Overview
The International Classification of Functioning, Disability, and Health (ICF) is a comprehensive framework that provides a standardized language for understanding health conditions, functioning, and disability in medical terms. The article emphasizes that the ICF's holistic approach enhances communication among healthcare providers, supports effective treatment planning, and facilitates the systematic collection of disability statistics, thereby improving patient care outcomes.
Introduction
The International Classification of Functioning, Disability, and Health (ICF) stands as a pivotal framework in the realm of healthcare, offering a comprehensive lens through which health and disability can be understood and addressed.
Developed by the World Health Organization, the ICF not only standardizes the language surrounding health conditions but also emphasizes the complex interactions between individual health and various contextual factors, including environmental and personal influences.
This multifaceted approach is essential for healthcare professionals, guiding them in the assessment, classification, and treatment of functioning and disability.
As the ICF continues to evolve, particularly with the introduction of its new web-based version, its application across clinical practice, health documentation, and interdisciplinary collaboration becomes increasingly critical.
This article delves into the significance of the ICF, exploring its components, recent developments, and its role in shaping effective healthcare strategies and outcomes.
Understanding the International Classification of Functioning (ICF)
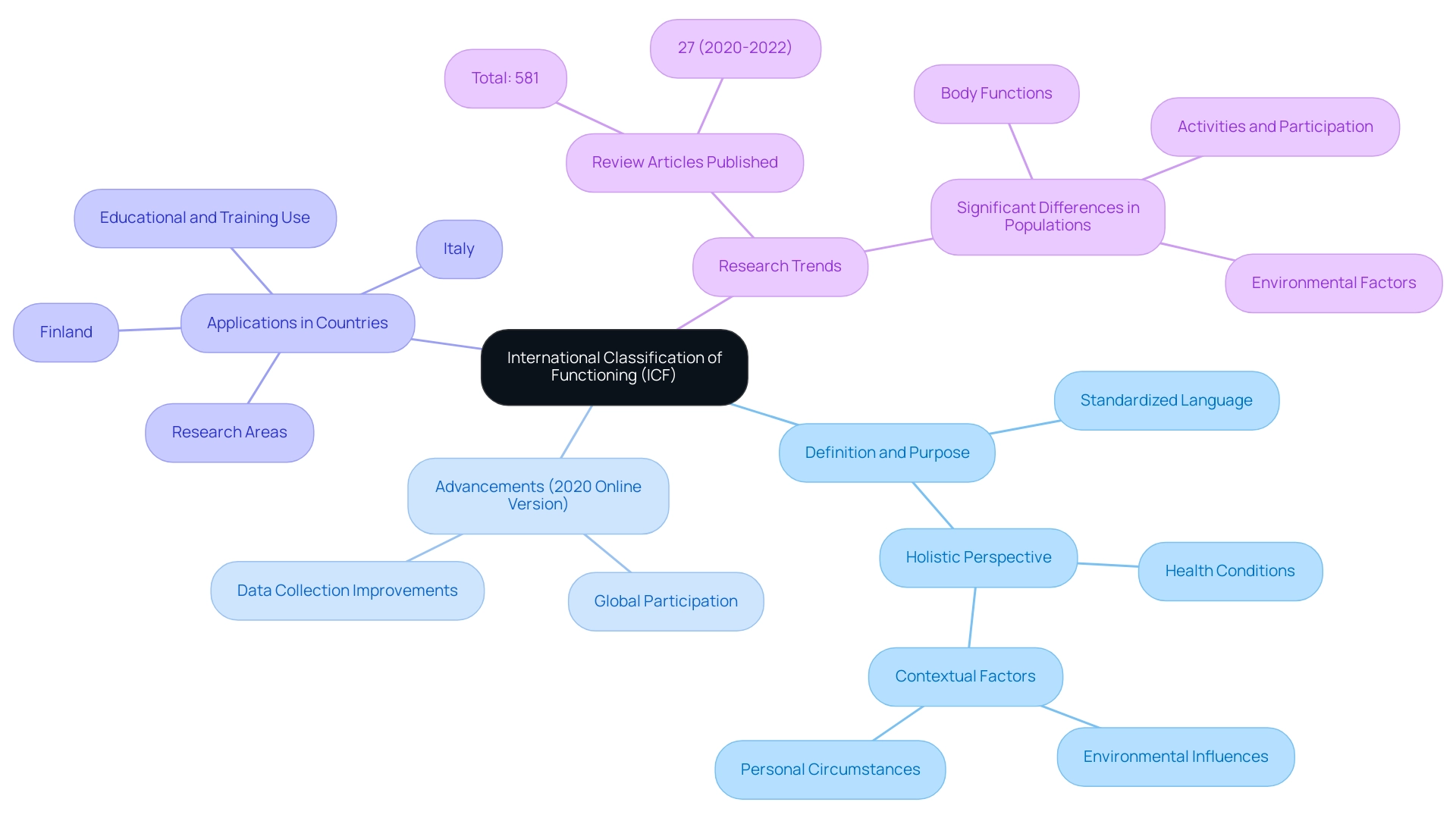
