Introduction
In the intricate landscape of modern healthcare, clinical indications serve as a cornerstone for effective patient management. These indications not only guide healthcare professionals in determining the appropriateness of treatments, medications, and procedures but also play a critical role in enhancing patient safety and outcomes.
As the medical field continues to evolve with advancements in technology and an increasing emphasis on evidence-based practices, understanding clinical indications becomes paramount. This article delves into the multifaceted nature of clinical indications, exploring their definitions, types, and the challenges faced in their implementation.
Through a comprehensive examination of recent studies and expert insights, the discussion highlights the vital importance of adhering to clinical indications in delivering quality care and navigating the complexities of regulatory compliance.
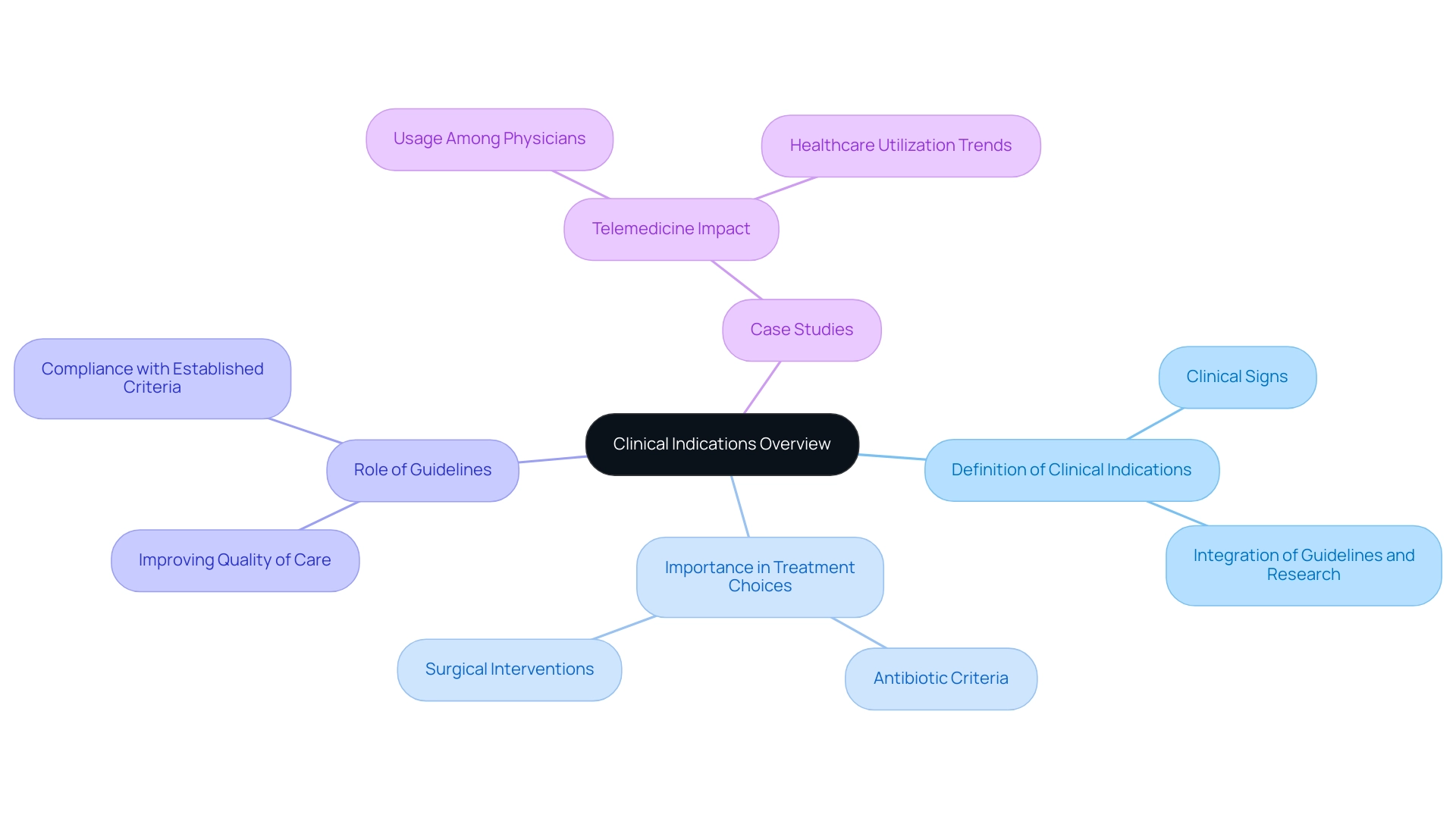
Defining Clinical Indications: An Overview
Clinical signs encompass the clinical indications meaning the specific circumstances or conditions that determine the appropriateness of a particular treatment, medication, or procedure for a patient. These signals stem from a thorough integration of medical guidelines, research findings, and professional expertise. For example, a medical reason for prescribing antibiotics is usually a confirmed bacterial infection, while the existence of a tumor may act as a medical reason for surgical intervention.
