Introduction
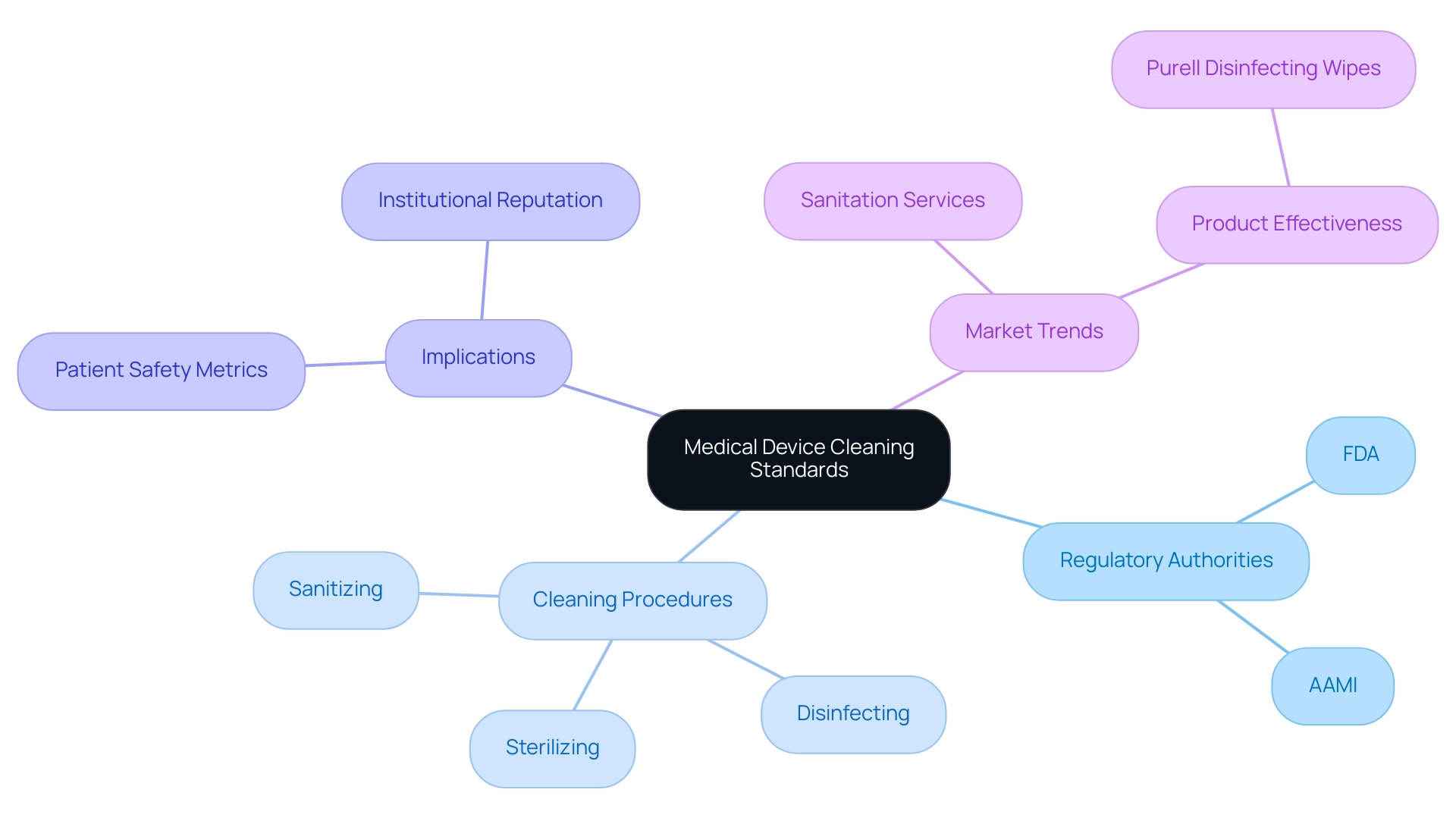
In the realm of healthcare, the cleanliness of medical devices is paramount, serving as a critical line of defense against infections and ensuring patient safety. As regulatory bodies like the FDA and AAMI establish stringent cleaning standards, healthcare providers are tasked with navigating a complex landscape of compliance and best practices.
