Introduction
In the realm of healthcare, the reliability and safety of medical devices are paramount, making rigorous testing methods essential before market introduction. As the medical device testing landscape evolves, various methodologies emerge, each with distinct advantages and challenges. From automated testing that enhances efficiency to usability assessments that prioritize user experience, these approaches play a critical role in ensuring devices meet stringent regulatory standards.
With North America leading the charge in this dynamic market, understanding the nuances of these testing methods is crucial for manufacturers aiming to navigate compliance and foster innovation. This article delves into the multifaceted world of medical device testing, exploring key methodologies, regulatory frameworks, and real-world applications that underscore the importance of thorough evaluations in advancing healthcare technology.
Overview of Medical Device Testing Methods
Medical equipment evaluation is a multifaceted process designed to assess the safety, efficacy, and quality of instruments prior to their market introduction. In 2024, North America emerged as the largest area in the medical equipment evaluation market, reflecting the essential nature of these assessments. Key evaluation methods include:
- Automated testing methods for medical devices leverage advanced software and hardware solutions to conduct tests with minimal human intervention, significantly enhancing both efficiency and accuracy. Recent advancements in automated testing have transformed how products are evaluated, allowing for rapid analysis and improved data reliability. Functional testing is one of the medical device testing methods that assesses whether an apparatus operates as intended under various conditions, ensuring that it meets established performance standards. It is essential for verifying that equipment operates correctly in real-world scenarios.
- Compliance Verification: Rigorous checks using medical device testing methods against regulatory standards are essential to verify that products adhere to safety and efficacy regulations. This verification is not only a legal requirement but also fosters trust among healthcare professionals and patients.
- Usability Testing: Concentrated on user experience, this approach evaluates how easily healthcare professionals and patients can engage with the medical device testing methods. Ensuring intuitive design and safety in usability can significantly influence the product's success in the market.
- Medical device testing methods include conducting clinical trials that involve testing the apparatus in a controlled environment with real patients, gathering vital data on performance and safety. The results of clinical trials are crucial in assessing a product's preparedness for extensive application. Furthermore, expedited healthcare product clinical study services, like those offered by bioaccess®, improve the effectiveness of these assessments in Latin America. With over 20 years of experience in Medtech, bioaccess® specializes in managing a range of studies, including Early-Feasibility Studies (EFS), First-In-Human Studies (FIH), Pilot Studies, Pivotal Studies, and Post-Market Clinical Follow-Up Studies (PMCF). Their tailored strategy guarantees thorough management and regulatory adherence throughout the evaluation process, directing companies toward successful acquisitions.
The supervision offered by INVIMA, Colombia's National Food and Drug Surveillance Institute, is essential as it is classified as a Level 4 health authority by PAHO/WHO, ensuring that health instruments meet rigorous safety and efficacy standards.
These medical device testing methods are often utilized together to provide a comprehensive appraisal of a health instrument's suitability for market introduction, contributing to local economies through job creation and advancements in healthcare. Significantly, firms such as Intertek Group, SGS, Bureau Veritas, and UL Solutions hold crucial positions in this market, ensuring that new products comply with strict evaluation standards. In the final quarter alone, the healthcare equipment sector launched 68 new products, featuring Johnson & Johnson's groundbreaking VELYS™ Robotic-Assisted Solution, emphasizing the continuous progress in health technology.
As Trishita Deb, a Market Research and Consulting Expert, points out, "The development of evaluation methods is vital for preserving the integrity of healthcare tools in a swiftly evolving environment." Furthermore, the purchase of MycoScience Inc. by Millstone Medical Outsourcing LLC in November 2022 illustrates strategic expansion focused on improving laboratory and environmental evaluation services, further highlighting the dynamic character of healthcare instrument assessment and its alignment with industry progress.