The significance of medical signs, often referred to as clinical indications meaning, cannot be emphasized enough, as they play a vital role in assisting professionals in making informed treatment choices. Recent data from the World Health Statistics report emphasize a rising focus on medical signs in health services, showing that accuracy in treatment choices is crucial for enhancing patient results. This precision is becoming increasingly vital as medical systems evolve, particularly in the context of telemedicine.
A case study named 'Telemedicine Usage Among Physicians by Physician Specialty: United States, 2021' demonstrates how medical factors can affect healthcare utilization and access. By employing electronic medical records, physicians can more efficiently assess the suitable application of telemedicine based on medical needs, ultimately improving care for individuals. Furthermore, the American Hospital Association (AHA) highlights this point, stating that 'One of the goals of AHA’s partnership with Vizient on this project was to assist in offering individuals, policymakers and the public with a more timely, accurate view of how hospitals are performing now instead of depending on older and sometimes outdated data.'
Such insights highlight the importance of following medical guidelines to improve the quality of care offered to individuals. Practical examples, such as the use of criteria for antibiotics, illustrate the clinical indications meaning and how these guidelines directly affect treatment decisions and the safety of individuals. Moreover, recent research has strengthened the influence of care protocols on treatment choices, showing that compliance with established criteria results in better health outcomes and resource usage.
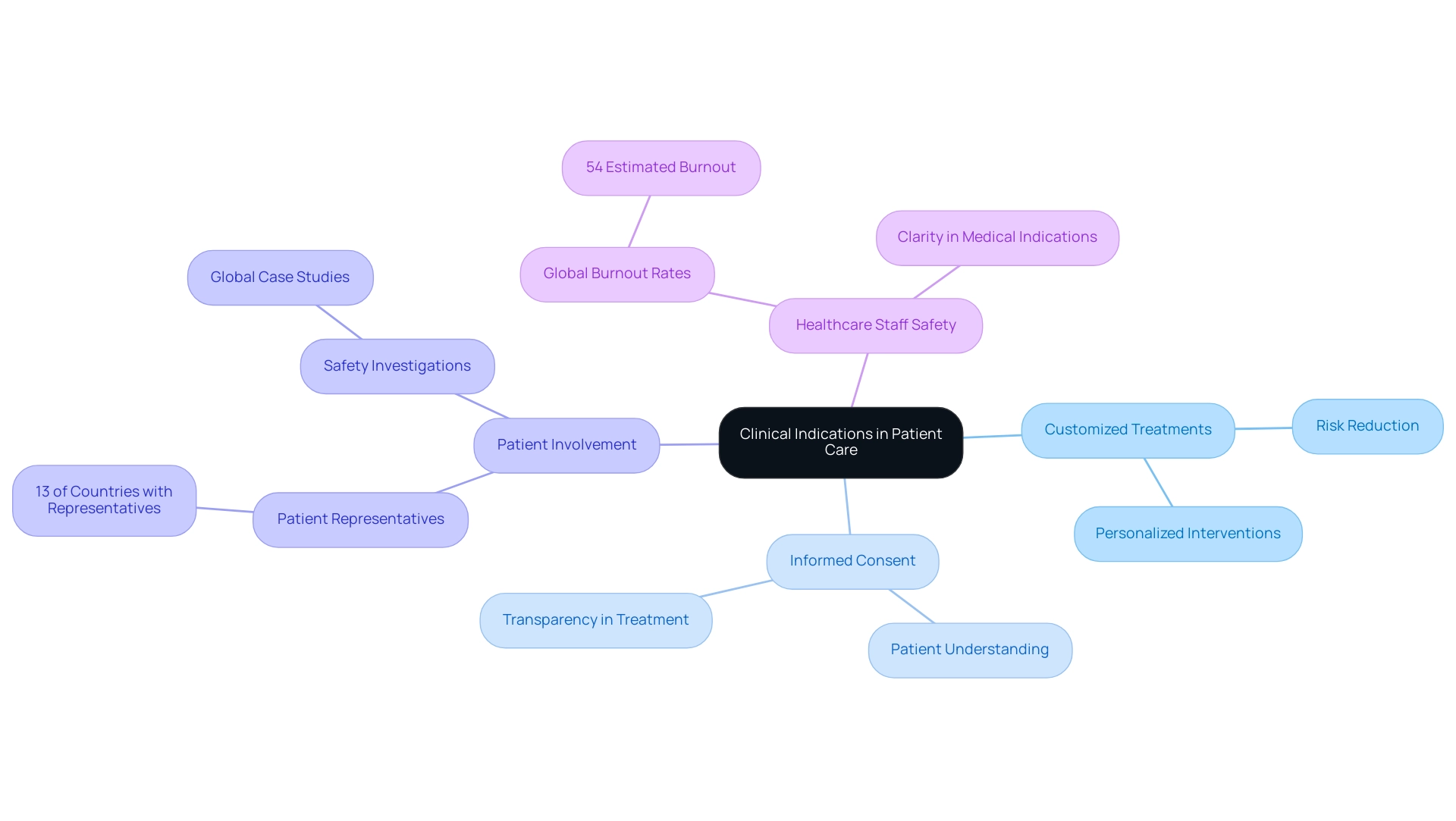
The Role of Clinical Indications in Patient Care and Safety