This article delves into the essential cleaning protocols, highlighting the importance of adherence to established guidelines and the role of innovative technologies in enhancing cleaning efficacy. By understanding the intricacies of medical device cleaning, professionals can foster safer healthcare environments, ultimately improving patient outcomes and maintaining the integrity of healthcare institutions.
Understanding Medical Device Cleaning Standards: Compliance and Safety Essentials
Cleaning criteria for medical instruments are vital for protecting patient safety by guaranteeing that tools are free from harmful contaminants. Regulatory authorities, particularly the FDA, create extensive guidelines that outline the medical device cleaning standards for sanitizing, disinfecting, and sterilizing medical devices. Compliance with these established guidelines is essential not only for patient safety but also for preserving the operational integrity of medical facilities.
Among the key criteria are those specified by the Association for the Advancement of Medical Instrumentation (AAMI) and ISO guidelines, which detail complex protocols for medical device cleaning standards. According to current statistics for 2024, adherence to these criteria has demonstrated a significant enhancement in patient safety metrics, fostering trust in medical practices. Medical practitioners must understand the intricacies of these guidelines, as they directly impact sanitation and upkeep processes, ultimately influencing patient results and the reputation of medical institutions.
For instance, Gojo Industries, Inc. emphasizes the effectiveness of Purell surface disinfecting wipes, which can eliminate numerous pathogens and viruses with a single swipe, making them a convenient solution for high-touch surfaces in medical facilities. Furthermore, insights from the 'Services to Buildings And Dwellings Global Market Report 2025' illustrate market trends and the significance of sanitation services in the healthcare industry, further underscoring the importance of rigorous compliance with hygiene standards.
Best Practices for Effective Cleaning and Disinfection of Medical Devices
Effective cleaning and disinfection of medical instruments necessitate well-defined procedures that comply with medical device cleaning standards and should be consistently implemented. A crucial first step is to classify items according to their risk levels: critical, semi-critical, and non-critical. For essential instruments, which come into direct contact with sterile tissues, steam sterilization or ethylene oxide gas are recommended to ensure complete microbial eradication.
Semi-critical instruments, which contact mucous membranes, require high-level disinfection methods. Non-critical devices, typically used in less invasive applications, can often be adequately cleaned using low-level disinfectants. It is essential that all sanitizing agents and methods meet medical device cleaning standards and undergo rigorous validation to confirm their efficacy in eliminating contaminants.
Regular training sessions and audits are essential to ensure adherence to medical device cleaning standards, allowing for timely updates as needed. Establishing a regular upkeep and maintenance schedule is vital for ensuring that all devices are consistently prepared for safe patient use. As emphasized by recent statistics, there was an 8.4% rise in cataract surgical procedures in the Czech Republic, underscoring the increasing need for effective sanitation and disinfection in the medical field.
Moreover, as observed by P&S Intelligence, the region's expansion indicates improvements in medical practices and an increasing consciousness of infection prevention strategies. Furthermore, medical establishments perform microbial testing on equipment after sanitization to confirm that sanitation procedures comply with medical device cleaning standards, which is particularly vital in delicate areas like surgical rooms to guarantee patient safety.
Navigating Regulatory Requirements for Medical Device Cleaning
Navigating the regulatory requirements for medical device cleaning standards is a complex yet essential task for manufacturers and healthcare providers. The FDA and AAMI are pivotal in establishing comprehensive guidelines, particularly the medical device cleaning standards, that must be adhered to. Specifically, the FDA mandates that manufacturers provide detailed instructions for sanitation and sterilization in their product labeling, ensuring that end-users are adequately informed.
