Introduction
The realm of medical device combination products is at the forefront of innovation, merging therapeutic and diagnostic capabilities to enhance patient care. These products, which integrate a medical device with drugs or biological elements, are subject to a complex regulatory landscape that varies significantly across regions. Understanding the classifications established by regulatory bodies such as the FDA and EMA is crucial for stakeholders aiming to navigate this intricate environment effectively.
As advancements in technology continue to reshape the healthcare landscape, the importance of rigorous clinical trials, compliance with post-market surveillance, and the role of key regulatory authorities cannot be overstated.
This article delves into the definitions, regulatory challenges, and clinical evidence requirements surrounding combination products, highlighting the significant impact these innovations have on patient outcomes and the healthcare industry as a whole.
Defining Medical Device Combination Products: An Overview
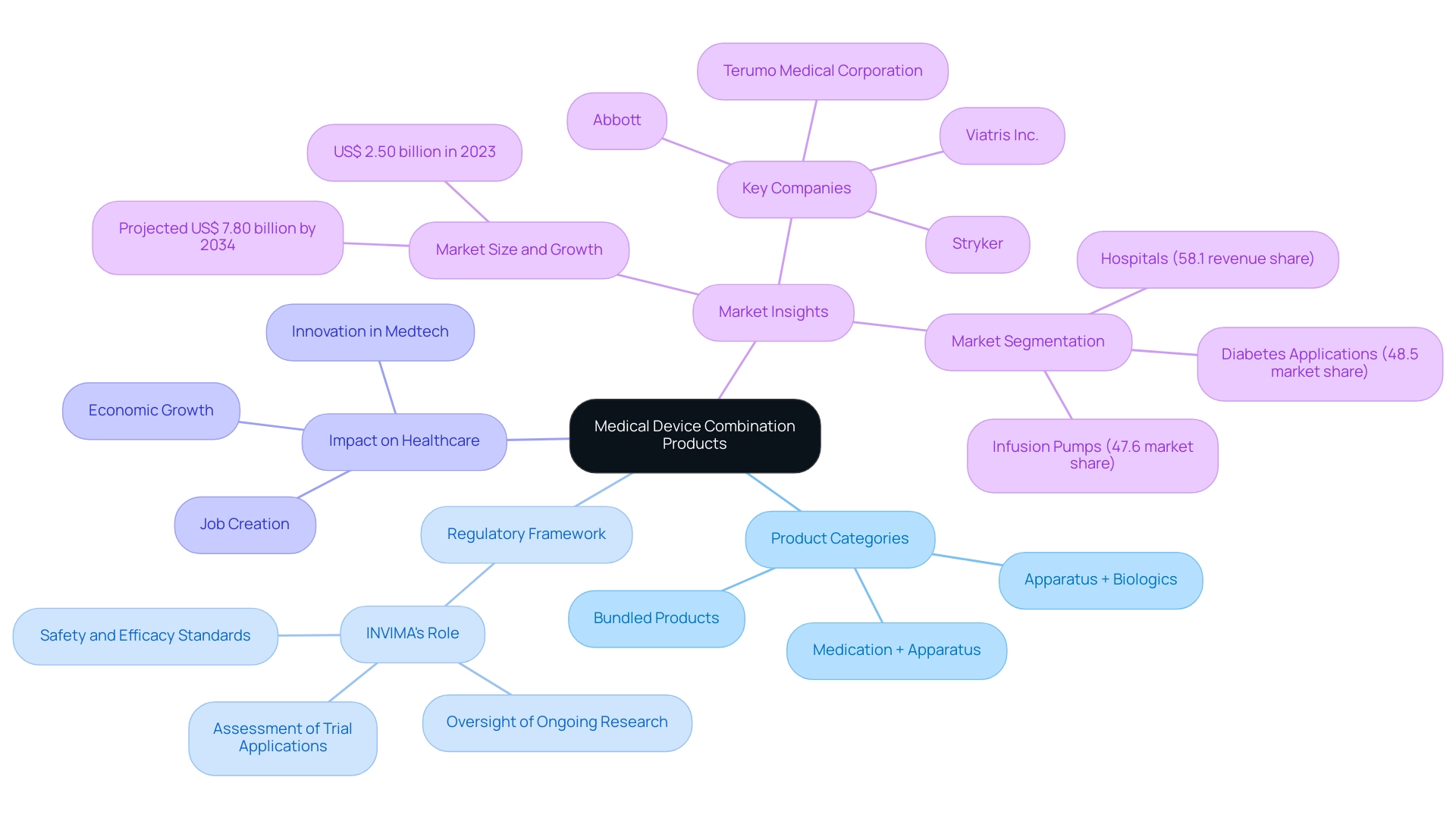
Medical device combination products are innovative entities that integrate therapeutic and diagnostic functionalities by merging a medical instrument with a drug, biological solution, or other instruments. The FDA categorizes medical device combination products into three main groups:
- Products that combine a medication with an apparatus
- Products that include an apparatus alongside biologics
- Products that are bundled together but can be used separately
This classification framework is critical as it guides stakeholders through the complex regulatory landscape associated with the development, approval, and marketing of medical device combination products.
