Introduction
In the intricate landscape of medical device development, adherence to compliance standards is paramount for ensuring safety and efficacy. A multitude of frameworks, including ISO 13485 and ISO 14971, guide manufacturers in establishing robust quality management systems and effective risk management strategies.
As the industry evolves, the integration of comprehensive testing and post-market surveillance practices becomes essential for navigating regulatory complexities and enhancing patient outcomes. This article delves into the critical aspects of compliance, validation, risk management, and testing, underscoring the importance of a meticulous approach to medical device safety in a rapidly advancing technological environment.
Through insights from industry experts and case studies, it aims to equip stakeholders with the knowledge necessary to thrive in this dynamic field.
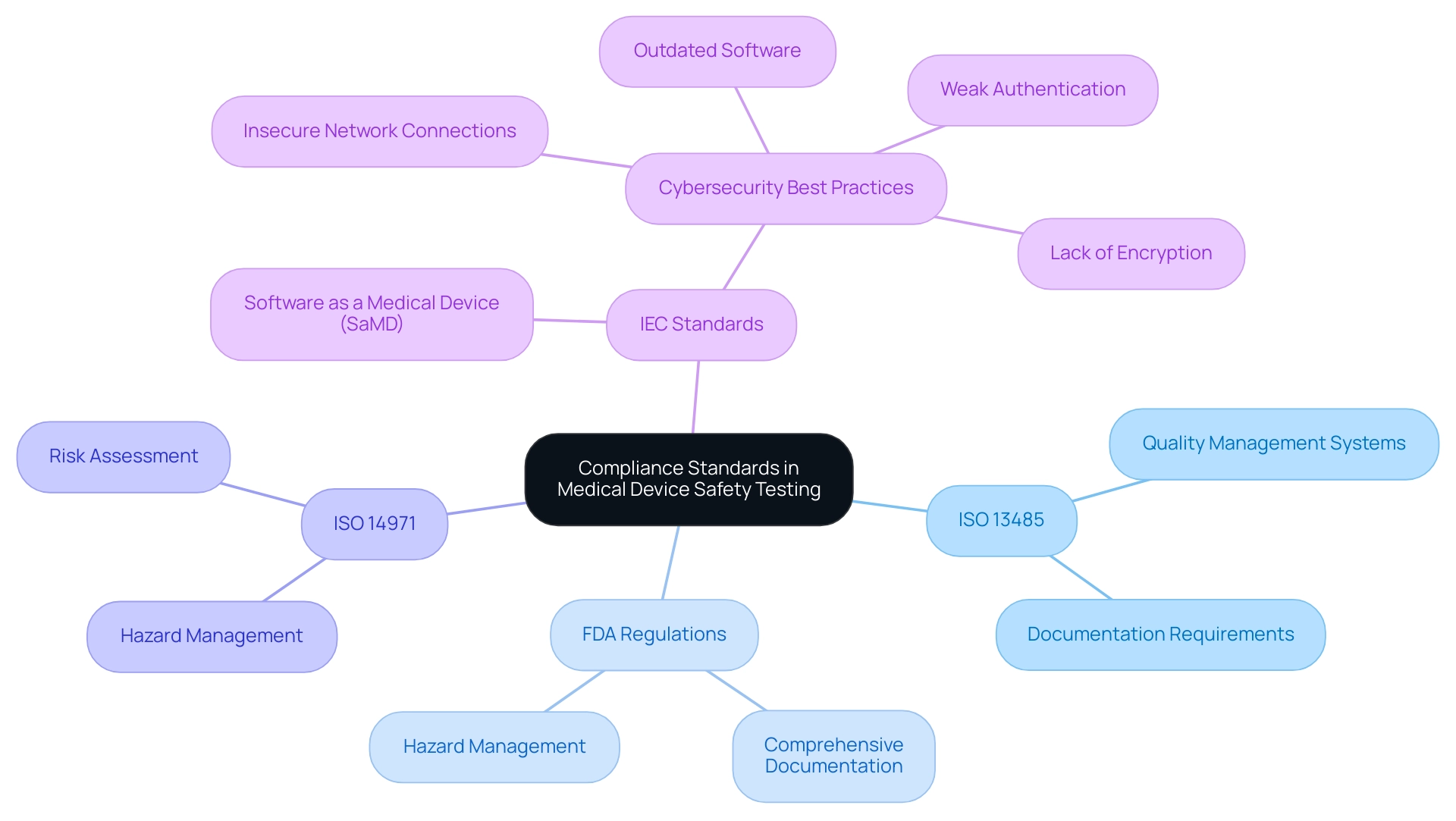
Understanding Compliance Standards in Medical Device Safety Testing
The safety evaluation of healthcare instruments involves medical device safety testing, which is directed by a strong set of compliance standards intended to guarantee that products fulfill stringent safety and effectiveness criteria. Among these, ISO 13485 stands out as a pivotal standard that delineates the requirements for quality management systems specific to medical equipment. In the United States, manufacturers must also comply with the FDA’s regulations for approval, which require comprehensive documentation throughout the design, development, and testing phases.
