Introduction
In the realm of clinical research, the selection and definition of endpoints are paramount to the success and integrity of trials. These specific events or outcomes serve as critical measures for evaluating the efficacy of treatments, guiding not only the study's objectives but also influencing the statistical analyses required for interpreting results.
As the landscape of clinical trials evolves, particularly with the advent of digital and novel endpoints, understanding the nuances of endpoint selection becomes increasingly vital. This article delves into the various types of endpoints, their implications for trial outcomes and regulatory approval, and emerging trends that are reshaping the future of clinical research.
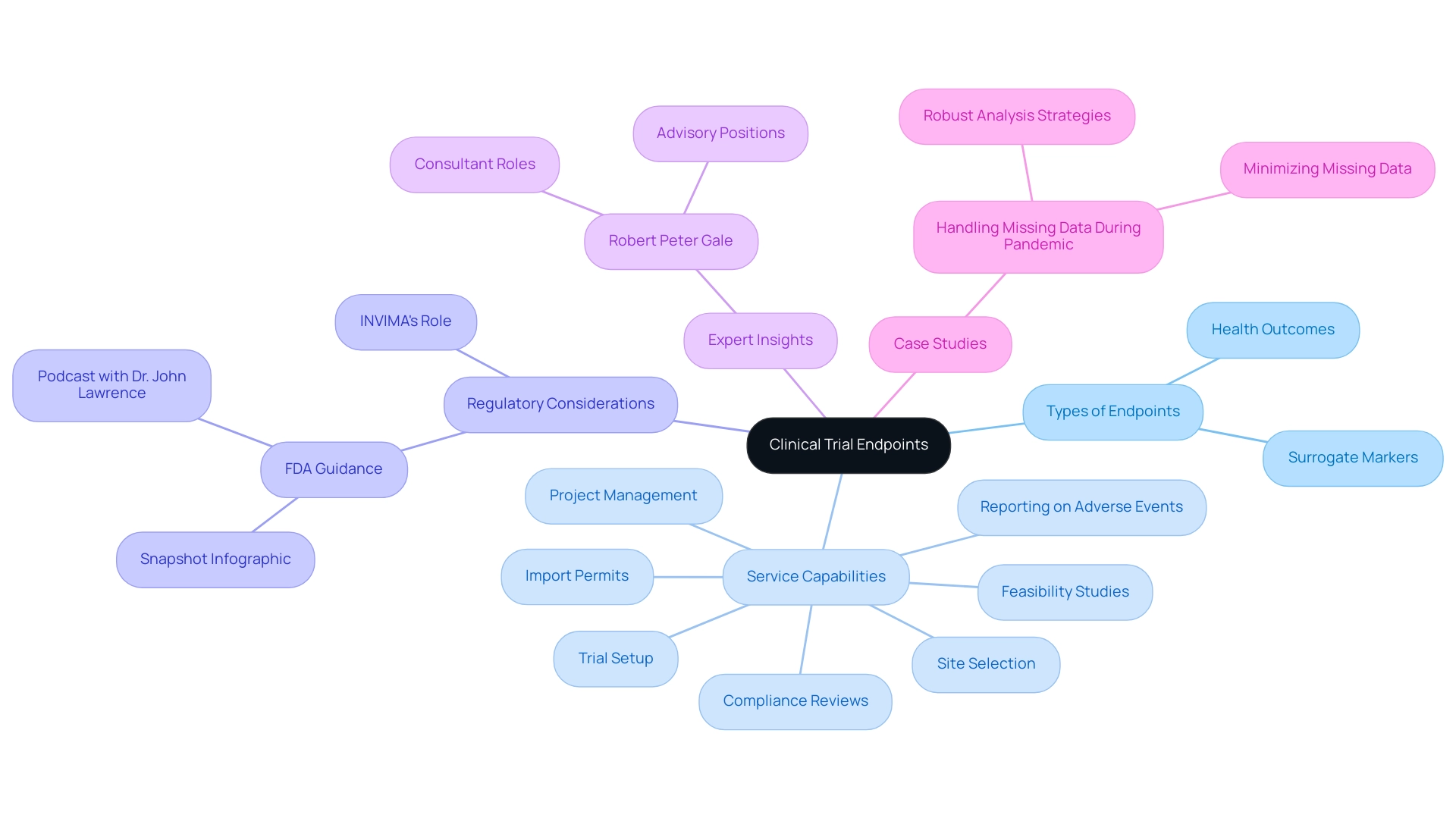
Through expert insights and case studies, the discussion highlights the importance of meticulous endpoint planning in ensuring reliable and actionable results in the pursuit of innovative therapies.
