Introduction
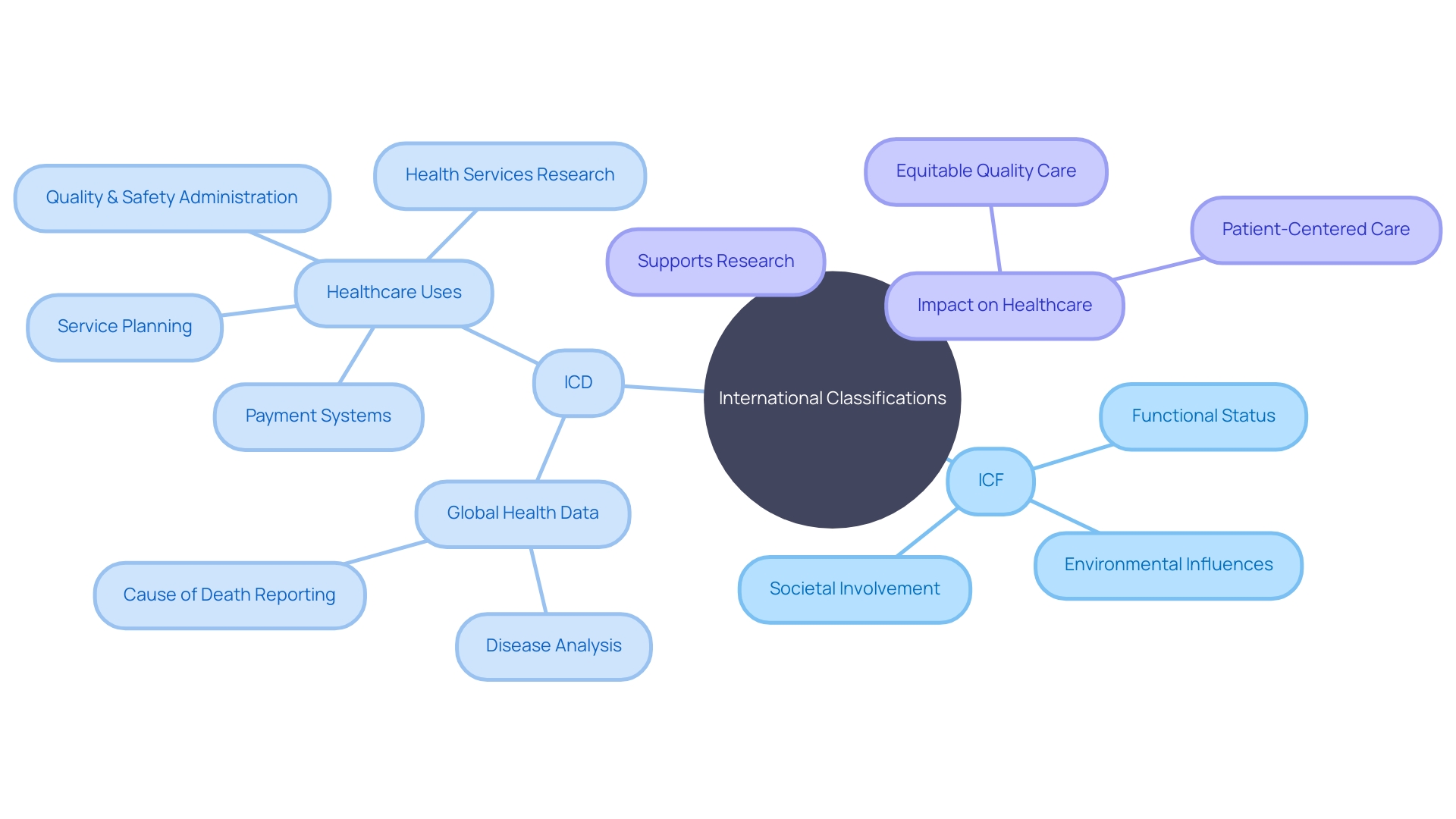
The International Classification of Functioning, Disability and Health (ICF) is a comprehensive framework established by the World Health Organization (WHO) to describe and measure health and disability levels. Unlike traditional medical diagnoses, the ICF takes into account an individual's functional status, environmental influences, and societal involvement. This inclusive approach is invaluable in healthcare and research settings, enabling the documentation and evaluation of how health conditions impact one's daily life and overall well-being.