The FDA stresses that producers must remain vigilant in recognizing and tackling hazards related to their products, making hazard management a vital component of this process. Adherence to ISO 14971, which stresses hazard management, is essential for recognizing and alleviating potential dangers linked to healthcare equipment. By systematically addressing these risks, manufacturers can significantly bolster the reliability of their products while ensuring compliance with stringent regulatory expectations.
Experts like Ana Criado, Director of Regulatory Affairs and CEO of Mahu Pharma, who has over five years of experience in executive roles at Colombia’s regulatory agency —INVIMA—, alongside Katherine Ruiz, who specializes in Regulatory Affairs for Medical Devices and In Vitro Diagnostics in Colombia, underscore the importance of understanding these standards. Ana's extensive background as a biomedical engineering professor at top Colombian universities and her consulting experience with global companies further solidify her authority in this field. As Eric Henry mentioned in a recent discussion, 'the evolving landscape of AI in MedTech centers on regulatory compliance and the future of AI in healthcare tools,' highlighting the significance of remaining up-to-date with compliance standards.
Moreover, compliance with IEC standards is becoming more crucial, especially in the realm of software as a healthcare solution (Sand), to ensure safety and efficacy in the changing environment of health technology. A case study on cybersecurity considerations in healthcare software highlights the necessity of adopting best practices to safeguard against vulnerabilities such as insecure network connections and outdated software. Comprehending and applying these compliance standards is not just beneficial; it is crucial for successfully maneuvering through the intricacies of medical device safety testing in today's regulatory landscape.
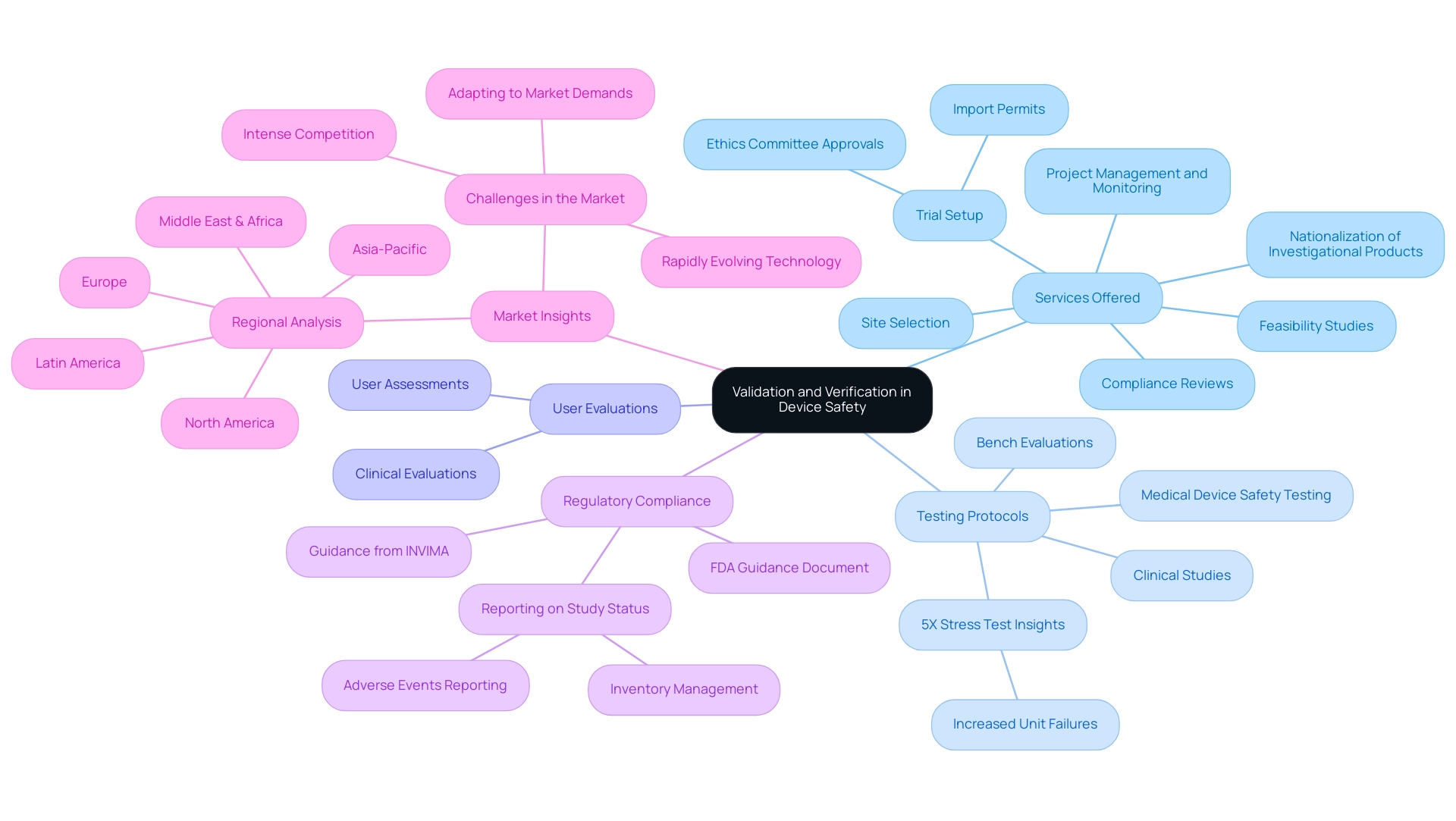
The Role of Validation and Verification in Ensuring Device Safety
Validation and verification are essential elements of medical device safety testing, ensuring that the medical equipment development process results in products that not only adhere to design specifications but also function effectively within their intended environments. In a market characterized by intense competition and rapidly evolving technology, a comprehensive validation and verification framework is essential. Our service capabilities support this framework by offering:
- Feasibility studies
- Site selection
