Overview
The article delineates the comprehensive steps essential for planning medical device clinical trials, underscoring their pivotal role in evaluating safety, efficacy, and regulatory compliance prior to market introduction. It elaborates on the various types of trials, the critical importance of adhering to regulatory guidelines, and effective strategies for patient recruitment. These elements are indispensable for ensuring that new medical technologies satisfy both market demands and patient safety standards.
Introduction
In the ever-evolving landscape of medical technology, clinical trials for medical devices represent a critical checkpoint, ensuring the safety and efficacy of innovative solutions prior to their market introduction. These trials not only safeguard patient health but also serve as a guiding framework for manufacturers and regulatory bodies navigating the complex journey of device development.
From evaluating potential risks to fulfilling stringent regulatory requirements, a comprehensive understanding of the multifaceted nature of these trials is essential for all stakeholders involved. As the industry adapts to emerging challenges and opportunities, the significance of clinical trials becomes increasingly vital in shaping the future of healthcare technology.
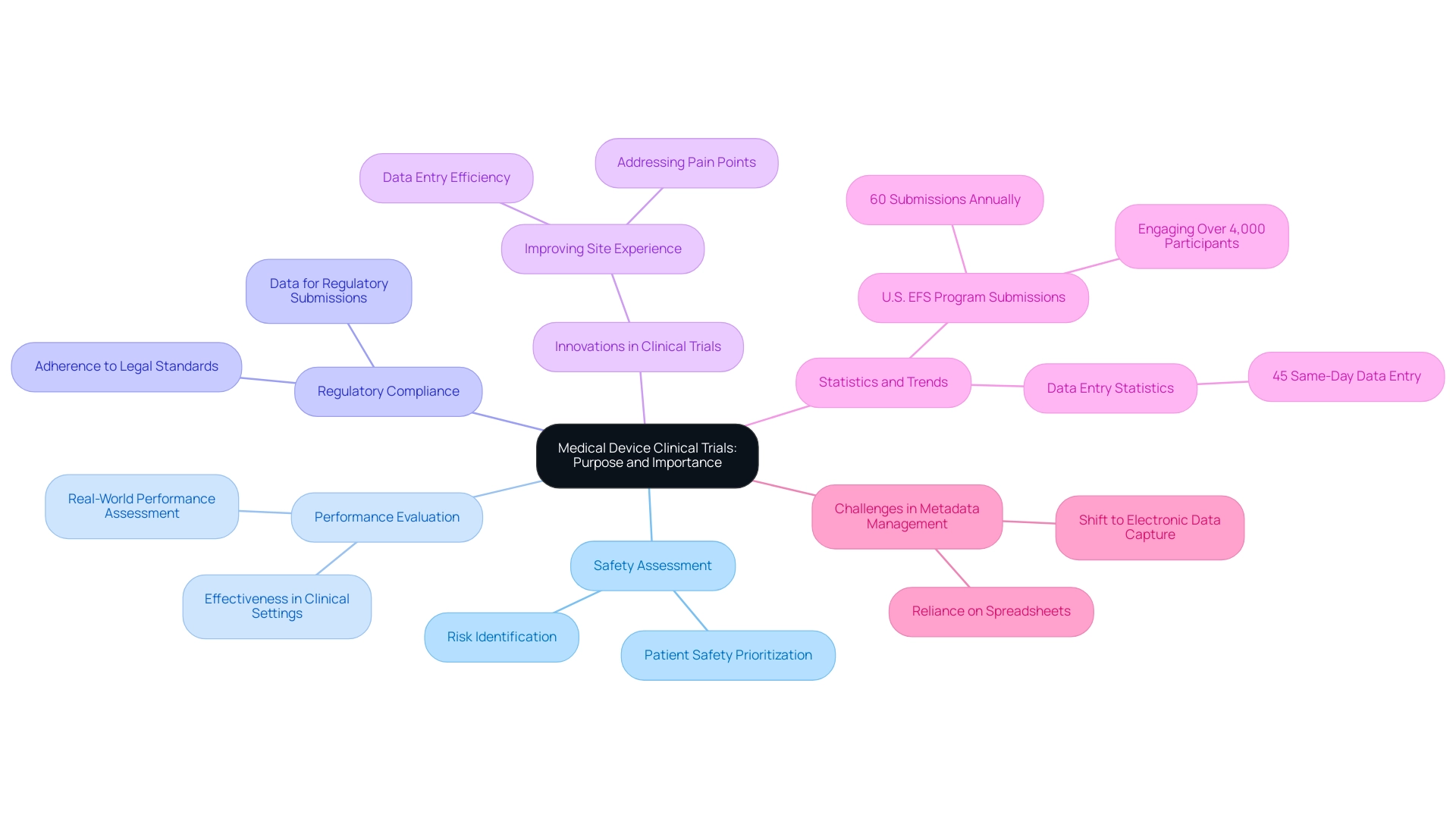
Understanding Medical Device Clinical Trials: Purpose and Importance
Planning medical device clinical trials is essential for evaluating the safety and effectiveness of innovative instruments prior to their market launch. These assessments are crucial not only for ensuring that devices function as intended but also for safeguarding patient well-being by identifying potential risks. For stakeholders—including manufacturers, regulatory bodies, and healthcare providers—planning medical device clinical trials is vital for understanding the significance of these evaluations, as it shapes the design and execution of studies that ultimately advance medical technology.
The multifaceted purposes of clinical trials for medical devices include:
- Safety Assessment: These trials are designed to uncover any potential risks associated with the device, ensuring that patient safety is prioritized.
- Performance Evaluation: Planning medical device clinical trials involves rigorously assessing whether the apparatus achieves its intended results, offering essential information on its performance in real-world scenarios.
- Regulatory Compliance: Planning medical device clinical trials produces the necessary data for regulatory submissions, confirming that devices adhere to legal standards before they can be commercialized.
bioaccess® specializes in comprehensive clinical study management services across Latin America, focusing on Early-Feasibility Studies (EFS), First-In-Human Studies (FIH), Pilot Studies, Pivotal Studies, and Post-Market Clinical Follow-Up Studies (PMCF). With more than 20 years of experience in Medtech, bioaccess® guarantees that each study is conducted with the utmost level of expertise and flexibility, addressing the unique challenges of the region.
Recent statistics underscore the significance of these assessments in 2025, with approximately 60 submissions supported annually by the U.S. Early Feasibility Study (EFS) program, engaging over 4,000 participants. This initiative reflects a growing commitment to adapt to the evolving needs of the industry, enhancing the landscape of medical device development.
Furthermore, the importance of safety and efficacy assessments in research studies cannot be overstated. For instance, a significant case study titled "Enhancing Site Experience in Research Studies" featuring Alcon highlights the impact of innovations aimed at improving site experiences in research studies. By addressing common pain points, such as data entry delays—where 45% of Alcon's data is entered on the same day as the visit date—Alcon has improved user-friendliness and streamlined operations, ultimately leading to better patient care outcomes.
