Introduction
In the realm of medical device manufacturing, the presence of endotoxins poses a significant challenge that can have dire implications for patient safety. These heat-stable lipopolysaccharides, originating from Gram-negative bacteria, can trigger severe inflammatory responses, leading to complications such as fever and septic shock.
The urgency of addressing endotoxin contamination is underscored by alarming statistics, including the prevalence of Pseudomonas aeruginosa infections in intensive care units.
As regulatory standards evolve and manufacturers strive to enhance safety protocols, understanding the sources, testing methods, and regulatory frameworks surrounding endotoxins becomes critical.
This article delves into the complexities of endotoxin testing, exploring best practices, challenges, and the emerging technologies that promise to revolutionize the landscape of medical device safety.
Understanding Endotoxins: Importance and Implications for Medical Devices
Endotoxin testing medical devices is crucial because endotoxins, which are heat-stable lipopolysaccharides found in the outer membrane of Gram-negative bacteria, present a significant risk. Upon the death of these bacteria, toxic substances are released, potentially triggering severe inflammatory responses in patients. Complications can range from fever and septic shock to more grave outcomes, including death.
Notably, Pseudomonas aeruginosa accounts for 23% of infections acquired in intensive care units (ICUs), underscoring the urgency of addressing endotoxin contamination. Comprehending the origins of these endotoxins—whether from production settings or raw materials—is crucial for guaranteeing device security.
To mitigate risks, manufacturers are required to implement thorough testing protocols that include:
- Endotoxin testing medical devices
- Adhering to safety standards
The recent updates detailed in Annex 1 of the European Union’s GMP highlight the incorporation of sterile cleanroom gloves into Quality Risk Management, aiming to reduce microbial and particulate contamination in medicinal products. This proactive approach is critical not only for protecting patient health but also for preserving the integrity of medical practices.
Furthermore, Pearson FC's comparison of the pyrogenicity of environmental contaminants and lipopolysaccharides highlights the varying risks associated with different sources of these substances, providing valuable insight into their potential impact. Additionally, the FAERS database from 2008 to 2021 recorded over 23 million adverse events, with approximately 1.38% linked to reactions consistent with pyrexia, indicating potential endotoxin-related complications. This information highlights the urgent requirement for strict contamination assessment criteria, particularly in the context of endotoxin testing medical devices, in the production of medical equipment.