The ICF works in parallel with the International Statistical Classification of Diseases and Related Health Problems (ICD), which provides robust classification and terminology for global health data collection and analysis. By adhering to these classification systems, healthcare professionals can better identify patients' unique needs and provide tailored responses, promoting equitable and quality care. In this article, we will explore the structure and contents of the ICF, its aims and purposes, and its applications in healthcare and rehabilitation.
We will also examine how the ICF aligns with emerging technologies and the future of healthcare delivery.
What is the International Classification of Functioning, Disability and Health (ICF)?
The International Classification of Functioning, Disability and Health (ICF), established by the World Health Organization (WHO), is an inclusive framework designed to describe and measure health and disability levels. It goes beyond medical diagnoses to incorporate the full scope of an individual's functional status, environmental influences, and societal involvement. This comprehensive approach is invaluable across healthcare and research settings, aiding in the documentation and evaluation of the consequences health conditions have on one's day-to-day life and general well-being.
Parallel to the ICF, the International Statistical Classification of Diseases and Related Health Problems (ICD) has been a critical tool for global health data collection and analysis. The latest ICD-11 iteration, implemented in January 2022, offers robust classification and terminology that allows for systematic data comparison across various regions and timeframes, fostering semantic data interoperability essential for decision making, resource allocation, and healthcare policy formulation. With a history stretching back to the 19th century, the ICD's data support numerous healthcare-related activities, from payment systems and service planning to quality administration and patient safety improvements.
Moreover, the ICD informs the certification and reporting of causes of death. By adhering to ICD standards, long-term health trends within populations can be discerned, and real-time epidemiological shifts, such as those during pandemics, can be monitored accurately. This rich vein of information propels health services research, patient-centered care initiatives, and the development of guidelines, ensuring that healthcare delivery adapts to the evolving needs of all patient groups, including those with disabilities.