As Vivienne van der Walle, Founder and Medical Director, aptly noted, "Anything that takes away time from patients is a pain point for a site, and anyone who resolves that is helping patient care."
In summary, planning medical device clinical trials while continuously enhancing research design and implementation is essential for the advancement of medical technologies. By prioritizing safety assessments, efficacy evaluations, and regulatory compliance, stakeholders can ensure that new technologies not only meet market demands but also contribute positively to patient health and well-being. Moreover, addressing challenges in scaling metadata management, particularly the reliance on spreadsheets, is crucial for improving the efficiency and effectiveness of medical research.
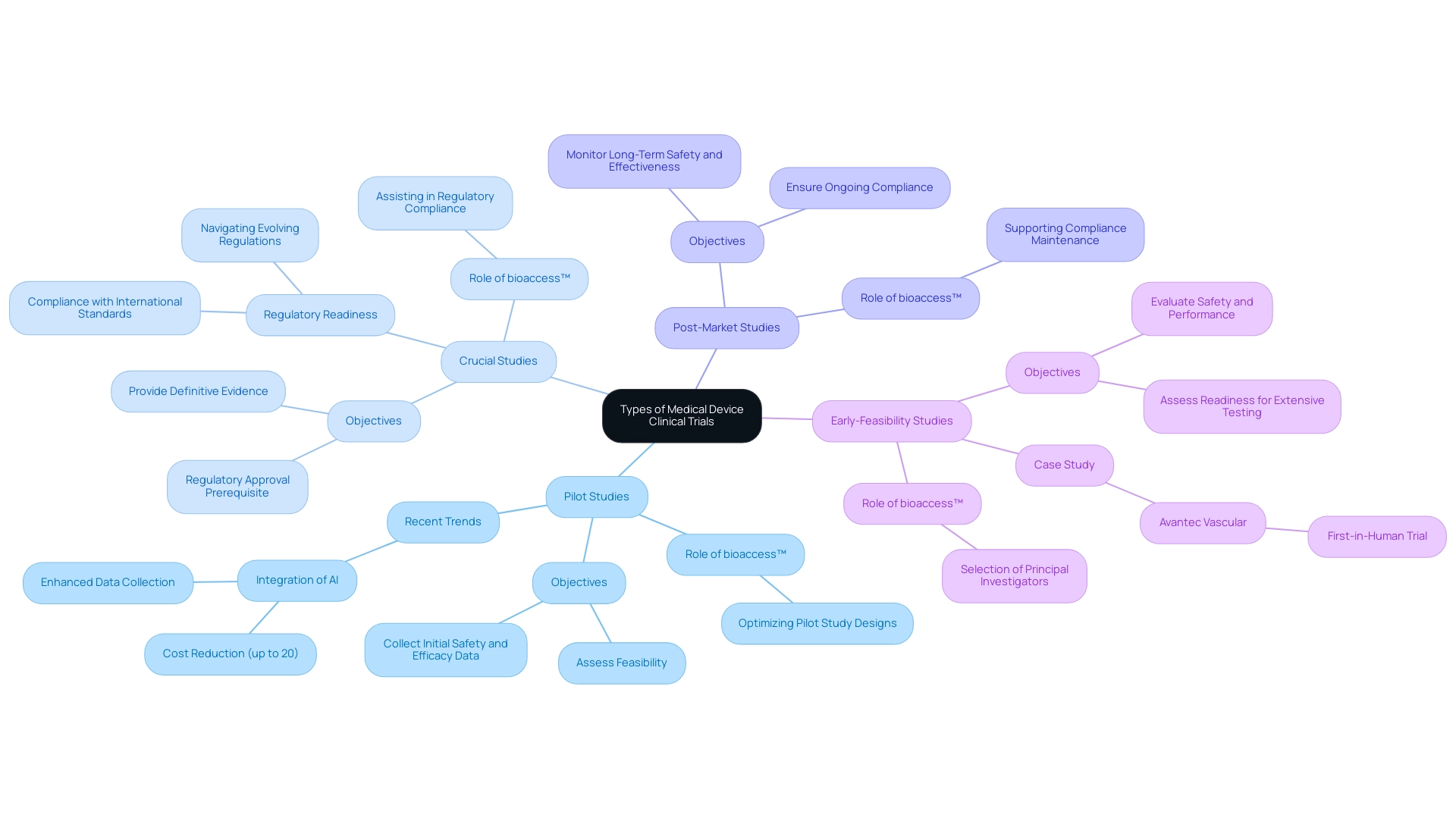
Types of Medical Device Clinical Trials: An Overview
Medical device clinical trials encompass various types, each tailored to specific objectives within the research and development process:
- Pilot Studies: These exploratory studies are crucial for assessing the feasibility of a medical device. They collect initial information on safety and efficacy, enabling researchers to recognize potential issues early in the development process. Recent trends indicate that pilot studies are increasingly incorporating artificial intelligence (AI) to enhance data collection and analysis, which can lead to cost reductions of up to 20%. This integration of AI not only streamlines processes but also enhances human efforts in clinical studies. bioaccess™ leverages its expertise to guide companies in optimizing pilot study designs.
- Crucial Studies: Larger in scale, crucial studies are designed to provide definitive evidence regarding a product's effectiveness and safety. These studies are often a prerequisite for regulatory approval, making them a critical step in the commercialization process. Experts highlight the significance of regulatory readiness in crucial evaluations, as evolving regulations require more comprehensive data and compliance with international standards. bioaccess™ assists clients in navigating these complexities, ensuring they remain compliant with FDA guidance and international regulations. As noted by Dipanwita Das, CEO & co-founder, "Last, but certainly not the least is regulatory preparedness. Regulations are getting more complex and more prescriptive and more demanding..."
- Post-Market Studies: After a device receives approval, post-market studies are conducted to monitor its long-term safety and effectiveness across a broader patient population. These studies are essential for ensuring ongoing compliance and addressing any emerging safety concerns. bioaccess™ supports companies in conducting these studies to maintain regulatory compliance.
- Early-Feasibility Studies: Conducted during the initial stages of development, these trials evaluate the safety and performance of a system in a small group of patients. They act as an essential step in assessing whether a tool is prepared for more extensive testing. For example, bioaccess™ has effectively assisted Avantec Vascular in their first-in-human trial of an innovative vascular tool in Latin America, illustrating the significance of expert guidance in early-feasibility studies. bioaccess™ also plays a key role in the selection of principal investigators for these studies.
The landscape of medical device studies is evolving, with a growing emphasis on simplifying site experiences and reducing patient burden. Clinical data leaders are actively exploring ways to streamline protocol designs by requesting less data and focusing on tangible patient benefits. Innovations in medical studies aim to enhance site experiences, reduce the burden of technology, and improve patient care.
This change is essential for enhancing research operations and ensuring that patient needs are prioritized. bioaccess™ is at the forefront of these innovations, adapting its services to meet the changing demands of the industry.