The International Classification of Functioning, Disability, and Health (ICF), created by the World Health Organization (WHO), is essential for understanding what does ICF mean in medical terms and for expressing well-being and related conditions. This comprehensive system not only provides a standardized language but also underscores the intricate interplay between health conditions and contextual factors, which include environmental influences and personal circumstances. Such a holistic perspective is crucial for healthcare professionals, as it supports the assessment and classification of functioning and limitations, which relates to what does ICF mean in medical terms, while guiding the crafting of effective treatment plans and interventions.
Recent advancements in the ICF, especially the new online version launched in 2020, seek to improve global participation and significance in collecting data on functioning and impairment. A survey on the future of ICF implementation suggests that despite existing limitations, there are elements fostering ICF application, particularly in countries like Italy and Finland, where its use spans educational, training, and research areas. Significantly, 581 review articles on the ICF were published, with 27% of these reviews appearing between 2020 and 2022, which raises the question of what does ICF mean in medical terms, emphasizing the model's increasing importance in recent research.
As Leonardi et al. have observed, the ICF has made considerable progress in altering the view of impairment over the past twenty years, reinforcing its significance in medical care and aiding in enhanced wellness results globally.
The Role of ICF in Clinical Practice and Health Documentation
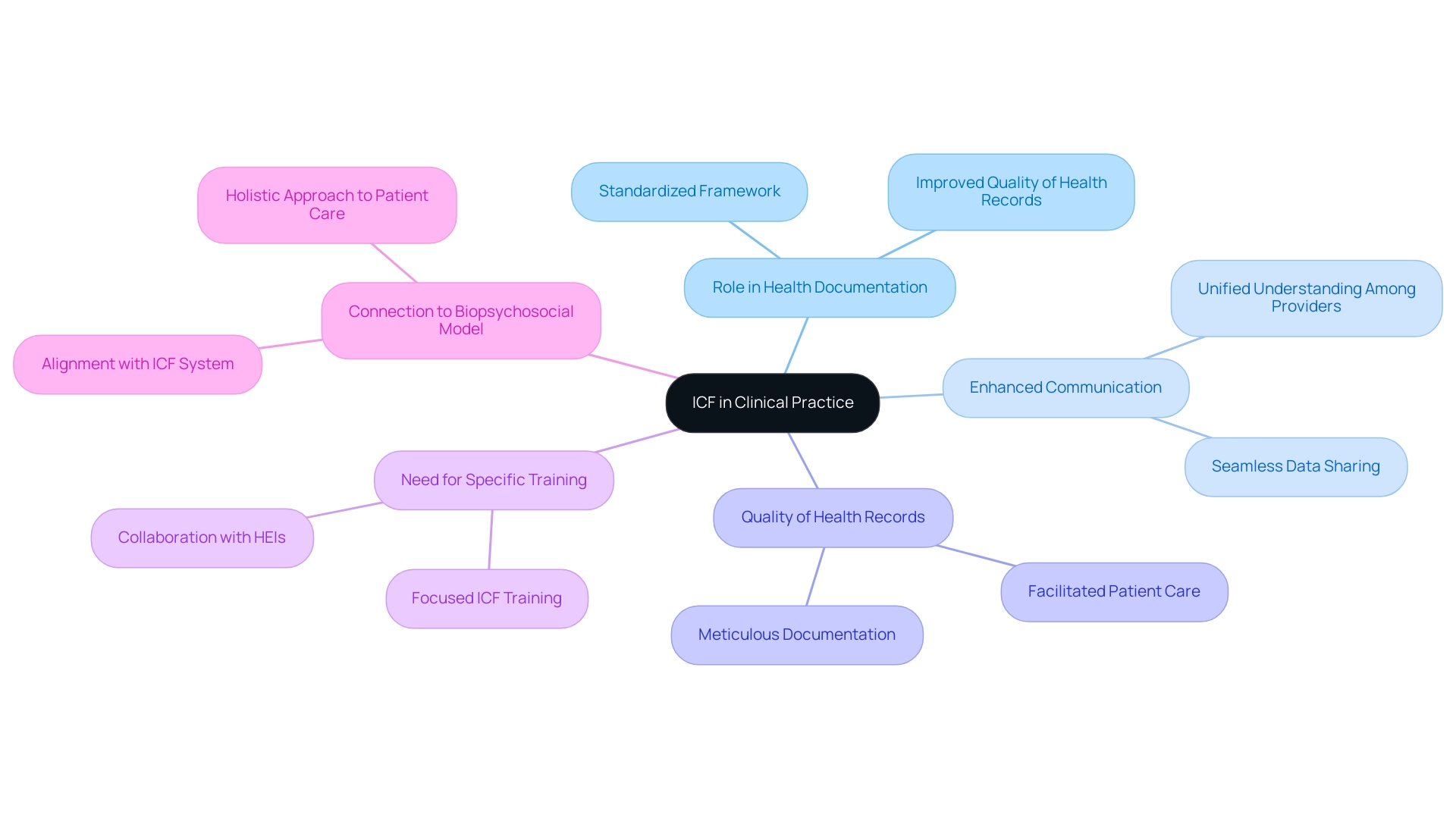
The International Classification of Functioning, Disability, and Health (ICF) is essential to clinical practice and medical documentation, raising the question of what does ICF mean in medical terms as it offers a thorough and standardized structure for evaluating patient functioning and disability. This classification system