As the landscape evolves, understanding these definitions becomes paramount for successful navigation. Notably, Sparta Biomedical's recent treatment of the first patients with the Ormi device represents a significant milestone in Medtech, showcasing the potential of innovative solutions in improving patient outcomes in Latin America. Moreover, PAVmed's successful first-in-human implantations of the PortIO™ Intraosseous Infusion System in Colombia not only highlight advancements in research studies but also reflect the challenges faced by Medtech companies in bridging gaps in research and innovation.
The regulatory environment, especially the supervision by INVIMA, designated by PAHO/WHO as a Level 4 health authority, plays a vital role in ensuring compliance and facilitating market entry for these innovative offerings. INVIMA's responsibilities encompass the assessment of trial applications, oversight of ongoing research, and ensuring that items meet safety and efficacy standards. The impact of Medtech research studies extends beyond healthcare improvements; they contribute to local economies through job creation, economic growth, and international collaboration.
As this sector continues to grow, the projected market expansion for medical device combination products, especially in infusion pumps and diabetes-related applications, underscores the increasing intersection of technology and healthcare. Comprehensive clinical trial management services, including feasibility studies, site selection, compliance reviews, trial setup, and project management, are essential to navigating this complex landscape and ensuring successful outcomes.
Navigating Regulatory Compliance for Combination Products
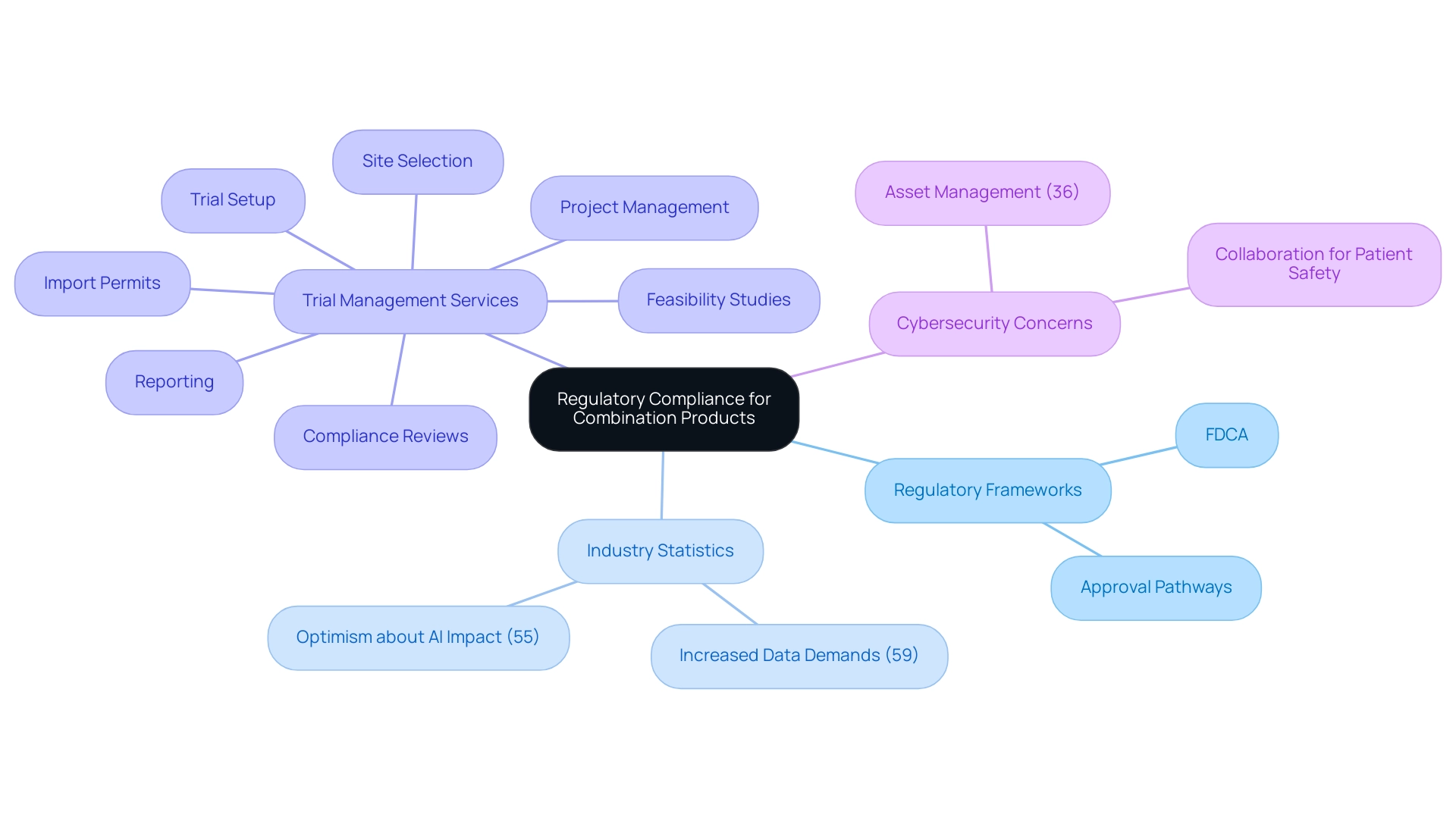
Navigating compliance for medical device combination products necessitates a comprehensive understanding of multiple frameworks, primarily dictated by the FDA. Central to this process are the regulations outlined in the Food, Drug, and Cosmetic Act (FDCA), which governs the approval pathways for medications and products. In this landscape, expert services like those provided by Katherine Ruiz—specializing in compliance matters for medical devices and in vitro diagnostics in Colombia—are invaluable.
Recent statistics indicate that:
- 59% of industry professionals believe regulatory agencies are demanding more trial data than in previous years, underscoring the need for meticulous pre-market evaluations to ensure safety, efficacy, and quality standards are met.
- 55% of respondents express optimism about the future impact of AI on the MedTech sector, suggesting that advancements in technology could streamline compliance processes and enhance the development of combination products.
Comprehensive trial management services, including:
- Feasibility studies
- Site selection
- Compliance reviews
- Trial setup
- Import permits
- Project management
- Reporting
are essential to meet these elevated expectations.
Specifically, the feasibility and selection of research sites and principal investigators are critical steps in this process, ensuring that trials are conducted efficiently and effectively. Producers must carry out thorough trials and follow Good Manufacturing Practices (GMP) to comply with oversight requirements. Additionally, it is crucial to grasp the unique requirements for post-market surveillance and reporting to maintain compliance throughout the item lifecycle.
Organizations such as bioaccess®, a frontrunner in MedTech clinical research in Latin America, highlight the importance of innovation and compliance excellence in supporting these efforts. In their quest to bolster compliance capabilities, strategic alliances are vital for enhancing worldwide presence and meeting the needs of the industry. The intricacy surrounding compliance challenges for medical device combination products necessitates strong systems that offer visibility and control over every element, ensuring efficient tracking and management, particularly as cybersecurity issues increase—36% of medical equipment companies identified asset management as their primary security concern in 2024.
Furthermore, the healthcare sector must emphasize cybersecurity as a component of patient safety strategies, necessitating cooperation among manufacturers, healthcare providers, and governing bodies. By addressing these multifaceted regulatory demands, including the specific challenges for medical device combination products, manufacturers can better position themselves in the evolving landscape of medical device development.
