Introduction
In the intricate landscape of clinical research, the development of a robust clinical development plan is paramount for successful FDA submissions. This comprehensive document serves as a blueprint, detailing every aspect of the clinical trial process, from study objectives to risk management strategies.
As organizations navigate the complexities of regulatory compliance, resource allocation, and stakeholder communication, understanding the essential components and best practices for creating an effective plan becomes critical.
This article delves into the key elements that comprise a clinical development plan, the challenges faced during its creation, and the strategies that can enhance its efficacy, ultimately paving the way for successful clinical trials and regulatory approvals.
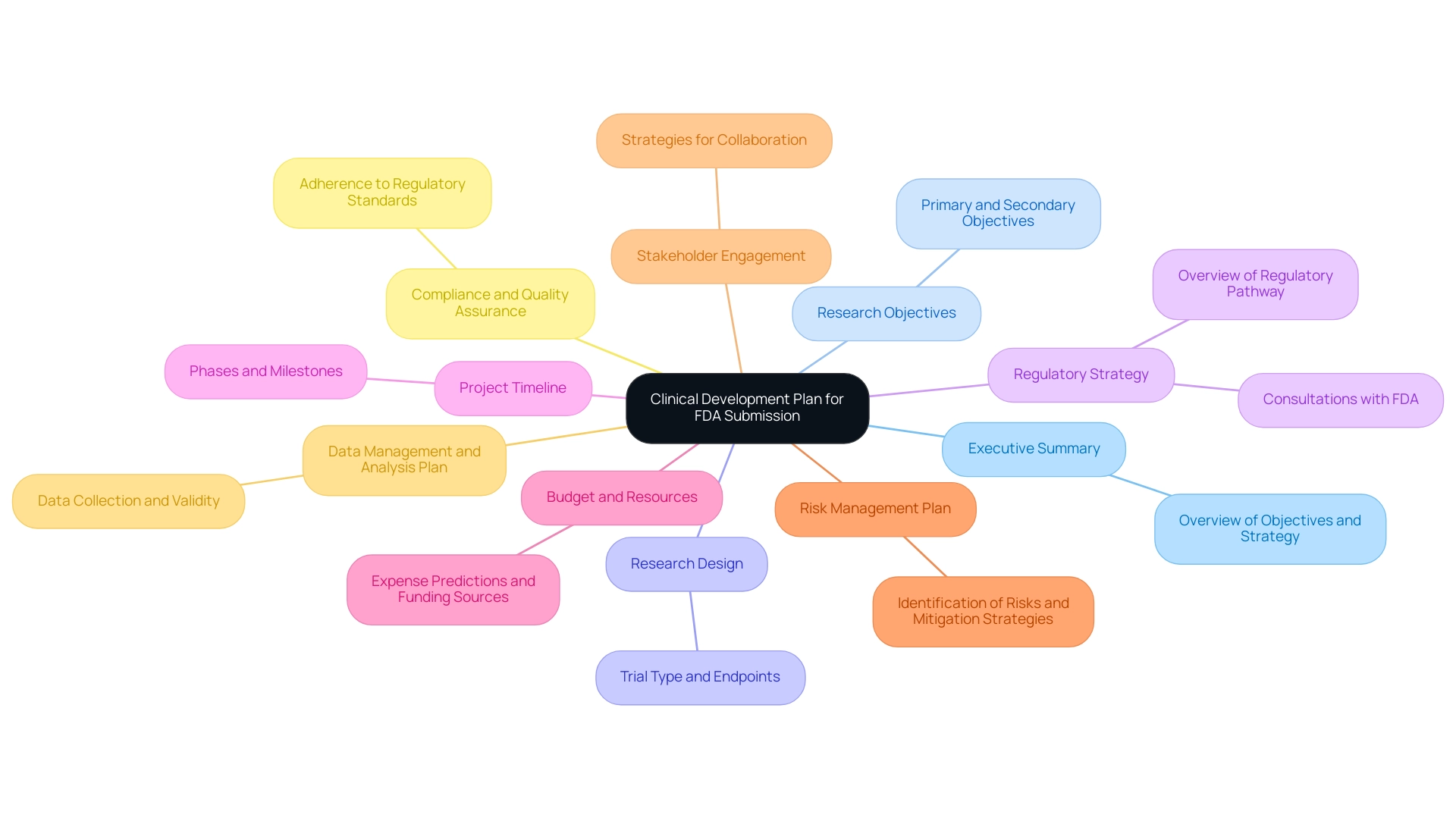
Key Components of a Clinical Development Plan for FDA Submission
When preparing a clinical development plan for FDA submission, it is crucial to encompass the following key components:
- Executive Summary: This section should succinctly outline the project's objectives, significance, and the overall development strategy, providing a snapshot of what the plan entails.