significantly enhances communication among healthcare providers, enabling all team members to share a unified understanding of a patient's condition. Furthermore, the implementation of ICF supports the meticulous documentation of health information, leading to improved quality in health records and facilitating seamless data sharing among providers—an essential component for coordinated patient care.
Notably, extended ICFs, some reaching up to 25 pages, may take between 34 to 48 minutes to read, highlighting the depth of information they encompass. By effectively incorporating ICF into clinical practice, healthcare professionals can better address patient needs and customize interventions accordingly. Jaana Paltamaa emphasizes this point, stating,
Specific ICF training is needed in clinical practice: ICF education is not enough.
This highlights the significance of focused training to maximize the advantages of the ICF model in enhancing patient care outcomes. As the healthcare landscape evolves, it is important to ask what does ICF mean in medical terms, as its role in standardizing health documentation becomes increasingly vital, impacting both patient care and health documentation practices. Furthermore, upcoming advancements should concentrate on improving cooperation and guidance between higher education institutions (HEIs) and clinical practice to ensure that the ICF model is effectively incorporated into training programs.
Furthermore, the biopsychosocial model of illness, as mentioned in a recent article in Clinical Rehabilitation, aligns closely with the ICF system, emphasizing the need for a holistic approach to patient care. Furthermore, the balance between utilizing data analytics and AI tools in clinical trials, as highlighted in a case study, illustrates the operational efficiencies that can be achieved while implementing ICF in clinical settings.