Clinical signs are essential for guaranteeing that medical therapies are accurately customized to the distinct requirements of every individual. By assisting healthcare professionals in choosing suitable interventions, medical signs help reduce the risk of negative effects and greatly improve safety for individuals. For instance, a thorough grasp of the medical uses for a specific medication allows doctors to evaluate its appropriateness considering an individual's medical background and present health condition.
Furthermore, medical signs play an essential role in the informed consent process, providing individuals with the necessary reasoning behind prescribed treatments. This commitment to recognized medical guidelines not only fosters a culture of safety within medical environments but also enables individuals in their treatment paths. Consequently, this organized method results in enhanced health results, showcasing the inherent connection between medical signs and efficient care for individuals.
Moreover, with global burnout rates estimated at 54%, ensuring clarity in medical indications can alleviate some of the pressures faced by healthcare staff, thereby enhancing their ability to provide safe care. It's also significant that 13% of nations have a representative for individuals receiving care on their governing boards or a similar mechanism in 60% or more hospitals, emphasizing the essential role of individual involvement in medical decision-making. Insights from the 'Global Case Studies in Safety' report illustrate successful efforts in involving individuals in safety investigations, which can further enhance safety practices globally.
Moreover, understanding perceptions of safe care, as examined by the OECD's pilot measures, underscores the ongoing need to address current healthcare challenges related to clinical indications meaning and patient safety.