Key Regulatory Bodies and Their Roles
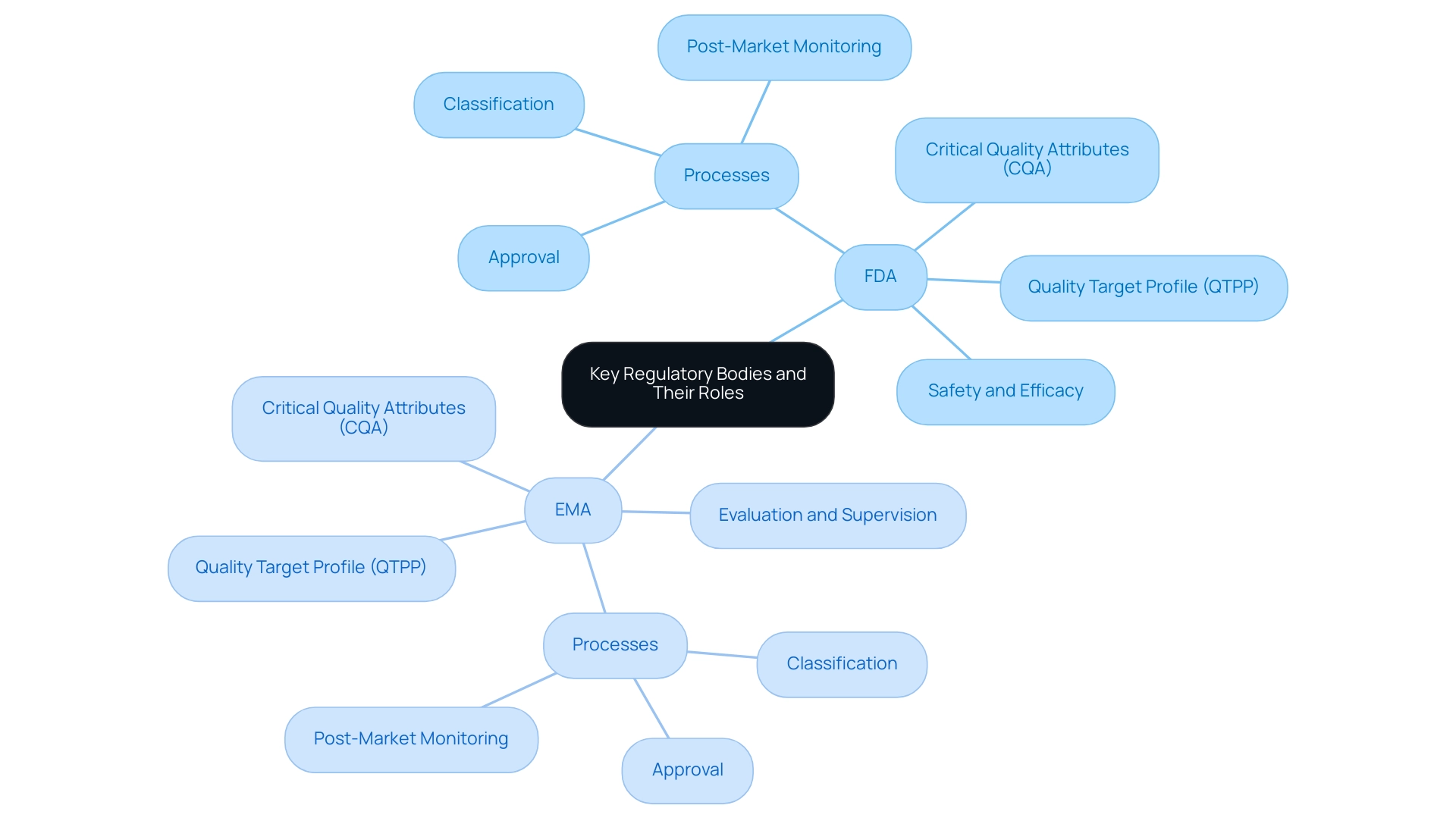
The regulation of combination items is primarily governed by two key bodies: the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA). The FDA's mandate is to ensure that these items are both safe and effective for public use, while the EMA is tasked with the evaluation and supervision of medicinal goods across Europe. Each agency has established specific processes for the classification, approval, and post-market monitoring of medical device combination products, which are crucial for manufacturers to comprehend in order to achieve compliance with regulations.
