Overview
Using wearable technology in post-market studies involves monitoring the safety and efficacy of medical devices after their public release, enabling continuous data collection and enhancing patient engagement. The article underscores the importance of rigorous post-market surveillance protocols, as they ensure compliance with safety standards and facilitate timely product improvements based on real-world user experiences and data.
Introduction
The evolution of wearable technology has ushered in a new era in healthcare, particularly in the realms of clinical research and patient monitoring. As these devices become increasingly integrated into medical practices, understanding their role in post-market surveillance and clinical trials is essential.
This article delves into the multifaceted landscape of wearable technology, exploring its regulatory implications, benefits, and the challenges it presents. With a focus on the critical processes that ensure the safety and efficacy of these devices, the discussion highlights the importance of data accuracy and patient engagement in enhancing clinical outcomes.
As the market for wearable health devices is projected to expand significantly, comprehending the intricacies of their application in clinical settings becomes paramount for stakeholders aiming to harness their full potential.
Understanding Post-Market Surveillance in Wearable Technology
Post-market surveillance (PMS) includes the systematic processes aimed at monitoring the safety and efficacy of medical products, particularly using wearable technology in post-market studies, after they receive approval for public use. This phase is critical as it helps identify potential issues that may arise once products are in consumer hands. Regulatory agencies, including INVIMA (Colombia's National Food and Drug Surveillance Institute), mandate PMS to ensure ongoing compliance with safety standards.
INVIMA, designated as a Level 4 regional reference health authority by PAHO/WHO, plays a pivotal role in overseeing medical equipment in Colombia, ensuring their manufacturing and marketing comply with high-quality standards. Specifically, INVIMA is responsible for:
- Evaluating medical device applications
- Conducting inspections
- Enforcing compliance with established regulations and safety standards
Using Wearable Technology in Post-Market Studies involves collecting data on device performance, user experiences, and any adverse events encountered in the field of technology that can be worn. Recent findings indicate that 58.1% of authors acknowledge the accuracy and reliability of these devices as critical to their effectiveness. A notable study led by Nigam H Shah highlights the feasibility and efficacy of an electronic health record (EHR)-based surveillance system for consumer devices, particularly for pre diagnosing atrial fibrillation (AF).
This highlights the necessity for strong PMS protocols, particularly using wearable technology in post-market studies, to guide essential product enhancements, enable prompt recalls, and guarantee regulatory adherence, ultimately improving patient safety and the overall effectiveness of innovative devices.
Furthermore, as the health and Fitbit device market is anticipated to hit USD 75 billion by 2026, the significance of these technologies keeps increasing. However, there are challenges in research on devices that can be worn, particularly in identifying all relevant studies, especially those from smaller companies or non-English publications. This highlights the necessity for comprehensive research on wearables, particularly in low-resource settings, to fully understand their potential in health research.
Involving partners like bioaccess®, with over 20 years of expertise in managing research studies—including post-market follow-up studies—can significantly enhance the evaluation and regulatory processes for medical devices in Latin America.