Through classification systems like the ICF and ICD, healthcare professionals are better equipped to identify patients' unique needs and provide tailored responses. This is especially crucial for vulnerable groups that may face increased risk of harm in clinical settings due to systemic safety inequities. Hence, these classification frameworks are more than mere tools for recording health statistics; they serve as foundational elements that enable the delivery of equitable, quality care across the healthcare spectrum.
Structure and Contents of the ICF
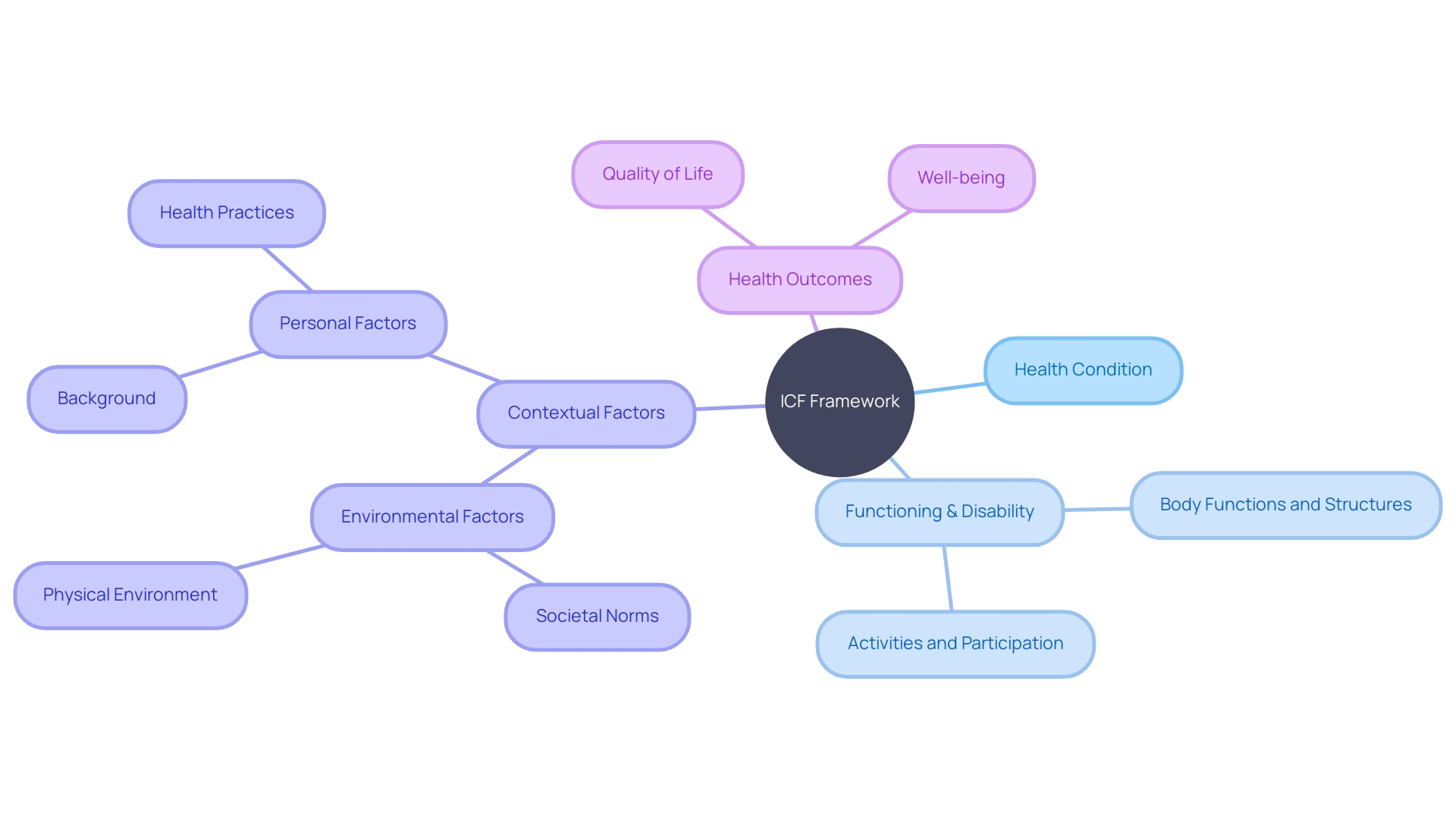
The International Classification of Functioning, Disability and Health (ICF) is a dual-component framework that intricately maps out the nuanced relationship between an individual's health condition and their overall functioning. The first component, Functioning and Disability, delves into body functions and structures, along with the level of an individual's activities and participation. The second, Contextual Factors, encompasses environmental and personal factors that further influence one’s health status.
For instance, case studies highlight how the perception of ageing among migrants in the UK, originally from India, Pakistan, and Turkey, is influenced by cultural norms that impact their engagement with health-promoting behaviors. This perspective is pivotal as it illustrates the complex interplay of societal norms and personal health practices, which are integral to the ICF framework.
The importance of such frameworks is echoed in the ICD-11, which standardizes health data collection globally. This standardization is critical as it allows for the systematic comparison of mortality and morbidity across different regions and times, enhancing our understanding of health conditions and outcomes.
Recent statistics from Statistics Canada underline the relevance of the ICF, reporting that while Canadians are living longer without disabilities, chronic conditions remain prevalent, affecting 45% of the population. These findings underscore the importance of considering both personal and environmental factors, as outlined by the ICF, in addressing health outcomes.
Incorporating the ICF within clinical and public health practices provides a comprehensive approach to understanding and improving health outcomes, by considering a person's functional status and the diverse factors contributing to it.
