Overview
The article centers on the critical factors influencing the design of medical device trials, asserting the necessity of:
- Clear objectives
- Well-defined target populations
- Measurable endpoints
- Strict adherence to ethical standards
It substantiates this assertion by delineating best practices and critical-to-quality factors that bolster the integrity and success of trials. Ultimately, these elements ensure compliance with regulatory requirements and enhance patient outcomes.
Introduction
In the rapidly evolving landscape of medical device trials, grasping the fundamental principles and methodologies is essential for success. As the industry adapts to emerging technologies and regulatory demands, the design of clinical studies must emphasize:
- Clear objectives
- Robust data management
- Ethical considerations
With over two decades of experience, bioaccess® stands at the forefront, providing tailored solutions that navigate the complexities of trial management. This article explores:
- The essential elements of effective trial design
- The critical-to-quality factors that ensure reliability
- The emerging trends shaping the future of clinical research
By delving into these themes, stakeholders can gain valuable insights into optimizing their approach to medical device development, ultimately enhancing patient outcomes.
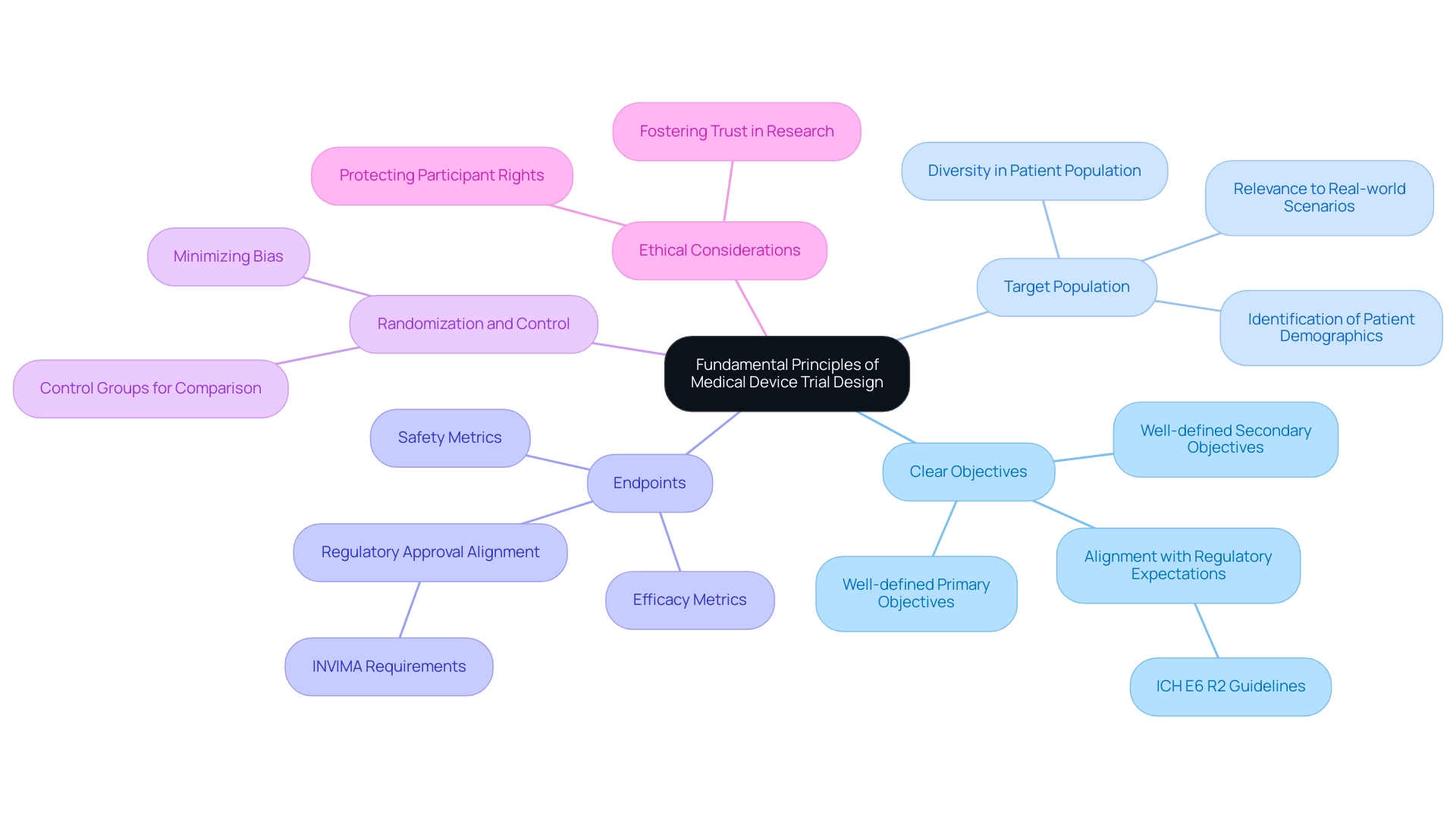
Fundamental Principles of Medical Device Trial Design
The fundamental concepts of factors in designing device trials are essential for ensuring the success and integrity of research. Key elements include:
- Clear Objectives: Establishing well-defined primary and secondary objectives is crucial. These objectives not only guide the research's focus but also align with regulatory expectations, as highlighted by the ICH E6 R2 guidelines, which mandate sponsors to manage risk in a way that reduces the burden on sites. At bioaccess®, we emphasize the importance of these objectives in our comprehensive clinical study management services, ensuring that they are tailored to meet the specific needs of each study.
- Target Population: Identifying and characterizing the patient population is vital. This population should accurately represent the intended use of the device, ensuring that the results are applicable to real-world scenarios. Recent statistics indicate that a diverse patient demographic can enhance the relevance of study outcomes, ultimately leading to improved patient care. Our expertise in Early-Feasibility Studies (EFS) and First-In-Human Studies (FIH) allows us to effectively target and engage the right populations in Latin America.
- Endpoints: Clear and measurable endpoints are necessary to evaluate the study's success. These endpoints typically include safety and efficacy metrics, which are critical for regulatory approval and market acceptance. The establishment of robust endpoints is increasingly recognized as a best practice in modern study design. At bioaccess®, we ensure that endpoints are not only well-defined but also aligned with the regulatory requirements set forth by INVIMA, Colombia's National Food and Drug Surveillance Institute.
- Randomization and Control: Implementing randomization minimizes bias and enhances the reliability of results. Control groups are essential for effective outcome comparison, allowing for a clearer understanding of the device's impact relative to standard treatments or placebo. Our team is proficient in creating experiments that incorporate these methodologies to ensure valid and reliable results.
- Ethical Considerations: Adhering to ethical standards is paramount in study design. Protecting the rights and well-being of participants not only fosters trust but also aligns with the growing emphasis on ethical practices in clinical research. bioaccess® is dedicated to maintaining these standards throughout the testing process.
With over 20 years of experience in Medtech, bioaccess® possesses the expertise and customized approach necessary to guide your company toward an acquisition. In 2025, the landscape of medical device studies is evolving, with a focus on simplifying site experiences and reducing patient burden. Innovations in trial methodologies are increasingly recognized for their potential to enhance patient outcomes by providing more relevant data.
