Introduction
The development of medical devices is a complex journey that hinges on critical milestones, one of the most significant being the design freeze. This pivotal moment not only signifies that the design is finalized but also sets the stage for rigorous validation and regulatory compliance, particularly in the context of Colombia's health oversight by INVIMA.
As organizations strive to streamline their development processes while managing stakeholder expectations, the design freeze emerges as a strategic tool that minimizes rework and enhances resource allocation.
However, navigating this stage is fraught with challenges, including evolving requirements and compliance issues that can derail progress.
By understanding the intricacies of the design freeze and implementing effective strategies, teams can ensure that their medical devices meet regulatory standards and ultimately succeed in a competitive market.
Understanding the Concept of Design Freeze in Medical Devices
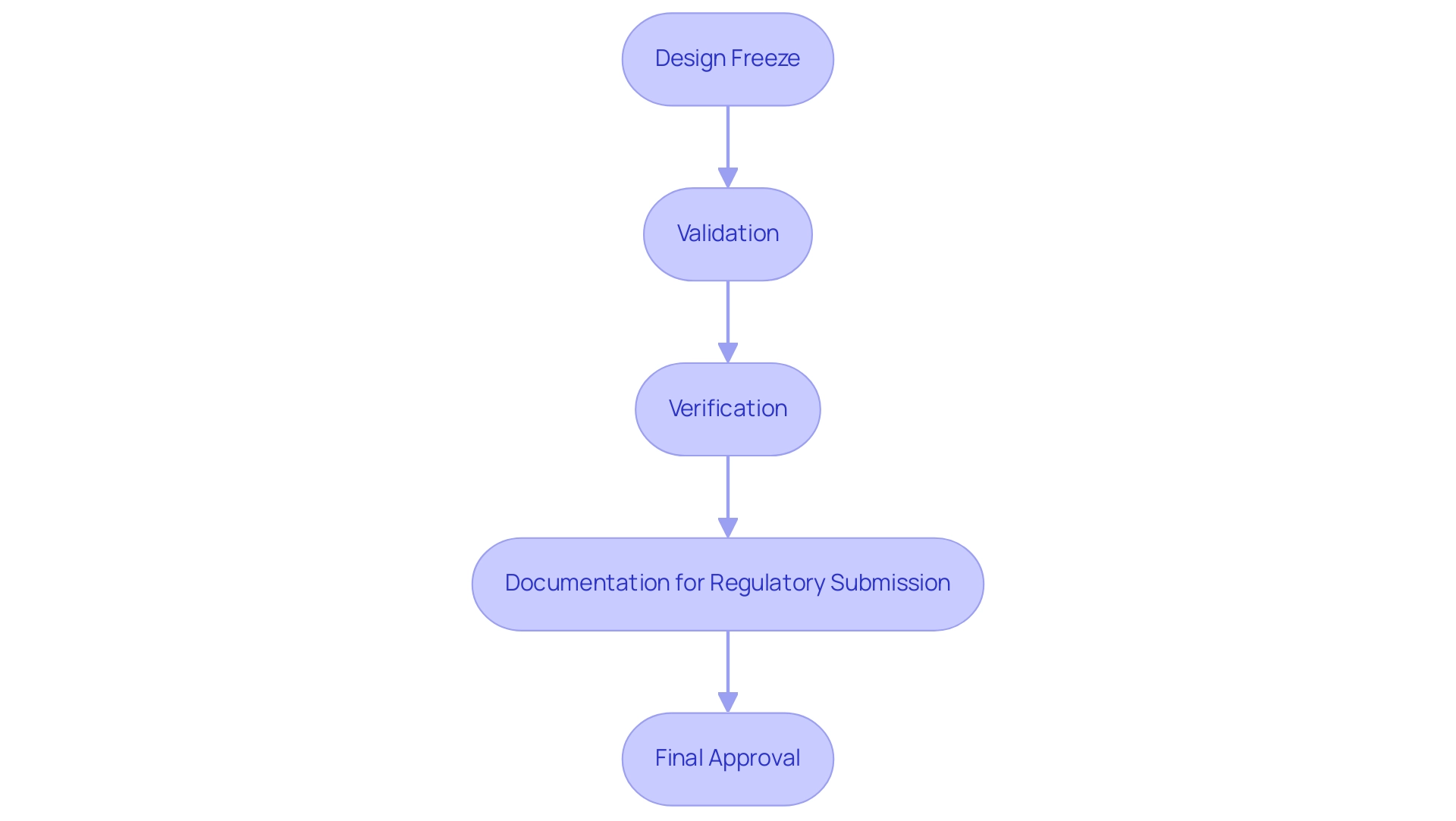
The design freeze medical device marks a crucial moment in the development process, indicating that the blueprint is considered final and any additional alterations necessitate significant justification. This milestone is essential for enabling teams to shift their efforts toward validation, verification, and compiling the necessary documentation for regulatory submissions, particularly under the oversight of INVIMA (Colombia National Food and Drug Surveillance Institute), which ensures compliance with health regulations in the country, especially as they approach the design freeze medical device phase. Implementing a design freeze medical device is essential for maintaining timelines and guaranteeing optimal resource distribution towards testing and quality assurance, instead of constantly altering the concept.