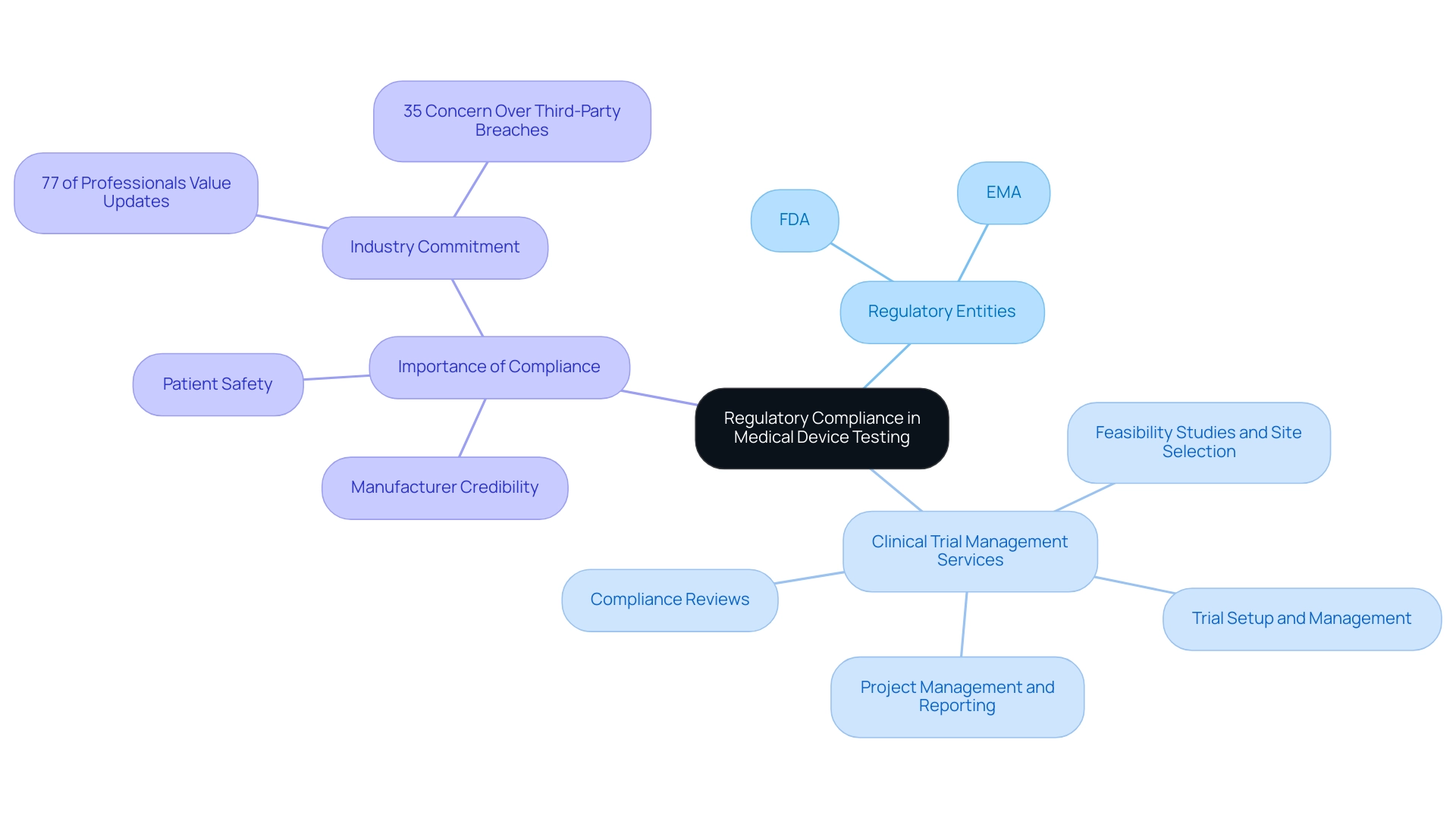
The Role of Regulatory Compliance in Medical Device Testing
Regulatory compliance acts as the foundation of the healthcare equipment evaluation process, ensuring that products conform to established safety and effectiveness standards. Key regulatory entities, including the FDA in the United States and the European Medicines Agency (EMA) in Europe, delineate stringent guidelines that manufacturers must adhere to concerning medical device testing methods in their testing protocols. This compliance framework is further supported by comprehensive clinical trial management services, which include:
- Feasibility Studies and Site Selection: Evaluating research sites and principal investigators (PIs) to ensure optimal trial execution.
- Compliance Reviews: Providing essential feedback on study documents to meet country-specific regulations.