For instance, the integration of human cells and tissues in drug discovery reflects a deeper understanding of biological responses, which is expected to accelerate the development of new treatments. This trend illustrates the industry's recognition of the value of using human-based models to improve the relevance of clinical data.
As Danish Mairaj, principal engineer of medical device design at RESYCA, notes, "This is one of the areas where AI can use a lot of data, but gaining insights from this data is only possible if you have certain use cases being implemented in relevant facilities." This emphasizes the significance of utilizing technology to improve design and execution.
As the sector continues to evolve, the importance of clear goals in medical studies cannot be overstated. These objectives serve as a foundation for successful study designs, guiding researchers in their quest to bring innovative medical devices to market efficiently. Moreover, contemporary testing techniques require sponsors to compile various data sources, underscoring the factors in designing device trials that necessitate thorough and clearly outlined goals to manage the complexities of medical research.
To discover more about how bioaccess® can assist with your research requirements, reach out to us today.
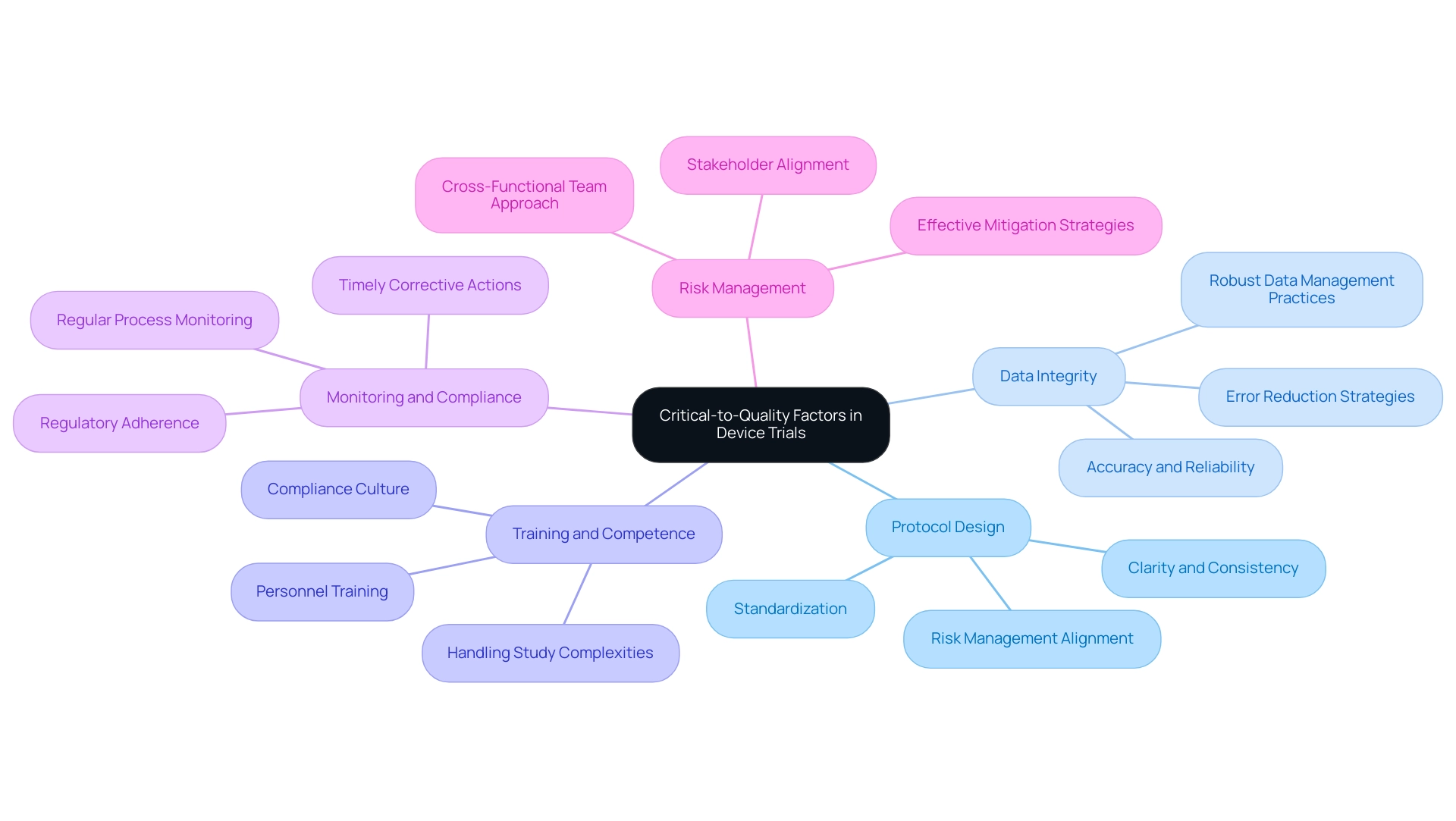
Critical-to-Quality Factors in Device Trials
Critical-to-quality (CTQ) factors in designing device trials play a pivotal role in ensuring the success and reliability of medical research. Key elements include:
- Protocol Design: A meticulously crafted protocol is fundamental for standardizing procedures and ensuring consistency across multiple sites. Effective protocol design not only enhances clarity but also aligns with the latest ICH E6 R2 and R3 revisions, which mandate sponsors to manage risk in a way that alleviates burdens on sites, including minimizing redundant data reviews.
At bioaccess®, we leverage over 20 years of Medtech experience to ensure that our protocols are designed with these factors in mind, reflecting our tailored approach to research.
-
Data Integrity: The integrity of data gathered during studies is paramount. Implementing robust data management practices is essential to guarantee the accuracy and reliability of this data. Recent statistics indicate that maintaining high data integrity can significantly reduce errors by up to 30% and enhance overall results. Our comprehensive clinical study management services include rigorous data integrity protocols to uphold these standards.
-
Training and Competence: Ensuring that all personnel involved in the study are adequately trained and possess the necessary competencies is crucial. This investment in human resources not only enhances the quality of the study but also fosters a culture of compliance and excellence. bioaccess® prioritizes training to ensure our teams are equipped to handle the complexities of Early-Feasibility, First-In-Human, Pilot, Pivotal, and Post-Market Follow-Up Studies.
-
Monitoring and Compliance: Regular monitoring of study processes and strict adherence to regulatory requirements are vital for maintaining quality throughout the study. Continuous oversight helps identify deviations early, allowing for timely corrective actions. Our knowledge in compliance evaluations guarantees that all studies fulfill the required regulatory criteria.
-
Risk Management: Actively recognizing potential risks and formulating effective mitigation strategies is crucial for the seamless advancement of research activities. A cross-functional team approach to risk assessment ensures that all stakeholders are aligned on terminology and expectations, thereby enhancing communication and efficiency. At bioaccess®, we implement customized risk management strategies that demonstrate our profound comprehension of the Latin American healthcare environment and the adaptability necessary in medical product evaluations.