Simultaneously, AAMI provides specific suggestions for sanitation procedures focused on removing pollutants and improving equipment safety. Significantly, the Diagnostic Centers division is projected to exhibit the quickest CAGR, propelled by the necessity for rigorous sanitation protocols for semi-critical and critical equipment. As the medical device sanitation market is projected to grow at an impressive CAGR of 17.60% from 2024 to 2032, adhering to medical device cleaning standards is essential for compliance and operational efficacy.
Facilities should prioritize regular reviews and updates of their sanitation practices to align with evolving medical device cleaning standards, thereby mitigating risks of costly penalties while simultaneously bolstering patient safety. As highlighted by Trishita Deb, a market research analyst with considerable experience in healthcare, adapting to regulatory mandates is not just a compliance matter; it is essential for upholding high levels of care in clinical settings. Furthermore, the FDA’s Sterilization Master File Program exemplifies an effective strategy for manufacturers to streamline compliance by referencing established master files for various sterilization methods, including ethylene oxide (EtO) sterilization.
This initiative not only simplifies regulatory requirements but also ensures that disinfection efficacy is upheld for approved sterilization techniques, thereby enhancing patient safety. Furthermore, with the disinfection sector expected to lead and be the quickest-expanding segment in the medical apparatus sanitation market in 2024, fueled by the rising occurrence of infections, adherence to these changing guidelines becomes even more essential. Experts like Ana Criado, who has extensive experience in Regulatory Affairs and has contributed to shaping sanitization and sterilization standards, play a vital role in ensuring adherence across the industry.
Her background in biomedical engineering and health economics further informs her understanding of the regulatory landscape, making her insights invaluable for manufacturers navigating these complex requirements.
The Importance of Cleaning Validation in Medical Device Safety
Validation of sanitation constitutes a critical systematic approach to verifying the effectiveness of methods utilized in compliance with medical device cleaning standards. This process requires the establishment of a comprehensive sanitation validation protocol, which encompasses:
- Risk assessments
- Sampling techniques
- Analytical testing
For instance, swab sampling is a widely adopted method for detecting residues after sanitation, providing assurance that the sanitation process meets stringent effectiveness standards.
The importance of thorough validation cannot be overstated; it is essential not only in ensuring compliance with medical device cleaning standards and rigorous regulatory demands but also in safeguarding patient safety by reducing the risks of infection or device malfunction due to inadequate hygiene practices. Recent statistics indicate that the reduction in sampling and optimized use of equipment has yielded higher productivity, allowing more batches to be produced within the same timeframe. This highlights the efficiency gains that can be achieved through effective sanitation validation protocols.
The Covid-19 pandemic has transformed market dynamics, highlighting the necessity for strong validation processes in pharmaceutical production. In light of this, maintaining an efficient workspace despite growing staff numbers is crucial. As industry leaders suggest,
- 'Use flexible workspaces'
- 'Vertical storage'
- 'Multipurpose furniture'
to enhance operational efficiency.
Regular re-validation is essential to adapt to any alterations in sanitation methodologies or products, ensuring ongoing compliance with medical device cleaning standards and safety. This proactive strategy for validation is essential as North America continues to lead the pharmaceutical validation market, driven by stringent FDA and Health Canada regulations that shape industry standards for 2024 and beyond.