Defining Clinical Trial Endpoints: An Overview
In the context of clinical trials, it is important to understand what are endpoints in clinical trials, as they signify particular events or results that researchers seek to measure within a medical investigation, acting as essential indicators for assessing the efficacy of a treatment or intervention. These points can encompass health outcomes, such as survival rates or enhancements in symptoms, along with surrogate markers—indirect measures that indicate treatment effectiveness. A thorough grasp of goals is essential, as they not only determine the project's objectives but also impact the choice of statistical analyses needed for interpreting results, especially when competing events, such as relapse versus death, may influence outcomes.
Therefore, understanding what are endpoints in clinical trials is crucial for evaluating the effectiveness of medical studies and plays a significant role in regulatory submissions and approvals. Our service capabilities include vital components such as:
- Feasibility studies
- Site selection
- Compliance reviews
- Trial setup
- Import permits
- Project management
- Reporting on serious and non-serious adverse events
This ensures that outcomes are effectively integrated into the design and execution of research studies. Recent guidance from the FDA, presented in a three-page 'Snapshot' infographic and discussed in a podcast with Dr. John Lawrence, emphasizes the changing nature of outcome selection and its significance within regulatory frameworks.
The continuous discussion regarding targets, including their definitions and importance, is highlighted by expert insights from Robert Peter Gale, who stresses that clearly defined goals are essential for ensuring strong research outcomes. Moreover, the case analysis titled 'Handling Missing Data During Pandemic' demonstrates effective strategies created to tackle missing data while ensuring thorough assessment of primary efficacy and safety objectives, additionally emphasizing the necessity for careful selection of goals in medical research. Furthermore, the effect of Medtech research on local economies, encompassing job creation and healthcare enhancement, underscores the wider importance of our services, while INVIMA's function as a regulatory body guarantees adherence and supervision in the research process.
Types of Endpoints in Clinical Trials: Primary, Secondary, and Beyond
In clinical studies, understanding what are endpoints in clinical trials is essential, as outcomes are usually classified into two main types: primary and secondary outcomes. The primary goal serves as what are endpoints in clinical trials, acting as the main result that the study is intended to assess and offering a direct indication of the research's primary aim. In cancer trials, this might encompass overall survival rates, a crucial metric for assessing treatment efficacy.
For instance, the analysis of survival by tumor response discussed by Anderson et al. highlights how these access points can directly influence treatment evaluations. Conversely, secondary outcomes help answer what are endpoints in clinical trials by providing additional insights into the treatment's effects, which may include factors such as quality of life assessments or progression-free survival rates.
Moreover, exploratory objectives can be included, helping to create hypotheses for future research.
Understanding what are endpoints in clinical trials is crucial for precise interpretation of study outcomes and their consequences for patient care. An examination of randomized controlled studies (RCTs) in cardiovascular medicine emphasized a lack of agreement on the optimal methods for choosing and documenting these outcomes, highlighting the necessity for a sophisticated approach to interpreting RCT results, as mentioned in the case study titled 'Best Practices for Reporting RCT Outcomes.' As Robert Peter Gale, a notable consultant in oncology, expresses, effective outcome categorization directly affects the reliability and applicability of research results.
With recent statistics showing a common false positive rate of 5% (0.05), the cumulative false positive rates demonstrate the increasing complexity of assessment—rising to:
- 9.75% with two tests
- 40% with ten tests
- 64% with twenty tests
- 92% with fifty tests
Such insights highlight the essential importance of classification in research studies, influencing both research outcomes and medical decision-making.