As mentioned by Farida Bendali, "Medical Device-Associated Biofilm Infections and Multidrug-Resistant Pathogens" are significant issues that further emphasize the necessity of addressing contamination standards in healthcare.
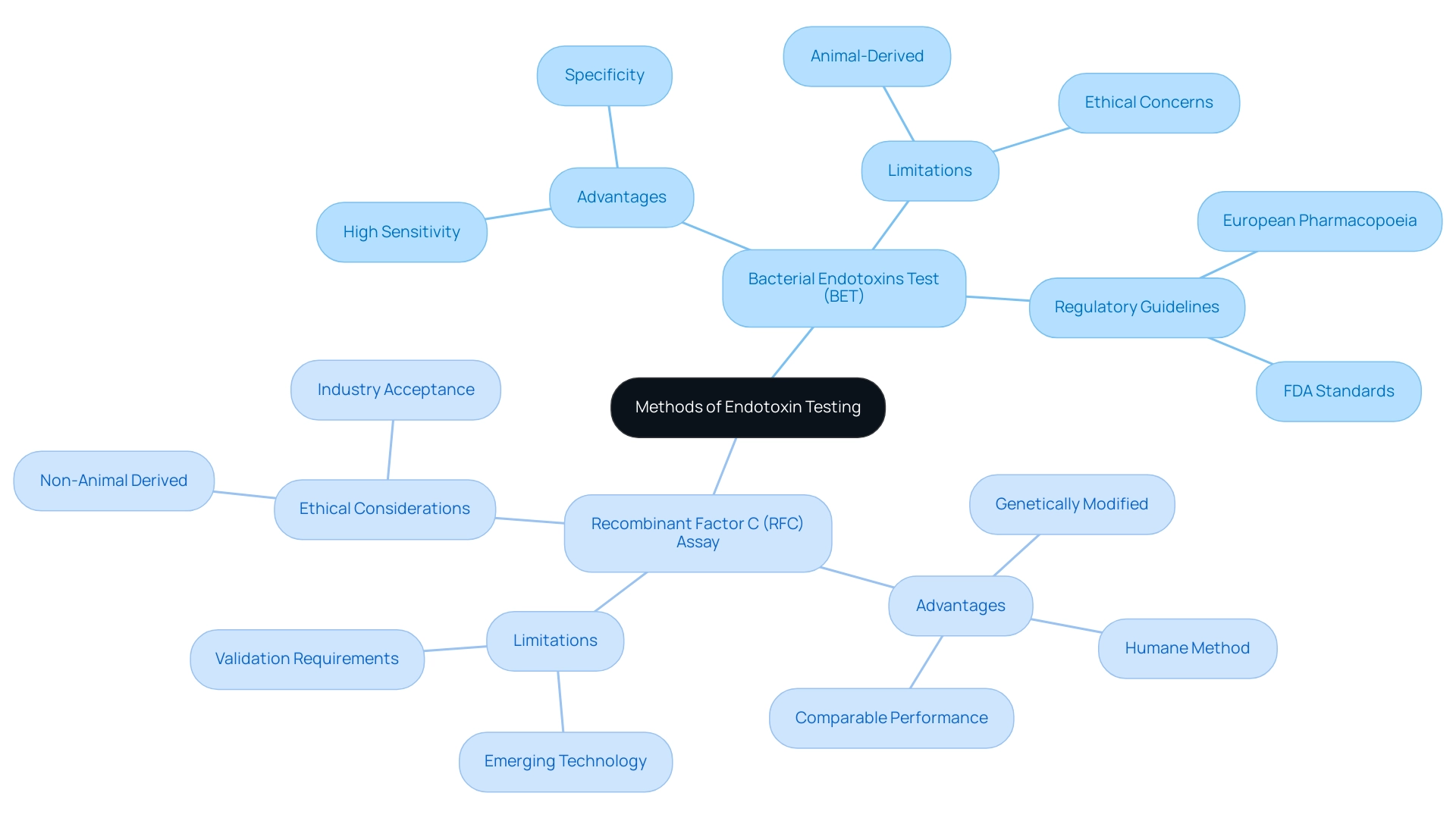
Methods of Endotoxin Testing: Best Practices and Guidelines
Endotoxin testing medical devices is crucial for ensuring their safety and efficacy, with several methods available, each offering distinct advantages and limitations. The most prevalent method is the Bacterial Endotoxins Test (BET), which employs Limulus Amebocyte Lysate (LAL) extracted from horseshoe crab blood. This approach is celebrated for its high sensitivity and specificity in identifying harmful substances, making it a dependable option for numerous producers.
However, ethical concerns surrounding animal-derived products have prompted the rise of the recombinant Factor C (RFC) assay as a promising alternative. The RFC assay employs genetically modified proteins, providing a more humane method for endotoxin evaluation while upholding strict performance standards.
Following standards established by regulatory bodies, such as the FDA and the European Pharmacopoeia, is essential in guaranteeing that all evaluation methods are validated and uniformly applied across different device batches. Recent advancements in the RFC assay have demonstrated comparable performance to traditional methods, making it an appealing choice for companies looking to enhance their evaluation protocols while addressing ethical considerations. According to the Rapid Microbiology Assessment Kits Global Market Report 2025, the demand for dependable contaminant analysis techniques is expected to increase considerably, emphasizing the significance of these methodologies in the sector.
Furthermore, the introduction of Chapter <86> in the USP–NF emphasizes the Bacterial Endotoxins Test using recombinant reagents, which could lead to a shift towards non-animal derived assessment methods. As David Hussong, former microbiology committee chair, stated, "I saw this statement as managerial overreach into a key job of the committee: to ascertain that the new tests were as safe as what the industry had already been using." Staying informed about best practices for endotoxin testing medical devices in 2024 will be essential for clinical research directors aiming to uphold safety and compliance in medical device development.
