Introduction
In the intricate landscape of medical device approval, the design of pivotal studies stands as a cornerstone for ensuring safety and efficacy. This multifaceted process demands meticulous planning and execution, guided by a series of critical steps that encompass everything from defining study objectives to managing stakeholder engagement.
As the medical field continues to evolve, the integration of comprehensive clinical trial management services emerges as a vital resource, facilitating the successful navigation of regulatory requirements and enhancing the overall integrity of clinical research.
This article delves into the essential strategies for designing effective pivotal studies, emphasizing the importance of:
- Quality control
- Regulatory interactions
- Stakeholder collaboration
in achieving favorable outcomes.
Designing Pivotal Studies for Medical Device Approval
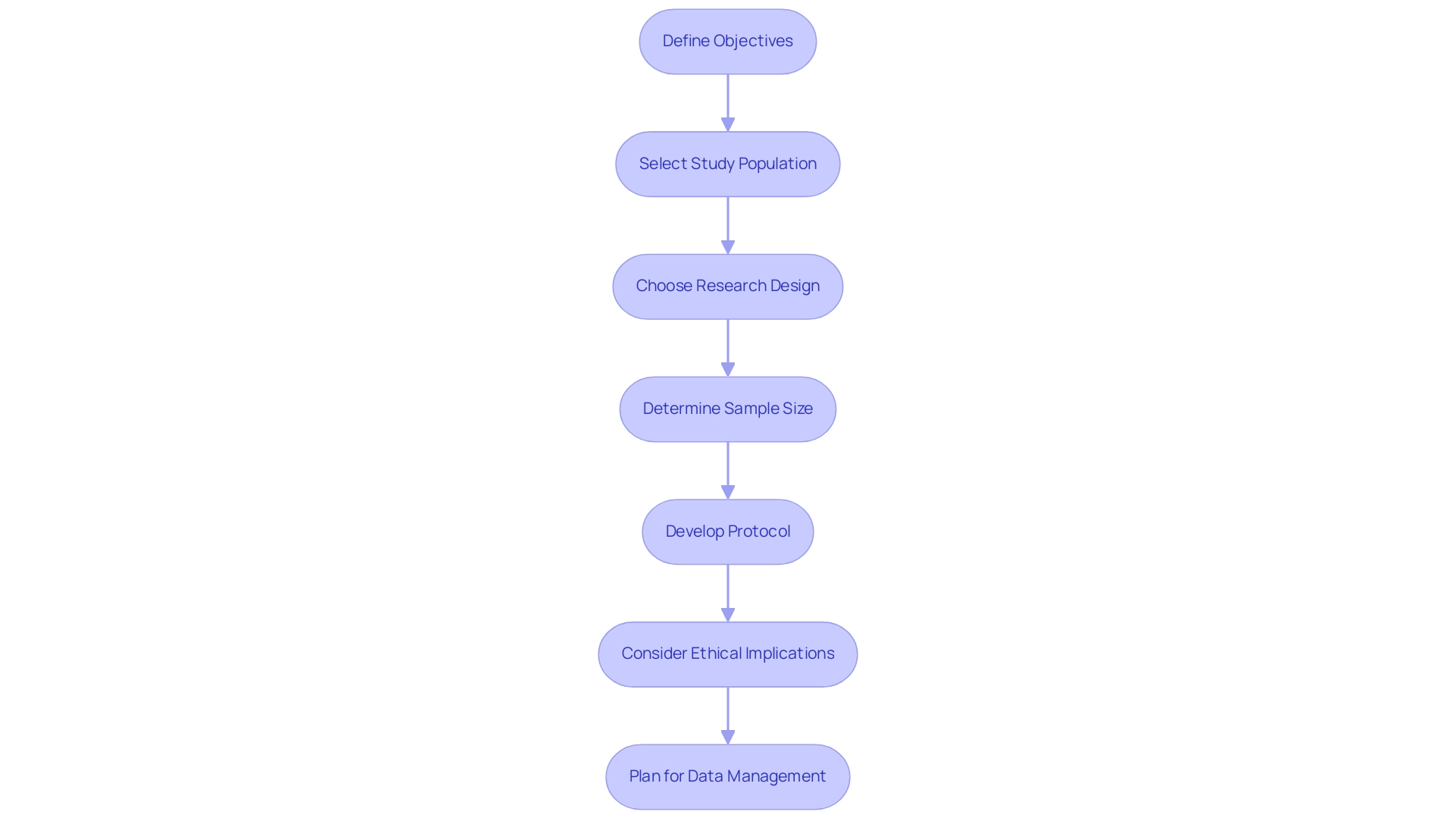
Designing pivotal studies for medical device approval requires careful planning and execution, and leveraging comprehensive clinical trial management services can significantly enhance this process. Here are the essential steps to consider:
-
Define Objectives: Clearly articulate the primary and secondary aims of the research.