- Trial Setup and Management: Overseeing the trial start-up process, including necessary approvals from ethics committees and health ministries, as well as the importation and nationalization of investigational products.
- Project Management and Reporting: Continuous monitoring of study status, inventory, and serious and non-serious adverse events, ensuring transparency and adherence to regulatory standards.
Adhering to these regulations is not only vital for patient safety but also plays a significant role in enhancing the credibility of manufacturers within the highly competitive healthcare sector. According to recent findings, 77% of corporate risk and compliance professionals find it important or very important to stay updated on the latest developments in these regulatory landscapes. This emphasizes the ongoing commitment required from industry players to remain compliant and trustworthy.
Furthermore, 35% of business and tech executives express concern over third-party breaches, underscoring the critical nature of regulatory compliance in safeguarding patient safety and manufacturer credibility. As mentioned by an FDA representative, 'Regulatory compliance is not merely a requirement; it's a pledge to ensuring the safety and efficacy of healthcare products for patients.
Comparative Analysis of Testing Methods: Pros and Cons
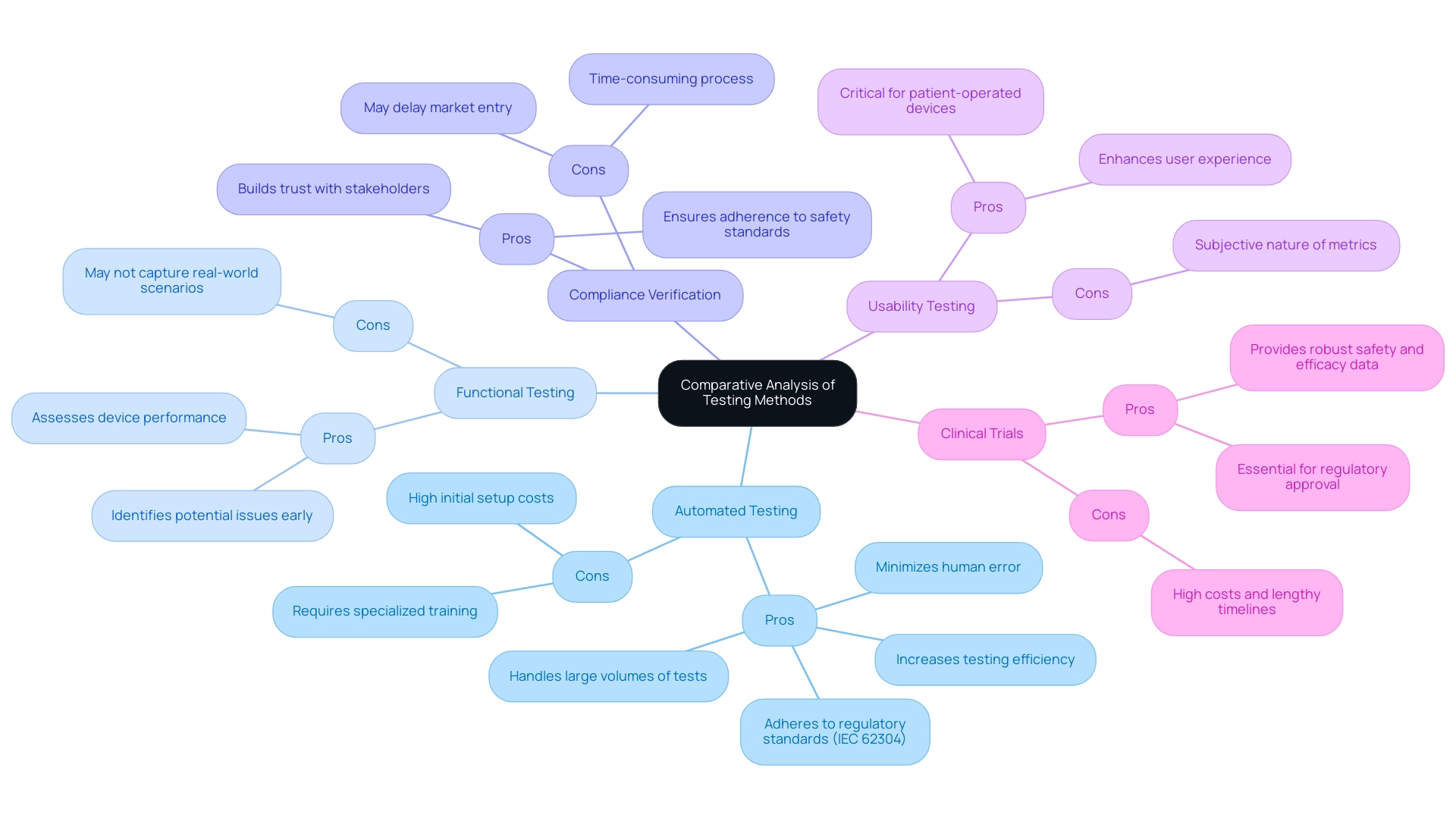
A comprehensive comparative analysis of medical device testing methods unveils distinct advantages and disadvantages that can guide manufacturers in their strategic decisions:
-
Automated Testing:
- Pros: This approach significantly increases testing efficiency, minimizes human error, and is capable of managing large volumes of tests, making it particularly advantageous for high-throughput environments. Medtronic, a prominent medical technology firm, utilizes automated evaluations to ensure the accuracy and reliability of their insulin pumps, reflecting industry best practices. Additionally, adherence to regulatory standards such as IEC 62304 is essential in automated testing, ensuring safety and reliability throughout the software lifecycle.
- Cons: However, the initial setup costs can be substantial, and implementing such systems often requires specialized training, which may pose a barrier for some organizations.
-
Functional Testing:
- Pros: Functional testing directly assesses device performance and is instrumental in identifying potential issues early in the development process, thereby enhancing product reliability. Given the increasing public familiarity with AI-driven surgical robots, this method's role in ensuring effective functionality has become even more critical.
- Cons: Nevertheless, it may not fully capture real-world usage scenarios, potentially leading to gaps in understanding how devices will perform outside of controlled environments.
-
Compliance Verification:
- Pros: Compliance verification ensures adherence to stringent safety standards, which is vital for building trust with stakeholders and regulatory bodies. The case study on regulatory adherence in automated evaluation emphasizes that compliance with standards such as IEC 62304 enhances medical device testing methods by reducing risks and improving the efficiency of medical apparatus.
- Cons: The process can be time-consuming, and navigating compliance requirements may delay market entry, impacting a company's competitive edge.
-
Usability Testing:
- Pros: Usability testing is critical for enhancing user experience, particularly for devices intended for patient use, ensuring that end-users can operate devices effectively. This aspect is increasingly important in a landscape where AI-driven solutions are becoming prevalent.
- Cons: The subjective nature of usability metrics may lead to varying interpretations of results, complicating the assessment of device effectiveness.
-
Clinical Trials:
- Pros: Clinical trials provide robust data on safety and efficacy, which is essential for regulatory approval and instills confidence in healthcare providers and patients alike. With bioaccess®'s expertise in managing Early-Feasibility Studies (EFS), First-In-Human (FIH) trials, and Post-Market Clinical Follow-Up (PMCF) studies, manufacturers can streamline their clinical study processes effectively. With over 20 years of experience in Medtech, bioaccess® brings a wealth of knowledge and a customized approach to address the unique challenges of each clinical trial.
- Cons: However, the high costs and lengthy timelines associated with clinical trials may limit their feasibility for some devices, particularly innovative solutions that require rapid market entry.
Bioaccess®'s adaptable approaches can assist in alleviating these obstacles, offering customized solutions to accelerate the process.
By comprehending these advantages and disadvantages and utilizing the extensive clinical trial management services from bioaccess®, manufacturers can customize their evaluation strategies, particularly through medical device testing methods, to conform with both regulatory standards and market demands, ultimately improving the safety and effectiveness of healthcare products.
Emerging Technologies in Medical Device Testing
Emerging technologies are poised to transform medical device evaluation through innovative medical device testing methods that significantly enhance both efficiency and precision. Among the key advancements are:
- Artificial Intelligence (AI): AI algorithms possess the capability to swiftly analyze vast datasets, uncovering patterns and anomalies that traditional testing methods may overlook. This capability is essential as it allows for more informed decision-making during the evaluation process of medical device testing methods.