Incorporating these CTQ factors into the design of device trials not only streamlines processes but also significantly enhances the probability of successful results. As the landscape of medical research evolves, embracing these best practices will be crucial for advancing medical devices effectively. Moreover, the varied uses of AI highlight its capacity to transform different dimensions of medical studies, making it essential for organizations to remain informed about these developments.
Additionally, a live webinar on overcoming challenges and accelerating clinical study completion, scheduled for March 19, 2025, underscores the ongoing relevance of these discussions.
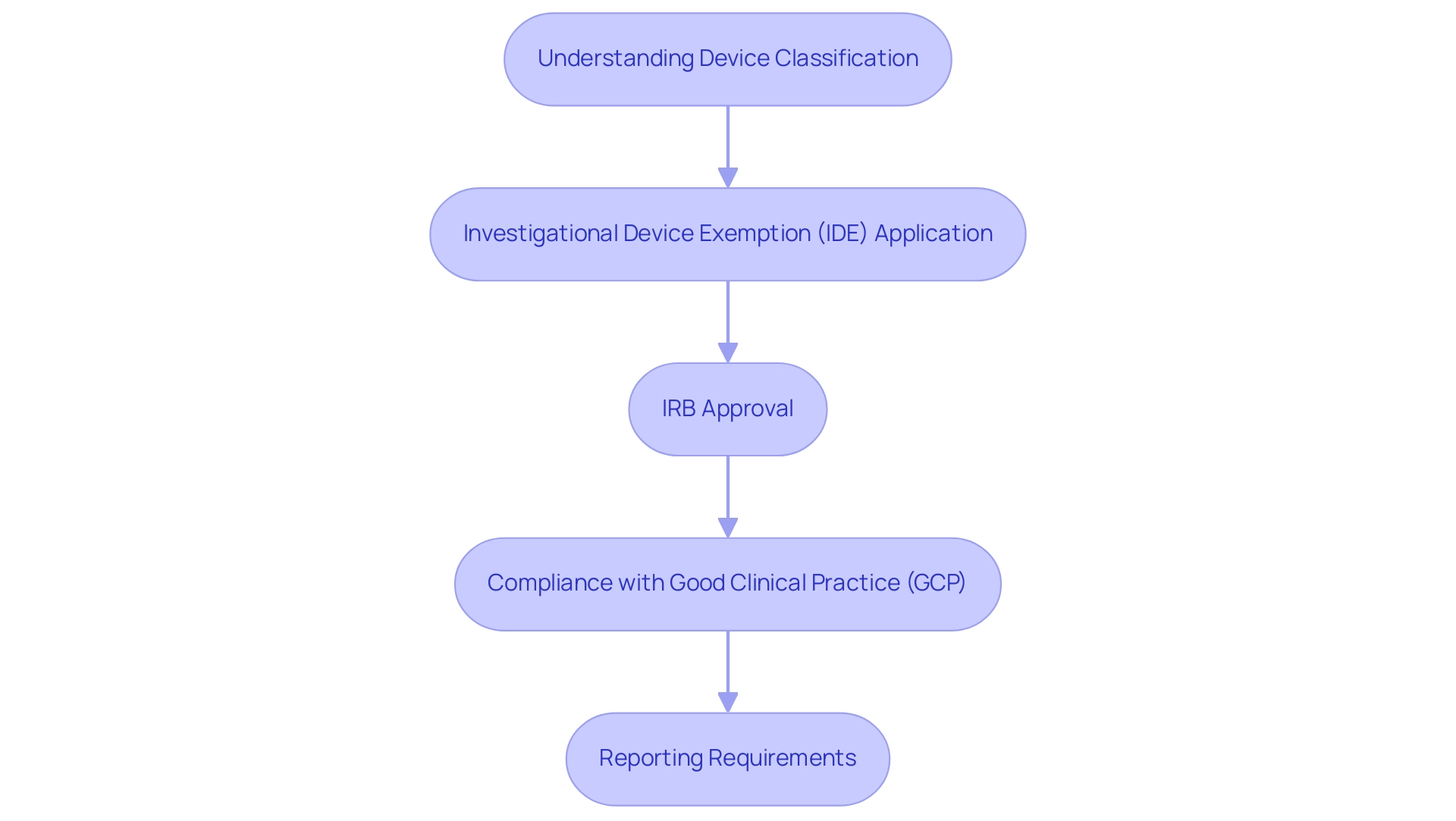
Navigating Regulatory Requirements for Device Trials
Navigating regulatory requirements for medical device trials is a multifaceted process that demands a thorough understanding of various components.
- Understanding Device Classification: The first step is to accurately determine the classification of the device, which can fall into Class I, II, or III categories. Each classification comes with its own set of regulations and requirements, which are critical factors in designing device trials and impacting the approval process. For instance, Class III products, typically considered high-risk, require more stringent regulatory scrutiny compared to Class I products.
- Investigational Device Exemption (IDE): If the device is classified as significant risk, applying for an Investigational Device Exemption (IDE) is crucial. This exemption permits the gathering of essential safety and effectiveness information during clinical studies, aiding the pathway to regulatory approval. Recent statistics indicate that the IDE application process has seen an increase in submissions, reflecting the growing innovation in the Medtech sector.
- Institutional Review Board (IRB) Approval: Securing IRB approval is vital to ensure that the study adheres to ethical standards and safeguards participant rights. The IRB assesses the study protocol, informed consent documents, and the overall risk-benefit ratio of the research, ensuring that participant welfare is prioritized.
- Compliance with Good Clinical Practice (GCP): Adhering to Good Clinical Practice guidelines is essential for maintaining the quality and integrity of study data. GCP compliance not only enhances the credibility of the research but also ensures that the findings are reliable and can withstand regulatory scrutiny.
- Reporting Requirements: It is imperative to be aware of and comply with the reporting requirements for adverse events and progress to regulatory bodies. Challenges in adverse event reporting, such as data quality, interoperability, and timeliness, must be addressed to ensure that all relevant information is communicated effectively.
In light of evolving regulatory frameworks, particularly in regions like LATAM, understanding the factors in designing device trials is more critical than ever, especially as proactive measures are taken to harmonize regulations with innovation. As Alan Rencher noted, "There is an urgent need to get advanced technologies into the healthcare ecosystem, but all products must first get regulatory approval."
With over 20 years of experience in the Medtech sector, bioaccess® provides extensive management services for research activities, including feasibility assessments, site selection, compliance evaluations, setup, import permits, project oversight, and reporting, ensuring that all elements of the research process are carefully managed. Case studies, such as the partnership between bioaccess and Caribbean Health Group to establish Barranquilla as a premier location for medical research in Latin America, backed by Colombia's Minister of Health, showcase effective navigation of these regulatory environments. Moreover, the 2025 Medical Device Industry Report acts as a beneficial resource for the intended audience, providing further perspectives on medical studies and strategies for addressing industry challenges.