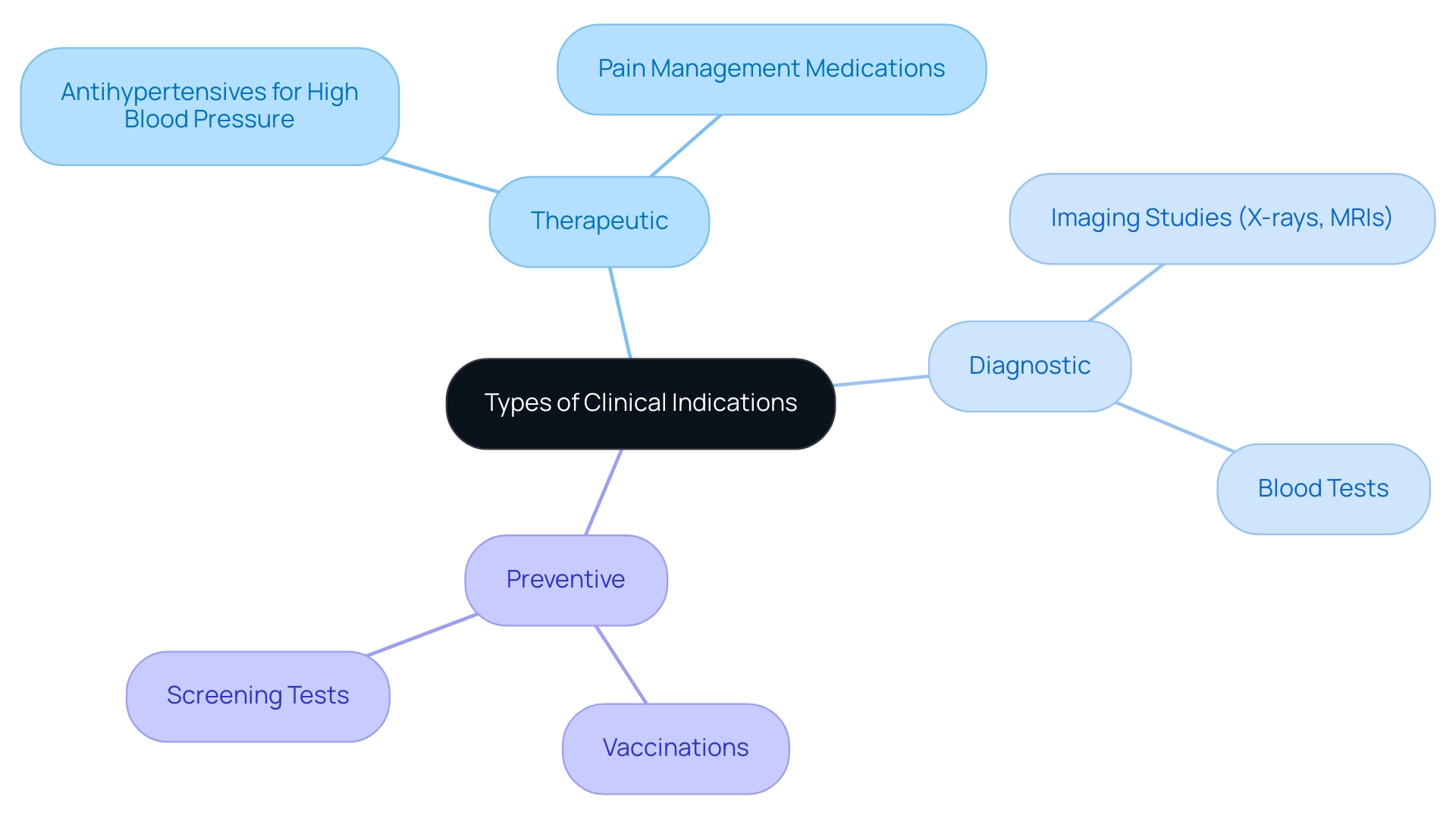
Types of Clinical Indications
Clinical signs are critical components of medical practice and can be categorized into three primary types: therapeutic, diagnostic, and preventive.
- Therapeutic purposes relate to the rationale behind administering treatments aimed at alleviating symptoms or curing conditions. For instance, prescribing antihypertensives for patients with high blood pressure exemplifies a therapeutic approach.
- Diagnostic signals involve procedures or tests aimed at confirming or ruling out specific diagnoses. A clear example is the use of imaging studies, such as X-rays or MRIs, to evaluate suspected fractures.
- Preventive indications focus on proactive measures designed to avert diseases, with vaccinations serving as a prime illustration.