The Importance of Endpoint Selection in Clinical Trials
Choosing suitable targets is a crucial aspect of clinical trial design, as understanding what are endpoints in clinical trials profoundly impacts the trial's validity and the interpretation of its results. Researchers must navigate various influencing factors, including the specific disease state, the characteristics of the patient population, and the available treatment options when establishing criteria. The challenge lies in ensuring that these targets are not only clinically meaningful and measurable but also reflective of genuine patient benefits.
Regulatory agencies closely scrutinize what are endpoints in clinical trials due to their implications for the approval process of new therapies. As observed by Mei-Jie Zhang, PhD, 'The ability to properly analyze results of clinical studies, especially randomized controlled studies (RCT), is a necessary skill for every physician.' This highlights the importance of choice selection, particularly in understanding what are endpoints in clinical trials, as incorrect decisions can jeopardize study results.
For instance, the case study titled 'Bias in Treatment Effect Estimates' highlights that open-label studies may experience bias due to missing visits correlated with treatment type. Implementing mitigating strategies, such as ensuring consistent follow-up and utilizing statistical methods to address missing data, is essential to avoid skewed treatment effect estimates stemming from absent data. Additionally, data shows that a considerable portion of research studies encounter difficulties in determining what are endpoints in clinical trials, highlighting the necessity for careful evaluation and strong rationale for outcome decisions.
Thus, guaranteeing that research studies yield dependable and practical outcomes depends on tackling these challenges efficiently.
Emerging Trends: Digital and Novel Endpoints in Clinical Trials
The scenery of clinical studies is experiencing a notable change because of the incorporation of digital and innovative measures, a transition driven by technological progress and changing patient requirements. Digital points, derived from wearable devices and mobile health applications, yield real-time data on patient outcomes, enhancing the granularity of information collected throughout trials. This real-time data collection enables a more nuanced understanding of treatment effects compared to traditional episodic assessments.
Concurrently, novel endpoints, which encompass diverse measures such as patient-reported outcomes and biomarkers, raise the question of what are endpoints in clinical trials, as they are increasingly recognized as vital components in capturing the full spectrum of treatment impact. These developments align closely with the growing emphasis on patient-centered care, ensuring that research remains relevant and responsive to patient experiences and expectations. Tackney MS highlights this transition by stating,
Unleashing the full potential of digital outcome measures in research requires addressing eight critical questions.
Moreover, the recent multi-stakeholder Knowledge Exchange event underscored the significance of cooperation and early involvement with regulators to improve digital outcomes, tackling issues such as patient adherence and study design. A significant example of the decentralization of medical evaluations through digital technologies demonstrates this method; the use of wearable devices and smartphone applications permits assessments to gauge health outcomes in participants' selected locations, facilitating high-frequency and sensitive measurements. As we advance into 2024, emerging trends suggest a sustained emphasis on the use of wearable technology and digital interfaces, highlighting the necessity for interdisciplinary cooperation and inventive study designs that prioritize patient involvement and compliance.

Impact of Endpoints on Clinical Trial Outcomes and Regulatory Approval
The choice of targets in clinical trials carries significant implications for both study outcomes and the subsequent regulatory approval of new therapies. Regulatory agencies, especially the FDA, place significant emphasis on outcome data when assessing the efficacy and safety of treatments. Clearly defined and strategically selected targets can streamline regulatory reviews, thereby increasing the likelihood of approval.
In contrast, poorly defined parameters can result in ambiguous findings, potentially complicating the approval process. A representative of a drug regulatory agency remarked,
There are a couple of companies who have approached us prior to proceeding with anything, seeking guidance, obtaining an agreement, then moving forward with the testing. And we see that those companies that come in this way, they just go through the system without any problems.
This emphasizes the significance of comprehensive planning regarding what are endpoints in clinical trials. Furthermore, studies that employ the Clinical Dementia Rating Sum of Boxes (CDR-SB) as a main objective have shown larger sample sizes compared to those that do not, emphasizing the importance of choosing suitable objectives. As shown by the systematic survey of primary outcomes in current Phase II/III studies for Alzheimer's Disease published in Alzheimer Dis Assoc Disord 2020, the strategic choice of outcomes is essential not only for the validity of research but also for the successful market introduction of new treatments.