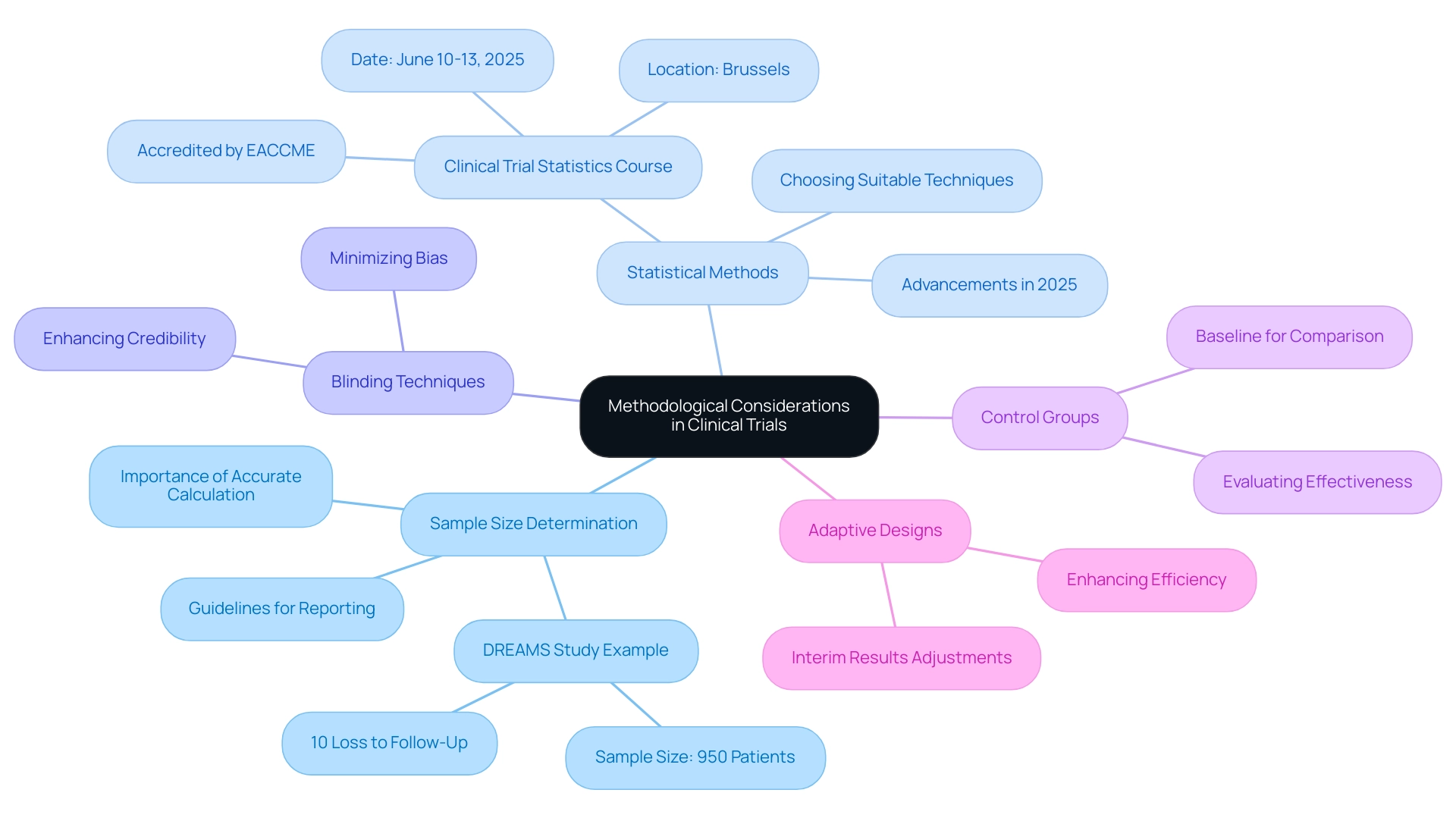
Methodological Considerations in Clinical Trials
Key methodological considerations in designing user-centered device trials encompass several critical elements, particularly within the context of navigating the Latin American Medtech landscape:
- Sample Size Determination: Accurately calculating the sample size is paramount to ensure the statistical power and validity of the trial results. For example, in the DREAMS research, a sample size of 950 patients was established, accounting for a 10% loss to follow-up, which demonstrates the significance of thorough planning in clinical investigations. Furthermore, guidelines for reporting research projects mandate that all aspects of sample size calculation should be included in the research manuscript to assess potential biases.
- Statistical Methods: Choosing suitable statistical techniques for data analysis is crucial for interpreting study outcomes effectively. As Jan Bogaerts, Director of Methodology Direction at EORTC Headquarters, emphasizes, "The design of a biomarker-based study is practical and requires a solid understanding of statistical methods." In 2025, advancements in statistical methods will continue to influence the environment of medical studies, allowing for more accurate assessments of healthcare products. Additionally, the Clinical Trial Statistics for Non-Statisticians course, scheduled for June 10 to June 13, 2025, in Brussels, aims to enhance the knowledge and skills of professionals in clinical trial statistics, further supporting the need for ongoing education in this area.
- Blinding Techniques: Implementing blinding strategies is crucial to minimize bias in outcome assessments. This practice enhances the credibility of results, ensuring that the findings reflect the true efficacy of the instrument rather than external influences.
- Control Groups: The use of control groups provides a necessary baseline for comparison, which is vital for evaluating the effectiveness of the medical instrument. This methodological approach allows researchers to draw more reliable conclusions about the device's performance.
- Adaptive Designs: Considering adaptive study designs can significantly enhance the efficiency and relevance of medical research. These designs permit alterations based on interim results, facilitating a more adaptive approach to management and enhancing the overall research process.
Integrating these strategies not only enhances the structure of medical studies but also addresses the factors in designing device trials that conform to the changing standards and expectations in the area of medical technology research. Moreover, utilizing the knowledge of bioaccess® in overseeing medical studies, including Early-Feasibility Studies, First-In-Human Studies, and Post-Market Follow-Up Studies, guarantees that companies can maneuver through the complexities of the Latin American market efficiently. Bioaccess® also provides extensive clinical research management services, including feasibility assessments, site selection, compliance evaluations, project setup, import permits, project oversight, and reporting, which are crucial for successful market entry in the region.