- Compliance reviews
- Trial setup—including ethics committee approvals and import permits
- Nationalization of investigational products
We also provide project management and monitoring, ensuring that all aspects of the trial are efficiently coordinated. Validation emphasizes verifying that the apparatus satisfies the requirements of end users and intended applications, which generally includes user assessments and clinical evaluations. For example, a strong user evaluation process offers essential insights into user interactions, thus improving the usability and safety of the product.
Verification guarantees that the apparatus was constructed in accordance with its design specifications through stringent assessment protocols, such as:
- Medical device safety testing
- Bench evaluations
- Clinical studies that validate the apparatus's performance and safety metrics
A recent analysis revealed that a 5X stress test results in five times as many unit failures compared to normal usage conditions, underscoring the necessity for thorough testing. Producers must apply this extensive framework across the product lifecycle to reduce uncertainties and guarantee adherence to changing regulatory standards, including guidance from agencies like INVIMA—the Colombian National Food and Drug Surveillance Institute, which supervises medical device safety testing as a Level 4 health authority by PAHO/WHO.
As Dr. Taylor aptly states,
Passing a variables sampling plan allows a Confidence/Reliability statement to be made.
Moreover, understanding regional differences, as highlighted in the case study titled 'Regional Analysis of Medical Device Validation and Verification Market,' is crucial for effectively targeting and growing within specific market segments. By adopting these practices, organizations can create safer products that improve patient outcomes while navigating the challenges of the healthcare equipment market.
Reporting on study status, inventory, and serious and non-serious adverse events is also essential for maintaining compliance and transparency throughout the clinical trial process.
Implementing Risk Management Strategies
Establishing efficient management strategies is essential for the creation of safe and compliant medical products, which involves medical device safety testing. According to ISO 14971, manufacturers must establish a comprehensive management process that encompasses analysis, evaluation, and control measures. This protocol involves identifying potential hazards linked to a device and assessing their implications for patient safety.
