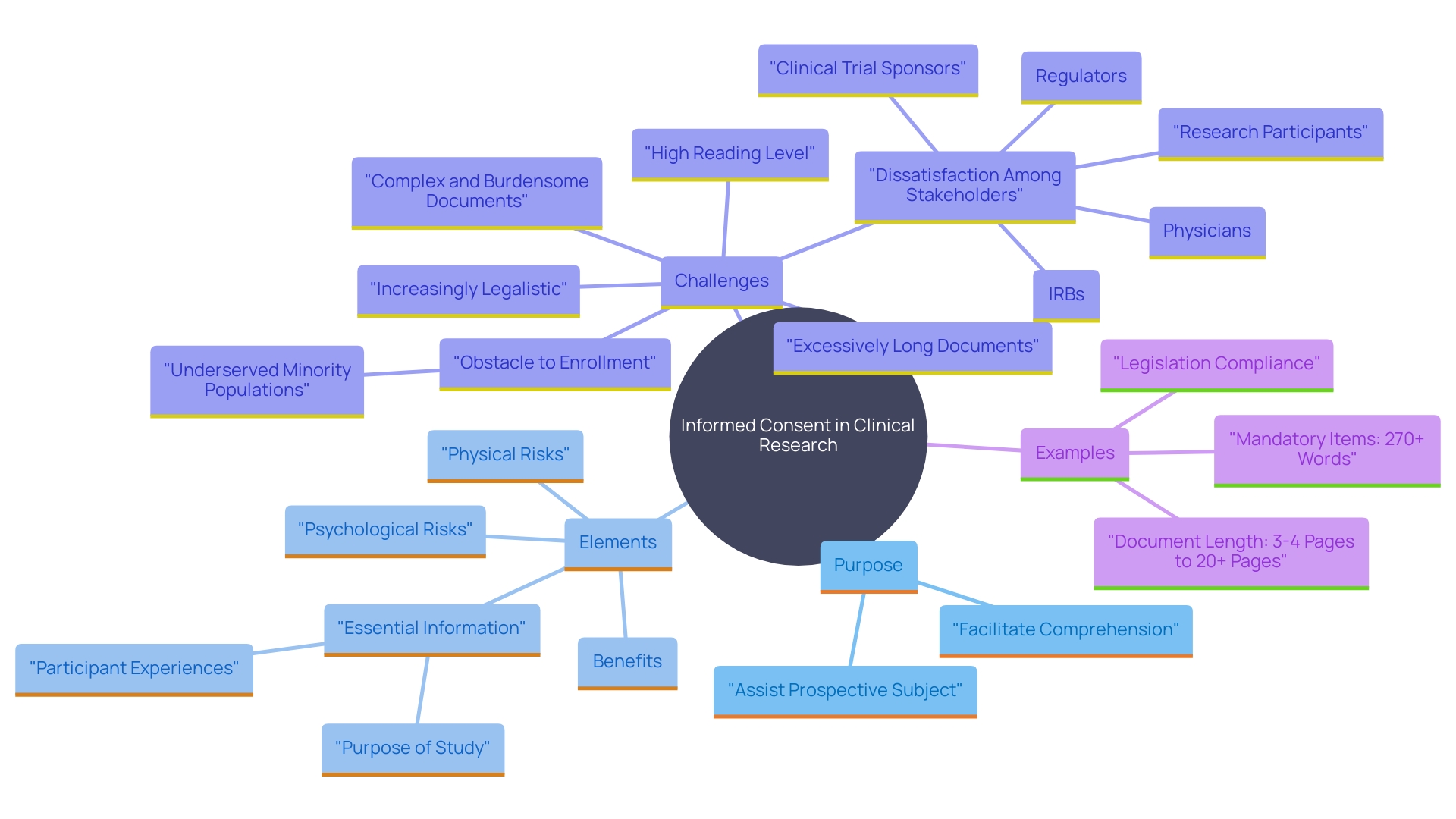
Participants must receive a thorough explanation of the research procedures, including any experimental aspects, interventions, or assessments they will undergo. This clarity is crucial to ensure participants fully grasp what their involvement entails. According to the draft guidance on informed consent, presenting key information in a clear and concise manner is essential. This encompasses detailing the aim of the investigation, possible hazards and advantages, along with the duration and methods involved. As Dawn Corbett, NIH’s Inclusion Policy Officer, emphasizes, effective communication is vital to ensure all contributors, including those from diverse backgrounds and individuals with disabilities, comprehend the study throughout its entirety. Melissa McGowan, Deputy Director of the Office of Clinical Research, also emphasizes the significance of language access to make studies inclusive and accessible to a broad spectrum of people. By adopting these practices, the investigation process becomes more transparent and accountable, empowering participants with the information they need to make knowledgeable choices.
Risks and Discomforts to the Subject
Revealing possible risks and discomforts is a vital part of understanding consent in clinical research. Participants must be informed of both physical and psychological risks to fully understand what they might face during the study. For instance, in clinical trials for conditions like transthyretin-mediated amyloidosis, individuals often endure invasive tests, manage new side effects, and worry about exposure to harmful substances. These trials, while essential for advancing medical knowledge, can exact a profound personal toll on those involved.
'Informed consent documents should present key information in a clear and concise manner, including the purpose of the investigation, possible risks and benefits, and the duration and procedures involved.'. This assists individuals in making a knowledgeable choice regarding their involvement. Recommendations from the FDA emphasize the importance of including this key information at the beginning of the consent document to facilitate understanding.
Real-world examples highlight the importance of transparency and clear communication. For example, Barbara, a contributor to the investigation, uncovered life-saving details regarding her health through her involvement. Such experiences highlight the dual nature of risks and benefits in clinical studies, making it essential for investigators to clearly communicate all possible outcomes to those involved.