The Role of Early-Feasibility and Pilot Studies
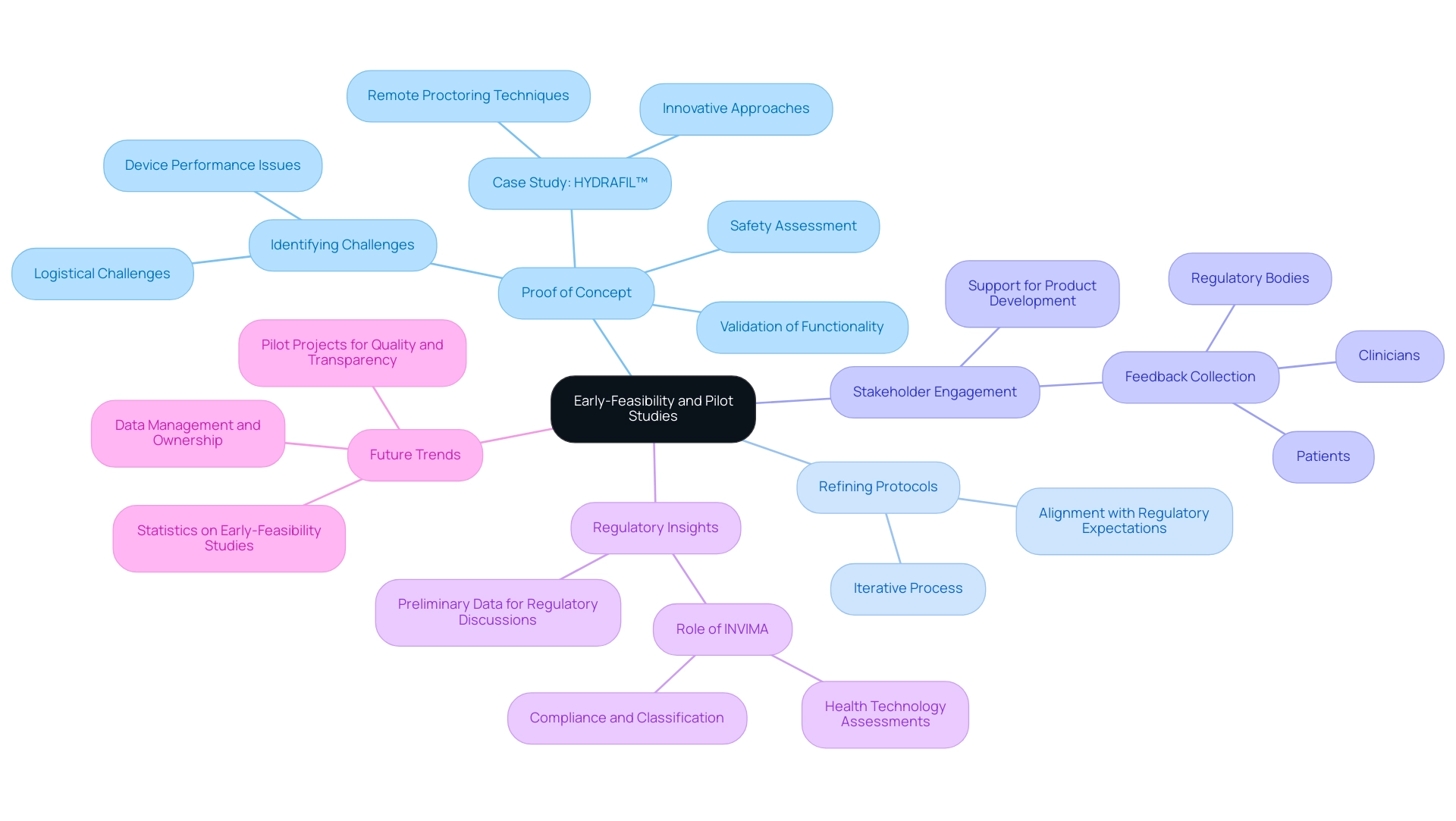
Early-feasibility and pilot studies are pivotal in the development of medical devices, serving multiple essential functions:
- Proof of Concept: These studies validate a device's functionality and safety within a small cohort before advancing to larger trials. This initial validation is critical for establishing confidence in the potential impact on patient care. Identifying challenges is crucial, as initial feasibility assessments help reveal possible obstacles related to the factors in designing device trials or device performance. For instance, ReGelTec's recent early feasibility assessment on HYDRAFIL™ for treating chronic low back pain in Colombia demonstrated how remote proctoring and innovative techniques can address logistical challenges, thereby enhancing the likelihood of success in subsequent phases.
- Refining Protocols: Insights gained from pilot experiments allow for the refinement of clinical protocols, which are key factors in designing device trials, leading to improved designs for larger trials. This iterative process ensures that the research is well-structured and aligned with regulatory expectations.
- Stakeholder Engagement: Engaging with stakeholders early in the development process is vital. Collecting feedback from clinicians, patients, and regulatory bodies encourages support for the product and can inform its development based on real-world insights.
- Regulatory Insights: Early-feasibility assessments provide preliminary data that can inform regulatory discussions and submissions. This data is increasingly important as regulatory bodies, such as INVIMA in Colombia, emphasize the need for structured frameworks in health technology assessments. As a Level 4 health authority recognized by PAHO/WHO, INVIMA plays a crucial role in overseeing medical device compliance and classification.
In 2025, the landscape for early-feasibility assessments is expected to evolve further, with a growing emphasis on data management and ownership. Sponsors are increasingly looking to unify data management, indicating a shift towards greater control over research data. This trend underscores the significance of pilot projects, which not only validate concepts but also streamline the path to market by enhancing product quality and regulatory transparency.
Statistics indicate that early-feasibility studies are becoming a standard practice, with a notable rise in their use throughout the Medtech sector, leading to more effective evaluations and enhanced patient results. As noted by Pietro Calameo, "Eliminating one 20-minute task per visit across 130,000 visits avoids 43,000 hours of work. Cras can focus on what matters," highlighting the efficiency gains that structured frameworks can provide.