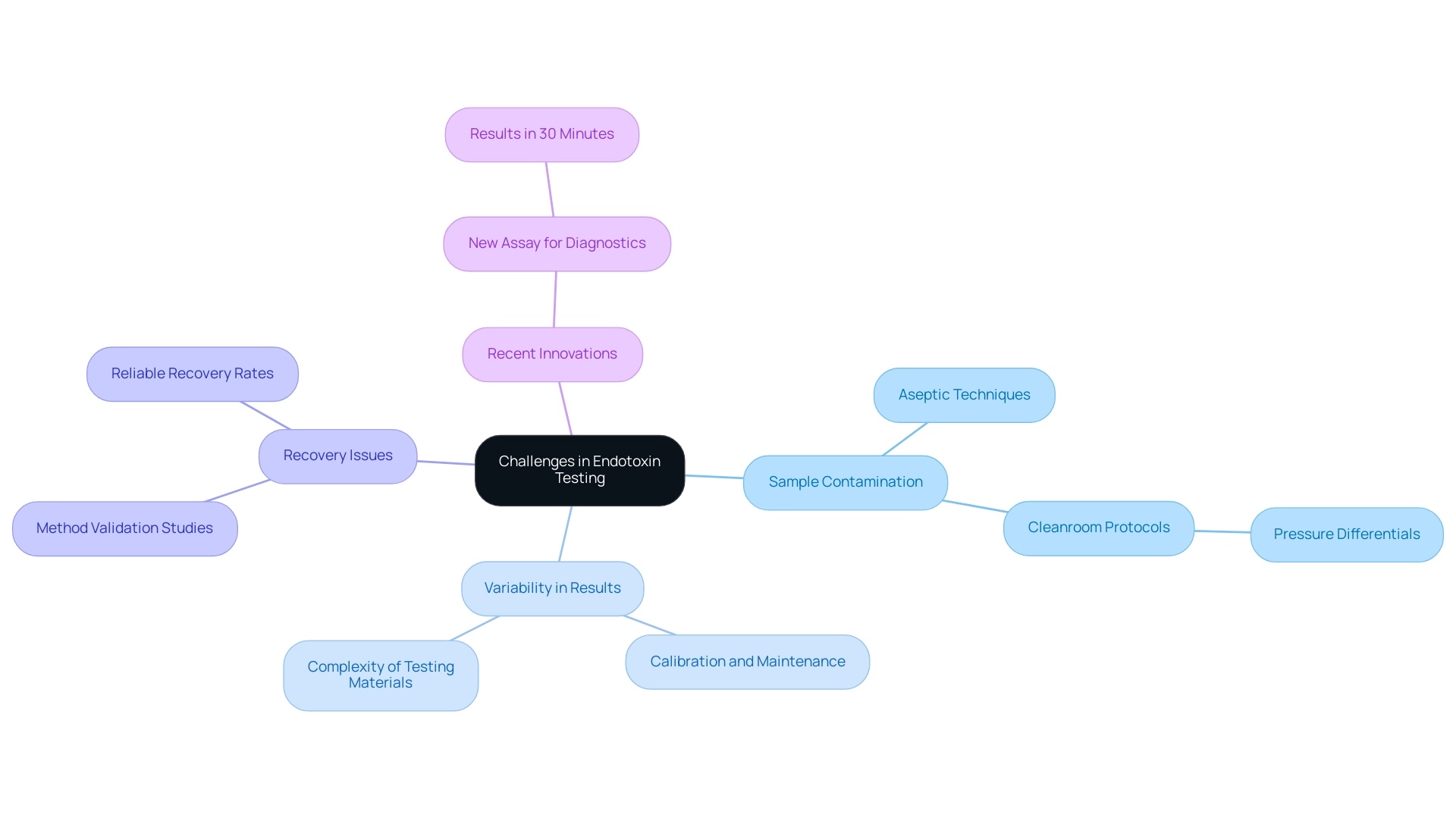
Challenges in Endotoxin Testing: Overcoming Common Obstacles
The challenges in endotoxin analysis can significantly affect the accuracy and reliability of endotoxin testing medical devices results. Among these, sample contamination, variability in test outcomes, and issues related to recovery are significant hurdles that laboratories face. Contamination can occur at various stages of the evaluation process, making the implementation of aseptic techniques paramount.