Comprehending these categories is crucial for healthcare providers, as understanding the clinical indications meaning allows them to make informed decisions regarding patient care and choose the most suitable interventions tailored to individual medical scenarios. Recent research indicates that the success rates of Phase III trials have notably risen to 66%, surpassing the 56% pre-pandemic average. This statistic highlights the changing environment of medical criteria and their uses in healthcare, especially concerning therapeutic interventions.
Moreover, the ongoing dialogue surrounding the importance of both statistical and practical significance highlights the necessity for researchers to evaluate study results comprehensively. Ron Wasserstein, the executive director of the American Statistical Association, aptly noted:
The value was never meant to substitute the scientific reasoning, which is of greater interest.
This viewpoint is especially pertinent in the realm of therapeutic and diagnostic purposes, where grasping their subtleties can greatly influence patient outcomes.
Furthermore, the case study titled 'Drug Overdose Deaths in the United States, 2003-2023' offers a real-world example that highlights the importance of comprehending medical signs in tackling public health emergencies, stressing the necessity for informed medical choices based on both statistical and medical significance.
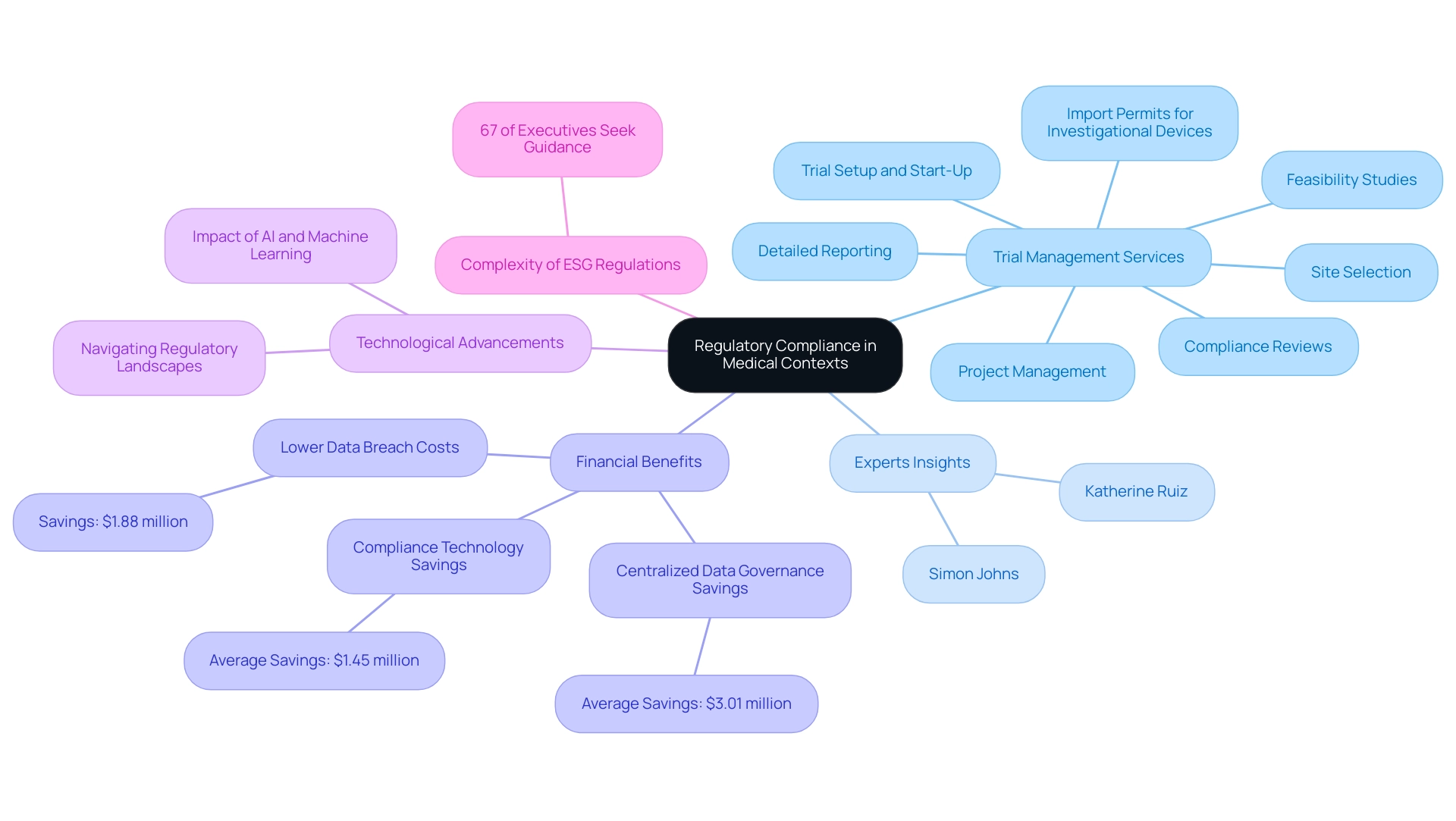
Clinical Indications and Regulatory Compliance
Regulatory compliance plays a crucial role in medical contexts, ensuring that treatments and procedures adhere to established guidelines and evidence-based practices. Our comprehensive trial management services encompass:
- Feasibility studies
- Site selection
- Compliance reviews
- Trial setup and start-up
- Import permits for investigational devices
- Project management
- Detailed reporting to facilitate this compliance