By adhering to this critical juncture, organizations can effectively manage stakeholder expectations while streamlining development processes. As emphasized by Arnd Huchzermeier, "We introduce, in addition to the familiar real option of abandonment, the option of corrective action that management can take during the project." This viewpoint highlights the strategic consequences of executing a layout halt.
Recent statistics suggest that clinical studies are linked to substantial planning, organization, and documentation efforts, resulting in considerably elevated costs, which further emphasizes the importance of a clearly defined project halt. Moreover, with INVIMA's classification as a Level 4 health authority, recent updates in compliance submissions for medical devices in 2024 stress the need for rigorous adherence to predefined protocols, especially in the context of the design freeze medical device acceptance criteria. Concentrating on reducing rework, the strategy for halting modifications, as shown in the case study on modular products, effectively identifies related tasks to be paused at the same time, assesses the decrease of rework, and establishes the best approach for halting modifications.
This methodology improves efficiency in the development lifecycle by considerably minimizing iterations, thereby emphasizing the significance of the design freeze medical device in attaining project objectives in accordance with Colombia's regulatory framework. Moreover, our clinical trial management services include feasibility studies, site selection, compliance reviews, trial setup, import permits, project management, and reporting, which are essential in supporting the configuration completion process. Moreover, the substantial expenses linked to clinical studies, projected to surpass millions of dollars, emphasize the essential requirement for a clearly defined project halt to manage resources efficiently.
Key Steps and Considerations Before Implementing Design Freeze
Before implementing a design freeze in medical device development, several essential steps must be effectively executed:
-
Evaluation Reviews:
Participate in thorough evaluation review meetings. These sessions are essential for assessing the layout against established requirements and identifying any necessary modifications.
-
Validation Testing:
Initial validation testing is crucial to verify that the structure aligns with intended use and meets user requirements. Engineering Verification Testing (EVT) is particularly significant, as it ensures that the design freeze medical device meets critical performance criteria before progressing to the verification and validation (V&V) stages.
Studies show that effective EVT can reduce the risk of costly redesigns later in the process.
-
Risk Management:
Conduct a thorough risk analysis to identify potential hazards and develop corresponding mitigation strategies. This process ensures that risks are proactively managed throughout the development lifecycle.
-
Documentation:
Assemble comprehensive documentation, including design history files, updated specifications, and verification reports. This documentation is essential for compliance with regulations and internal quality assurance.
-
Stakeholder Approval:
Secure approvals from key stakeholders, including regulatory bodies and quality assurance teams, to ensure a unified consensus on proceeding.
Adnan Ashfaq emphasizes the importance of confirming market viability before progressing, stating,
Once you have a proof of concept and are convinced that your device has a market position, is viable and financially feasible, only then should you begin to seek funding for prototyping and trial runs on your device.
Additionally, Wang W.-C. et al. propose a DEMATEL-based model for performance enhancement that can be utilized to improve control processes in matrix organizations.
Combining these steps not only streamlines the development process but also enhances the overall effectiveness of reviews, as supported by the case study highlighting the benefits of merging planning and risk management strategies into a cohesive plan template.
Navigating Challenges in Design Controls and the Design Freeze Dilemma
During the development halt phase, several challenges can significantly affect control measures, often arising from changing stakeholder requirements or unexpected technical issues. Key dilemmas include:
- Changing Requirements: Stakeholders may point out extra features or changes late in the process, complicating the finalization. This can hinder progress and lead to delays.
- Technical Challenges: Unexpected structural flaws or performance issues may arise, prompting discussions about revisiting the layout. These technical hurdles can lead to costly adjustments if not anticipated early.