The Role of Wearable Technology in Clinical Trials and Patient Monitoring
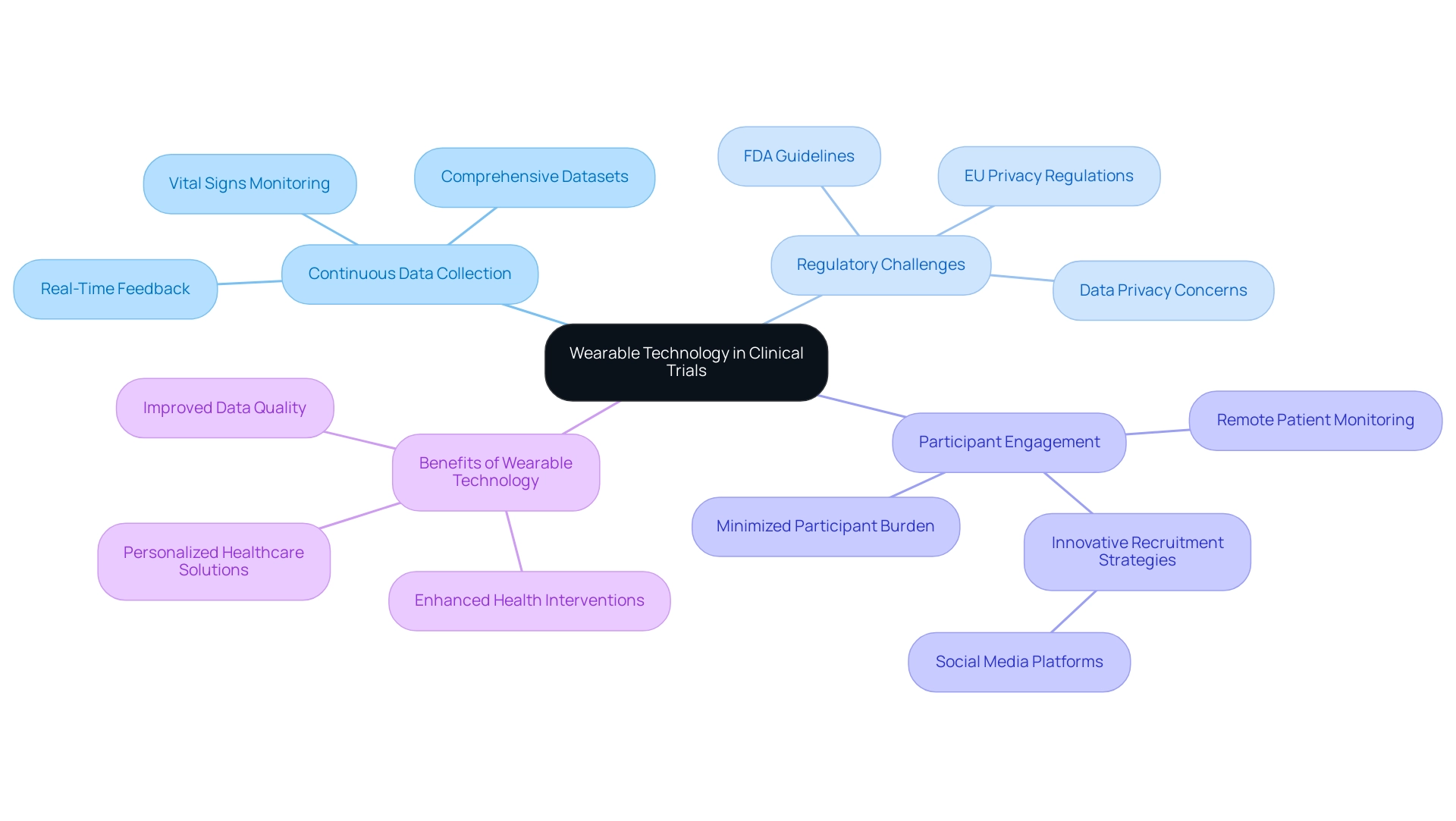
Using wearable technology in post-market studies is fundamentally transforming trials and patient monitoring through its ability to facilitate continuous data collection and real-time feedback from participants. Using wearable technology in post-market studies, devices such as smartwatches and fitness trackers are capable of monitoring a range of health metrics—including vital signs and activity levels—yielding comprehensive datasets that enhance the overall quality of clinical studies. A significant 58.1% of authors in recent analyses have underscored the accuracy and reliability of these devices, confirming their value in research settings.
Significantly, exclusion criteria in numerous studies have concentrated on those not examining wearable-generated information for health outcomes, highlighting the importance of using wearable technology in post-market studies to ensure that the findings are relevant and actionable. Furthermore, using wearable technology in post-market studies for remote patient monitoring enables innovative trial designs that decrease the necessity for frequent site visits, thereby minimizing participant burden. Researchers must also navigate challenges related to information privacy, particularly in light of stringent regulations highlighted by the European Union, which enforces the toughest privacy and security laws globally.
Additionally, the FDA has established guidelines for using digital health technologies in clinical research, addressing validation and data privacy concerns, which are crucial for maintaining participant trust and data integrity. Ensuring patient adherence to the use of these tools is also crucial for maximizing their effectiveness. Using wearable technology in post-market studies, along with innovative recruitment strategies such as those demonstrated by social media platforms, researchers are positioned to gain profound insights into patient behaviors and outcomes, paving the way for enhanced health interventions and more personalized healthcare solutions.