Components and Structure of the ICF
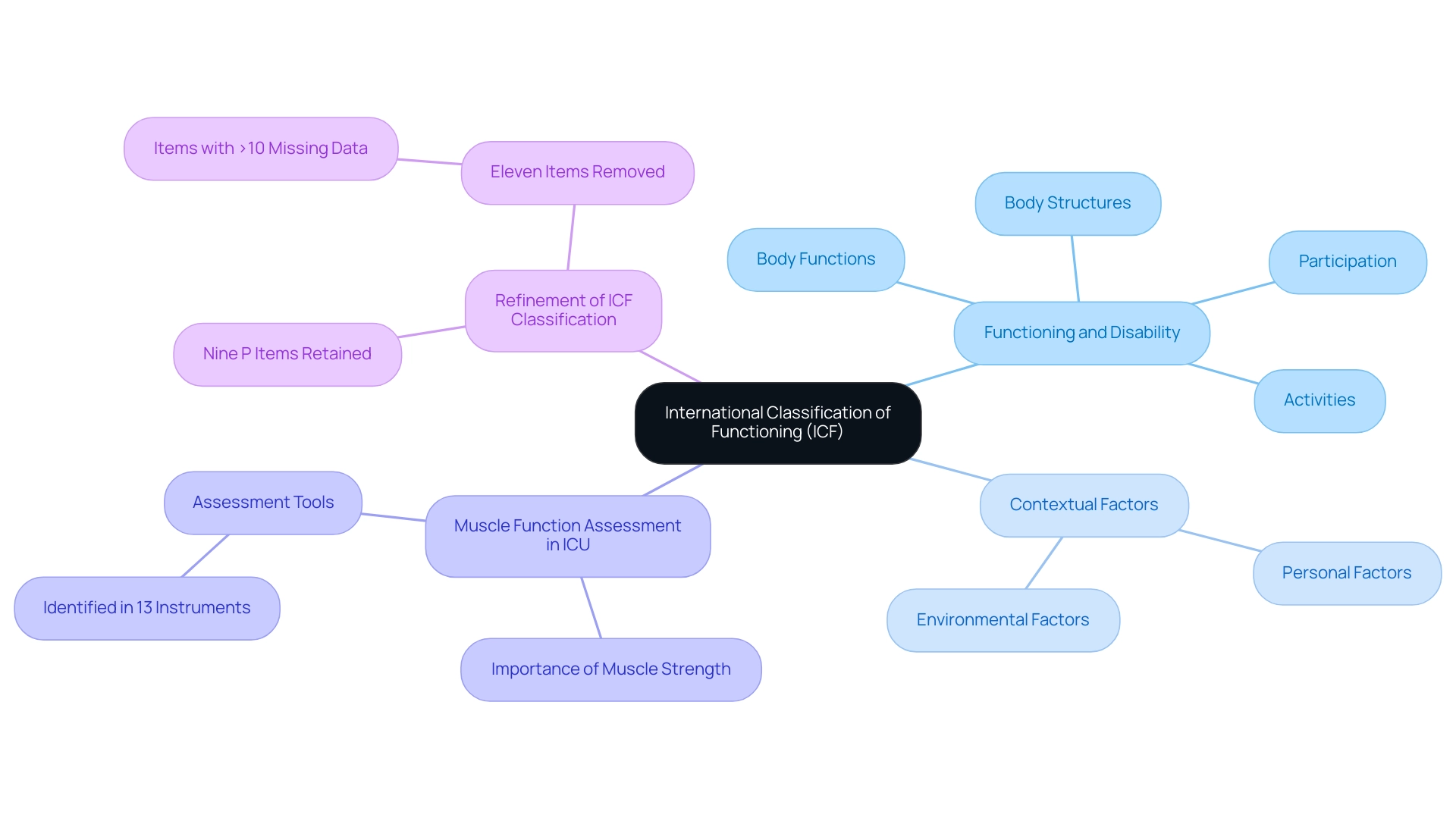
The International Classification of Functioning (ICF), which prompts the inquiry of what does ICF mean in medical terms, is fundamentally organized into two primary components: Functioning and Disability, alongside Contextual Factors. The Functioning and Disability component encompasses essential elements such as body functions and structures, activities, and participation. In contrast, Contextual Factors encompass both environmental and personal elements that significantly impact outcomes.
The ICF structure utilizes a comprehensive classification system that helps explain what does ICF mean in medical terms by incorporating different categories and qualifiers to clarify the severity and impact of medical conditions. This organized method is essential for healthcare practitioners as it promotes a nuanced comprehension of what does ICF mean in medical terms and the intricate interaction among various elements influencing personal well-being. For instance, recent research highlights that complete impairment is observed over 95% of the time in clinical populations, underscoring the necessity of thorough assessments in these settings.