- Research Objectives: Clearly articulated primary and secondary objectives are essential, delineating precisely what the research aims to achieve and how success will be measured.
- Research Design: Detailed descriptions of the research design must be included, specifying the type of trial (e.g., randomized, controlled), the target population, and the defined endpoints.
- Regulatory Strategy: An overview of the regulatory pathway should be provided, incorporating any pre-Investigational New Drug (IND) meetings or consultations with the FDA, which can inform the submission process. Leveraging the expertise of professionals such as Katherine Ruiz, an expert in regulatory affairs for medical devices and in vitro diagnostics in Colombia, can be invaluable in navigating these complexities.
- Project Timeline: A comprehensive timeline outlining the various phases of the research, including key milestones and critical deadlines, is imperative to keep the project on track.
- Budget and Resources: A comprehensive budget analysis that predicts expenses, recognizes funding sources, and distributes resources efficiently is essential for managing financial expectations throughout the project.
- Risk Management Plan: This plan should identify potential risks associated with the research and establish mitigation strategies to address them proactively.
- Stakeholder Engagement: Strategies for engaging with essential stakeholders—including investigators, ethics committees, and regulatory bodies—must be clearly outlined to facilitate collaboration and communication. Ana Criado, Director of Regulatory Affairs and an expert in biomedical engineering, emphasizes the importance of stakeholder engagement for successful trials.
- Data Management and Analysis Plan: A robust strategy for data collection, management, and analysis should be established, ensuring that the data collected will be both reliable and valid for regulatory scrutiny.
- Compliance and Quality Assurance: Procedures to maintain adherence to regulatory requirements and quality standards throughout the research are critical for a successful submission.
Incorporating these components not only ensures that the clinical development plan template FDA is comprehensive but also aligns with the FDA’s submission requirements, thus enhancing the likelihood of a successful review. Furthermore, essential service functions such as study setup, import permits, project oversight, and reporting on research status and adverse events must be incorporated into the plan to offer a comprehensive overview of research management services. Considering that medical studies can be a program’s most costly and high-risk element, adhering to the FDA Data Standards Catalog for compliance with submission formats is crucial.
As Kenya B., Executive Assistant at PharPoint, states, "Meeting the FDA's requirements is not just about compliance; it's about ensuring the integrity and success of the trial process." This perspective underscores the importance of a meticulous approach in developing these plans.