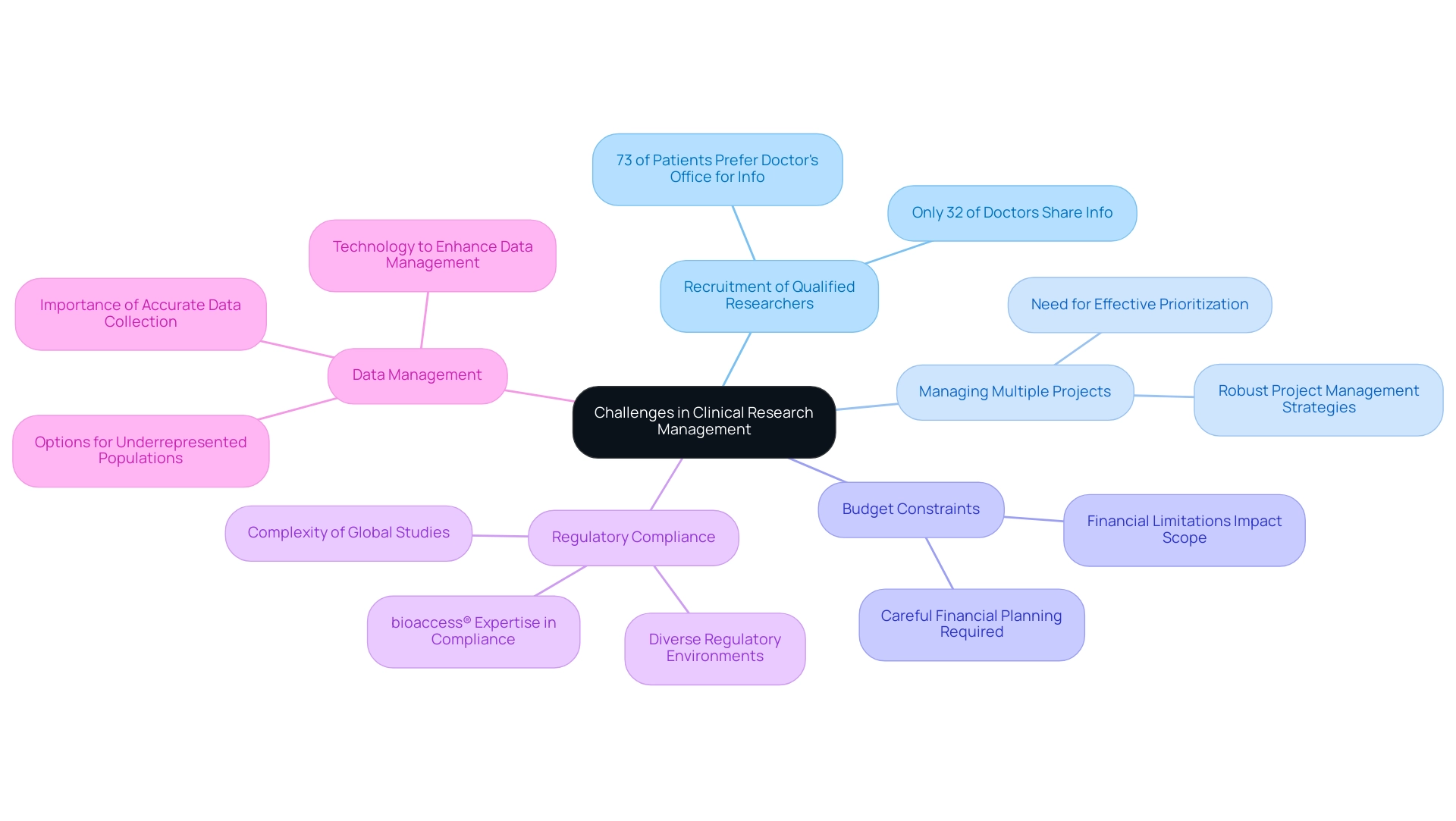
Challenges in Clinical Research Management
Common challenges in research management are multifaceted and can significantly affect the success of studies. Key issues include:
-
Recruitment of Qualified Researchers: The search for skilled personnel remains a critical hurdle. In 2025, the landscape of medical research is evolving, yet the recruitment of qualified researchers continues to be a challenge. This difficulty not only impacts the quality of evaluations but also the timelines for introducing innovative medical devices to market. Significantly, 73% of patients prefer to learn about clinical research opportunities from their doctor's office, yet only 32% indicated that their doctors had shared information about studies with them, highlighting a substantial gap in communication that impacts recruitment.
-
Managing Multiple Projects: The ability to balance multiple endeavors simultaneously is essential. Effective prioritization and resource allocation are crucial for ensuring that each project receives the attention it requires. As the number of attempts increases, so does the complexity of managing them, necessitating robust project management strategies. bioaccess® provides comprehensive clinical study management services, including feasibility studies, site selection, and project management, to streamline this process.
-
Budget Constraints: Financial limitations can severely restrict the scope and resources available for experiments. In an environment where funding is often limited, careful financial planning becomes essential to ensure that studies can proceed without compromising quality or outcomes.
-
Regulatory Compliance: Navigating the intricate web of regulatory requirements is a significant challenge. The complexity of global studies is increasing, as sponsors must contend with diverse regulatory environments across international markets. bioaccess® specializes in ensuring compliance with local regulations, including those set by INVIMA, the Colombia National Food and Drug Surveillance Institute, which plays a crucial role in medical device oversight. With over 20 years of experience in Medtech, bioaccess® is well-equipped to mitigate the challenges posed by regulatory disparities and cultural differences, ultimately enhancing patient enrollment and retention.
-
Data Management: Accurate and timely data collection and analysis are crucial for success. With the rise of technology in clinical research, there is an opportunity to enhance data management processes. For example, using technology to decrease site visits may enhance enrollment, especially for hard-to-reach patient populations. In 2025, underrepresented study populations will have more options for onboarding and visitations, which can facilitate better recruitment outcomes.
These challenges highlight the need for innovative recruitment strategies and effective management practices, which are key factors in designing device trials in research. As Bree Burks, Vice President of Site Strategy at Veeva, notes, "Sponsors will step up to solve site capacity issues," highlighting the industry's commitment to overcoming these obstacles. Tackling these obstacles is crucial for progressing medical equipment and ensuring that clinical studies are carried out efficiently and effectively, aiding in job creation and economic development in local communities.
Best Practices for Successful Device Trials
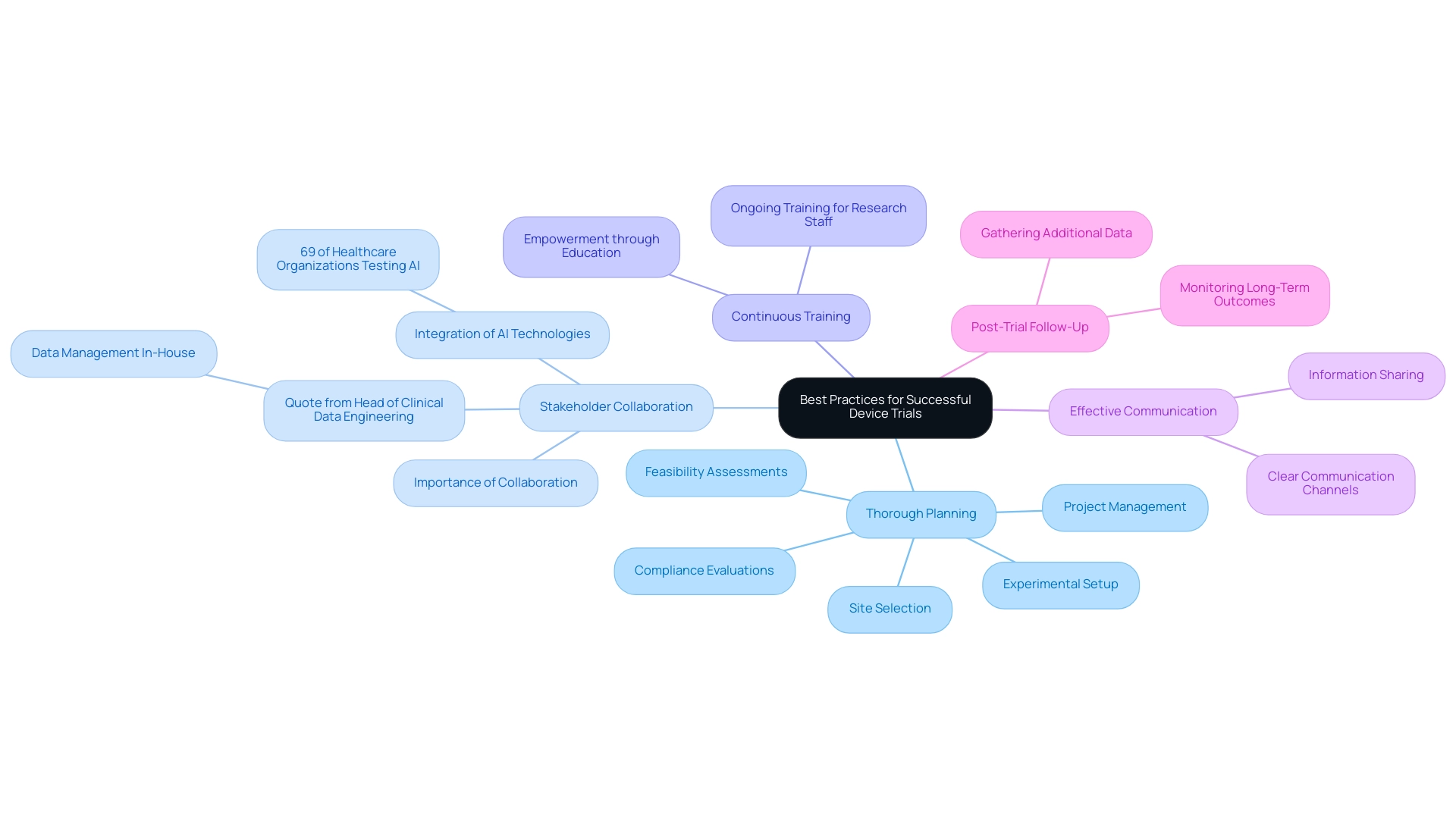
Best practices for conducting successful device trials encompass several critical strategies:
-
Thorough Planning: Investing time in meticulous planning is essential to anticipate potential challenges and streamline processes. A well-structured plan is crucial as one of the factors in designing device trials, enhancing efficiency and mitigating risks associated with unforeseen obstacles. bioaccess® offers comprehensive management services, including feasibility assessments, site selection, compliance evaluations, experimental setup, import permits, project management, and reporting, which are essential for effective planning in the Latin American Medtech landscape.