In the United States, the Food and Drug Administration (FDA) serves as a crucial regulatory body, offering frameworks that define the clinical indications meaning and how they should be articulated and utilized.
Such compliance is not only essential for the safety and efficacy of medical interventions but also for fostering public trust in the medical system. Katherine Ruiz, a Regulatory Affairs expert with extensive experience in medical devices and in vitro diagnostics in Colombia, has successfully guided numerous foreign manufacturers through the complexities of obtaining market clearance. Recent insights from experts, such as Simon Johns, Director of Medical Information and Marketed Product Safety, highlight the transformative impact of AI and machine learning on regulatory practices, particularly in addressing the complexities of compliance.
He emphasizes that staying updated with these advancements is vital for professionals navigating regulatory landscapes. Additionally, a survey conducted by Globalscape and the Ponemon Institute identified twelve best practices that can significantly reduce compliance costs, with a centralized data governance program saving an average of $3.01 million. Companies that enabled compliance technology also saved an average of $1.45 million in compliance costs, showcasing the tangible financial benefits of adhering to regulatory standards.
As organizations utilizing AI and automation reported $1.88 million lower data breach costs, it becomes increasingly important for medical professionals to incorporate the latest technological advancements into their practice. With 67% of executives voicing concerns about the complexity of ESG regulations and seeking clearer guidance, aligning medical criteria with the latest FDA guidelines is crucial to ensure that treatments stay effective and reliable.
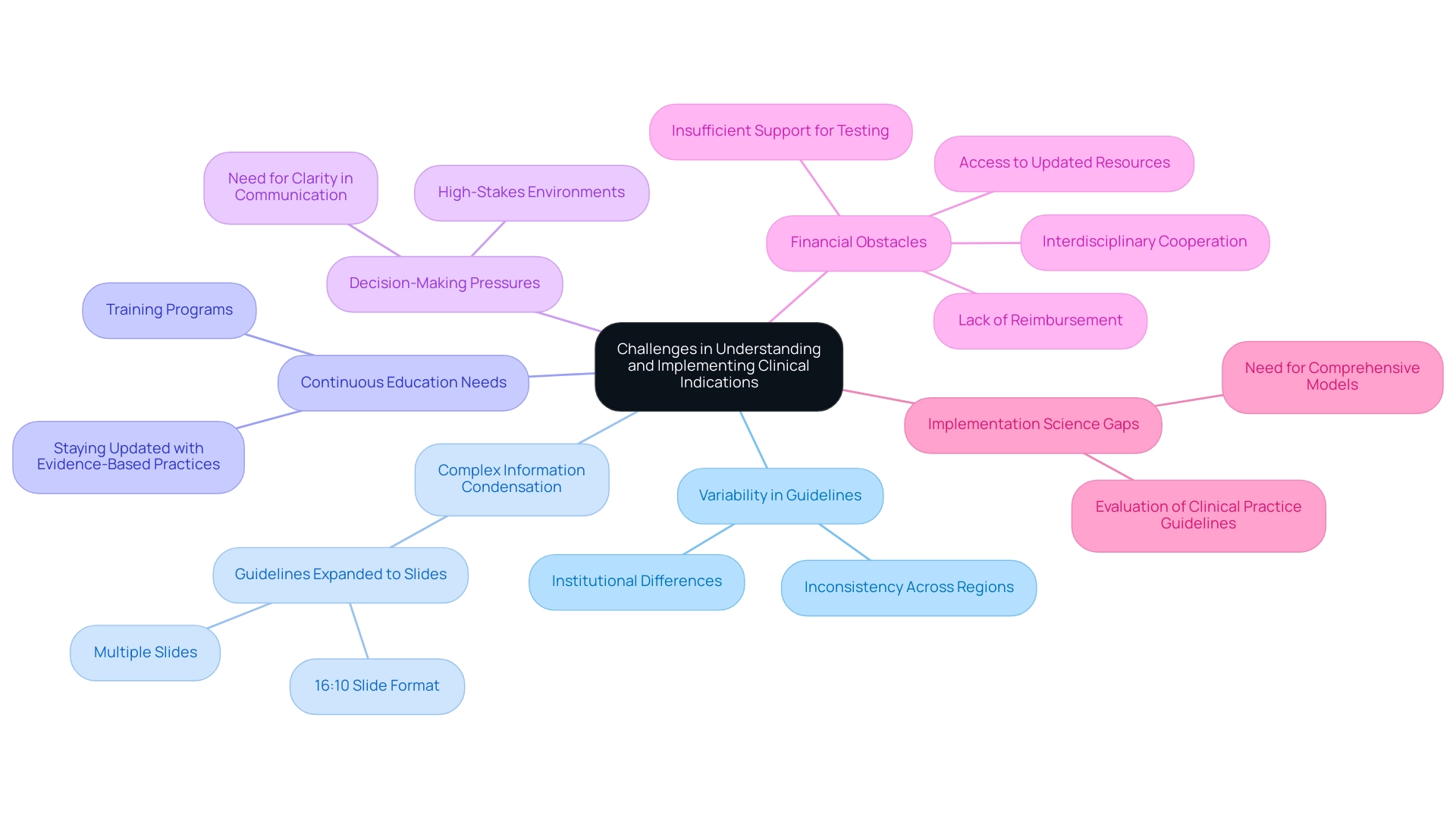
Challenges in Understanding and Implementing Clinical Indications