Regulatory Considerations for Wearable Technology in Clinical Research
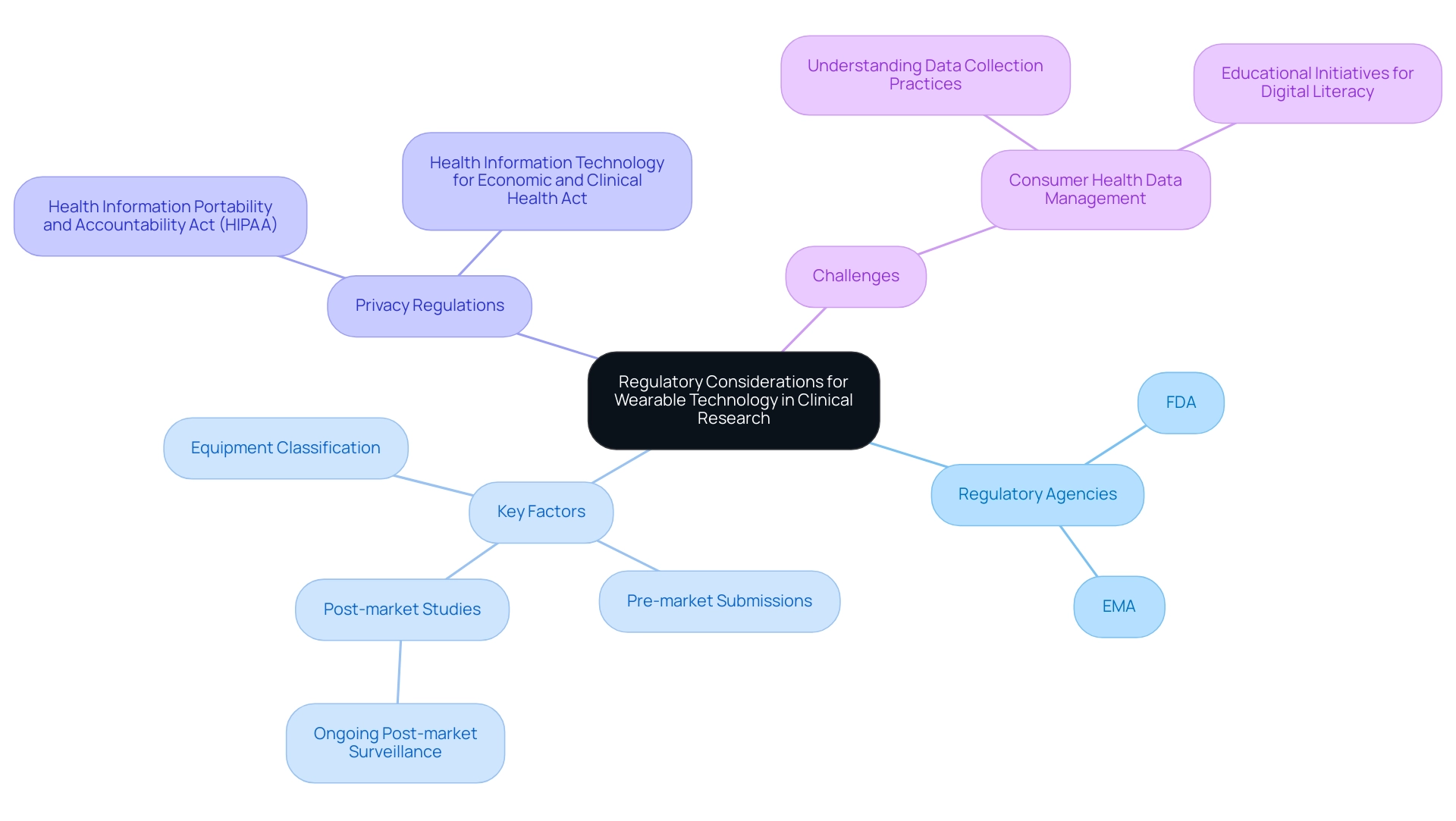
The integration of portable technology into medical research is enhanced through using wearable technology in post-market studies, which requires strict compliance with regulatory frameworks established to guarantee the safety and effectiveness of these devices. Regulatory agencies like the FDA and EMA establish extensive guidelines that oversee the testing, monitoring, and reporting procedures during research trials. For instance, the Dexcom G6, which provides real-time glucose readings every five minutes, exemplifies the practical use of technology in clinical research.