Furthermore, a case study focusing on muscle function assessment in Intensive Care Units (ICUs) revealed that muscle strength is critical for evaluating clinical interventions and determining suitable physical exercise regimens. This research recognized the muscle function area in 13 various assessment tools, emphasizing what does ICF mean in medical terms for efficiently applying the ICF model to evaluate functioning and impairment. Additionally, it is noteworthy that nine P items were retained while eleven items were removed from the item pool, including those with greater than 10% missing data, reflecting ongoing efforts to refine the ICF classification system.
As Diane Dixon stated, 'All authors read and approved the final manuscript,' highlighting the collaborative effort in this research. The ICF thus proves to be an invaluable resource for healthcare providers, helping them understand what does ICF mean in medical terms while addressing patient needs with precision and depth.
ICF as a Framework for Disability Statistics and Health Information
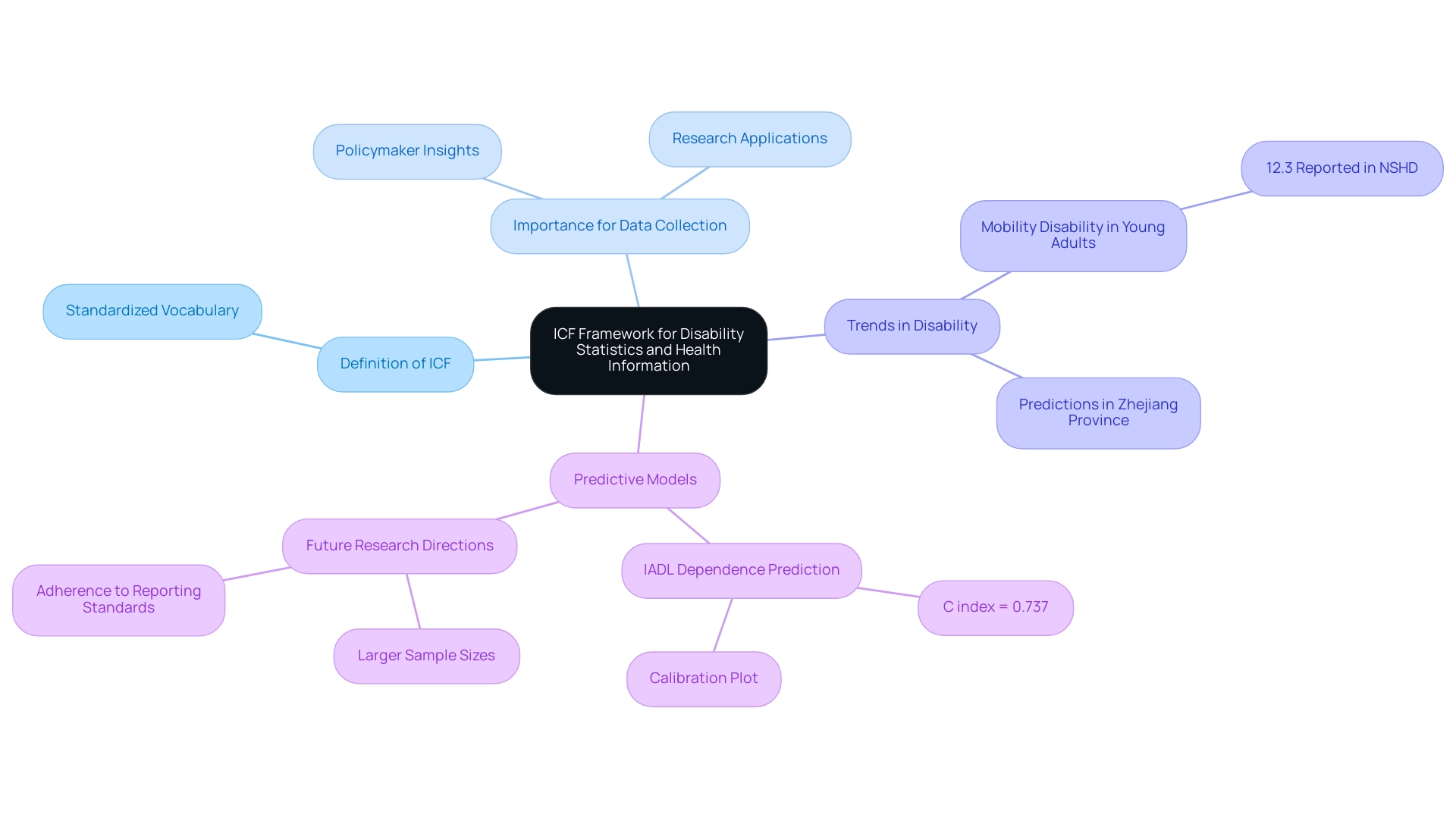
The International Classification of Functioning, Disability and Health (ICF) is essential for understanding what does ICF mean in medical terms, as it provides a foundational framework for the systematic collection and analysis of disability statistics and wellness information. By providing a standardized vocabulary for describing medical conditions, the ICF addresses what does icf mean in medical terms and facilitates the aggregation of data across diverse populations and settings. This consistency is crucial for policymakers and researchers aiming to identify trends, allocate resources effectively, and devise targeted interventions aimed at enhancing health outcomes.