- Compliance Issues: Inadequate documentation or failure to adhere to regulatory standards, such as those set forth by INVIMA, can necessitate revisions to the design freeze medical device prior to implementation. Effective compliance is essential to prevent setbacks during audits, especially in a landscape where the Colombian National Food and Drug Surveillance Institute plays a vital role in medical equipment oversight.
Alongside these challenges, extensive clinical trial management services are crucial for navigating the complexities of medical instrument investigations. This includes conducting feasibility studies to assess site capabilities, selecting appropriate research sites, and ensuring compliance reviews are thorough and timely. The trial setup process must align with regulatory requirements, including obtaining necessary import permits and approvals from ethics committees and health ministries.
Project management is vital throughout the trial, ensuring all aspects are monitored effectively, and reporting on study status, inventory, and adverse events is conducted diligently.
The medical device industry is vast, with the FDA having approved approximately 500,000 medical device models produced by around 23,000 different manufacturers by the late 1990s. This statistic emphasizes the importance of effective controls in such a complex landscape. To illustrate real-world challenges, consider the case study titled "Medical Device Development Phase II - Formulation, Concept, and Feasibility," which emphasizes the necessity of understanding regulatory requirements and incorporating customer feedback during the creation phase.
Furthermore, new trends, such as the incorporation of therapies with medical equipment and advancements in biotechnology and nanotechnology, are transforming the development landscape, making it essential for teams to modify their control processes accordingly. To effectively navigate these challenges, it is essential for teams to cultivate open communication among stakeholders and prioritize proactive risk management. This method not only foresees possible issues but also guarantees that thorough documentation is upheld from the project's beginning, protecting against risks linked to incomplete history files.
As Katherine Ruiz, an expert in Regulatory Affairs for medical devices and in vitro diagnostics in Colombia, notes, the growth and innovation in medical devices depend on our ability to effectively manage the complexities surrounding the design freeze medical device process.
The Role of Prototyping in Achieving Effective Design Freeze
Prototyping is essential to the freeze process, enabling teams to rigorously test and refine their concepts prior to finalization. The key benefits of a systematic prototyping approach include:
-
User Feedback: Prototypes enable early user testing, providing essential insights that can direct improvements.
The voices of users are essential; as noted by Kevin Kallmes, co-founder of Nested Knowledge,
You should have a Z axis going back into it,
emphasizing the need for comprehensive feedback channels that align with a systematic approach to clinical evidence management. This approach connects user feedback directly to decision-making processes, ensuring that the final outcome is informed by real-world insights.
-
Technical Validation: Prototyping enables teams to evaluate the technical viability of the concept, identifying potential problems before they develop into major challenges.
-
Risk Mitigation: Identifying flaws and areas for improvement during the prototyping phase is crucial.
This proactive approach significantly minimizes the risks linked to the final layout. The use of effective prototyping methods can result in a more certain design freeze, ensuring the product is production-ready and adheres to compliance standards. Notably, bioaccess® offers comprehensive clinical trial management services that facilitate studies such as Early-Feasibility Studies (EFS), First-In-Human Studies (FIH), and Post-Market Clinical Follow-Up Studies (PMCF).
Their expertise in navigating regulatory requirements, including compliance with INVIMA, ensures that clinical trials in Latin America are conducted efficiently and effectively. These services support the prototyping phase by ensuring that all necessary compliance reviews and project management practices are in place, which ultimately enhances the reliability of the prototyping process. Furthermore, the case study titled Validation Methods for Conceptual Modeling in Medical Instruments illustrates how a comprehensive model for medical instrument development was validated using various methods, confirming its credibility and usability for novice developers through effective user feedback mechanisms.
This case study highlights the methodologies employed during clinical trials, reinforcing the importance of structured feedback in the development process. For additional reference, see PMID: 26229119, which discusses the significance of these methodologies in the context of medical innovation.
Regulatory Considerations and Compliance Related to Design Freeze
The idea of finalizing specifications carries considerable legal implications for medical device producers, especially regarding adherence to standards like ISO 13485. With experts like Ana Criado, Director of Regulatory Affairs, professor with deep knowledge in biomedical engineering, and founder and CEO of Mahu Pharma, along with Katherine Ruiz, an authority in Regulatory Affairs for Medical Devices and In Vitro Diagnostics in Colombia, it is imperative to understand several key considerations:
-
Documentation Requirements: Detailed documentation of all modifications and decisions made before the project cut-off is vital for aiding regulatory submissions.