Navigating the terrain of medical recommendations presents significant challenges for healthcare professionals, primarily due to variability in medical guidelines across regions and institutions. This inconsistency can create confusion regarding the suitable treatment guidelines, ultimately impacting patient care. A recent review highlighted that guidelines which could not condense all relevant medical information onto a single page were frequently expanded to a 16:10 slide format or even distributed across multiple slides, illustrating the complexity of distilling critical information effectively.
Moreover, the rapid evolution of medical knowledge mandates continuous education and adaptation amongst providers, who must stay abreast of the latest evidence-based practices. The pressure to make swift decisions in high-stakes environments can further complicate adherence to established medical indications. As one specialist remarked,
We can offer a rational and comprehensible explanation for individuals,
highlighting the necessity for clarity in communication along with compliance to guidelines.
To tackle these difficulties, continuous training, interdisciplinary cooperation, and access to updated medical resources are crucial. Recent articles have highlighted that financial obstacles, including the absence of reimbursement from insurance providers and inadequate support for testing, significantly impede the application of practice guidelines. Furthermore, a case study titled 'Evaluation of Clinical Practice Guidelines Implementation' highlighted that despite advancements in implementation science, existing models often fail to encompass all necessary domains for comprehensive evaluation, underscoring a critical gap that must be addressed.
This gap can lead to inconsistencies in how clinical indications meaning is applied, further complicating patient care across different settings. In summary, fostering an environment that encourages continuous learning and provides robust support structures will empower healthcare professionals to effectively implement clinical indications meaning, ultimately improving patient outcomes.