Recent forecasts concerning impairment trends in areas like Zhejiang Province suggest an upward trajectory of rates with age, highlighting the necessity of reliable data. Significantly, mobility impairment was reported by 12.3% of young adults in the NSHD, emphasizing the importance of addressing challenges across all age groups. Moreover, in a study by Lu (2022) involving inpatients aged 60 and older in a Zunyi City hospital, 65.95% were classified as having mild to severe disability based on comprehensive assessments.
This illustrates the practical use of the ICF model and answers what does icf mean in medical terms in real-world situations. Furthermore, Zhang et al. have emphasized that the ICF is effective in predicting Instrumental Activities of Daily Living (IADL) dependence in individuals aged 60 and above, achieving an acceptable discrimination index (C index = 0.737) and calibration, with calibration plots aligning closely with the 45-degree line.
The utilization of the ICF within information systems significantly enhances the quality of collected data, which raises the question of what does icf mean in medical terms, ensuring it accurately reflects the complexities of well-being and functioning in various populations. As research continues to evolve, it will be essential to adhere to reporting standards and utilize larger sample sizes to improve predictive models and further our understanding of disability statistics through the ICF framework.
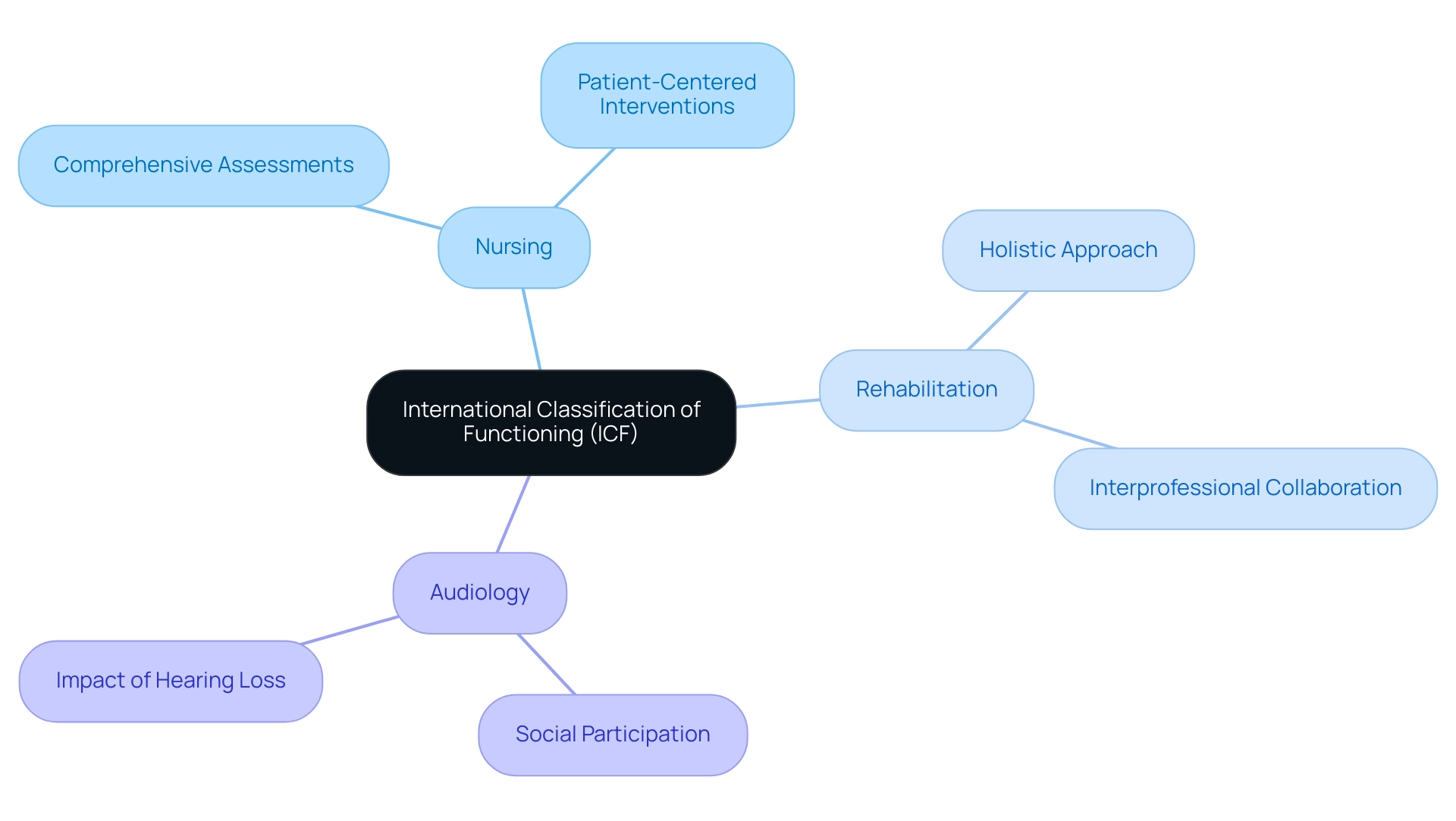
Interdisciplinary Applications of ICF in Health Care
The International Classification of Functioning, Disability and Health (ICF) raises the question of what does ICF mean in medical terms, as it offers extensive interdisciplinary applications that permeate various healthcare sectors, notably nursing, rehabilitation, and audiology. In nursing, the ICF, or what does ICF mean in medical terms, serves as a crucial tool, guiding comprehensive assessments and interventions by framing patient functioning in the context of their medical conditions. For instance, in audiological management, the ICF allows practitioners to evaluate how hearing loss affects daily activities and social participation.