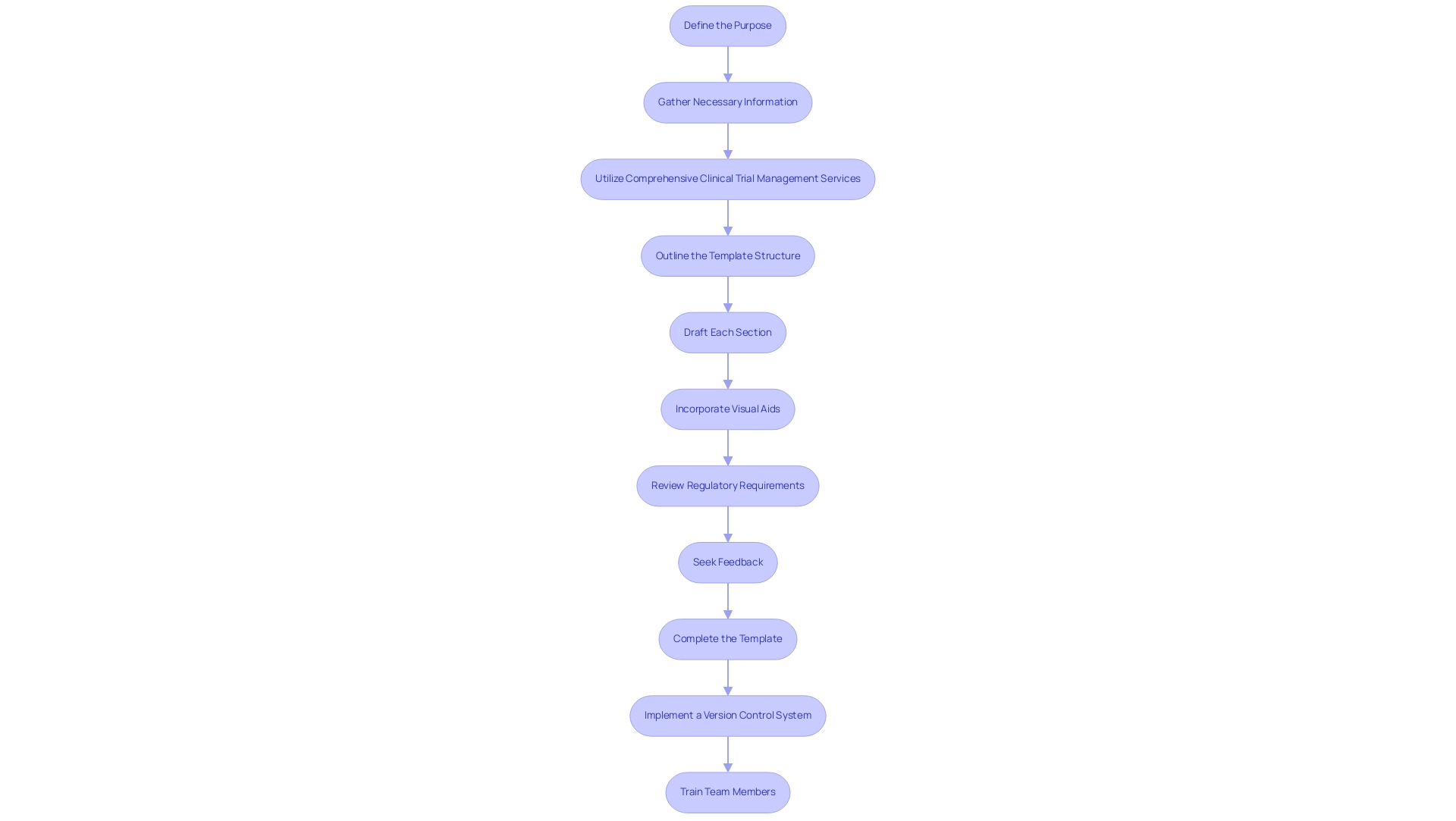
Step-by-Step Guide to Creating an Effective Clinical Development Plan Template
Creating an effective medical research plan template involves several essential steps that ensure compliance and relevance in the research field:
- Define the Purpose: Begin by clearly articulating the purpose of the clinical development plan template FDA, identifying the target audience and outlining the intended use of the plan, which is crucial for aligning with regulatory expectations.
- Gather Necessary Information: Collect comprehensive data, encompassing regulatory guidelines, previous research results, and input from stakeholders. This foundational step ensures that the clinical development plan template FDA is constructed on a solid base of relevant information.