Key factors include:
- The classification of equipment
- Pre-market submissions
- Using wearable technology in post-market studies as part of ongoing post-market surveillance (PMS) requirements
The FDA's recent updates on compliance emphasize the critical need for research entities to focus on using wearable technology in post-market studies to align their practices with established standards. Furthermore, researchers must navigate protection regulations such as the Health Information Portability and Accountability Act (HIPAA), which mandates the safeguarding of patient information and requires entities to notify affected individuals 'without unreasonable delay' in the event of a personal information breach.
The Health Information Technology for Economic and Clinical Health Act further emphasizes the enhancement of privacy and security measures, although challenges persist in fully addressing issues surrounding consumer health information. Furthermore, recent advocacy for FDA supervision on health tracking information from devices highlights the significance of using wearable technology in post-market studies to guarantee reliability and precision, as well as consumer comprehension of privacy considerations. A relevant case study titled 'Consumer Literacy and Health Information Management' underscores the obstacles faced by users in understanding collection practices, particularly with wearable health devices.
This study advocates for educational initiatives aimed at bolstering digital and health literacy among these users, thereby empowering them to better manage their personal health data. By adhering to these regulatory guidelines and leveraging comprehensive trial management services—such as feasibility studies, site selection, compliance reviews, detailed trial setup processes, project management strategies, and thorough reporting mechanisms—researchers not only uphold the integrity of their studies but also reinforce participant rights, ultimately bolstering the credibility of findings. Katherine Ruiz, an expert in Regulatory Affairs for medical products and in vitro diagnostics in Colombia, plays a pivotal role in ensuring these processes meet the necessary standards, linking regulatory compliance directly to effective trial management.
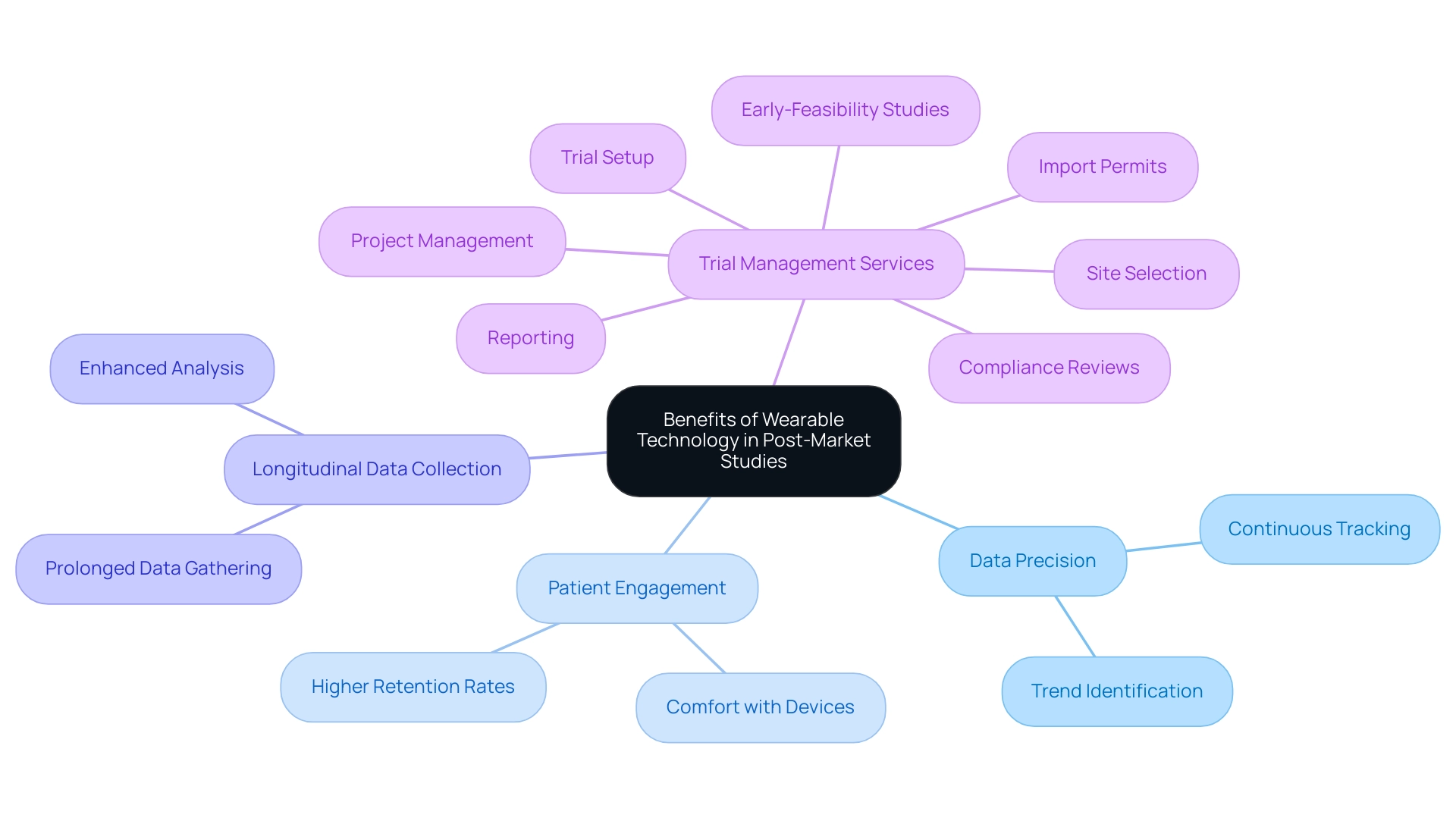
Benefits of Using Wearable Technology in Post-Market Studies
Using wearable technology in post-market studies offers a variety of benefits that greatly improve data precision, patient involvement, and the ability to collect longitudinal data over prolonged durations. With a market share of 7.1% in 2022, companies like Xiaomi exemplify the growing acceptance of wearable technology in health monitoring, especially through using wearable technology in post-market studies, which can be pivotal in clinical trial management. These instruments enable continuous tracking of health metrics, allowing researchers to identify trends and anomalies that may not be apparent through traditional study methodologies.