Aims and Purposes of the ICF
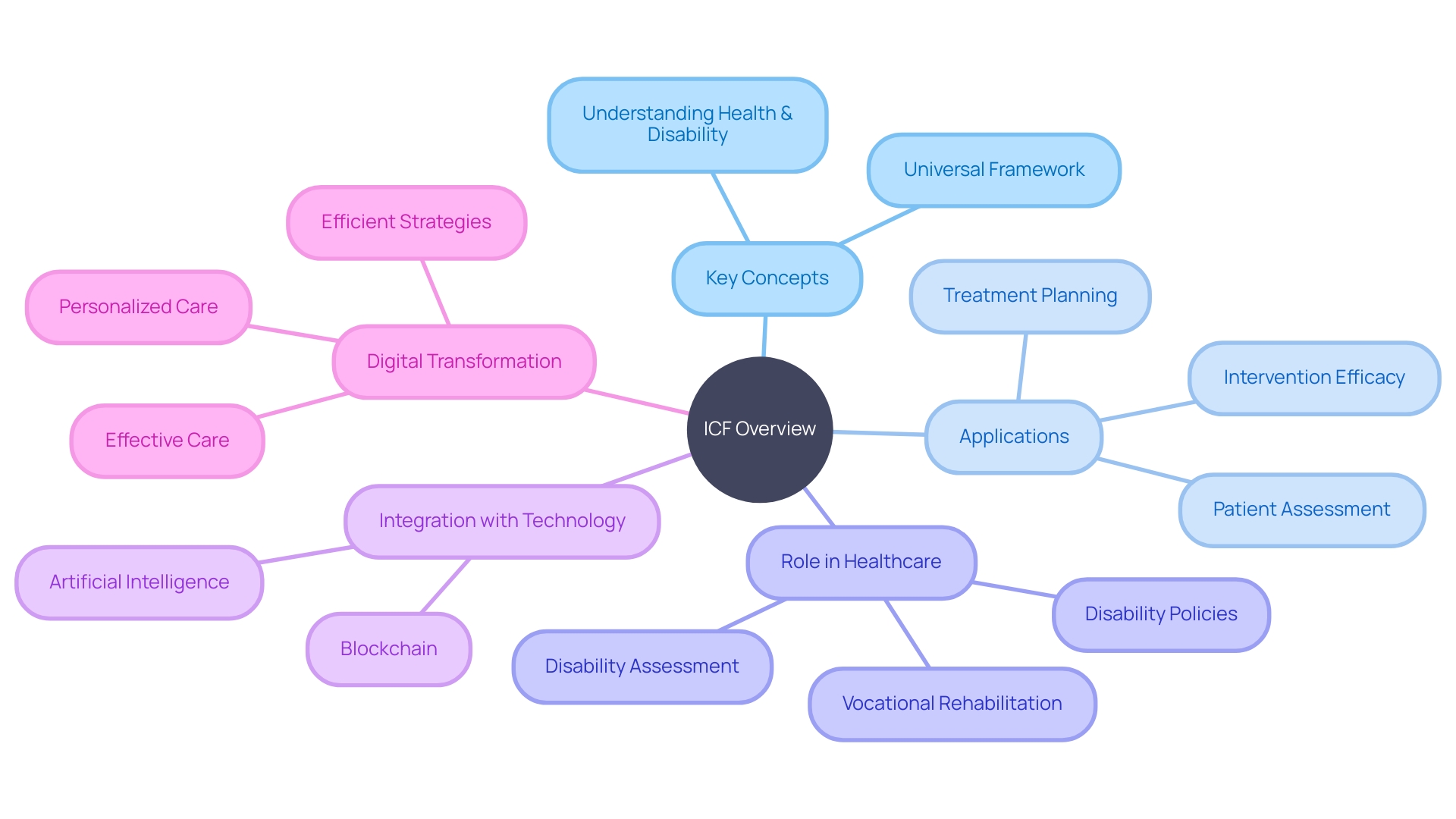
The International Classification of Functioning, Disability and Health (ICF) is a universally accepted framework developed to foster a consistent and standardized approach to evaluating and documenting the functional status and disability of individuals. ICF's comprehensive classification system transcends cultural and national boundaries, facilitating the communication and cooperation among healthcare practitioners, researchers, and policymakers. Its implementation directly impacts the assessment of intervention efficacy, the measurement of health outcomes, and the shaping of healthcare policies.
Given the global prevalence of mental health issues and the associated challenges in accessing quality care, particularly in low-income countries, the ICF plays a crucial role. Approximately one billion individuals worldwide live with a mental disorder, representing a significant portion of global disability. Despite this, there is a stark lack of access to mental health services, with an estimated 71% of individuals with psychosis not receiving the necessary care. The adoption of ICF can help bridge the gap in understanding and managing the complex interplay between mental and physical health, particularly for individuals with severe mental illnesses who are at a higher risk of physical multimorbidity.