- Utilize Comprehensive Clinical Trial Management Services: Participate in feasibility assessments and choose suitable research locations and principal investigators (PIs). This step is vital for ensuring the study's success and compliance with local regulations. Additionally, ensure thorough trial set-up and start-up processes are detailed to facilitate timely approvals from ethics committees and health ministries.
- Outline the Template Structure: Create a structured outline that includes key components vital for a strong development plan. This outline serves as the backbone of your clinical development plan template FDA, guiding the subsequent sections.
- Draft Each Section: Begin drafting each section methodically, addressing all necessary components. Utilize clear and concise language to effectively convey information, making it accessible to all stakeholders involved.
- Incorporate Visual Aids: Where applicable, enhance the template with visual aids such as charts, graphs, and timelines. These tools can significantly improve understanding and readability, clarifying complex information for the reader.
- Review Regulatory Requirements: Rigorously cross-check the draft against the clinical development plan template FDA guidelines to ensure full compliance. This may involve consultation with regulatory experts, including those familiar with INVIMA's oversight in Colombia, to address any potential gaps. Additionally, include a thorough review and feedback on study documents to ensure compliance with country requirements, and perform quality assurance reviews by individuals other than those collecting the data, essential for maintaining compliance with protocols.
- Seek Feedback: Share the draft template with key stakeholders, including team members and external collaborators. Gathering feedback is vital for refining the template and ensuring it meets the needs of all parties involved. Input from medical researchers and subject matter experts can help define experimental endpoints, ensuring the template reflects the trial's scientific goals.
- Complete the Template: After integrating feedback, complete the template, ensuring it is refined and prepared for application in future healthcare planning.
- Implement a Version Control System: Establish a robust version control system to track changes and updates to the template. This ensures that all users have access to the most current and accurate version.
- Train Team Members: Provide comprehensive training for team members on the effective utilization of the template. Highlight the significance of following the specified procedures to uphold the integrity of the research.