In summary, comprehending the different kinds of medical equipment research studies and their respective functions is crucial for planning medical device clinical trials and efficient implementation. As the industry keeps advancing, remaining knowledgeable about the latest developments and expert opinions will be essential for success in research.
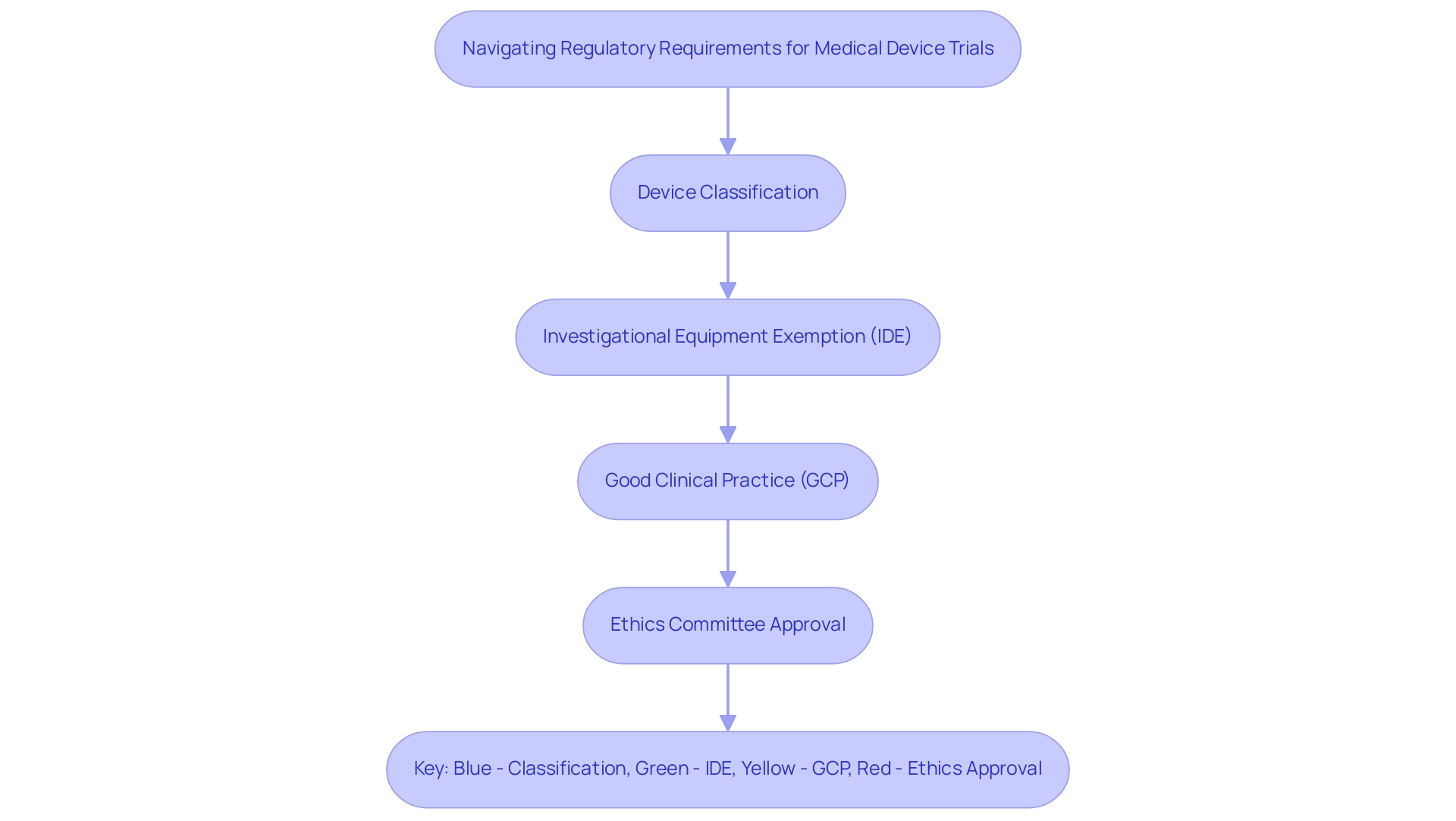
Navigating Regulatory Requirements for Medical Device Trials
A thorough understanding of the guidelines established by regulatory authorities such as the FDA and EMA is essential for planning medical device clinical trials and navigating the regulatory requirements. Key steps in this process include:
-
Device Classification: Accurately determining the classification of the device—Class I, II, or III—is crucial as it dictates the regulatory pathway and the level of scrutiny required during the approval process. For example, Class III instruments, which are generally high-risk, necessitate more comprehensive research to show safety and effectiveness.
-
Investigational Equipment Exemption (IDE): For higher-risk instruments, obtaining an IDE is crucial to carry out research studies. This exemption allows for the investigation of devices that may not yet have received full market approval, which is essential for planning medical device clinical trials to gather critical data on performance and safety in a clinical setting.
-
Good Clinical Practice (GCP): Following GCP guidelines is essential for planning medical device clinical trials to guarantee the protection of participants' rights and welfare throughout the study. Adhering to these standards not only improves the credibility of the results but also promotes trust among stakeholders.
-
Ethics Committee Approval: Obtaining authorization from an ethics committee or institutional review board (IRB) is a prerequisite before starting any clinical study. This step ensures that the study design is ethically sound and that participant safety is prioritized when planning medical device clinical trials.
In 2025, the landscape of regulatory requirements is evolving, with international harmonization efforts simplifying compliance for manufacturers engaged in planning medical device clinical trials across multiple regions. This trend is reflected in the increasing number of successful Investigational Device Exemption (IDE) applications, which have risen as companies focus on planning medical device clinical trials to adapt to these streamlined processes. For instance, bioaccess provides extensive services that encompass feasibility studies, site selection, compliance reviews, setup, import permits, project management, and reporting, which are vital for effectively navigating these regulatory landscapes.
Furthermore, it is essential for the investigator's brochure to include comprehensive instructions for installation, maintenance, and use of the apparatus, along with adherence to national legislation regarding labeling and instructions for use when planning medical device clinical trials. This requirement is essential as it directly affects regulatory compliance and the overall success of the study. As Nicole Latimer, CEO of Medrio, emphasizes, "Utilizing patient-reported outcomes in medical device studies is vital for shaping commercialization plans and ensuring that the devices meet the needs of patients."
Additionally, it is important to note that 46% of respondents from companies with more than 1,000 employees reported halting new hiring, indicating the current challenges in the industry. As the regulatory landscape keeps changing, planning medical device clinical trials will require remaining aware of the most recent FDA and EMA guidelines to ensure effective study design and implementation.