The ICF also aligns with the current push for more inclusive healthcare systems, where access to assistive technology is severely limited. Over 2.5 billion people worldwide require some form of assistive technology, yet a mere 5-35% of those who need wheelchairs have one, and only 10% of the global demand for hearing aids is met. These statistics highlight the critical need for integrating assistive technology into primary healthcare and universal health coverage to enable full societal participation and reduce the risk of exclusion and poverty for persons with disabilities. The ICF's role in this context is to provide the necessary data and framework to support advocacy and policy development aimed at making healthcare more equitable and accessible.
Furthermore, the ICF's utility is reinforced by its linkage with the International Statistical Classification of Diseases and Related Health Problems (ICD), which has served as a pivotal tool for global health reporting and statistics. The ICD's diagnostic guidance and standardized data collection facilitate large-scale research and inform health service administration, quality control, and safety measures. Together, ICF and ICD provide a powerful combination for comprehending and enhancing patient safety, a concern highlighted by the theme of World Patient Safety Day, which emphasizes the importance of engaging patients in safety initiatives.
In essence, the ICF's universal language and classification system is indispensable for advancing global health outcomes, advocating for essential assistive technologies, and informing healthcare policies that prioritize the well-being and inclusivity of all individuals.
Applications of the ICF in Healthcare and Rehabilitation
The International Classification of Functioning, Disability and Health (ICF) embodies a universal framework for understanding health and disability. It's a tool of immense value in clinical practice, where it informs patient assessment, treatment planning, and gauges the efficacy of interventions. The ICF's reach extends into the research domain, allowing for the measurement and comparison of outcomes across various populations, interventions, and healthcare systems.
The ICF is instrumental in disability assessment, playing a pivotal role in vocational rehabilitation and shaping disability policies. Its comprehensive nature encourages a holistic view of health and rehabilitation, transcending medical conditions to encompass an individual's overall functioning and societal involvement.
Machine Learning and Digital Health are among the Medical 4.0 Technologies transforming healthcare. The integration of Artificial Intelligence and blockchain is revolutionizing the way health services are delivered, as seen in the digital-assurance process employed by healthcare institutions to vet technology adoption. This ensures that new digital technologies meet stringent standards of security, relevance, and compliance.
An example of ICF's application in modern healthcare is the use of Artificial Intelligence to standardize treatments following international clinical guidelines. This initiative, aimed at enhancing chronic wound care, illustrates ICF's potential when combined with innovative technologies.
Furthermore, ICF's relevance is highlighted by Dominic Williams' discussions at the World Economic Forum in Davos, where the future of technology in enterprise was a key topic. The ICF model can be seen as an enterprise solution within healthcare, supporting the creation of systems that improve patient outcomes. As the healthcare sector continues to embrace digital transformation, the ICF will undoubtedly be central to developing more personalized, efficient, and effective care strategies.
Conclusion
In conclusion, the International Classification of Functioning, Disability and Health (ICF) is a comprehensive framework established by the World Health Organization (WHO) to describe and measure health and disability levels. It takes into account an individual's functional status, environmental influences, and societal involvement, providing a more inclusive approach in healthcare and research settings. The ICF's structure consists of two components: Functioning and Disability, which delves into body functions and structures, and the level of activities and participation, and Contextual Factors, which encompass environmental and personal factors that influence one's health status.
The ICF aims to foster a standardized approach to evaluating and documenting the functional status and disability of individuals, transcending cultural and national boundaries. Its applications extend into healthcare and rehabilitation, informing patient assessment, treatment planning, and measuring intervention efficacy. The ICF also plays a pivotal role in disability assessment and shaping disability policies, promoting a holistic view of health and rehabilitation.
Overall, the ICF is a vital tool that enables healthcare professionals to identify patients' unique needs and provide tailored responses, promoting equitable and quality care. Its structure, aims, and applications make it indispensable in understanding and improving health outcomes, advocating for inclusivity, and informing healthcare policies.
Learn how the ICF can improve healthcare outcomes and promote inclusivity.