Recent guidelines emphasize the necessity for discussions surrounding the impact of the medical device on the Quality Target Profile (QTPP), Critical Quality Attributes (CQA), and control strategy of the drug to be included in submission dossiers. For example, some items designed for use together do not fulfill the official criteria of combination items, such as syringes promoted for general drug delivery. Clarifying these misconceptions aids in ensuring proper adherence to guidelines and understanding of classifications.
Moreover, four medical device combination products were authorized via priority review, emphasizing the changing environment of oversight processes. As R.J. noted, 'the majority of the new drugs approved by both FDA and EMA were first approved in the USA,' emphasizing the significance of understanding these oversight requirements for effectively navigating the complexities associated with medical device combination products. Ana Criado, in her role as the Director of Compliance Affairs, brings invaluable expertise from her leadership positions at Colombia’s oversight agency —INVIMA— and her experience as an external consultant for major global companies.
Her background in biomedical engineering and health economics enhances the understanding of these governance frameworks, particularly in the context of medical devices and digital health innovations. Furthermore, as the founder and CEO of Mahu Pharma, Ana plays a pivotal role in cannabis regulation, contributing to the development of compliant practices in the cultivation and manufacturing of cannabis-based items, which is increasingly relevant in today's regulatory landscape.
Clinical Trials and Evidence Requirements
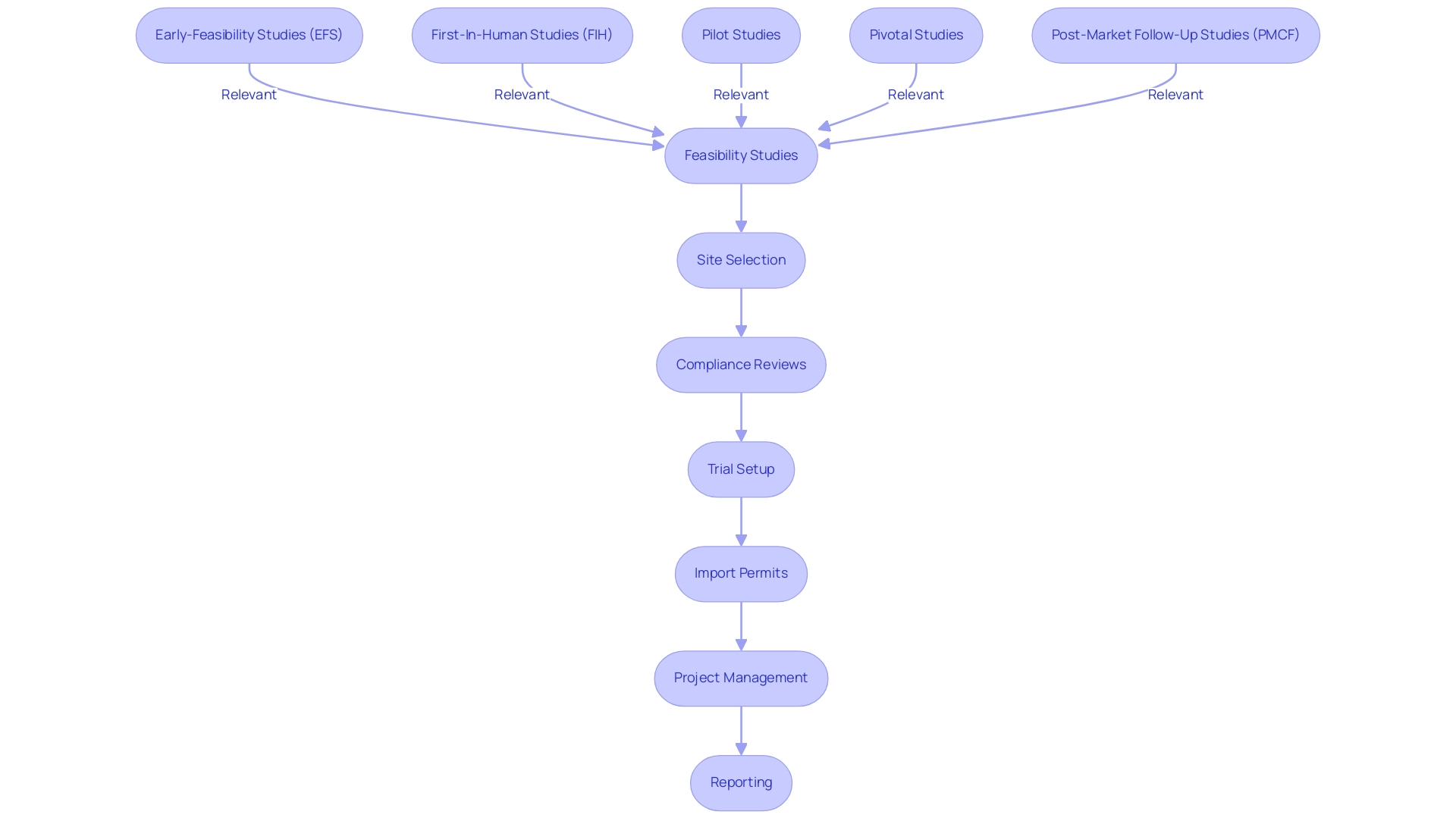
Clinical trials play an essential role in establishing the safety and efficacy of medical device combination products, particularly in the rapidly evolving fields of digital health and MedTech. Manufacturers must design trials that adhere to Good Clinical Practice (GCP) guidelines for medical device combination products, ensuring that both device and pharmaceutical components are thoroughly assessed. At bioaccess®, with over 20 years of experience in Medtech, we specialize in comprehensive trial management services, including:
- Feasibility studies
- Site selection
- Compliance reviews
- Trial setup
- Import permits
- Project management
- Reporting
Our expertise encompasses:
- Early-Feasibility Studies (EFS)
- First-In-Human Studies (FIH)
- Pilot Studies
- Pivotal Studies
- Post-Market Follow-Up Studies (PMCF)