Innovations and Future Directions in Medical Device Cleaning Practices
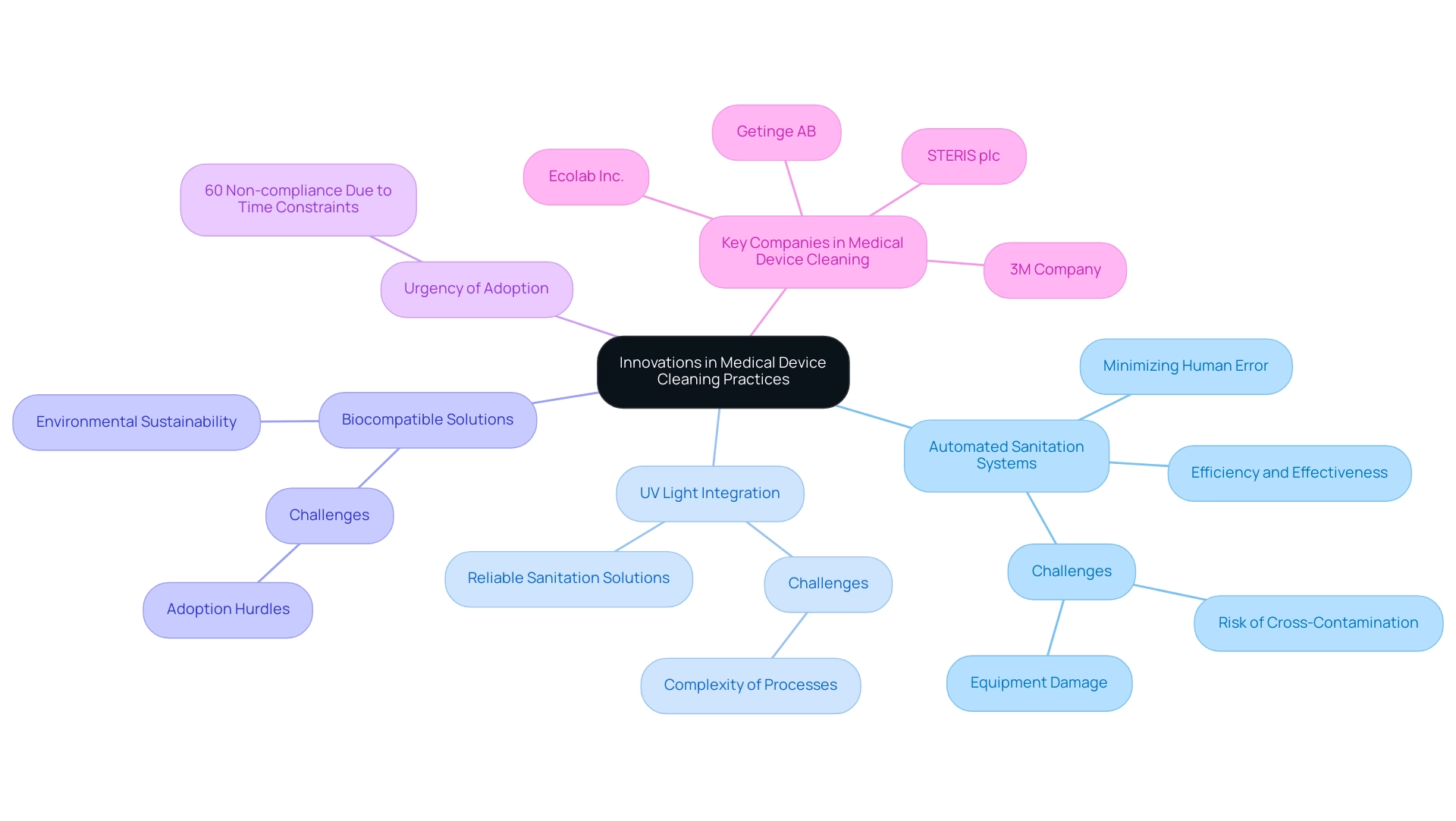
As the medical sector progresses, so do the methods and technologies that comply with medical device cleaning standards for sanitizing medical devices. Automated sanitation systems are increasingly being adopted in healthcare environments, enhancing both efficiency and effectiveness while minimizing the potential for human error during maintenance processes. However, the complexity of these sanitation processes presents significant challenges, particularly the risk of cross-contamination and equipment damage, which can hinder the adoption of new sanitation technologies.