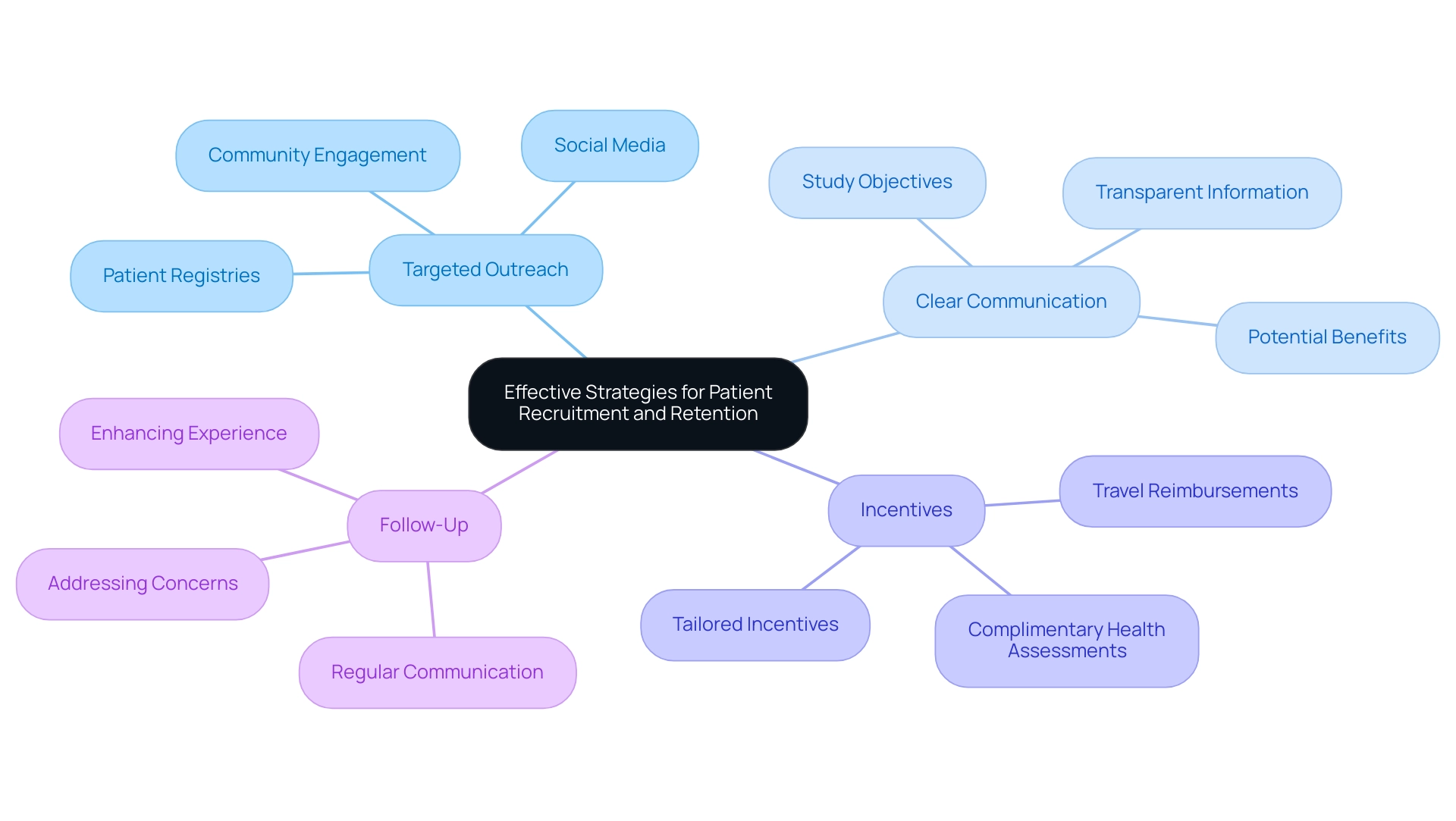
Effective Strategies for Patient Recruitment and Retention
Efficient patient recruitment and retention approaches are essential for the success of research studies, particularly in the evolving landscape of 2025. Here are several best practices to consider:
- Targeted Outreach: Leverage social media platforms, patient registries, and community engagement initiatives to effectively connect with potential participants. This approach not only broadens the reach but also fosters a sense of community and trust.
- Clear Communication: Providing transparent information regarding the study's objectives, procedures, and potential benefits is vital. This clarity can significantly enhance participant willingness to engage and remain involved throughout the study.
- Incentives: Offering incentives, such as travel reimbursements or complimentary health assessments, can motivate participation. These incentives should be tailored to address the specific needs and preferences of the target population, making participation more appealing.
- Follow-Up: Regular communication with participants is essential. Keeping them informed and addressing any concerns can enhance their experience and encourage continued involvement. This ongoing engagement is particularly important in maintaining high retention rates, projected to improve with more patient-centric strategies.
In 2025, the patient recruitment process is expected to be more efficient, equitable, and focused on patient needs. Creating recruitment strategies that prioritize patient preferences is crucial for building trust and increasing enrollment in research studies. For instance, case studies, such as the one titled "Patient-Centered Recruitment Strategies," have demonstrated that by offering flexible participation options and ensuring clear communication, sponsors can significantly enhance patient engagement and drive higher enrollment rates.
As emphasized in a blog entry from February 19, 2025, making medical studies more accessible and inclusive is essential for addressing challenges encountered by conventional models. Furthermore, as Ursula Türcke, Senior Director of Clinical Operations at FGK Clinical Research GmbH, noted, AstraZeneca's "no cure – no pay" model exemplifies a patient-centric approach that can foster trust and participation. As the sector progresses towards more inclusive and accessible studies, these strategies will be crucial in achieving successful outcomes.