By adhering to these steps, you will produce a detailed clinical development plan template FDA that aligns with submission criteria and improves the overall quality of research initiatives. As highlighted by the NIAMS Executive Secretary,
The investigator will be responsible for ensuring participants’ safety on a daily basis and for reporting Serious Adverse Events and Unanticipated Problems to his or her Institutional Review Board, NIAMS, and the Monitoring Body, and FDA as required.
This emphasizes the essential role of safety and adherence in the medical research process.
Moreover, the interim analysis scheduled at the conclusion of year one, anticipating roughly 50% of participants to be monitored for a minimum of six months, highlights the significance of participant tracking in the research strategy.
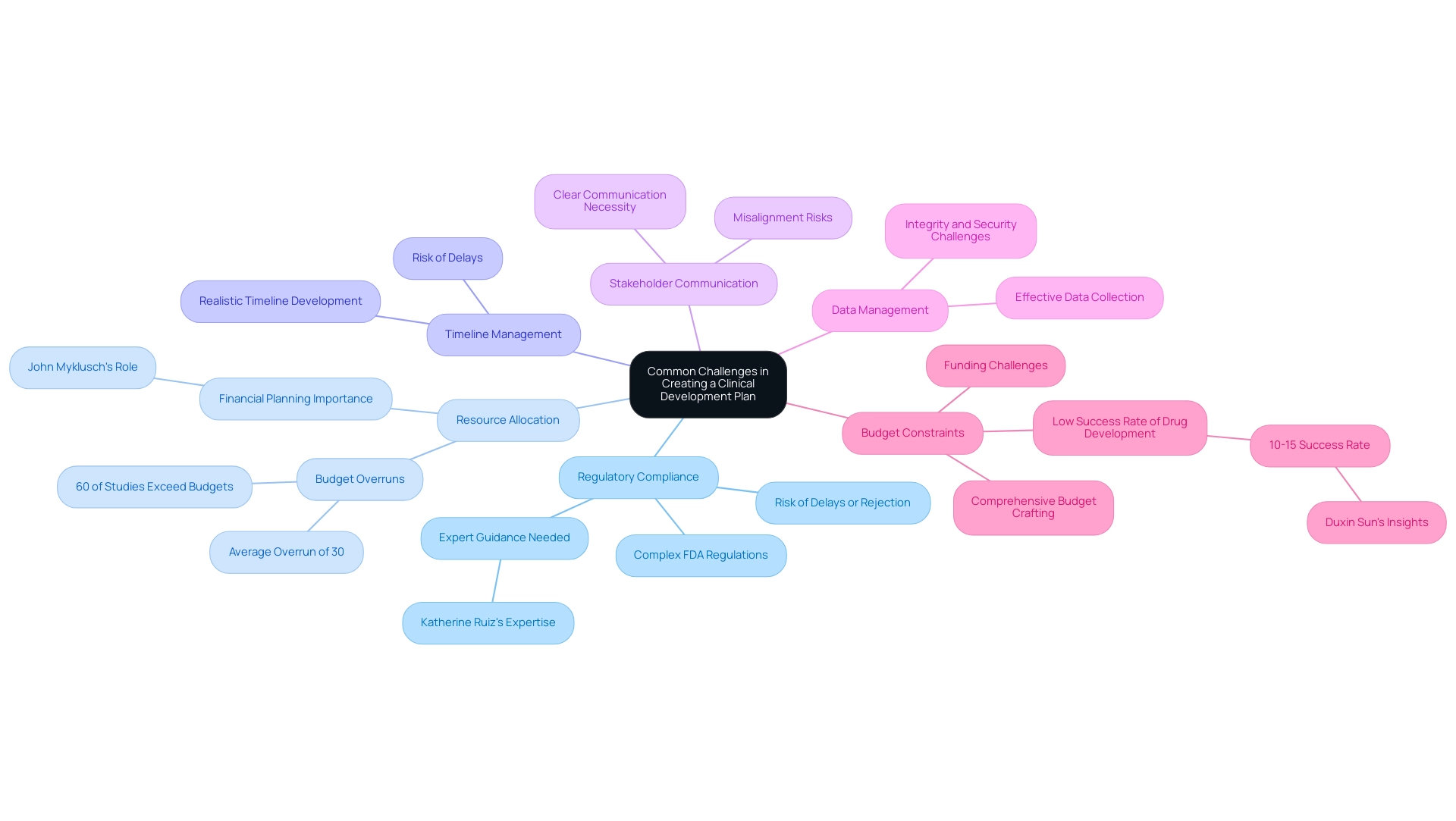
Common Challenges in Creating a Clinical Development Plan
Developing a medical advancement plan is fraught with challenges that can significantly impact the success of medical device evaluations. Key challenges include:
-
Regulatory Compliance: Navigating the complexities of FDA regulations can be particularly daunting for new researchers.
The stakes are high, as non-compliance can lead to delays or rejection of submissions. With the expertise of professionals like Katherine Ruiz, an expert in regulatory affairs for medical devices and in vitro diagnostics in Colombia, teams can better navigate these complexities through compliance reviews and strategic guidance.
-
Resource Allocation: Balancing limited resources with project demands often results in conflicts and inefficiencies.
For example, a staggering 60% of research studies experience budget overruns, averaging 30% above initial estimates, underscoring the need for meticulous financial planning. John Myklusch, our Chief Financial Officer, leverages over 20 years of experience in financial strategy and risk management to help steer projects towards success. In fact, the average cost per failed clinical trial project is $1.3 billion, highlighting the financial stakes involved in clinical development.
-
Timeline Management: Developing a realistic timeline that accounts for potential delays is crucial yet frequently underestimated.
Without careful consideration, projects risk falling behind schedule, which can jeopardize overall objectives.
-
Stakeholder Communication: Maintaining clear communication among diverse stakeholders is essential.
Misunderstandings can lead to misalignment in project goals and expectations, complicating the progress process.