-
Stakeholder Collaboration: Fostering collaboration among all stakeholders—including sponsors, investigators, and regulatory bodies—is vital. Effective collaboration ensures that all parties are aligned with the trial's objectives and can contribute their expertise, ultimately leading to improved outcomes. As highlighted by the Head of Clinical Data Engineering, "Traditionally, data management was outsourced to our CRO vendor partners. Part of the initiative is to bring all our research in-house so that our internal teams can start working on it. They can be more hands-on, and we operationalize studies in-house and we are able to take control of our data, and we deliver for our patients with high quality." This shift highlights the significance of effective communication and collaboration in clinical studies. Recent statistics indicate that 69% of healthcare organizations are actively testing or adopting artificial intelligence technologies, underscoring the growing trend of integrating advanced solutions to enhance stakeholder engagement and operational efficiency.
-
Continuous Training: Providing ongoing training for research staff is crucial to ensure they remain well-versed in protocols and best practices. This commitment to education not only empowers the team but also improves the overall quality of the study, particularly in understanding the factors in designing device trials when navigating the complexities of the Latin American market.
-
Effective Communication: Maintaining clear communication channels among team members facilitates information sharing and problem-solving. Open lines of communication are essential for addressing issues promptly and ensuring that all stakeholders are informed of developments throughout the process.
-
Post-Trial Follow-Up: Implementing a robust post-trial follow-up process is necessary to monitor long-term outcomes and gather additional data. This step is essential for evaluating the apparatus's performance in practical environments and for guiding future research.
Incorporating these best practices can significantly improve the success of medical equipment studies by addressing the factors in designing device trials, ensuring that they meet regulatory standards and ultimately benefit patient care. The case study titled "Site-Centric Approaches in Project Startup" highlights the necessity for participant involvement and efficient site oversight, reinforcing the significance of careful planning and stakeholder cooperation in project assessments. Moreover, by 2020, more than 89% of hospitals had implemented EHR systems for in or outpatients, emphasizing the technological progress in healthcare that pertains to the integration of AI and other technologies in medical studies.
Future Trends in Medical Device Clinical Trials
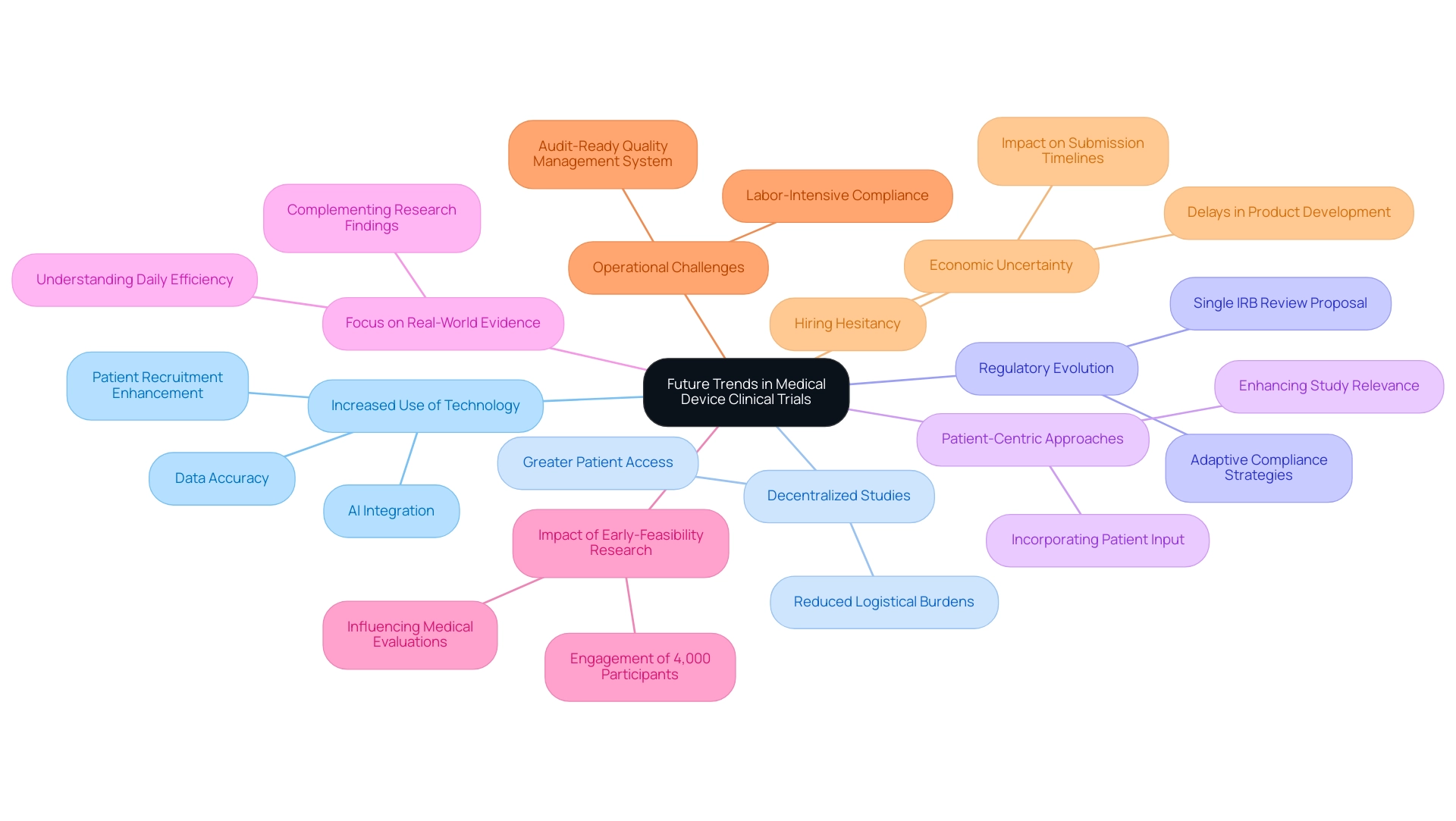
Factors in designing device trials are poised to significantly reshape the landscape of future trends in medical device clinical studies, driven by technological advancements and evolving regulatory frameworks. Key developments include:
-
Increased Use of Technology: The integration of artificial intelligence (AI) and machine learning is set to revolutionize data analysis and patient recruitment processes. As of 2025, these technologies are anticipated to streamline operations, enhance data accuracy, and improve participant engagement, ultimately leading to more efficient study outcomes.