One effective method in this process is the Failure Mode and Effects Analysis (FMEA), which allows teams to prioritize threats based on their severity and likelihood, thereby enabling targeted mitigation strategies. Furthermore, continuous threat monitoring post-market is essential for adapting to new data and ensuring sustained compliance. As emphasized in the case study on the in-vitro diagnostics market, which was valued at $91.2 billion in 2022 and is projected to grow to $118 billion by 2030, with a CAGR of 3.2%, the focus on thorough management of uncertainties becomes even more relevant.
John Myklusch, Chief Financial Officer and experienced Exit Planner with over 20 years of expertise, highlights the significance of incorporating financial hazard management into the wider management strategies for healthcare product manufacturers. His expertise in mergers and acquisitions and financial controls underscores the necessity for manufacturers to adopt effective risk management strategies to navigate the evolving landscape successfully. Katherine Ruiz, a specialist in regulatory matters for medical instruments and in vitro diagnostics in Colombia, emphasizes the significance of following thorough evaluation standards, including endotoxin, performance, and usability assessments.
These testing methods are essential for medical device safety testing to ensure that equipment meets regulatory requirements while also operating safely and effectively for patients. Furthermore, Trishita Deb, a specialist in healthcare who has written more than 400 reports, highlights that the incorporation of management training is essential for staff engaged in the process. Such training not only provides teams with the essential skills to recognize and reduce hazards effectively but also emphasizes the significance of a strategic focus on management in healthcare product development.
By adopting a holistic risk management approach, organizations not only enhance safety but also foster trust with stakeholders and regulatory bodies, positioning themselves favorably in this dynamic landscape.

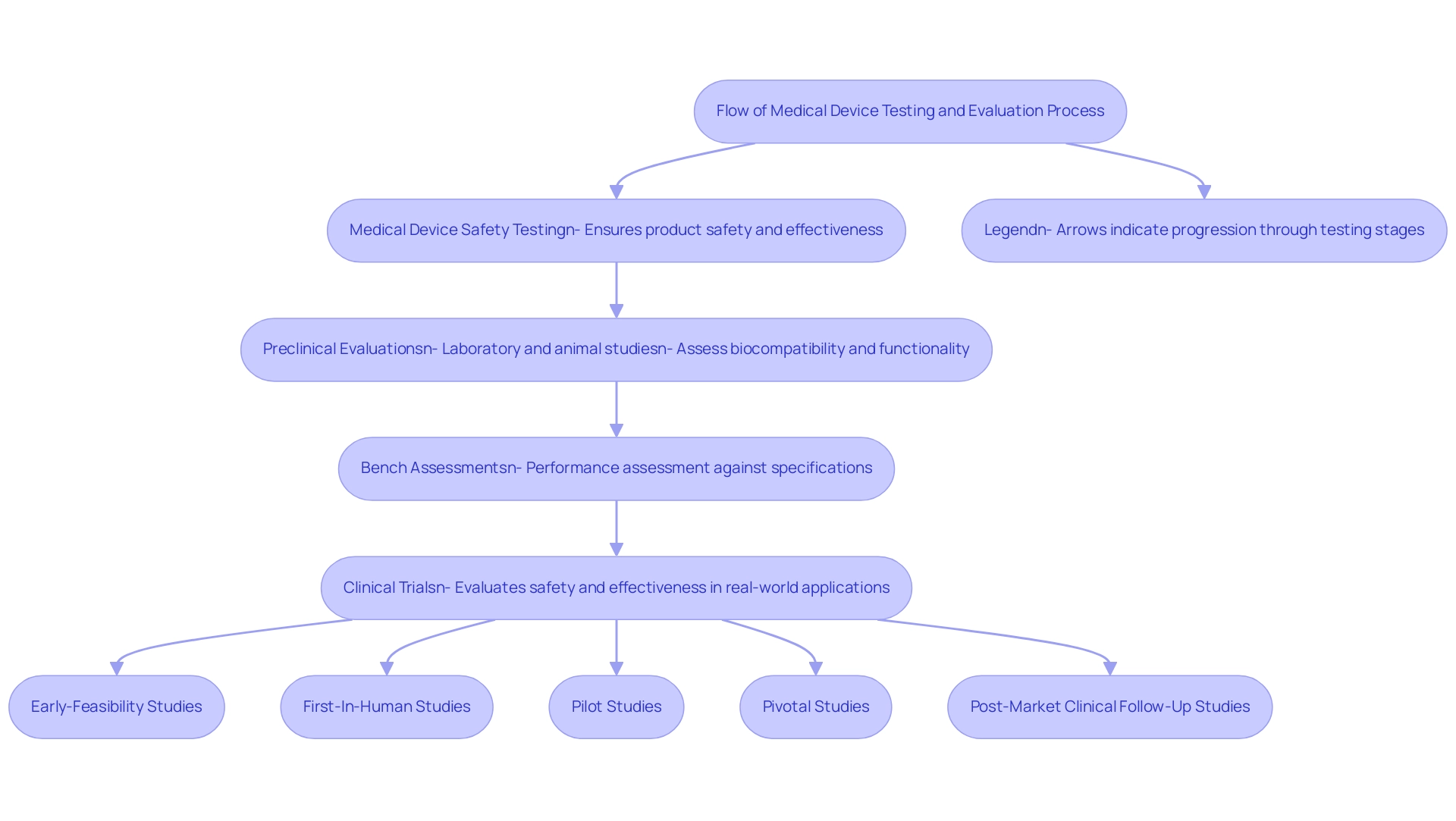
Conducting Comprehensive Testing and Evaluation
Carrying out thorough assessment and evaluation is crucial in the medical device safety testing and development process. Producers are urged to adopt a multi-dimensional strategy that includes:
- Medical device safety testing
- Preclinical evaluations
- Bench assessments
- Clinical trials
to guarantee product safety and effectiveness. Preclinical evaluation encompasses laboratory and animal studies aimed at assessing biocompatibility and functionality, providing foundational data before moving forward.
Following this, bench testing assesses the performance of the equipment against established specifications, ensuring it meets operational requirements. Clinical trials, overseen by specialists such as bioaccess®, involve human subjects to evaluate the system's safety and effectiveness in real-world applications. With over 20 years of Medtech experience, bioaccess® specializes in conducting:
- Early-Feasibility Studies
- First-In-Human Studies
- Pilot Studies
- Pivotal Studies
- Post-Market Clinical Follow-Up Studies
across Latin America, ensuring compliance with established protocols and guidelines such as those outlined by the FDA and ISO.
Their flexibility and specialized knowledge allow them to adapt to the unique challenges of each trial, which is crucial for success. This not only generates robust evidence to support device submissions but also builds trust among healthcare providers and patients. For instance, plugging 2 in for the RQL results in n = 5.9212, rounded up to n = 6 years, highlighting the importance of statistical rigor in evaluation methodologies employed by bioaccess®.
Moreover, extra resources like guides and courses on validation sampling plans and acceptance sampling are accessible, strengthening the industry's dedication to thorough evaluation methods. This comprehensive evaluation procedure, which includes medical device safety testing, is essential for regulatory approval and instrumental in promoting trust in new healthcare technologies. Dr. Wayne A. Taylor emphasizes this sentiment, stating, '> This book is designed for engineers and scientists in the healthcare industry <,' underscoring the necessity of a rigorous framework for medical device safety testing to advance safe and effective solutions.
Furthermore, bioaccess® offers the knowledge and tailored method required to guide your firm towards acquisition, guaranteeing a strategic route ahead in the competitive healthcare equipment environment.