-
Data Management: Effective data collection and management, while ensuring integrity and security, present ongoing challenges.
The complexity of data environments necessitates robust strategies to safeguard sensitive information.
-
Budget Constraints: Crafting a comprehensive budget that accurately reflects the project's needs can be complex, particularly when securing necessary funding proves challenging.
As observed by Duxin Sun, the overall success rate for medical drug creation remains low at only 10%–15%, which emphasizes the vital need for effective financial supervision due to the substantial expenses involved.
A pertinent case analysis highlights that budget overruns are common in medical examinations, with 60% surpassing their budgets by an average of 30%. This highlights the significance of efficient financial planning, as a biotech consulting firm can offer strategic financial management to ensure research projects remain within budget while upholding quality.
By identifying these challenges early in the planning phase and applying strategic solutions, including the thorough trial management services provided by bioaccess®, such as feasibility studies, site selection, trial setup, and project management, teams can create a clinical development plan template FDA to reduce risks and improve their likelihood of successful FDA submissions. Recent discussions in the industry have also pointed to the potential of generative AI to streamline processes within Contract Research Organizations (CROs), suggesting innovative avenues for overcoming these regulatory compliance hurdles. Bioaccess® specializes in Early-Feasibility Studies, First-In-Human Studies, Pilot Studies, Pivotal Studies, and Post-Market Clinical Follow-Up Studies, ensuring a tailored approach to meet the unique needs of each project.
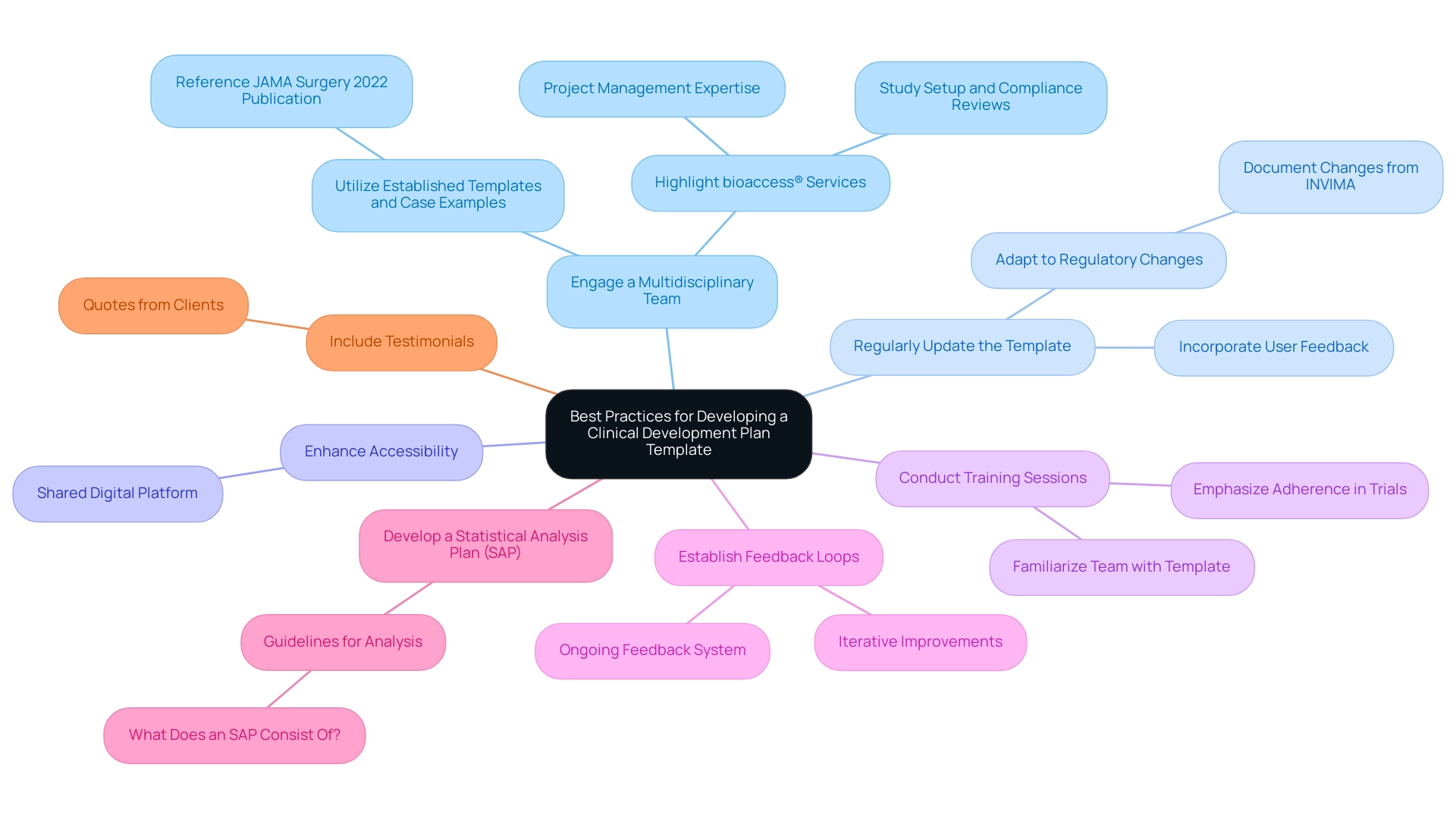
Best Practices for Developing a Clinical Development Plan Template
Creating an effective medical advancement plan template necessitates adherence to several best practices that leverage the strengths of a multidisciplinary approach:
-
Engage a Multidisciplinary Team: Involve experts from medical, regulatory, and statistical domains to ensure a comprehensive perspective that enriches the development process. This is particularly vital for managing the intricacies of medical studies in Latin America, where bioaccess® has over 20 years of expertise.