This includes identifying the endpoints that will effectively demonstrate the device's safety and efficacy, adhering to industry standards.
-
Select Study Population: Determine the target group for the research.
This involves considering diverse factors such as age, sex, medical history, and the specific conditions that the device aims to address to ensure representative and relevant results.
-
Choose Research Design: Select the appropriate research design based on the objectives and the nature of the device.
Common options include randomized controlled trials (RCTs), cohort analysis, and case-control investigations, each offering distinct advantages suited to different research scenarios.
-
Determine Sample Size: Calculate the necessary sample size to achieve statistically significant outcomes.
This calculation should incorporate the expected effect size, variability within the population, and the statistical power required to support the research findings.
-
Develop Protocol: Create a comprehensive research protocol that details every aspect of the project.
This should include methodology, data collection techniques, and statistical analysis plans, ensuring clarity and consistency throughout the research process.
-
Consider Ethical Implications: It is vital to adhere to ethical standards in research design.
This includes obtaining informed consent from participants and implementing measures to ensure their safety and wellbeing throughout the research duration.
-
Plan for Data Management: Establish a robust framework for data collection, management, and analysis.
This should ensure data integrity and adherence to relevant regulatory requirements, ultimately bolstering the credibility of research results.
At bioaccess®, our specialized approach facilitates these essential steps. We facilitate feasibility assessments, site selection, compliance reviews, trial setup, and project management to navigate your clinical trials successfully. Our team, with over 20 years of experience in Medtech, is skilled at managing various types of research, including Early-Feasibility Assessments, First-In-Human Trials, Pilot Trials, and Pivotal Studies for Medical Device Approval, as well as Post-Market Clinical Follow-Up Trials.
Recent discussions have emphasized the significance of conducting research free from premature disclosure and outside pressures, reinforcing the need for a well-organized approach in crucial research designs that prioritize both scientific integrity and participant safety. Moreover, the involvement of stakeholders in crucial research discussions, as highlighted in feedback received by the FDA, emphasizes the cooperative effort necessary for successful clinical tests. Transparency in clinical trials remains paramount, ensuring that all aspects of the research meet consumer needs.