This allows us to effectively navigate the complexities of research with flexibility and specialized knowledge. The evidence requirements for these trials can vary significantly based on classification, typically necessitating comprehensive data from preclinical studies, alongside Phase I, II, and III trials to substantiate claims. The expanding musculoskeletal disorders pharmaceuticals market, expected to attain $163.94 billion by 2026, highlights the urgent need for strong medical data driven by an aging population and rising healthcare requirements.
Moreover, the trend towards minimally invasive procedures and consistent-dosing treatment options emphasizes the essential need for thorough data gathering and analysis during the trial process, ensuring that offerings not only satisfy compliance standards but also correspond with the expectations of healthcare providers and patients alike. Through our dedicated approach, bioaccess® is committed to leading Medtech clinical research in Latin America with a focus on innovation and compliance excellence, supporting local economies through job creation and healthcare improvement, and guiding companies towards successful acquisitions.
Post-Market Surveillance and Reporting Requirements
After obtaining market approval, producers of medical device combination products must actively participate in post-market surveillance (PMS) to ensure ongoing safety and performance, particularly under the framework established by INVIMA, the Colombia National Food and Drug Surveillance Institute. This process involves:
- The systematic collection of data concerning adverse events
- Conducting regular safety reviews
- Submitting detailed findings to oversight bodies such as INVIMA
Adherence to the Medical Device Regulation’s post-market monitoring requirements is crucial for manufacturers to acquire and retain the CE marking, which indicates that their products meet the essential safety and performance standards for sale in the European market.
Adherence to the post-market reporting requirements is not merely a regulatory obligation but a fundamental aspect of maintaining product approval and safeguarding user health. Notably, the FDA requires post-market monitoring for any products intended for implantation in the human body for over a year, emphasizing the essential nature of this oversight. A proactive approach to PMS, including regular staff training on procedures, is vital for effective documentation and investigation of feedback.
One such case study demonstrates that continuous improvement in PMS processes, through regular training and refinement of systems, can significantly enhance safety, increase customer satisfaction, and support ongoing business development. Manufacturers must also be prepared for potential recalls or safety alerts should significant issues arise during surveillance activities, ensuring a robust response mechanism is in place. As industry leaders like Pedro Sancha emphasize, 'a commitment to rigorous PMS is essential for fostering trust and accountability in the rapidly evolving MedTech landscape.'