Benefits to the Subject or Others
Participants must be informed of the advantages that may arise from their participation in the research. These benefits can be both direct and immediate, such as receiving valuable health insights that could lead to early diagnosis and treatment. For example, Barbara, an individual who signed up for an investigation via an online portal, uncovered a notable but previously unnoticed heart condition. She now takes medication daily and feels fortunate to have avoided a potential heart attack. This highlights how participation can lead to life-saving discoveries.
Moreover, individuals add to wider progress in healthcare and medical studies. Information from studies can guide future scientific advancements and enhance health results on a broader level. Summaries of study results can enhance individuals' awareness of their contributions, cultivating a sense of collective dedication and confidence in the process. These summaries can also serve as educational tools, enhancing health literacy and providing insights into how lifestyle choices impact health risks.
In addition, engaging in research can promote health equity by improving representation of historically underrepresented communities in biomedical research. This is crucial for ensuring that scientific advancements benefit all segments of the population. Research participation is not only about personal health benefits but also about contributing to the collective progress in medical science.
Disclosure of Alternative Procedures or Courses of Treatment
Researchers must clearly outline any alternative treatments or procedures available to individuals outside of the study. This clarity is essential for enabling individuals to make knowledgeable choices based on their personal situations. For example, the National Organization for Rare Disorders (NORD) highlights the significance of accessible consent procedures, which enable individuals to thoroughly comprehend the risks and advantages of clinical trials. This includes considering individual needs such as language barriers or health literacy competencies.
The impact of providing alternative treatment options is evident in the context of pharmacogenomic testing, where patients may receive genetic information that influences their treatment decisions. For instance, Myriad Health's GeneSight™ testing product has shown significant benefits in psychiatric care by enabling personalized treatment plans. This highlights the necessity for individuals to be aware of all available options to make choices that best suit their medical needs.
Moreover, the guidance from regulatory bodies, such as the FDA, highlights the necessity of presenting key information early and concisely in the informed consent process. This includes details on voluntary involvement and the right to discontinue, ensuring that individuals are fully aware of their options. By offering detailed information on alternative therapies and making sure it is easily comprehensible, researchers can assist individuals in making informed choices that align with their health objectives.
Confidentiality of Records and Potential Inspection
Maintaining the privacy of individuals' records is a fundamental aspect of ethical practices. This section comprehensively details the measures in place to protect data of individuals, adhering to stringent ethical, legal, and social standards. Participants are made aware of who might view their data, including scholars, regulatory agencies, and oversight groups, ensuring clarity and confidence in the study process. Notably, the FDA's guidelines emphasize the importance of presenting key information about data access and confidentiality in a clear and concise manner, facilitating understanding and informed consent. By implementing robust data privacy protocols and maintaining a transparent approach, researchers can balance the need for data utility with the obligation to protect personal privacy, ultimately fostering a more secure and trustworthy environment for inquiry.
Compensation and Medical Treatments for Injury
In the case of harm associated with involvement in the study, it is crucial to specify the compensation and medical care accessible to those engaged. This section should clearly define the rights of individuals regarding injury claims and the support mechanisms in place. By addressing ethical, legal, and social considerations, researchers can ensure transparency and trust. According to the Declaration of Helsinki, ethical practices in studies must prioritize the safety of individuals involved, emphasizing the importance of clear guidelines for compensation and medical care in case of injury. Historical precedents, such as the initial HSPC transplants performed only on terminally ill patients, underscore the necessity of robust ethical standards in studies. Additionally, global comparisons show that changing regulations and governance frameworks seek to enhance the safety of study subjects. By providing detailed information on compensation and medical treatment, researchers can uphold ethical standards and foster the confidence of those involved.
Voluntary Participation and Right to Withdraw
Emphasizing the voluntary nature of participation in research is essential to uphold ethical standards and respect for participants. Individuals must be made aware of their right to withdraw from the study at any point, without facing any penalties or losing benefits. This principle aligns with the Declaration of Helsinki and the Belmont Report, which emphasize respect for the individual and the necessity of knowledgeable consent. By reinforcing individuals' autonomy in the decision-making process, we ensure that their involvement is genuinely voluntary and informed. This approach not only protects participants' rights but also enhances the integrity and reliability of the research outcomes.
Conclusion
Informed consent is a fundamental aspect of ethical clinical research, ensuring that participants are fully aware of their involvement and the implications thereof. The process begins with a clear statement of the research's purpose, objectives, and duration, enabling participants to understand the significance of their contribution. Emphasizing transparency and effective communication throughout the consent process is crucial, as it fosters informed and voluntary participation, aligning with established ethical guidelines like the Declaration of Helsinki and the Belmont Report.
A comprehensive description of research procedures, including any experimental aspects, is vital for participants to grasp what their involvement entails. Clarity in presenting risks and discomforts, both physical and psychological, ensures that participants can make informed decisions about their participation. Furthermore, highlighting the potential benefits of participation—ranging from immediate health insights to contributions toward broader medical advancements—reinforces the importance of clinical trials in advancing healthcare.
The ethical obligation to disclose alternative procedures or treatments available outside the study empowers participants to make choices suited to their individual circumstances. Ensuring confidentiality of records and outlining compensation and medical treatment in the event of injury further upholds ethical standards and fosters trust in the research process. Lastly, reinforcing the voluntary nature of participation, alongside the right to withdraw at any time, respects participants' autonomy and enhances the integrity of the research outcomes.
By adhering to these principles, researchers can cultivate an ethical research environment that prioritizes participant welfare, promotes transparency, and ultimately contributes to the advancement of medical knowledge. The commitment to informed consent not only safeguards participant rights but also strengthens the foundation of trust necessary for successful clinical research.