Navigating Regulatory Interactions for Successful Study Approval
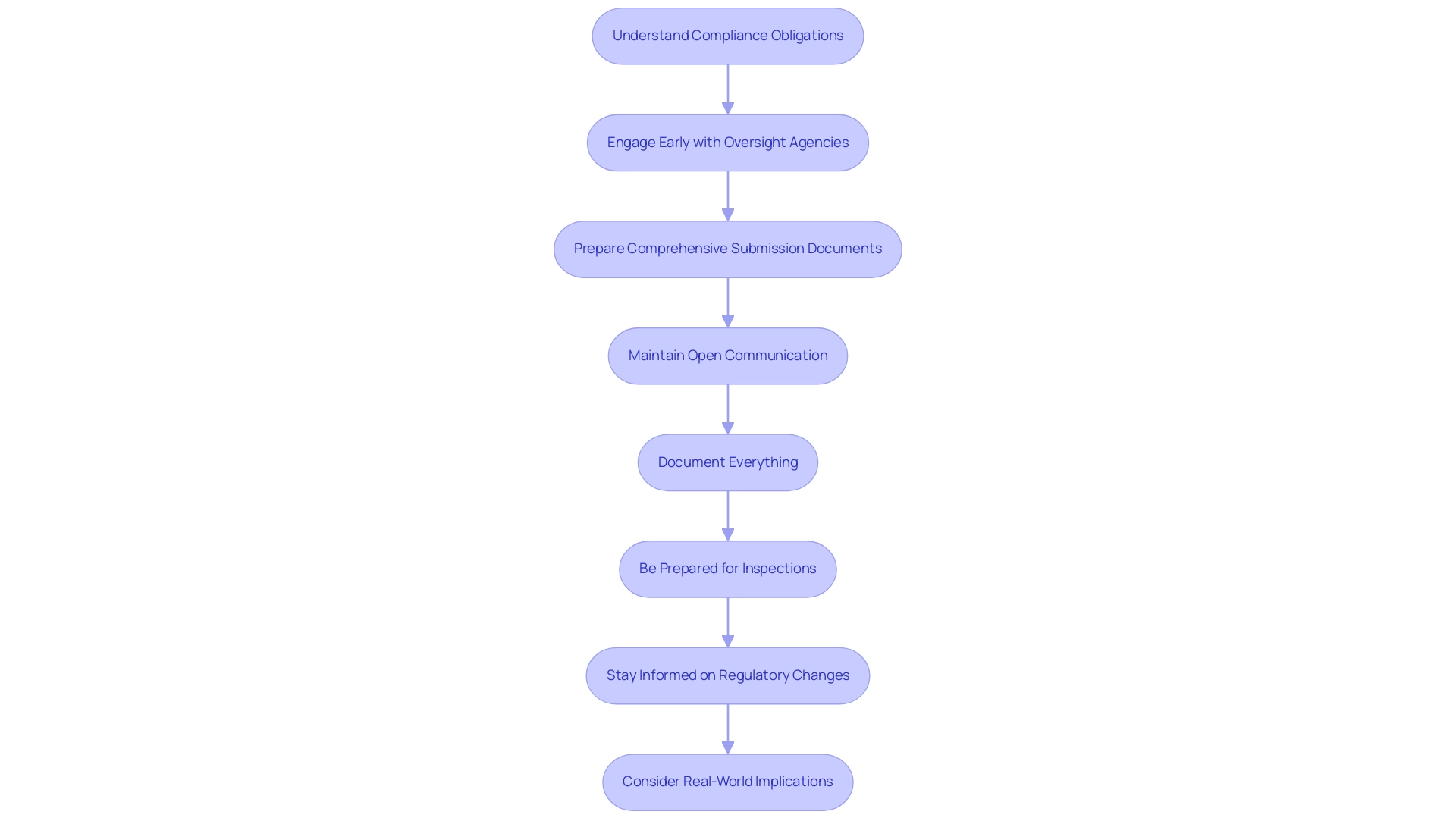
To successfully manage compliance interactions in medical device research, consider implementing the following strategies:
- Understand Compliance Obligations: It's essential to become acquainted with the current guidelines overseeing medical device research in 2024. This includes guidance documents issued by agencies such as the FDA and EMA, which outline essential criteria for pivotal studies for medical device approval and compliance. As a statistic illustrates, the negative percent agreement in a new scenario is 99.2%, emphasizing the importance of adhering to these regulations.
- Engage Early with Oversight Agencies: Initiating pre-submission meetings with oversight bodies can significantly enhance your research's design and objectives. Early engagement allows for valuable feedback, enabling refinement of plans and mitigation of potential issues before submission. Experts such as Ana Criado, who has her extensive background in compliance affairs and biomedical engineering, emphasize that early communication can greatly influence the outcomes of pivotal studies for medical device approval.
- Prepare Comprehensive Submission Documents: Ensure that all submission materials, including the research protocol, informed consent forms, and data management plans, are meticulously prepared. These documents must align with compliance standards to facilitate a smooth review process.
- Maintain Open Communication: Establish and maintain open lines of communication with oversight agencies throughout your study. Promptly addressing inquiries or concerns fosters a collaborative relationship, which is vital for successful interactions.
- Document Everything: Keep detailed records of all interactions with regulatory agencies, including meeting notes, correspondence, and feedback received. Comprehensive documentation is essential for reference during the review process and can aid in clarifying any points of contention.
- Be Prepared for Inspections: Regulatory agencies may conduct inspections or audits as part of their oversight. Ensure that all research activities adhere to Good Clinical Practice (GCP) guidelines to demonstrate compliance and assure quality in your study.
- Stay Informed on Regulatory Changes: Regularly review updates to regulations and guidance that may affect your research. Proactively monitoring these changes ensures that your research remains compliant and adapts to evolving governance landscapes.