Innovations such as the integration of ultraviolet (UV) light for disinfection exemplify the shift towards more reliable sanitation solutions. Additionally, the emergence of biocompatible solutions that are effective and environmentally sustainable is gaining momentum. According to Trishita Deb, a market research analyst with extensive experience in the medical field, continuous innovation in sanitation technologies is essential for maintaining compliance with medical device cleaning standards and ensuring patient safety.
Given that 60% of reported non-compliance with cleaning protocols arises from time constraints, the urgency for medical facilities to adopt these advancements cannot be overstated. Companies like 3M Company and STERIS plc are at the forefront of this innovation, leveraging their expertise to address these challenges and drive market growth. By embracing such innovations, healthcare providers can enhance patient outcomes while significantly improving operational efficiency and ensuring compliance with medical device cleaning standards.
Conclusion
The significance of maintaining rigorous cleaning standards for medical devices cannot be overstated, as it serves as a fundamental pillar of patient safety and operational integrity within healthcare settings. This article has explored the essential cleaning protocols established by regulatory authorities such as the FDA and AAMI, emphasizing the necessity of compliance with these guidelines to mitigate risks associated with infections and device malfunctions. Understanding the classification of medical devices and the corresponding cleaning methods is crucial for healthcare professionals striving to uphold the highest safety standards.
Moreover, the importance of cleaning validation has been highlighted as a systematic approach to ensuring that cleaning methods are effective and compliant with regulatory demands. The integration of innovative technologies, such as automated cleaning systems and environmentally sustainable cleaning agents, presents exciting opportunities for enhancing cleaning efficacy while minimizing human error. As the healthcare landscape continues to evolve, staying informed about advancements in cleaning practices will be vital for professionals aiming to protect patient health and maintain the credibility of healthcare institutions.
In conclusion, fostering a culture of rigorous adherence to cleaning standards and embracing innovative solutions will not only improve patient outcomes but also enhance the overall quality of care provided in healthcare facilities. By prioritizing compliance and investing in effective cleaning technologies, healthcare professionals can ensure a safer environment for patients, thereby reinforcing the trust placed in healthcare systems.
Frequently Asked Questions
Why are cleaning criteria for medical instruments important?
Cleaning criteria are vital for protecting patient safety by ensuring that medical tools are free from harmful contaminants.
Who establishes the guidelines for medical device cleaning standards?
Regulatory authorities, particularly the FDA, create extensive guidelines that outline the standards for sanitizing, disinfecting, and sterilizing medical devices.
What organizations provide key criteria for medical device cleaning?
The Association for the Advancement of Medical Instrumentation (AAMI) and ISO guidelines provide crucial criteria that detail complex protocols for cleaning medical devices.
What impact does adherence to cleaning standards have on patient safety?
Compliance with cleaning standards has demonstrated a significant enhancement in patient safety metrics, fostering trust in medical practices.
How should medical instruments be classified for cleaning purposes?
Medical instruments should be classified according to their risk levels: critical, semi-critical, and non-critical.
What cleaning methods are recommended for critical instruments?
Critical instruments, which come into direct contact with sterile tissues, should undergo steam sterilization or ethylene oxide gas treatment to ensure complete microbial eradication.
What disinfection methods are required for semi-critical instruments?
Semi-critical instruments, which contact mucous membranes, require high-level disinfection methods.
How should non-critical devices be cleaned?
Non-critical devices, used in less invasive applications, can often be cleaned adequately using low-level disinfectants.
What is necessary to ensure the efficacy of sanitizing agents and methods?
All sanitizing agents and methods must meet medical device cleaning standards and undergo rigorous validation to confirm their effectiveness in eliminating contaminants.
Why is regular training and audits important in medical cleaning procedures?
Regular training sessions and audits are essential to ensure adherence to cleaning standards and allow for timely updates as needed.
What is the significance of microbial testing in medical establishments?
Medical establishments perform microbial testing on equipment after sanitization to confirm that sanitation procedures comply with cleaning standards, especially in sensitive areas like surgical rooms, to guarantee patient safety.