This ensures transparency and traceability in the development process.
-
Validation Protocols: Adherence to rigorous validation protocols is crucial, as they confirm that the final layout meets established safety and efficacy standards.
This step is vital for maintaining compliance and ensuring patient safety.
-
After establishing a design freeze medical device, any modifications must adhere to a stringent change control process.
This is necessary to uphold compliance and mitigate risks associated with unregulated changes.
Engaging experts like Ana Criado can significantly enhance adherence to these standards and safety protocols, ensuring a smoother path to compliance. The oversight landscape is evolving, particularly due to digital transformation within the manufacturing sector, which is now essential for competitiveness.
This transformation introduces new complexities that manufacturers must navigate. Understanding the differences between 'Locked vs. Adaptive Algorithms' is crucial, as locked algorithms require human intervention for changes while adaptive algorithms adjust automatically based on input data.
For example, a case study involving an AI/ML tool highlighted the compliance challenges when the algorithm's adaptive nature conflicted with existing legal frameworks, illustrating the importance of thorough understanding of regulations.
Failing to meet these compliance requirements can lead to significant delays and increased costs in the product development lifecycle.
As Dr. Tina Priewasser aptly notes,
Regulation should affect both manufacturers and users,
highlighting the shared responsibility in ensuring compliance. Understanding these regulatory considerations is paramount for successful product development and market approval in the competitive medical device landscape.
Conclusion
The design freeze represents a crucial milestone in the medical device development journey, serving as a formal declaration that the design is final and ready for validation and regulatory compliance. By effectively implementing a design freeze, organizations can streamline their development processes, allocate resources more efficiently, and minimize the risks associated with late-stage modifications. The importance of this stage is underscored by the oversight of INVIMA, which mandates strict adherence to regulatory standards in Colombia.
Key steps such as:
- Conducting thorough design reviews
- Validating testing
- Managing risks
are essential for successfully navigating the design freeze phase. Challenges, including evolving stakeholder requirements and compliance issues, must be proactively addressed to maintain project momentum. Moreover, the integration of prototyping within the design freeze process allows for the identification of potential issues early on, further enhancing the likelihood of regulatory compliance and market success.
Ultimately, understanding and implementing a well-defined design freeze strategy is vital for medical device manufacturers. By recognizing its significance in the development lifecycle and adhering to regulatory requirements, organizations can not only ensure the safety and efficacy of their products but also achieve a competitive edge in the marketplace. As the landscape of medical device innovation continues to evolve, the ability to manage these complexities will be paramount for success.
Frequently Asked Questions
What is a design freeze in medical device development?
A design freeze marks a critical moment in the development process when the blueprint is considered final, and any further changes require substantial justification. This milestone allows teams to focus on validation, verification, and preparing documentation for regulatory submissions.
Why is the design freeze important for medical device development?
The design freeze is essential for maintaining timelines and ensuring optimal resource allocation towards testing and quality assurance, rather than ongoing modifications. It helps manage stakeholder expectations and streamlines the development process.
What are the steps to take before implementing a design freeze?
The essential steps include: 1. Evaluation Reviews: Conduct thorough meetings to assess the layout against requirements. 2. Validation Testing: Perform initial validation testing to ensure the design meets user needs. 3. Risk Management: Conduct a risk analysis to identify hazards and develop mitigation strategies. 4. Documentation: Assemble comprehensive documentation for compliance and quality assurance. 5. Stakeholder Approval: Obtain approvals from key stakeholders to confirm consensus on proceeding.
What role does INVIMA play in the design freeze process?
INVIMA, the Colombia National Food and Drug Surveillance Institute, oversees compliance with health regulations, particularly during the design freeze phase. Adhering to INVIMA's protocols is crucial for regulatory submissions in Colombia.
How does a design freeze impact project costs and efficiency?
A clearly defined project halt minimizes rework and reduces costs associated with clinical studies, which can reach millions of dollars. It enhances efficiency in the development lifecycle by decreasing iterations and focusing resources effectively.
What are the consequences of not adhering to a design freeze?
Failing to implement a design freeze can lead to ongoing alterations that disrupt timelines, increase costs, and complicate compliance with regulatory requirements, ultimately jeopardizing project objectives.
What are the benefits of merging planning and risk management strategies?
Combining planning and risk management enhances the overall effectiveness of reviews and streamlines the development process, as demonstrated by case studies that highlight improved control processes in matrix organizations.