- Consider Real-World Implications: A case analysis titled 'Impact of Prevalence on Agreement Measures' illustrates how the agreement between a new test and a non-reference standard can change based on the prevalence of the condition in the population examined. This underscores the impact of prevalence on agreement metrics and the significance of comprehending this dynamic in regulatory interactions.
By utilizing the knowledge of professionals like Ana Criado and Katherine Ruiz, who possess extensive experience in regulatory affairs for medical devices and clinical evaluations, including Pivotal Studies for Medical Device Approval alongside services such as feasibility assessments, setup, import permits, and reporting of research status and adverse events, you can improve your strategy for fulfilling regulatory requirements and ensuring successful outcomes.
Implementing Quality Control Measures
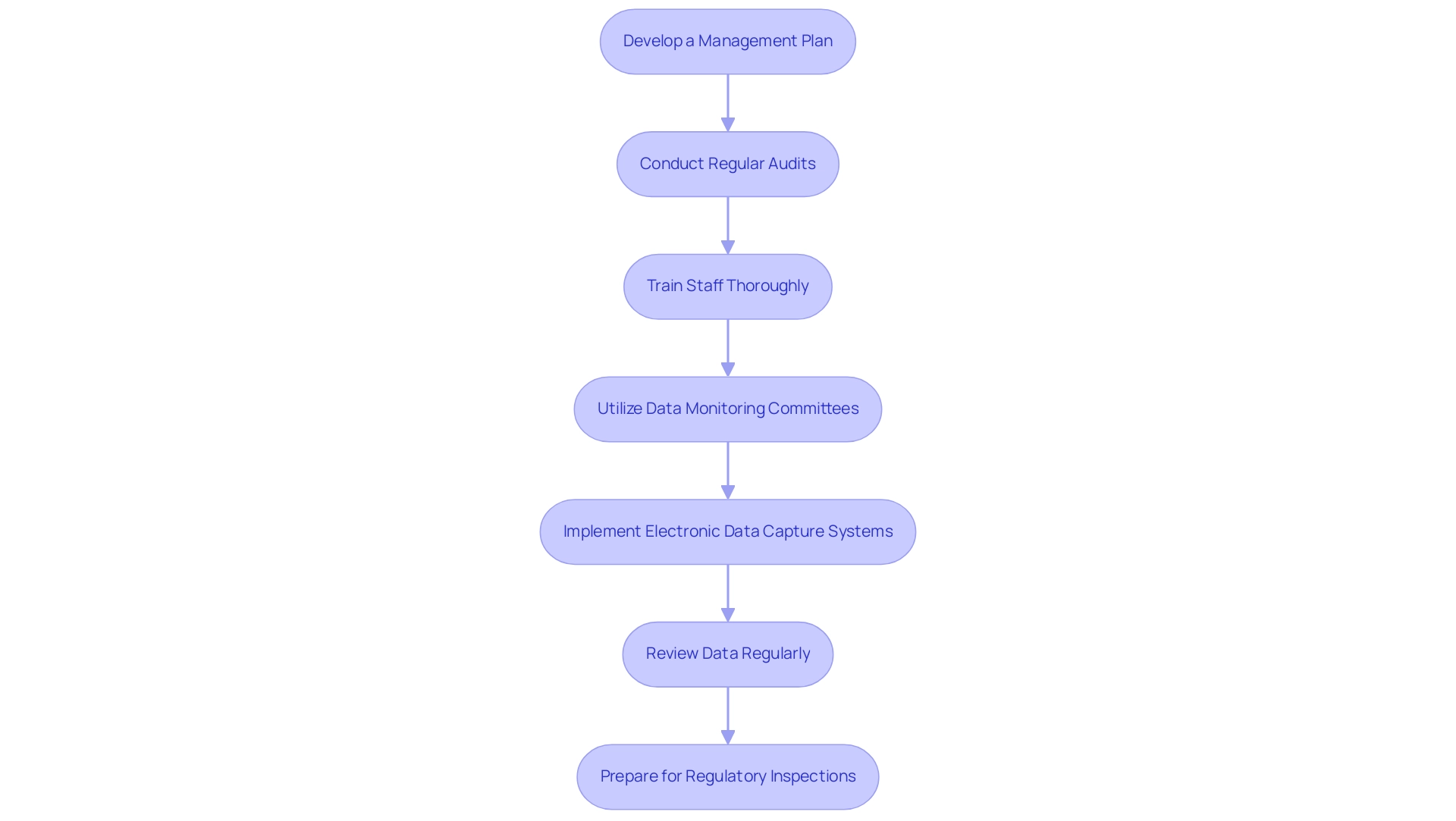
Applying strong assurance procedures in crucial research necessitates a strategic method, particularly in the realm of clinical trials in Latin America. Here are essential steps to consider:
-
Develop a Management Plan: Formulate a detailed management plan that delineates performance objectives, applicable standards, and procedures to be adhered to throughout the research.