- Utilize Established Templates and Case Examples: Reference existing templates and successful case examples, such as those outlined in the 2022 JAMA Surgery publication, which highlight practical statistical considerations in healthcare research, including the importance of recording and summarizing medical history by body system using the MedDRA dictionary for coding. These resources can provide valuable guidance and structure.
-
Regularly Update the Template: Maintain the relevance of the template by incorporating user feedback and adapting to the latest regulatory changes, particularly those from INVIMA, Colombia's National Food and Drug Surveillance Institute. Adjustments in statistical analysis methodologies from the protocol should be recorded and justified in the final research study report, ensuring transparency and rigor.
- Prioritize Clarity and Conciseness: Employ clear, straightforward language while avoiding jargon, making the plan accessible and understandable to all stakeholders involved.
-
Enhance Accessibility: Ensure that the template is readily available to all team members through a shared digital platform, facilitating collaboration and communication.
-
Conduct Training Sessions: Implement training programs to familiarize team members with the template’s application and emphasize the significance of adherence in trials. As noted by Cytel,
We dare to evolve because we must — innovation is the heartbeat of our mission to advance the future of human health through the power of data science.
-
Establish Feedback Loops: Create a robust system for ongoing feedback and iterative improvements based on user experiences, ensuring that the template evolves to meet the needs of the medical development process.
-
Develop a Statistical Analysis Plan (SAP): Refer to the case documentation titled 'What Does an SAP Consist Of?' to demonstrate the significance of creating a Statistical Analysis Plan alongside the research protocol, emphasizing the necessity for comprehensive guidelines for analysis.
-
Highlight bioaccess® Services: Incorporate details about bioaccess®'s specific services, including study setup, compliance reviews, and project management, emphasizing their flexibility and specialized knowledge in managing various study types, such as Early-Feasibility Studies and First-In-Human Studies.
-
Include Testimonials: Add quotes or testimonials from clients to enhance credibility and provide social proof of bioaccess®'s capabilities.