As Dr. Tim Sandle from Bio Products Laboratory Limited emphasizes, "Maintaining strict adherence to cleanroom protocols is essential, especially in environments where pressure differentials between cleanroom grades are crucial to prevent cross-contamination." This highlights the critical nature of these protocols in ensuring reliable testing outcomes.
Moreover, the variability in results can often stem from the complexities associated with endotoxin testing medical devices or the materials being tested. Recent statistics indicate that up to 30% of endotoxin tests can yield inconsistent results due to these challenges. This necessitates the regular calibration and rigorous maintenance of measurement equipment to ensure consistent performance.
To address recovery issues, particularly when dealing with complex devices, conducting method validation studies for endotoxin testing medical devices is essential. These studies help establish reliable recovery rates, ultimately enhancing the validity of the assessment process.
Furthermore, progress in toxin analysis is evident in the recent authorization of a new assay for human diagnostic application, able to produce results in only 30 minutes. This innovation underscores the need for laboratories to adapt their protocols to incorporate such advancements, thereby improving efficiency and patient outcomes.
By actively addressing these challenges and incorporating best practices, organizations can greatly enhance the strength of their evaluation protocols, resulting in more reliable outcomes that are essential for patient well-being and regulatory adherence. The incorporation of these strategies is not only beneficial but crucial in managing the intricacies of contemporary medical equipment evaluation.
Regulatory Standards for Endotoxin Testing in Medical Devices
Regulatory agencies like the FDA and ISO have established strict protocols for endotoxin testing medical devices, which is essential for ensuring patient safety. The FDA's draft guidance document (2020-16340), published in the Federal Register, outlines acceptable contamination levels customized for different product classifications, requiring that manufacturers conduct thorough evaluations to ensure adherence. In parallel, ISO 10993-11 outlines a framework for assessing the biocompatibility of medical devices, which includes endotoxin testing medical devices as a vital component.
Professionals in the area, such as Ana Criado, Director of Regulatory Affairs and CEO of Mahu Pharma, emphasize the significance of following these standards to guarantee protection. Edward C. Tidswell from Merck & Co. highlights this importance, stating, 'Recently, some health authorities had mistakenly proposed the addition of an arbitrary protection factor into a specification limit for toxins.' This underscores the necessity of adhering strictly to established standards rather than introducing potentially flawed modifications.
Furthermore, the FDA's guidance on establishing limits for toxins during the development of investigational oncology drugs and biological products serves as a relevant case study for endotoxin testing medical devices, illustrating how adherence to these guidelines can ensure safety and efficacy in drug development. Notably, the comment period for this guidance closed on September 28, 2020, reflecting the ongoing collaborative effort between stakeholders, including regulatory consultants like Katherine Ruiz, to refine and finalize these essential standards, which are pivotal for manufacturers aiming to ensure their products are compliant and safe for patient use.
The Future of Endotoxin Testing: Innovations and Emerging Technologies
The field of toxin analysis is on the brink of notable progress, fueled by new technologies that aim to improve both efficiency and precision. Automated evaluation systems are being designed to optimize the workflow, thereby minimizing human error and increasing throughput. This is particularly crucial in a market projected to grow at a compound annual growth rate (CAGR) of 8.4%, reaching an estimated size of USD 4.81 million in 2024, with a forecast period extending to 2033 and historical data available from 2011 to 2023.
Furthermore, innovative biosensors utilizing nanotechnology are emerging, allowing for rapid and highly sensitive identification of toxic substances. According to Cognitive Market Research:
- "The endotoxin examination market is driven by:
- increasing drug development
- rising infectious diseases
- technological advancements in detection methods
- emphasis on quality control
- expanding biotechnology sector
- healthcare expenditure growth
- manufacturing contamination risks
- the rise of Contract Research Organizations (CROs)."
These innovations not only aim to streamline the assessment process but also play a pivotal role in enhancing the safety of medical devices through endotoxin testing medical devices, thereby positively impacting patient outcomes.