Conclusion
In the evolving landscape of healthcare, the significance of clinical indications cannot be overstated. They are essential in guiding healthcare professionals in making informed decisions regarding treatments, medications, and procedures tailored to individual patient needs. By categorizing clinical indications into therapeutic, diagnostic, and preventive types, practitioners can enhance their decision-making processes and improve patient safety. The adherence to these guidelines not only minimizes the risk of adverse effects but also fosters a culture of safety and empowerment for patients throughout their treatment journeys.
Moreover, the role of clinical indications extends beyond patient safety to encompass regulatory compliance, which is critical for maintaining public trust in healthcare systems. By aligning treatment practices with established guidelines and leveraging advancements in technology, healthcare providers can navigate the complexities of regulatory landscapes more effectively. The integration of artificial intelligence and machine learning further underscores the need for continuous adaptation to ensure compliance and enhance the overall quality of care delivered to patients.
Despite the challenges posed by variability in clinical guidelines and the rapid pace of medical advancements, fostering an environment of ongoing education and interdisciplinary collaboration is vital. By addressing these barriers and ensuring access to updated clinical resources, healthcare professionals can effectively implement clinical indications, ultimately leading to improved patient outcomes. The commitment to understanding and adhering to clinical indications will not only enhance individual patient care but also contribute to the overarching goal of elevating healthcare quality across the board.
Frequently Asked Questions
What are clinical signs and why are they important?
Clinical signs, or clinical indications, refer to the specific circumstances that determine the appropriateness of treatments, medications, or procedures for patients. They are crucial for making informed treatment choices and improving patient outcomes by ensuring that interventions are tailored to individual needs.
How do clinical signs influence treatment decisions?
Clinical signs help healthcare professionals assess the medical necessity for specific treatments, such as prescribing antibiotics for confirmed bacterial infections or recommending surgery for tumors. They guide practitioners in making precise and effective treatment decisions.
What types of clinical signs exist?
Clinical signs can be categorized into three primary types: Therapeutic (related to treatments aimed at alleviating symptoms, e.g., prescribing antihypertensives for high blood pressure), Diagnostic (involving tests or procedures to confirm or rule out diagnoses, e.g., imaging studies like X-rays), and Preventive (focused on measures to avert diseases, e.g., vaccinations).
How do clinical signs contribute to patient safety?
By ensuring that medical therapies are customized to individual needs, clinical signs help reduce the risk of negative effects and enhance the overall safety of care. They also support the informed consent process by providing patients with the rationale behind prescribed treatments.
What role do medical guidelines play in healthcare?
Medical guidelines are essential for improving the quality of care and ensuring compliance with established practices. They help healthcare professionals make informed decisions based on the latest research and evidence, ultimately leading to better health outcomes.
How does telemedicine relate to clinical signs?
Telemedicine utilizes clinical signs to assess the appropriate application of remote healthcare services based on medical needs, improving access to care. Electronic medical records facilitate this process, allowing physicians to make informed decisions regarding patient treatment.
What challenges do healthcare professionals face regarding clinical indications?
Professionals encounter variability in medical guidelines across regions and institutions, which can lead to confusion in treatment choices. Continuous education and access to updated resources are necessary to navigate these challenges effectively.
How can compliance with clinical guidelines impact healthcare costs?
Adhering to regulatory compliance and established clinical guidelines can significantly reduce compliance costs for healthcare organizations. Utilizing technology and centralized data governance can lead to substantial financial savings and improved efficiency in medical practices.
What is the significance of patient involvement in clinical decision-making?
Involving patients in their care fosters a culture of safety and enhances treatment outcomes. It emphasizes the importance of clear communication and shared decision-making between healthcare providers and patients.
How has the landscape of clinical indications evolved recently?
Recent research indicates a growing emphasis on clinical indications in healthcare, particularly with the rise of telemedicine and the need for accurate treatment choices. This evolution underscores the importance of adapting to new medical knowledge and practices to improve patient care.