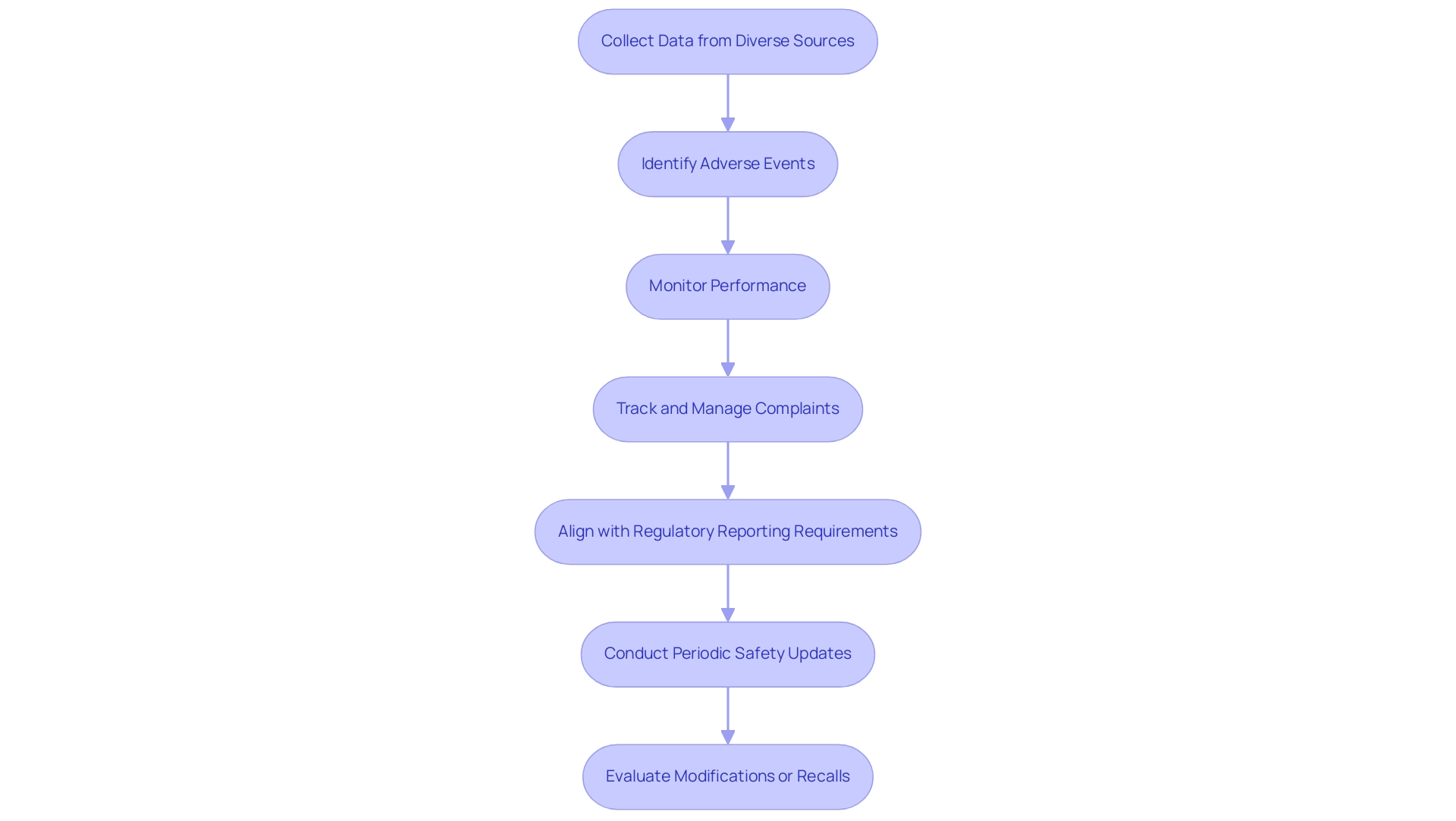
Establishing Post-Market Surveillance Practices
Establishing comprehensive post-market surveillance (PMS) practices is vital for ensuring the ongoing safety and effectiveness of medical instruments, which includes medical device safety testing. Manufacturers are mandated to monitor performance following market entry, which involves identifying adverse events and potential product failures. This monitoring is facilitated through the collection of data from diverse sources, including user feedback, clinical registries, and reports from healthcare professionals.
An effective system for tracking and managing complaints not only enables manufacturers to respond swiftly to safety concerns but also aligns with regulatory reporting requirements outlined in 21 CFR Part 806, which emphasizes the significance of reporting corrections and removals. Furthermore, periodic safety updates and risk assessments are essential for evaluating whether modifications or recalls are warranted. By adopting a proactive stance on PMS, organizations can substantially enhance patient safety and fulfill regulatory obligations through medical device safety testing, promoting the long-term success of their healthcare products.
As highlighted by the FDA, adherence to regulations related to medical device safety testing is crucial for manufacturers of healthcare products to show their dedication to patient safety and fulfill continuous performance monitoring obligations. This commitment is evident in the increasing emphasis on adverse event reporting, with the Government Accountability Office (GAO) emphasizing recent conversations with FDA officials and healthcare stakeholders about best practices in monitoring safety. Specific statistics from the GAO review indicate that adverse event reporting rates have seen a significant increase, underscoring the importance of robust practices in medical device safety testing.