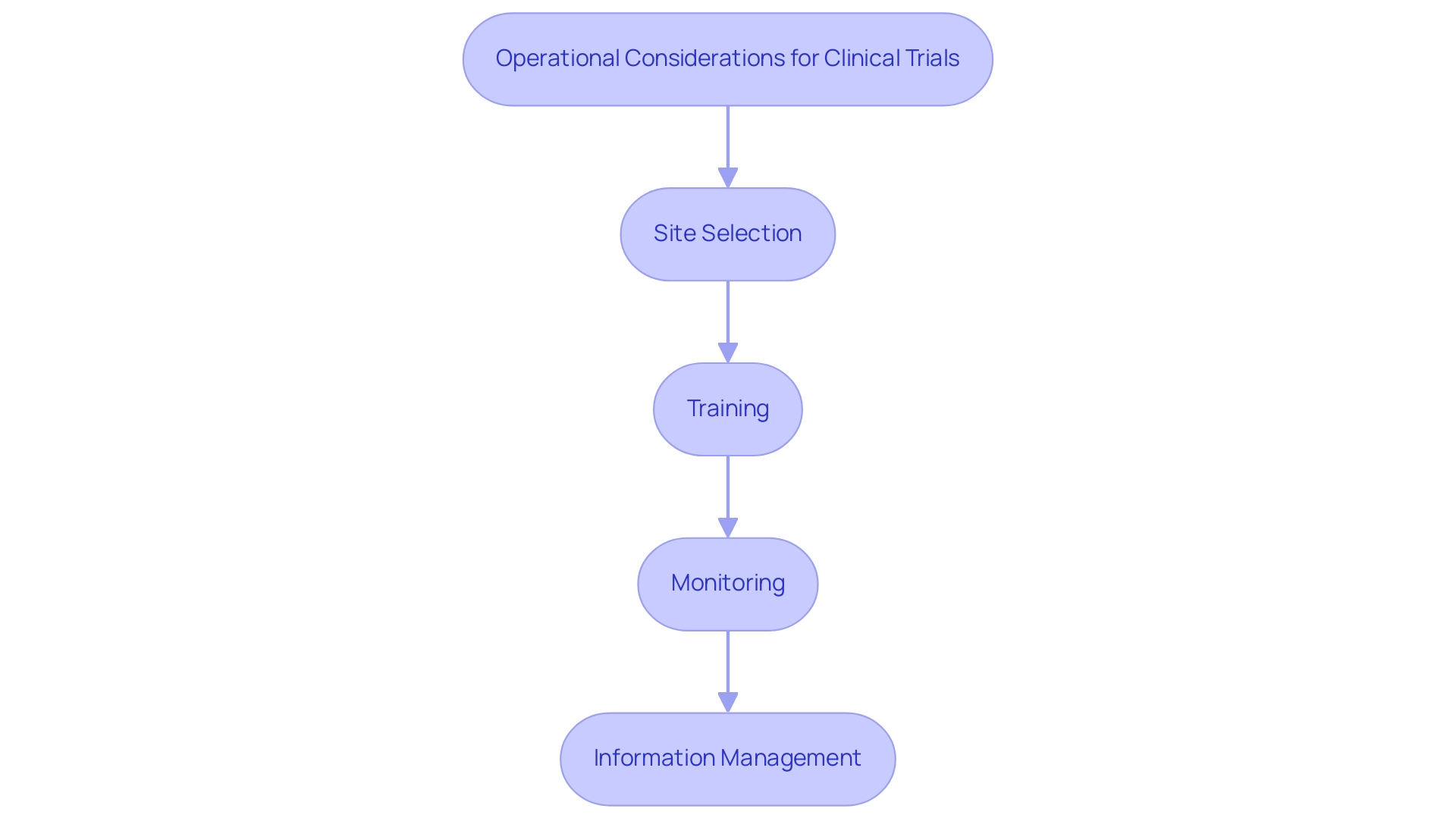
Operational Considerations: Conducting Clinical Trials Effectively
Conducting clinical trials effectively necessitates a meticulous approach to operational considerations that can significantly influence outcomes.
- Site Selection: Prioritize sites with a proven track record in clinical trials and a robust connection to the target patient population. In 2025, the criteria for site selection have evolved, emphasizing the need for sites that not only have experience but also demonstrate a commitment to diversity and inclusion in patient recruitment. This approach aligns with industry trends highlighted in the case study "2025 Trends in Clinical Studies," which discusses the importance of diverse participant demographics to enhance the generalizability of study results. Notably, bioaccess™ is actively collaborating with Caribbean Health Group to position Barranquilla as a leading destination for clinical studies in Latin America, supported by Colombia's Minister of Health.
- Training: It is crucial to ensure that all personnel involved in the study are thoroughly trained in both the study protocols and the regulatory landscape. As regulations become increasingly complex, comprehensive training programs are essential. For instance, organizations are adopting innovative training modules that incorporate real-world scenarios and regulatory updates to prepare staff effectively. As noted by Dipanwita Das, CEO & co-founder of bioaccess®, "Last, but certainly not the least is regulatory preparedness. Regulations are getting more complex and more prescriptive and more demanding..." This emphasizes that regulatory preparedness is key to a smooth commercialization process.
- Monitoring: Regular oversight of progress is vital to ensure adherence to protocols and to swiftly address any emerging issues. Implementing a structured monitoring plan can help maintain compliance and enhance the overall integrity of the trial. This proactive approach is supported by the integration of advanced information management systems that facilitate real-time oversight.
- Information Management: Leveraging electronic information capture systems is essential for streamlining information collection and ensuring information integrity. In 2025, the focus on data management has intensified, with an emphasis on utilizing real-world evidence to inform study design and patient recruitment strategies. This not only improves the efficiency of research studies but also aids in the creation of guidelines through standardized outcome measures across investigations, which is vital for future comparisons among interventions. Moreover, GlobalCare Clinical Studies has collaborated with bioaccess™ to improve ambulatory services in Colombia, achieving over 50% reduction in recruitment duration and 95% retention rates.
By following these best practices, research teams can enhance their processes, ultimately resulting in more effective and efficient studies that contribute to the progress of medical technologies. With over 15 years of experience in the Medtech sector, bioaccess® is well-positioned to guide organizations through these complexities. Additionally, insights from the LATAM Medtech Leaders Podcast highlight the importance of understanding local market dynamics and fostering relationships with local stakeholders to navigate the unique challenges of the Latin American Medtech landscape.