This plan serves as the foundation for maintaining quality throughout the research process, particularly when navigating regulatory frameworks like those established by INVIMA.
-
Conduct Regular Audits: Schedule systematic audits to evaluate research processes, data collection techniques, and adherence to the established protocol. Such audits are critical for early identification and correction of potential issues, safeguarding research integrity, and ensuring compliance with local regulations.
-
Train Staff Thoroughly: Invest in comprehensive training for all team members regarding research protocols, regulatory requirements, and assurance practices. Ongoing education is essential, as it guarantees that staff are well-prepared to maintain quality standards and adjust to the specific challenges of conducting studies in Latin America.
-
Utilize Data Monitoring Committees: Establish independent data monitoring committees responsible for overseeing the project's progression.
These committees play a crucial role in ensuring that safety and efficacy data are collected in accordance with established guidelines, reflecting the meticulous oversight required in pivotal studies.
-
Implement Electronic Data Capture Systems: Leverage electronic data capture (EDC) systems to enhance data collection efficiency and reduce the likelihood of errors associated with manual data entry. The integration of EDC systems is increasingly acknowledged for its positive effect on data accuracy in clinical trials, particularly when handling complex research such as Early-Feasibility and First-In-Human investigations.
-
Review Data Regularly: Conduct continuous data reviews to detect trends, discrepancies, or anomalies that could influence research outcomes. Promptly addressing identified issues is essential for maintaining the study's validity. Monitoring should commence when the number of enrolled participants hits 30, as this is a crucial threshold for implementing control measures.
-
Prepare for Regulatory Inspections: Ensure that all control documentation and processes are meticulously organized and ready for examination by regulatory agencies during inspections. This preparation is vital for showcasing adherence and cultivating trust in the findings, especially considering INVIMA's role in supervising medical device assessments in Colombia.
A practical example of effective control can be observed in the Beta-Binomial model for QTL monitoring, which utilizes Bayesian methods to track tolerance limits (QTLs) in clinical evaluations. This method employs historical information to guide the previous distribution of event probabilities, facilitating a detailed comprehension of event occurrences and allowing for the detection of out-of-control processes based on the posterior predictive distribution.
As highlighted by industry authorities, including John Kirkpatrick, effective assurance measures are crucial in preserving the integrity of clinical evaluations, particularly in the realm of pivotal studies for medical device approval overseen by seasoned partners like bioaccess®.
bioaccess® provides extensive services, including viability assessments, location selection, trial preparation, project oversight, and approval procedures, ensuring that all elements of clinical trials are carefully managed to achieve the highest standards of quality and adherence.