As pharmaceutical companies accelerate drug development efforts, the focus on thorough evaluation protocols becomes increasingly crucial, exemplified by recent expansions in examination facilities, such as Wickham Micro's initiative to meet the rising demand for microbiology services. Additionally, it is important to note that there is a default error of the BET ranging from 50-200%, highlighting the need for precision in evaluation. Embracing these advancements in endotoxin testing medical devices technology will be essential for maintaining high standards of product safety and compliance.
Conclusion
The complexities surrounding endotoxin testing in medical device manufacturing underscore its critical importance for ensuring patient safety. The presence of endotoxins, particularly from Gram-negative bacteria, poses significant risks, including severe inflammatory responses that can lead to dire health complications. As outlined, the prevalence of infections such as those caused by Pseudomonas aeruginosa in intensive care units highlights the urgent need for effective contamination control measures and stringent testing protocols.
Advancements in endotoxin testing methodologies, such as the Bacterial Endotoxins Test (BET) and the recombinant Factor C (rFC) assay, reflect a growing commitment to enhancing testing accuracy and ethical considerations. These methods, alongside adherence to evolving regulatory standards from bodies like the FDA and ISO, are vital in establishing a robust framework for ensuring the safety and efficacy of medical devices. The challenges faced in endotoxin testing, including sample contamination and variability in results, necessitate the implementation of best practices and innovative technologies to improve testing reliability.
Looking ahead, the future of endotoxin testing is poised for transformation, driven by innovations in automated systems and biosensors that promise to enhance both efficiency and accuracy. As the demand for rigorous testing protocols continues to grow, embracing these advancements will be essential for manufacturers aiming to uphold the highest standards of product safety and regulatory compliance. Ultimately, a proactive approach to endotoxin safety not only protects patients but also preserves the integrity of healthcare practices, reinforcing the critical role of effective endotoxin management in the medical device industry.
Frequently Asked Questions
Why is endotoxin testing crucial for medical devices?
Endotoxin testing is essential because endotoxins, which are heat-stable lipopolysaccharides from Gram-negative bacteria, can trigger severe inflammatory responses in patients, leading to complications such as fever, septic shock, or even death.
What are the risks associated with endotoxin contamination in healthcare settings?
Risks include severe infections, particularly in intensive care units, where Pseudomonas aeruginosa is a significant concern, accounting for 23% of infections. Understanding the sources of endotoxins is vital for ensuring device safety.
What protocols should manufacturers implement to mitigate endotoxin risks?
Manufacturers must conduct thorough endotoxin testing, adhere to safety standards, and incorporate sterile cleanroom gloves into their Quality Risk Management practices to reduce microbial and particulate contamination.
What does the recent update in the European Union's GMP entail regarding endotoxin testing?
The update emphasizes the importance of incorporating sterile cleanroom gloves into Quality Risk Management to enhance the safety of medicinal products by minimizing contamination.
What is the most common method for endotoxin testing?
The most prevalent method is the Bacterial Endotoxins Test (BET), which uses Limulus Amebocyte Lysate (LAL) from horseshoe crab blood, known for its high sensitivity and specificity.
Are there alternatives to the traditional endotoxin testing methods?
Yes, the recombinant Factor C (RFC) assay has emerged as a humane alternative, using genetically modified proteins while maintaining strict performance standards.
How do regulatory bodies influence endotoxin testing methods?
Regulatory bodies like the FDA and the European Pharmacopoeia set standards that ensure all endotoxin testing methods are validated and consistently applied across different device batches.
What advancements have been made in the RFC assay?
Recent advancements indicate that the RFC assay performs comparably to traditional methods, making it an attractive option for companies seeking to improve their testing protocols while addressing ethical concerns.
What is the significance of Chapter <86> in the USP–NF regarding endotoxin testing?
Chapter <86> emphasizes the use of recombinant reagents for the Bacterial Endotoxins Test, potentially leading to a shift towards non-animal derived testing methods.
Why is it important for clinical research directors to stay informed about endotoxin testing best practices?
Staying informed is crucial for ensuring safety and compliance in medical device development, particularly with evolving testing methodologies and regulatory standards.