- Machine Learning: By utilizing machine learning, evaluation protocols can adapt dynamically based on real-time data inputs. This adaptability not only improves the accuracy of results but also accelerates the time to market for new devices.
- Automated Evaluation Frameworks: These frameworks integrate various assessment methodologies into a unified system, minimizing manual intervention and thereby increasing throughput. This integration supports a more streamlined evaluation process, reducing the likelihood of human error.
- Digital Twins: The creation of virtual replicas of devices allows for predictive evaluation, simulating real-world scenarios without the necessity for physical prototypes. This innovation enhances the ability to foresee potential issues and refine designs prior to production.
The adoption of these technologies is not merely an operational upgrade; it reflects the industry's broader movement towards more efficient and cost-effective medical device testing methods. Notably, only 1.9% of companies have published their post-market outcome data, highlighting the need for more robust reporting mechanisms that these advancements can facilitate. As Dr. Till Myrach states, "Osmometry is a method to determine a sample's osmolality.
This is the total number of osmotically active particles solved in a solution. These particles affect the colligative properties of the solution, which encompass the boiling and freezing point as well as the vapor pressure, highlighting the significance of accurate measurements in medical device testing methods.
Additionally, bioaccess® is dedicated to managing the full spectrum of clinical studies, leveraging over 20 years of experience in Medtech to ensure successful outcomes. This includes Early-Feasibility Studies, First-In-Human Studies, Pilot Studies, Pivotal Studies, and Post-Market Clinical Follow-Up Studies (PMCF). The recent clinical trial launched by Hebrew SeniorLife to investigate the effects of probiotics and prebiotics on bone health in older adults exemplifies innovative evaluation approaches.
This trial aims to provide insights into dietary interventions that could enhance bone density and overall health in the elderly, showcasing the potential of emerging technologies in addressing critical health issues.
As the FDA progressively approves tools utilizing AI and machine learning innovations across different healthcare sectors, the incorporation of these emerging technologies, directed by specialists like Dr. Sergio Alvarado, will be essential in establishing new benchmarks for healthcare apparatus evaluation. Bioaccess®'s specialized knowledge and flexibility in navigating clinical trials further underscore their commitment to advancing the field.
Case Studies: Real-World Applications of Testing Methods
Practical uses of medical device testing methods highlight their essential function in guaranteeing reliability and safety. Recent developments in the field reveal that the research community comprises over 25 million members and produces approximately 160 million publication pages, highlighting the growing interest and advancements in medical device evaluation. Experts foresee a sustained increase in this sector by 17.7% from 2021 to 2028, further highlighting the significance of medical device testing methods in thorough evaluation methodologies.
At bioaccess®, we utilize over 20 years of experience in overseeing various clinical studies, including:
- Early-Feasibility Studies (EFS)
- First-In-Human Studies (FIH)
- Pilot Studies
- Pivotal Studies
- Post-Market Clinical Follow-Up Studies (PMCF)
This ensures that our clients navigate clinical trials with confidence. Our approach not only facilitates efficient evaluation methodologies but also contributes to local economies through job creation and healthcare improvement, highlighting the broader impact of our work.
Core-Lab operates with fewer full-time equivalents (FTE) while processing the same number of assessments compared to pre-Core-Lab, demonstrating significant efficiency in evaluation methodologies.
- Case Study 1: Automated Evaluation in Cardiac Devices: A prominent manufacturer recently adopted automated assessment for their latest cardiac monitor. This strategic shift resulted in a 30% reduction in evaluation time while significantly decreasing human error rates. By leveraging automation, the company expedited its regulatory submission process, leading to a quicker market entry and improved product availability for healthcare providers.
- Case Study 2: Usability Testing for Surgical Instruments: In a focused effort to enhance surgical instruments, a leading company conducted extensive usability tests involving healthcare professionals. Feedback from these sessions facilitated critical design modifications, which not only improved user satisfaction but also reduced procedural errors. This case illustrates how user-centered design can directly impact clinical outcomes and operational efficiencies when applying medical device testing methods.
- Case Study 3: Clinical Trials for Implantable Products: A novel implantable product underwent comprehensive clinical trials that demonstrated its safety and efficacy across a diverse patient population. The thorough evaluation produced valuable information that not only helped in obtaining regulatory approval but also offered insights for future versions of the apparatus. Such findings are crucial in enhancing healthcare instruments to meet evolving clinical needs.