Katherine Ruiz, an expert in Regulatory Affairs for Medical Devices and In Vitro Diagnostics in Colombia, underscores the importance of adhering to INVIMA's standards for medical device combination products, which include specific pre- and post-market programs and technical standards for manufacturing, to ensure compliance and safety in the development of these medical technologies. Additionally, INVIMA's classification as a Level 4 health authority signifies its competence and efficiency in regulating health products, further enhancing the credibility of its oversight in ensuring the safety, efficacy, and quality of medical devices.

Conclusion
The landscape of medical device combination products is characterized by a blend of therapeutic and diagnostic innovations that hold the potential to significantly enhance patient care. Understanding the classifications set forth by regulatory bodies such as the FDA and EMA is essential for stakeholders navigating this complex terrain. The article outlines the critical role of comprehensive clinical trials and robust post-market surveillance in ensuring that these products not only meet safety and efficacy standards but also contribute positively to healthcare outcomes and local economies.
Navigating the regulatory compliance landscape presents challenges that require meticulous attention to detail and a clear understanding of the multifaceted frameworks governing combination products. The insights shared in this article underscore the importance of collaboration among manufacturers, regulatory bodies, and healthcare providers to address these challenges effectively. As advancements in technology, such as artificial intelligence, continue to reshape the MedTech sector, the potential for improving compliance processes and product development remains promising.
Ultimately, the ongoing evolution of medical device combination products, along with the regulatory environment, highlights the need for continuous innovation and adherence to best practices. By prioritizing rigorous clinical evidence and proactive post-market activities, manufacturers can not only fulfill regulatory obligations but also build trust and accountability within the healthcare ecosystem. The commitment to excellence in this field will pave the way for future advancements, ensuring that combination products fulfill their promise of improving patient outcomes and transforming healthcare delivery.
Frequently Asked Questions
What are medical device combination products?
Medical device combination products are innovative entities that integrate therapeutic and diagnostic functionalities by merging a medical instrument with a drug, biological solution, or other instruments.
How does the FDA categorize medical device combination products?
The FDA categorizes medical device combination products into three main groups: 1) Products that combine a medication with an apparatus, 2) Products that include an apparatus alongside biologics, and 3) Products that are bundled together but can be used separately.
Why is the classification of medical device combination products important?
The classification framework is critical as it guides stakeholders through the complex regulatory landscape associated with the development, approval, and marketing of these products.
What recent advancements in medical device combination products have been noted?
Notable advancements include Sparta Biomedical's treatment of the first patients with the Ormi device and PAVmed's successful first-in-human implantations of the PortIO™ Intraosseous Infusion System in Colombia.
What role does INVIMA play in the regulation of medical device combination products?
INVIMA is responsible for assessing trial applications, overseeing ongoing research, and ensuring that products meet safety and efficacy standards, facilitating market entry for innovative offerings.
How do medical device combination products impact local economies?
Medtech research studies contribute to local economies through job creation, economic growth, and international collaboration.
What is the projected market trend for medical device combination products?
There is an increasing market expansion for medical device combination products, particularly in infusion pumps and diabetes-related applications.
What services are essential for managing clinical trials in this sector?
Comprehensive clinical trial management services essential for navigating this landscape include feasibility studies, site selection, compliance reviews, trial setup, and project management.
What are the current regulatory challenges faced by the MedTech industry?
Regulatory agencies are demanding more trial data than in previous years, necessitating meticulous pre-market evaluations to ensure safety, efficacy, and quality standards are met.
How can technology, particularly AI, impact the MedTech sector?
55% of industry professionals express optimism about the future impact of AI on the MedTech sector, suggesting that advancements in technology could streamline compliance processes and enhance the development of combination products.
What are Good Manufacturing Practices (GMP) in the context of medical device combination products?
Producers must carry out thorough trials and follow Good Manufacturing Practices (GMP) to comply with oversight requirements, ensuring the quality and safety of their products.
What is the significance of cybersecurity in the healthcare sector regarding medical device combination products?
Cybersecurity is a crucial component of patient safety strategies, and cooperation among manufacturers, healthcare providers, and governing bodies is necessary to address regulatory demands and security concerns.