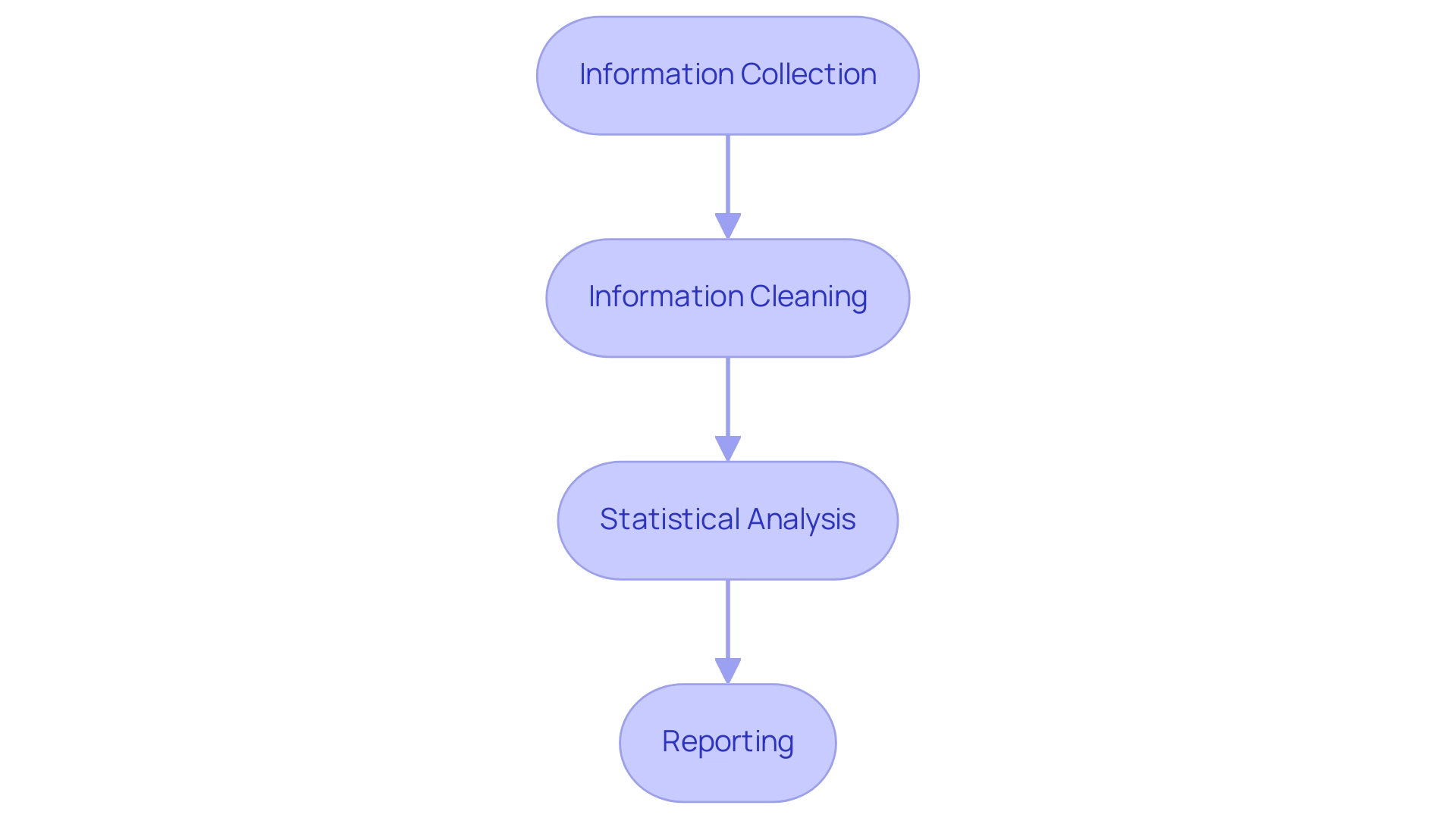
Data Management and Analysis in Medical Device Trials
Planning medical device clinical trials necessitates efficient information management and examination, which are vital for the success of these studies, influencing both the quality of results and regulatory adherence. A systematic approach to information management can significantly enhance the reliability of experimental outcomes, particularly within the context of the comprehensive research management services provided by bioaccess®.
-
Information Collection: The implementation of standardized forms and electronic information capture systems is crucial for ensuring accurate and consistent information collection. This strategy minimizes variability and bolsters the integrity of the information gathered during trials, aligning seamlessly with bioaccess®'s dedication to high-quality clinical research.
-
Information Cleaning: Regular reviews and cleaning processes are imperative. Identifying and rectifying errors prior to analysis not only improves quality but also guarantees that the findings are grounded in reliable information, which is essential for making informed decisions.
-
Statistical Analysis: The choice of statistical techniques is critical to the examination of trial information. Utilizing appropriate techniques that correspond with the study's objectives enables meaningful interpretations of the results. For example, methods such as regression analysis, survival analysis, and ANOVA are frequently employed to assess the efficacy and safety of medical instruments. Current trends reveal an increasing focus on advanced statistical techniques to enhance insights, reflecting the industry's transition towards more sophisticated analytical frameworks.
-
Reporting: Comprehensive reporting is vital for summarizing findings and providing insights into the device's safety and efficacy. Reports should not only present data but also contextualize results within the framework of regulatory standards and medical relevance, particularly important in Latin America, where local regulatory requirements, such as those from INVIMA, must be thoroughly understood.
The trend towards consolidating information management in-house is transforming the process of planning medical device clinical trials. As articulated by the Head of Clinical Information Engineering, 'Traditionally, information management was outsourced to our CRO vendor partners.' This initiative aims to bring all studies in-house, enabling internal teams to take a more hands-on approach.
By managing studies internally, we enhance our ability to oversee information, thereby providing high-quality services for our patients. By managing their information effectively, sponsors can improve operational efficiency and information quality, ultimately leading to better patient outcomes. This shift corresponds with expert opinions emphasizing the importance of robust information management practices in medical equipment evaluations, particularly in the context of planning medical device clinical trials in Latin America, where understanding local regulatory standards is crucial. Planning medical device clinical trials while adhering to Good Clinical Practice (GCP) and ISO 14155:2020 guidelines further ensures participant safety and information integrity, reinforcing our commitment to high-quality clinical research.
The conclusion of the case study titled 'Best Practices for Medical Equipment Trials' underscores the importance of meticulous planning in medical device clinical trials to ensure participant safety, information integrity, and regulatory compliance.
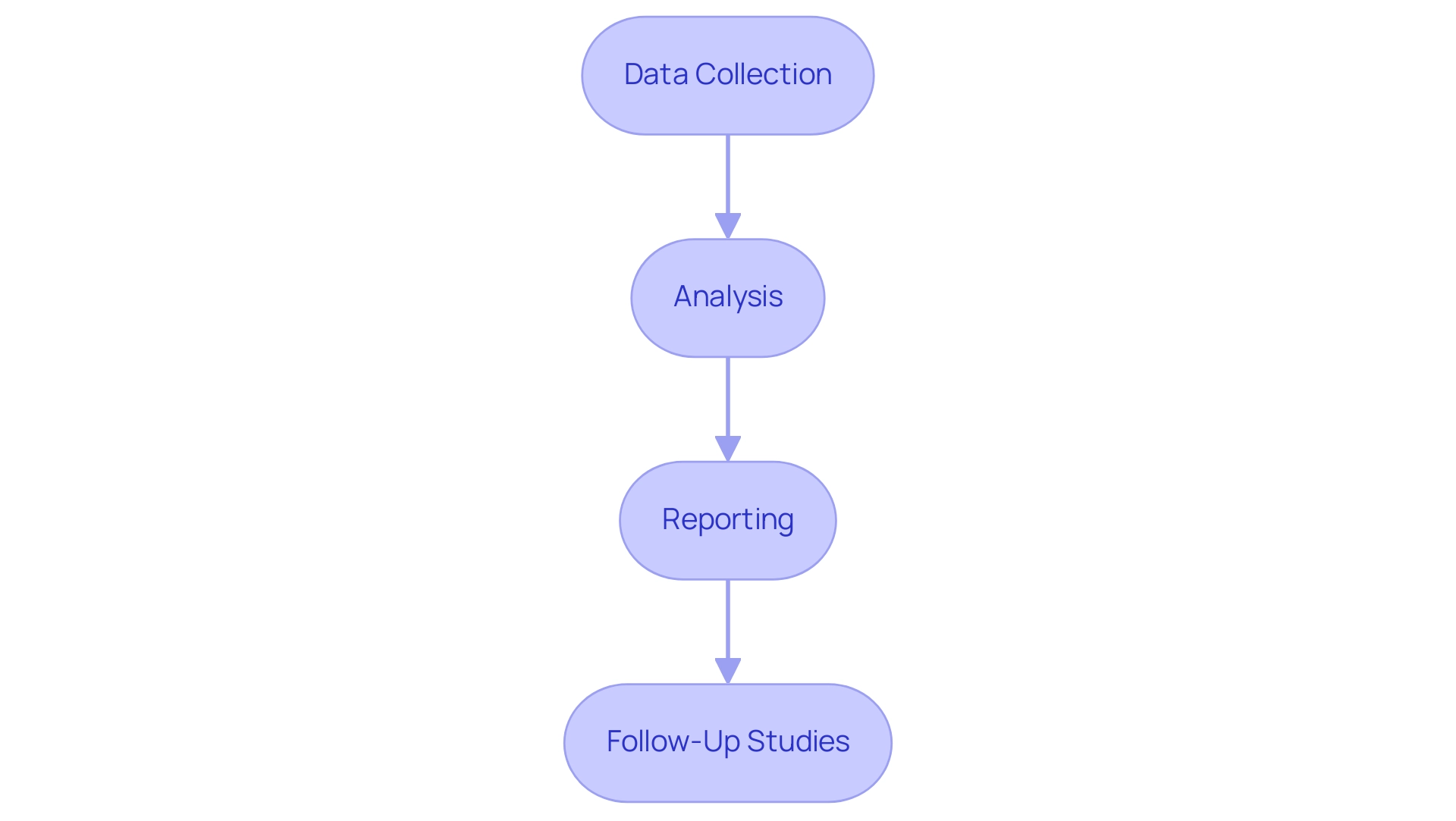
Post-Market Surveillance: Ensuring Long-Term Safety and Efficacy
Post-market surveillance stands as a crucial element in the medical product lifecycle, playing a pivotal role in ensuring ongoing safety and efficacy. This process encompasses several critical components:
- Data Collection: Continuously gathering data on device performance and adverse events from users and healthcare providers is vital. Efficient information gathering techniques, including surveys, user feedback forms, and electronic health records, provide a comprehensive perspective on the system's real-world performance.
- Analysis: Regular examination of post-market information is essential for identifying trends and potential safety issues. Recent statistics reveal that technical success rates for embolization coils have reached impressive levels: 95.4% for Nester, 94.0% for Tornado, and 98.6% for MReye coils. This data not only demonstrates the effectiveness of these tools but also highlights the significance of continuous monitoring to uphold high safety standards.
- Reporting: Findings from post-market analyses must be reported to regulatory authorities as required, ensuring transparency and compliance with safety regulations. This reporting is crucial for maintaining trust with stakeholders and the public, as it reflects a commitment to the safety of the equipment.
- Follow-Up Studies: Conducting follow-up studies is necessary to gather additional data on long-term safety and effectiveness. These studies yield insights into the apparatus's performance over time, aiding in the identification of any emerging safety concerns. Manufacturers are required to establish a post-market surveillance system that systematically collects and evaluates feedback on product performance and safety, ensuring a proactive approach to risk management throughout the product's lifecycle. As Michael E. Matheny, MD, MS, MPH, observes, "The evolving nature of many LLMs through continuous learning challenges the robust performance and sustainability of applications based on such models," underscoring the need for ongoing vigilance in monitoring performance.
In 2025, the landscape of post-market surveillance is evolving, with an increasing emphasis on long-term safety monitoring. Expert opinions stress the necessity of robust post-market systems to ensure that medical products consistently meet safety standards. The incorporation of real-world data will be essential for supporting the long-term effectiveness of medical instruments, ultimately enhancing patient safety and reliability.
At bioaccess®, our expertise in managing post-market research follow-up studies, combined with extensive experience in Early-Feasibility Studies (EFS), First-In-Human Studies (FIH), Pilot Studies, and Pivotal Studies, positions us to effectively support your needs in this critical area. Moreover, we recognize the significance of regulatory oversight, including the role of INVIMA as a Level 4 health authority, in upholding the highest standards of safety and efficacy in medical products.
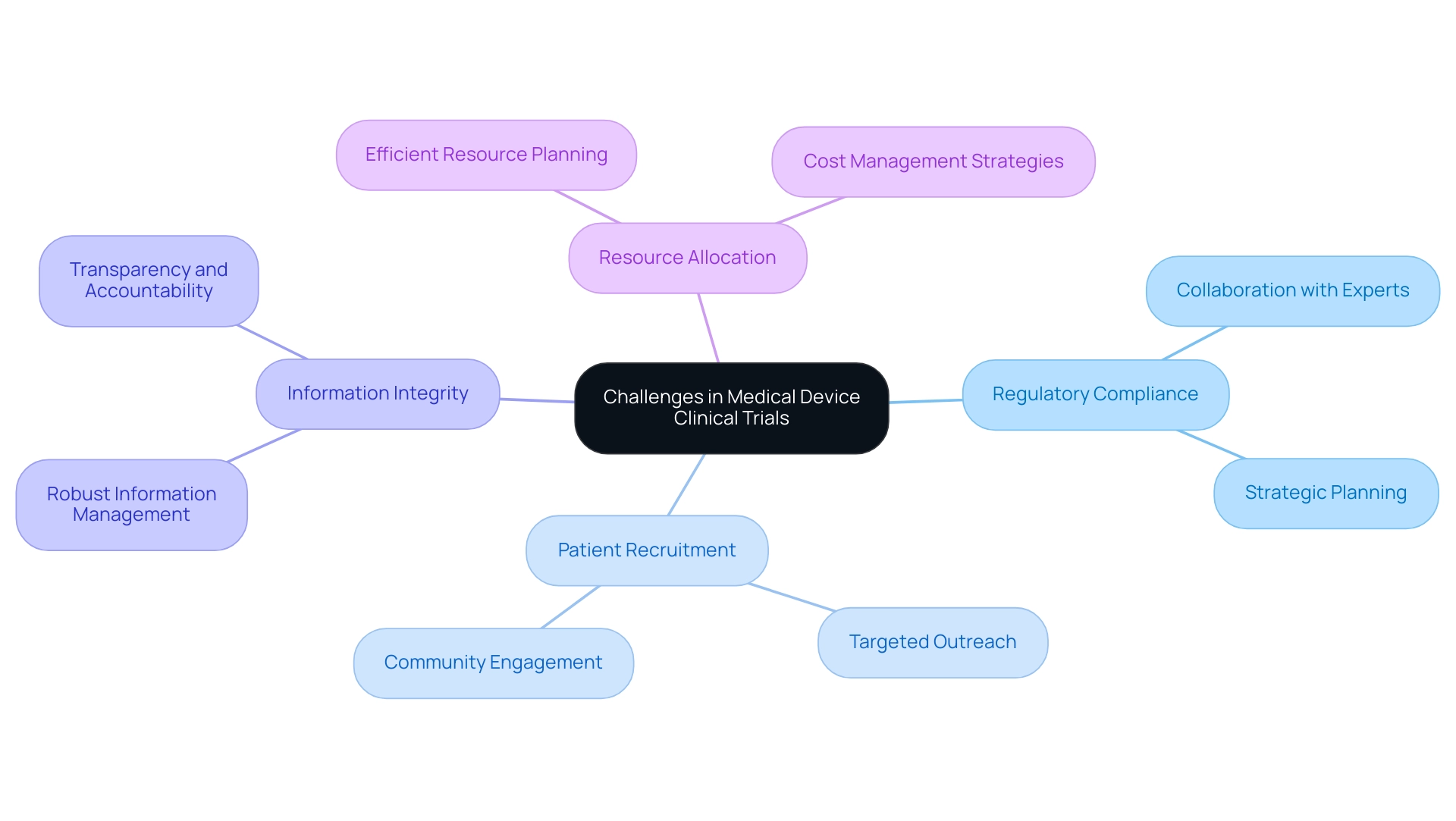
Challenges in Medical Device Clinical Trials and How to Overcome Them
Medical device clinical trials face a myriad of challenges that can significantly impact their success rates:
-
Regulatory Compliance: The landscape of medical device regulations is intricate and perpetually evolving. Staying abreast of these changes is vital for success throughout the process. Collaborating with regulatory experts, such as Katherine Ruiz, who specializes in Regulatory Affairs for medical devices and in vitro diagnostics in Colombia, can offer invaluable guidance, assisting sponsors in navigating the complexities of compliance and circumventing costly delays. As Kevin Coker, Innovation Strategist and Head of MedTech Development at MD Anderson Cancer Center, emphasizes, "Conducting tests across various countries sounds great but navigating different regulations, cultures, and standards is no small feat." This underscores the necessity for strategic planning and local insight, particularly when planning medical device clinical trials, given the anticipated regulatory differences that complicate global studies.