Furthermore, using wearable technology in post-market studies enhances patient engagement, resulting in higher retention rates as participants are more likely to adhere to study protocols when utilizing devices they are comfortable with. This rise in engagement is vital; as pointed out by Thijs et al., the outcomes of undisclosed algorithms can weaken standardization and analysis, emphasizing the necessity for transparency in handling information. By adopting a data-driven approach, researchers can make better-informed decisions regarding product improvements and patient care strategies.
Additionally, advancements in portable technology, including intelligent feedback systems and interdisciplinary collaboration, promise to enhance user experience and data reliability. Future research should also focus on the usability of these devices in low-resource settings, ensuring that these technologies can be effectively utilized across diverse healthcare environments. Ultimately, as the landscape of healthcare evolves, the potential for devices as effective tools for health management relies on rigorous testing and validation, which highlights the importance of using wearable technology in post-market studies and comprehensive trial management services offered by bioaccess®, including:
- early-feasibility studies
- site selection
- compliance reviews
- trial setup
- import permits
- project management
- reporting
With more than 20 years of experience in Medtech, bioaccess® is prepared to manage the intricacies of trials, ensuring adaptability and specialized knowledge throughout the process.
Challenges and Limitations of Wearable Technology in Clinical Research
While portable technology offers remarkable prospects for advancing clinical research, it simultaneously presents a range of challenges that must be effectively managed. Key among these is the need for interoperability, which is essential to prevent the overestimation of capabilities and enhance personalized healthcare outcomes. Data security continues to be a major concern, as incidents related to technology in studies can compromise participant privacy and trust.
Moreover, the accuracy and reliability of data gathered by devices are variable, underlining the necessity for stringent validation processes. A recent review highlighted that 58.1% of studies reported validation, accuracy, and clinical certification as strengths of affordable devices, showcasing their potential when implemented correctly. However, the review also acknowledges limitations in the scope of included studies, such as the exclusion of non-English publications and smaller companies' devices, which may lead to an incomplete understanding of the field.