By adhering to these best practices, clinical teams can significantly enhance the effectiveness and efficiency of their clinical development plan template FDA submissions, thereby streamlining the submission process to the FDA and ultimately contributing to the success of clinical trials, especially when leveraging the comprehensive services offered by bioaccess®.
Conclusion
The development of a clinical development plan is integral to navigating the complexities of FDA submissions and ensuring the success of clinical trials. By focusing on key components such as:
- A well-defined executive summary
- Clear study objectives
- A comprehensive risk management plan
organizations can create a robust framework that addresses regulatory requirements and enhances the likelihood of approval.
In addition to outlining essential elements, this article emphasizes the importance of addressing common challenges such as:
- Regulatory compliance
- Resource allocation
- Stakeholder communication
Recognizing these challenges early allows for the implementation of strategic solutions, ultimately streamlining the clinical trial process. Best practices, including engaging multidisciplinary teams and utilizing established templates, further contribute to the creation of effective clinical development plans.
Ultimately, a meticulous approach to developing these plans not only facilitates successful FDA submissions but also fosters the integrity of the clinical research process. By prioritizing clarity, compliance, and collaboration, organizations can pave the way for innovative advancements in healthcare, ensuring that clinical trials are conducted efficiently and ethically.
Frequently Asked Questions
What are the key components of a clinical development plan for FDA submission?
The key components include an Executive Summary, Research Objectives, Research Design, Regulatory Strategy, Project Timeline, Budget and Resources, Risk Management Plan, Stakeholder Engagement, Data Management and Analysis Plan, and Compliance and Quality Assurance.
What should be included in the Executive Summary of the clinical development plan?
The Executive Summary should succinctly outline the project's objectives, significance, and overall development strategy, providing a snapshot of what the plan entails.
Why are clearly articulated research objectives important?
Clearly articulated primary and secondary research objectives are essential to delineate precisely what the research aims to achieve and how success will be measured.
What details are necessary in the Research Design section?
The Research Design section must include detailed descriptions of the trial type (e.g., randomized, controlled), the target population, and defined endpoints.
What does the Regulatory Strategy overview entail?
The Regulatory Strategy should provide an overview of the regulatory pathway, including any pre-Investigational New Drug (IND) meetings or consultations with the FDA.
Why is a comprehensive Project Timeline important?
A comprehensive Project Timeline outlines the various phases of the research, including key milestones and critical deadlines, which is imperative to keep the project on track.
What should the Budget and Resources section include?
The Budget and Resources section should include a comprehensive budget analysis that predicts expenses, recognizes funding sources, and distributes resources efficiently.
What is the purpose of a Risk Management Plan?
The Risk Management Plan should identify potential risks associated with the research and establish mitigation strategies to address them proactively.
What strategies should be outlined for Stakeholder Engagement?
Strategies for engaging with essential stakeholders—including investigators, ethics committees, and regulatory bodies—must be clearly outlined to facilitate collaboration and communication.
How should data be managed and analyzed according to the plan?
A robust Data Management and Analysis Plan should be established to ensure that data collection, management, and analysis will yield reliable and valid results for regulatory scrutiny.
Why is Compliance and Quality Assurance critical in the research plan?
Compliance and Quality Assurance procedures are critical to maintain adherence to regulatory requirements and quality standards throughout the research, which is essential for a successful submission.
What additional service functions should be incorporated into the clinical development plan?
Additional service functions such as study setup, import permits, project oversight, and reporting on research status and adverse events should be incorporated to offer a comprehensive overview of research management services.
Why is adherence to the FDA Data Standards Catalog important?
Adhering to the FDA Data Standards Catalog for compliance with submission formats is crucial because medical studies can be costly and high-risk, and it enhances the likelihood of a successful review.
What is the significance of a meticulous approach in developing clinical development plans?
A meticulous approach is important as it ensures compliance with FDA requirements and helps maintain the integrity and success of the trial process.