In Colombia, INVIMA plays a critical role in this landscape as a Level 4 national regulatory authority, overseeing health products through its Directorate for Medical Items and Other Technologies, which is responsible for monitoring compliance with established safety and quality standards, suggesting technical standards, and tracking pre- and post-market programs. INVIMA was founded in 1992 under Colombia's Ministry of Health and Social Protection, and its supervision is crucial for ensuring that health products meet safety and efficacy standards. Insights from industry leaders, including Pedro Sancha, highlight the need for a forward-thinking approach in public health and the TIC sector, emphasizing that a robust PMS system not only prioritizes patient safety but also fosters innovation through medical device safety testing, ensuring that medical devices can thrive in a competitive healthcare landscape.
Conclusion
In the realm of medical device development, adherence to compliance standards is not just a regulatory necessity; it is the foundation of patient safety and product efficacy. The importance of frameworks such as ISO 13485 and ISO 14971 cannot be overstated, as they provide critical guidelines for establishing quality management systems and effective risk management strategies. By systematically addressing risks and ensuring compliance with stringent regulations, manufacturers can enhance the reliability of their devices, ultimately safeguarding patient outcomes.
Moreover, the integration of robust validation and verification processes, coupled with comprehensive testing and evaluation, ensures that medical devices perform as intended across various environments. This meticulous approach not only fulfills regulatory requirements but also builds trust among healthcare providers and patients alike. Continuous risk management and post-market surveillance practices further reinforce the commitment to safety, allowing for the identification of potential hazards and swift responses to adverse events.
As the medical device landscape evolves, embracing these compliance standards and best practices is essential. Organizations that prioritize a proactive stance on compliance and risk management will not only navigate the complexities of regulatory frameworks more effectively but also contribute to the advancement of safe and innovative healthcare solutions. In doing so, they will position themselves favorably in a dynamic market, ultimately enhancing the quality of care delivered to patients.
Frequently Asked Questions
What is the purpose of medical device safety testing?
Medical device safety testing ensures that healthcare instruments meet stringent safety and effectiveness criteria, guided by compliance standards.
What is ISO 13485 and why is it important?
ISO 13485 is a pivotal standard that outlines the requirements for quality management systems specific to medical equipment, ensuring manufacturers maintain high-quality processes.
What are the FDA’s requirements for medical device manufacturers in the United States?
Manufacturers must comply with FDA regulations that require comprehensive documentation throughout the design, development, and testing phases of medical devices.
Why is hazard management critical in medical device safety?
Hazard management is essential for recognizing and addressing potential dangers associated with healthcare equipment, which helps improve product reliability and compliance with regulatory standards.
What is ISO 14971 and how does it relate to hazard management?
ISO 14971 focuses on hazard management, emphasizing the identification and mitigation of risks related to medical devices, which is crucial for ensuring product safety.
Who are some experts in the field of regulatory compliance for medical devices?
Experts include Ana Criado, Director of Regulatory Affairs and CEO of Mahu Pharma, and Katherine Ruiz, who specializes in Regulatory Affairs for Medical Devices and In Vitro Diagnostics in Colombia.
How is compliance with IEC standards becoming more relevant?
Compliance with IEC standards is increasingly important, especially for software as a healthcare solution, to ensure safety and efficacy in the evolving health technology landscape.
What role does validation and verification play in medical device safety testing?
Validation and verification ensure that medical devices meet design specifications and function effectively in their intended environments, thus enhancing safety and usability.
What types of services support the validation and verification framework?
Services include feasibility studies, compliance reviews, trial setup, nationalization of investigational products, and project management.
What is the significance of user evaluations in the validation process?
User evaluations provide critical insights into user interactions, which helps improve the usability and safety of the medical device.
How do producers ensure compliance with changing regulatory standards?
Producers apply a comprehensive validation and verification framework throughout the product lifecycle to reduce uncertainties and adhere to evolving regulations.
Why is it important to understand regional differences in medical device validation and verification?
Understanding regional differences is crucial for effectively targeting and growing within specific market segments, allowing organizations to create safer products that enhance patient outcomes.
What is the importance of reporting during clinical trials?
Reporting on study status, inventory, and adverse events is essential for maintaining compliance and transparency throughout the clinical trial process.