-
Decentralized Studies: The movement towards decentralized and hybrid study models is gaining momentum, allowing for greater patient access and engagement. This approach not only facilitates participation from diverse populations but also reduces the logistical burdens associated with traditional study settings.
-
Regulatory Evolution: The regulatory landscape is continuously evolving, with recent proposals such as the FDA's mandate for single Institutional Review Board (IRB) reviews for FDA-regulated research. This shift aims to minimize duplicative reviews and expedite research initiation, emphasizing the factors in designing device trials that require researchers to adopt adaptive strategies to remain compliant and efficient.
-
Patient-Centric Approaches: There is an increasing emphasis on incorporating patient input and experience into research designs. By prioritizing the viewpoints of participants, researchers can enhance the relevance and applicability of study outcomes, which are crucial factors in designing device trials, ultimately leading to better product acceptance in the market.
-
Focus on Real-World Evidence: The utilization of real-world data is becoming increasingly vital in complementing research findings. This trend illustrates a wider industry movement towards understanding the factors in designing device trials, thus offering a more thorough perspective on the efficiency and safety of medical instruments in daily environments.
-
Impact of Early-Feasibility Research: The EFS program has involved over 4,000 participants from diverse areas since its inception, emphasizing the increasing significance of early-feasibility research in influencing upcoming medical evaluations. bioaccess® focuses on overseeing these investigations, guaranteeing a comprehensive method that complies with regulatory standards and customer requirements.
-
Operational Challenges: As mentioned by Matt McFarlane, the factors in designing device trials emphasize that sustaining an audit-ready quality management system (QMS) is a labor-intensive endeavor for both pre-commercial and commercialized organizations, highlighting the operational difficulties encountered in the changing environment of medical assessments. bioaccess® provides extensive management services for research studies, including compliance evaluations and project oversight, to assist in navigating these complexities.
-
Economic Uncertainty: Recent case studies indicate that economic factors have led to hesitancy among medical equipment companies, with 46% of larger firms halting new hiring. This uncertainty has resulted in delays in new product development and technology investments, impacting submission timelines and market entry strategies.
-
Data Management Trends: Sponsors are increasingly shifting towards insourced models for data management, seeking full ownership and transparency of their data, which reflects a broader trend in the industry. bioaccess® is committed to ensuring information security and client trust, addressing data protection concerns through established grievance procedures.
These trends underscore the importance of adapting to technological advancements and regulatory changes, ensuring that clinical trials not only meet current standards but also anticipate future needs in the medical device sector.
Conclusion
The landscape of medical device trials is experiencing a significant transformation, propelled by advancements in technology, evolving regulatory frameworks, and an increasing focus on patient-centric approaches. Foundational principles such as establishing clear objectives, robust data management, and ethical considerations remain essential to the success of clinical studies. The integration of artificial intelligence and machine learning is poised to enhance data accuracy and streamline processes, while decentralized trial models promise greater patient access and engagement.
Furthermore, the rising importance of early-feasibility studies underscores the necessity for thorough preliminary assessments that can inform regulatory discussions and refine trial designs. Addressing challenges such as recruitment, budget constraints, and regulatory compliance will be crucial for navigating the complexities of clinical research management. By adopting best practices and leveraging innovative methodologies, stakeholders can optimize their clinical trial strategies, ultimately leading to improved patient outcomes and successful market entry for new medical devices.
As the industry continues to evolve, staying informed about these trends and implementing effective trial designs will be vital for advancing medical technology. Organizations like bioaccess® are strategically positioned to guide companies through these challenges, offering tailored solutions that ensure compliance and enhance the overall quality of clinical trials. Embracing these changes will not only contribute to the success of individual trials but also foster a more efficient and effective medical device development process, benefiting patients and healthcare systems alike.
Frequently Asked Questions
What are the fundamental concepts in designing device trials?
The fundamental concepts include clear objectives, target population, measurable endpoints, randomization and control, and ethical considerations. These elements are essential for ensuring the success and integrity of research.
Why are clear objectives important in device trials?
Clear objectives guide the research's focus, align with regulatory expectations, and help manage risks to reduce the burden on study sites, as emphasized by the ICH E6 R2 guidelines.
How does identifying the target population affect device trials?
Identifying and characterizing the patient population ensures that the results are applicable to real-world scenarios, enhancing the relevance of study outcomes and ultimately improving patient care.
What role do endpoints play in device trials?
Clear and measurable endpoints are necessary to evaluate the success of the study, typically including safety and efficacy metrics essential for regulatory approval and market acceptance.
How does randomization and control contribute to the reliability of study results?
Randomization minimizes bias and enhances the reliability of results, while control groups allow for effective outcome comparisons, providing a clearer understanding of the device's impact.
What ethical considerations should be taken into account in device trials?
Adhering to ethical standards is crucial for protecting participants' rights and well-being, fostering trust, and aligning with the emphasis on ethical practices in clinical research.
What is the significance of protocol design in device trials?
A meticulously crafted protocol standardizes procedures and ensures consistency across multiple sites, enhancing clarity and aligning with the latest regulatory revisions.
Why is data integrity important in device trials?
Maintaining high data integrity is essential for guaranteeing the accuracy and reliability of data gathered during studies, which can significantly reduce errors and enhance overall results.
How does training and competence affect the quality of device trials?
Adequate training and competence among study personnel enhance study quality and foster a culture of compliance and excellence.
What is the role of monitoring and compliance in device trials?
Regular monitoring of study processes and adherence to regulatory requirements are vital for maintaining quality throughout the study, allowing for timely corrective actions when deviations occur.
How is risk management implemented in device trials?
Active recognition of potential risks and the formulation of effective mitigation strategies are crucial, often involving a cross-functional team approach to enhance communication and efficiency.
How do CTQ factors enhance the success of device trials?
Incorporating critical-to-quality (CTQ) factors streamlines processes and significantly increases the probability of successful results, making best practices essential for advancing medical devices effectively.