-
Patient Recruitment: Enrolling a diverse patient population is crucial for the validity of clinical studies. However, many studies encounter difficulties in this area, leading to elevated dropout rates that can undermine results. Statistics reveal that high dropout rates in medical device studies can significantly affect the validity of findings. Implementing targeted outreach strategies, such as community engagement and partnerships with local healthcare providers, can bolster recruitment efforts. Successful case studies, including those from Global Care Clinical Trials in partnership with bioaccess®, demonstrate that tailored recruitment campaigns can markedly enhance participant diversity and retention, ultimately resulting in more comprehensive outcomes.
-
Information Integrity: Safeguarding information integrity is paramount in clinical trials. Robust information management practices, including regular audits and real-time monitoring, can mitigate risks associated with inaccuracies. Cultivating a culture of transparency and accountability within the research team further fortifies data integrity, ensuring that results are both reliable and credible.
-
Resource Allocation: Limited resources frequently challenge operations, making efficient resource allocation essential. Careful planning and prioritization of tasks can enhance operational efficiency. For example, engaging project management consultants who specialize in cost management can yield substantial savings. A case study on cost management in medical equipment evaluations illustrates how these experts develop detailed project timelines, outsource tasks to cost-effective vendors, and continuously monitor evaluation progress to avert budget overruns, thereby ensuring that evaluations stay on track and within budget.
By addressing these challenges with knowledgeable strategies and expert insights, research organizations can refine their designs and elevate the likelihood of successful outcomes in planning medical device clinical trials. With over 20 years of experience in Medtech, bioaccess® aims to accelerate the development of medical devices through their expertise and tailored approach, providing valuable solutions to these pressing challenges, including their commitment to positioning Barranquilla as a premier location for research studies in Latin America. Their comprehensive clinical trial management services encompass feasibility studies, compliance reviews, project management, and more, ensuring a thorough approach to navigating the complexities of clinical trials.
Conclusion
The intricate world of medical device clinical trials is essential for ensuring that innovative technologies are both safe and effective for patients. These trials play critical roles, including:
- Safety assessments
- Efficacy evaluations
- Regulatory compliance
By understanding the various types of trials—from pilot studies to post-market studies—stakeholders can navigate the complexities of medical device development and contribute to advancements in healthcare technology.
As the industry evolves, the importance of effective patient recruitment and retention strategies cannot be overstated. Engaging patients through clear communication and targeted outreach fosters trust and encourages participation, ultimately leading to more robust trial outcomes. Furthermore, operational considerations such as site selection, training, and data management are crucial for conducting efficient and successful trials.
The ongoing challenges faced in medical device clinical trials, including regulatory compliance and maintaining data integrity, require strategic solutions and expert guidance. By proactively addressing these issues, organizations can enhance their trial designs and better meet the needs of patients.
In summary, the future of medical device trials hinges on a collaborative approach that prioritizes patient safety, regulatory adherence, and innovative strategies. As the landscape continues to shift, fostering a deeper understanding of these trials will be vital for all stakeholders involved in advancing healthcare technology.
Frequently Asked Questions
Why is planning medical device clinical trials important?
Planning medical device clinical trials is essential for evaluating the safety and effectiveness of innovative instruments before their market launch. It ensures that devices function as intended and safeguards patient well-being by identifying potential risks.
What are the main purposes of clinical trials for medical devices?
The main purposes include: Safety Assessment: To uncover potential risks and prioritize patient safety. Performance Evaluation: To assess whether the device achieves its intended results in real-world scenarios. Regulatory Compliance: To produce necessary data for regulatory submissions, confirming adherence to legal standards.
What types of clinical studies does bioaccess® specialize in?
Bioaccess® specializes in Early-Feasibility Studies (EFS), First-In-Human Studies (FIH), Pilot Studies, Pivotal Studies, and Post-Market Clinical Follow-Up Studies (PMCF).
How does bioaccess® ensure quality in clinical studies?
With over 20 years of experience in Medtech, bioaccess® guarantees that each study is conducted with expertise and flexibility, addressing the unique challenges of the region.
What recent trends highlight the importance of medical device clinical trials?
In 2025, approximately 60 submissions supported by the U.S. Early Feasibility Study (EFS) program engaged over 4,000 participants, reflecting a growing commitment to adapt to the evolving needs of the industry.
What are the different types of medical device clinical studies?
The types include: Pilot Studies: Exploratory studies assessing feasibility and collecting initial safety and efficacy data. Crucial Studies: Larger studies providing definitive evidence for regulatory approval. Post-Market Studies: Conducted after approval to monitor long-term safety and effectiveness. Early-Feasibility Studies: Evaluating safety and performance in a small group of patients during initial development stages.
How are innovations impacting medical device studies?
Innovations aim to enhance site experiences, reduce patient burden, and streamline protocol designs by requesting less data and focusing on tangible patient benefits.
Why is regulatory compliance critical in medical device studies?
Regulatory compliance is crucial to ensure that devices meet legal standards before commercialization and to navigate the increasingly complex regulations requiring comprehensive data.