Maintaining Stakeholder Engagement
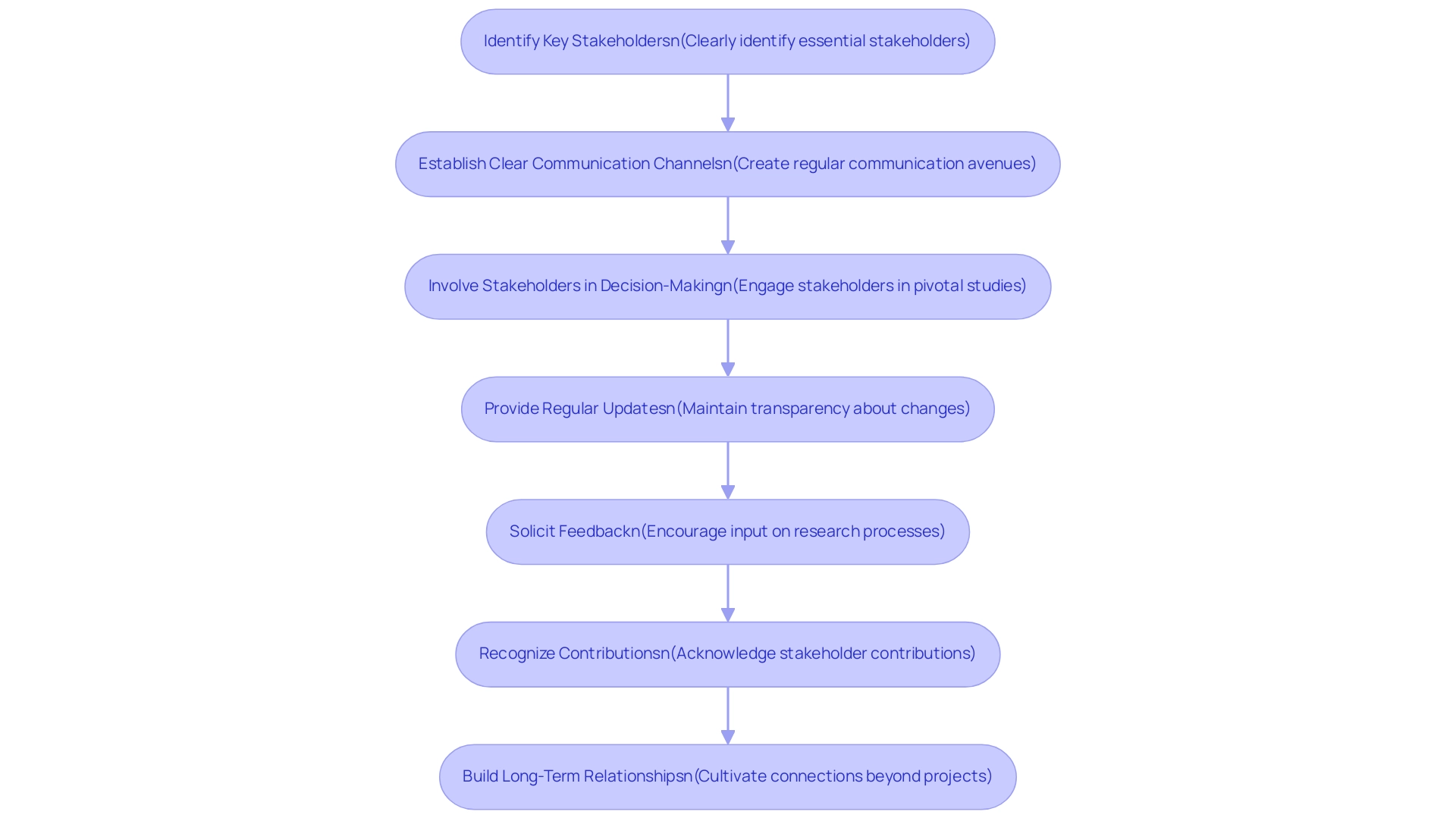
To ensure effective stakeholder engagement throughout essential research, it is crucial to implement the following strategies:
- Identify Key Stakeholders: Clearly identify essential stakeholders, including investigators, sponsors, regulatory bodies, and ethics committees, to facilitate focused engagement.
- Establish Clear Communication Channels: Create regular communication avenues such as meetings, newsletters, or updates, ensuring stakeholders are consistently informed about project progress and developments. This is vital as effective communication can significantly influence educational outcomes. As noted by Julie Kennedy Lesch from the Patient-Centered Outcomes Research Institute, effective communication is pivotal in ensuring that stakeholder perspectives are integrated into research processes.
- Involve Stakeholders in Decision-Making: Actively engage stakeholders in pivotal studies for medical device approval, including research design and recruitment strategies. Their insights can be invaluable in addressing concerns and enhancing the project's relevance.
- Provide Regular Updates: Maintain transparency by regularly informing stakeholders about any changes to the research protocol, timelines, or outcomes. This openness fosters trust and collaboration among all parties involved.
- Solicit Feedback: Encourage stakeholders to provide input on research processes and outcomes. This practice not only leads to improvements but also enhances overall learning quality, as highlighted in recent research, which cataloged 387 discrete examples of influence across 58 investigations.