Researchers must also be cognizant of the risk of participant fatigue or disengagement caused by continuous monitoring, which could impact study outcomes. To address these challenges, the Critical Path Institute (C-Path) ePro Consortium offers recommendations for devices that can be worn, focusing on safety, suitability for trial objectives, and data validity. Addressing these challenges proactively is critical for maximizing the effectiveness of using wearable technology in post-market studies, ensuring that research yields meaningful and actionable results.
As articulated in expert opinions, this proactive approach can significantly reduce the burden on patients, minimizing their need for extensive visits to clinical settings and lowering associated medical costs.
Conclusion
The integration of wearable technology into healthcare represents a transformative shift in clinical research and patient monitoring. The systematic processes of post-market surveillance ensure that these devices maintain safety and efficacy standards even after they have been approved for public use. Regulatory agencies, such as INVIMA, play a crucial role in monitoring compliance and addressing any emerging issues, thereby reinforcing the importance of ongoing oversight.
Wearable devices facilitate continuous data collection, enhancing the quality of clinical trials and patient monitoring. Their ability to provide real-time feedback allows researchers to gain deeper insights into patient behaviors, improving health interventions and personalizing care. However, challenges such as data privacy, participant engagement, and the accuracy of collected data necessitate a rigorous approach to research design and regulatory compliance.
The benefits of wearable technology in post-market studies are evident, with improved patient engagement and the ability to gather longitudinal data that traditional methodologies may overlook. Nonetheless, researchers must navigate the complexities of interoperability, data security, and the potential for participant fatigue. Proactive measures, including adherence to regulatory guidelines and the implementation of comprehensive trial management services, are essential for maximizing the effectiveness of wearables in clinical settings.
As the market for wearable health devices continues to expand, understanding their implications for clinical research becomes increasingly vital. Stakeholders are called to embrace the potential of these technologies while remaining vigilant about the challenges they present. By doing so, they can harness the full spectrum of benefits that wearable technology offers, ultimately leading to enhanced patient outcomes and more efficient healthcare delivery.
Frequently Asked Questions
What is post-market surveillance (PMS)?
Post-market surveillance (PMS) refers to the systematic processes aimed at monitoring the safety and efficacy of medical products after they receive approval for public use, particularly using wearable technology in post-market studies.
Why is PMS critical for medical products?
PMS is critical as it helps identify potential issues that may arise once products are in consumer hands, ensuring ongoing compliance with safety standards mandated by regulatory agencies like INVIMA.
What role does INVIMA play in post-market surveillance?
INVIMA, Colombia's National Food and Drug Surveillance Institute, is responsible for evaluating medical device applications, conducting inspections, and enforcing compliance with established regulations and safety standards.
How does wearable technology contribute to post-market studies?
Wearable technology facilitates continuous data collection and real-time feedback from participants, monitoring various health metrics and enhancing the overall quality of clinical studies.
What percentage of authors acknowledge the accuracy and reliability of wearable devices in research?
Recent analyses indicate that 58.1% of authors recognize the accuracy and reliability of wearable devices as critical to their effectiveness in research settings.
What recent study highlights the use of electronic health records in surveillance systems?
A notable study led by Nigam H Shah emphasizes the feasibility and efficacy of an electronic health record (EHR)-based surveillance system for consumer devices, particularly for pre-diagnosing atrial fibrillation.
What are some challenges associated with using wearable technology in post-market studies?
Challenges include identifying all relevant studies, especially those from smaller companies or non-English publications, and navigating information privacy concerns due to stringent regulations.
How does the market for health and fitness devices relate to post-market surveillance?
The health and Fitbit device market is expected to reach USD 75 billion by 2026, highlighting the increasing significance of these technologies and the need for strong PMS protocols for their ongoing evaluation.
How can partnerships enhance post-market surveillance processes?
Collaborating with experienced partners like bioaccess®, which has over 20 years of expertise in managing research studies, can significantly improve the evaluation and regulatory processes for medical devices in Latin America.
What guidelines have the FDA established regarding digital health technologies?
The FDA has established guidelines addressing validation and data privacy concerns for using digital health technologies in clinical research, which are crucial for maintaining participant trust and data integrity.