Furthermore, the case analysis titled 'Tools for Clinical Trial Design' explores various instruments available for trialists, including the STEEP criteria and ESMO-MCBS, which seek to standardize outcome definitions. Despite the availability of these tools, the study found that less than one-third of experiments met the ESMO-MCBS thresholds for meaningful clinical benefit, indicating a need for improved study design. Katherine Ruiz, a specialist in Regulatory Affairs for medical devices and in vitro diagnostics in Colombia, emphasizes the importance of understanding what are endpoints in clinical trials as part of a comprehensive strategy for outcome selection, ensuring adherence to national requirements, including trial setup, ethics committee approvals, and monitoring of serious and non-serious adverse events.
For further inquiries regarding what are endpoints in clinical trials or to seek guidance, individuals are encouraged to contact the authors of the alert or their Hogan Lovells attorney, thereby ensuring a thorough understanding of endpoint selection and its implications.
Conclusion
Selecting and defining endpoints in clinical trials is not merely a procedural task; it is a foundational element that shapes the entire research process and influences regulatory outcomes. The article has highlighted the importance of various types of endpoints, including primary, secondary, and exploratory measures, and their roles in providing meaningful insights into treatment efficacy. The complexities involved in endpoint selection underscore the necessity for meticulous planning, as improper choices can lead to biases and ambiguous results that may hinder the approval of new therapies.
Emerging trends in digital and novel endpoints signify a transformative shift in clinical research, driven by technological advancements and a growing emphasis on patient-centered care. The integration of real-time data collection from wearable devices and mobile health applications not only enhances the granularity of information but also aligns research with patient experiences and expectations. This evolution is crucial for ensuring that clinical trials remain relevant and capable of delivering actionable results.
Ultimately, the careful selection and definition of endpoints are pivotal for the success of clinical trials. They directly impact not only study outcomes but also the regulatory approval process, determining the pathway for innovative therapies to reach patients. As the field continues to evolve, a commitment to rigorous endpoint planning will be essential in navigating the complexities of clinical research and ensuring that trials yield reliable and meaningful results.
Frequently Asked Questions
What are endpoints in clinical trials?
Endpoints in clinical trials are specific events or results that researchers aim to measure within a medical investigation, serving as indicators for assessing the efficacy of a treatment or intervention.
What types of outcomes are classified as endpoints in clinical trials?
Outcomes are typically classified into two main types: primary outcomes, which indicate the main result the study is designed to assess, and secondary outcomes, which provide additional insights into the treatment's effects.
Can you give examples of primary outcomes in clinical trials?
In cancer trials, a primary outcome might include overall survival rates, which are crucial for evaluating treatment efficacy.
What are secondary outcomes in clinical trials?
Secondary outcomes provide further insights into the treatment effects and may include quality of life assessments or progression-free survival rates.
What is the significance of understanding endpoints in clinical trials?
Understanding endpoints is essential for the precise interpretation of study outcomes and their implications for patient care, as well as for regulatory submissions and approvals.
What role does the FDA play in the context of clinical trial endpoints?
The FDA provides guidance on outcome selection, emphasizing its significance within regulatory frameworks, as highlighted in recent communications such as infographics and podcasts.
What are exploratory objectives in clinical trials?
Exploratory objectives are additional goals that can help generate hypotheses for future research beyond the primary and secondary outcomes.
How do endpoints influence statistical analyses in clinical trials?
The choice of endpoints impacts the statistical analyses needed for interpreting results, especially when competing events may influence outcomes.
Why is careful selection of endpoints crucial in medical research?
Careful selection of endpoints is vital for ensuring strong research outcomes and effective assessment of primary efficacy and safety objectives.
What are the implications of false positive rates in clinical trials?
The cumulative false positive rates increase with the number of tests conducted, highlighting the complexity of assessment and the importance of endpoint classification in influencing research outcomes and medical decision-making.