- Recognize Contributions: Acknowledge and appreciate the contributions of stakeholders throughout the research process. Recognition reinforces their importance to the project's success and fosters a collaborative environment.
- Build Long-Term Relationships: Focus on cultivating long-term connections with stakeholders that extend beyond individual projects. This approach can facilitate future collaborations and support, aligning with the recommendations from the report titled Future Directions for Stakeholder Engagement Research, which advocates for enhanced understanding and practices in stakeholder engagement. This report highlights the necessity for descriptive and evaluative analysis that can assist in reducing the variability in reporting quality and content concerning stakeholder involvement in research.
Incorporating these strategies improves stakeholder involvement and aligns with our comprehensive clinical trial management services, including feasibility assessments, site selection, compliance reviews, trial setup, import permits, project management, monitoring, and reporting. Furthermore, by conducting clinical studies, we contribute to the local economy through job creation, economic growth, and improved healthcare, while fostering international collaboration.
Conclusion
Designing effective pivotal studies for medical device approval is a complex yet essential process that hinges on meticulous planning and execution. The article underscores the importance of:
- Clearly defining study objectives
- Selecting an appropriate study population
- Utilizing suitable study designs
These foundational steps, coupled with a well-structured protocol and rigorous ethical considerations, ensure that the studies not only comply with regulatory standards but also yield reliable and valid results.
Moreover, maintaining robust quality control measures and engaging effectively with regulatory agencies are paramount in navigating the intricate landscape of medical device approvals. By understanding regulatory requirements, preparing comprehensive submission documents, and fostering open communication, stakeholders can significantly enhance the likelihood of successful study outcomes. Regular audits and thorough staff training further solidify the integrity of the research process, which is critical in the evolving field of medical technology.
Lastly, the emphasis on stakeholder engagement throughout the study process cannot be overstated. Identifying key stakeholders, establishing clear communication channels, and involving them in decision-making are crucial strategies that contribute to the overall success of pivotal studies. By fostering collaboration and transparency, the research community can not only improve study quality but also build lasting relationships that benefit future endeavors.
In conclusion, the meticulous design of pivotal studies, underpinned by quality control, regulatory compliance, and active stakeholder engagement, is vital for advancing medical device innovation. As the landscape of clinical research continues to evolve, embracing these strategies will ensure that the safety and efficacy of medical devices are thoroughly evaluated, ultimately leading to better health outcomes for patients globally.
Frequently Asked Questions
What are the essential steps for designing pivotal studies for medical device approval?
The essential steps include defining objectives, selecting the study population, choosing the research design, determining sample size, developing a protocol, considering ethical implications, and planning for data management.
Why is it important to define objectives in a medical device study?
Defining objectives is crucial as it articulates the primary and secondary aims of the research and identifies endpoints that demonstrate the device's safety and efficacy according to industry standards.
How do you select the appropriate study population for a medical device study?
The study population should be selected based on diverse factors such as age, sex, medical history, and specific conditions the device addresses, ensuring the results are representative and relevant.
What types of research designs can be chosen for medical device studies?
Common research designs include randomized controlled trials (RCTs), cohort analysis, and case-control investigations, each offering distinct advantages for different research scenarios.
How is the sample size for a study determined?
The sample size is calculated based on the expected effect size, variability within the population, and the statistical power needed to achieve statistically significant outcomes.
What should a comprehensive research protocol include?
A research protocol should detail methodology, data collection techniques, and statistical analysis plans to ensure clarity and consistency throughout the research process.
What ethical considerations must be taken into account in medical device research?
Ethical considerations include obtaining informed consent from participants and implementing measures to ensure their safety and well-being during the research.
Why is data management planning important in clinical trials?
A robust data management plan ensures data integrity, adherence to regulatory requirements, and bolsters the credibility of research results.
How can organizations like bioaccess® assist in the clinical trial process?
Bioaccess® offers services such as feasibility assessments, site selection, compliance reviews, trial setup, and project management to navigate clinical trials successfully.
What role does stakeholder engagement play in medical device research?
Stakeholder engagement is vital for ensuring that various perspectives are integrated into the research process, enhancing relevance and trust among all parties involved.