- Case Study 4: Voice-Activated Disease Detection: Vocalis Health has developed a smartphone app that analyzes voice changes to detect diseases, including common colds and COVID-19. This groundbreaking assessment approach assists clinics in recognizing instances that necessitate additional examination or isolation, illustrating how machine learning can improve healthcare diagnostics and patient support.
These case studies collectively emphasize how different medical device testing methods contribute to the effectiveness of healthcare tools. They highlight the necessity of choosing suitable medical device testing methods tailored to the unique challenges of each instrument, ultimately enhancing patient care and safety. Furthermore, Cigniti’s Medical Devices Testing Center of Excellence addresses challenges such as device compatibility, security breaches, and cloud adoption, providing a comprehensive view of the current landscape in medical device testing methods.
Conclusion
Medical device testing is critical for ensuring the safety, efficacy, and quality of healthcare technologies. Various methodologies, including:
- Automated testing
- Functional assessments
- Compliance verification
- Usability evaluations
- Clinical trials
each offer distinct advantages and challenges that manufacturers must navigate within complex regulatory frameworks.
Regulatory compliance is fundamental in this process, fostering trust among stakeholders and ensuring adherence to stringent safety and effectiveness standards set by organizations like the FDA and EMA. This commitment to compliance enhances manufacturers' credibility while safeguarding patient health.
Emerging technologies such as artificial intelligence and machine learning are transforming testing methodologies, providing greater efficiency and precision. These advancements allow manufacturers to accelerate the introduction of innovative solutions, ultimately improving patient outcomes. Real-world applications of these testing methods further demonstrate their vital role in enhancing device reliability and safety.
In summary, the evolution of medical device testing underscores the necessity of rigorous evaluation methods in advancing healthcare technology. By adopting innovative strategies and maintaining regulatory compliance, manufacturers can ensure their devices meet market demands while prioritizing patient safety. As the industry continues to evolve, a steadfast commitment to comprehensive testing will remain essential for fostering innovation and upholding the integrity of medical devices.
Frequently Asked Questions
What is the purpose of medical equipment evaluation?
Medical equipment evaluation is designed to assess the safety, efficacy, and quality of instruments before they are introduced to the market.
Which region had the largest market for medical equipment evaluation in 2024?
North America emerged as the largest area in the medical equipment evaluation market in 2024.
What are some key evaluation methods used in medical equipment assessment?
Key evaluation methods include automated testing methods, compliance verification, usability testing, and conducting clinical trials.
How do automated testing methods enhance the evaluation process?
Automated testing methods leverage advanced software and hardware solutions to conduct tests with minimal human intervention, improving both efficiency and accuracy.
Why is compliance verification important in medical equipment evaluation?
Compliance verification ensures that products adhere to safety and efficacy regulations, which is essential for legal requirements and building trust among healthcare professionals and patients.
What does usability testing focus on?
Usability testing evaluates how easily healthcare professionals and patients can engage with the medical device, ensuring intuitive design and safety.
What role do clinical trials play in medical device evaluation?
Clinical trials involve testing the apparatus in a controlled environment with real patients to gather vital data on performance and safety, which is crucial for assessing a product's preparedness for market application.
What is the significance of regulatory compliance in the healthcare equipment evaluation process?
Regulatory compliance ensures that products conform to established safety and effectiveness standards, enhancing patient safety and the credibility of manufacturers.
Which regulatory entities are involved in overseeing medical device testing methods?
Key regulatory entities include the FDA in the United States and the European Medicines Agency (EMA) in Europe.
What are some services included in comprehensive clinical trial management?
Services include feasibility studies, compliance reviews, trial setup and management, and project management and reporting.
How does regulatory compliance impact manufacturers in the healthcare sector?
Adhering to regulations enhances the credibility of manufacturers and is vital for patient safety, making it important for companies to stay updated on regulatory developments.
What recent trends highlight the importance of regulatory compliance in the healthcare industry?
A significant percentage of corporate risk and compliance professionals prioritize staying updated on regulatory developments, and many executives express concern over third-party breaches, underscoring the critical nature of compliance.