This holistic approach not only informs clinical decision-making but also fosters collaboration across disciplines, ultimately enhancing the quality of care provided to patients. Research conducted at the IRIS Institute highlights what does ICF mean in medical terms, as it underpins the development of an interprofessional culture and promotes person-centered practices, ensuring that all facets of a patient's health and well-being are integrated into treatment planning. Notably, a statistic revealed that 14 out of 16 parents felt involved and taken seriously in this process, underscoring the effectiveness of the ICF in promoting such involvement.
As one parent stated, "We felt involved and taken seriously," which reinforces the positive results associated with the ICF model. Furthermore, Francescutti et al. emphasized the need for a common disability assessment framework in 2009, which aligns with the relevance of the ICF in contemporary healthcare settings.
Additionally, the World Health Organization's Interprofessional Education Framework illustrates that improved education and collaborative practice among health professionals can significantly strengthen health systems, facilitating effective interdisciplinary applications of the ICF in healthcare settings.
Conclusion
The International Classification of Functioning, Disability, and Health (ICF) serves as a crucial framework in the healthcare landscape, emphasizing the intricate relationship between health conditions and contextual factors. By providing a standardized language and a comprehensive approach, the ICF enhances communication among healthcare professionals, facilitating better assessments, classifications, and treatment plans for patients. Recent advancements, including the new web-based version, further underscore its growing relevance in clinical practice and research, particularly as healthcare systems continue to evolve.
The ICF's structured components—Functioning and Disability alongside Contextual Factors—enable healthcare providers to gain a nuanced understanding of individual health dynamics. This holistic framework not only aids in meticulous health documentation but also fosters interdisciplinary collaboration, ensuring that all aspects of a patient’s experience are considered in care strategies. As evidenced by various studies, the ICF enhances the quality of data collected, allowing for more informed decision-making and resource allocation in healthcare settings.
In conclusion, the ongoing integration and application of the ICF framework are vital for improving health outcomes and advancing the understanding of disability across diverse populations. As healthcare professionals embrace this comprehensive approach, they can better address the complexities of patient needs, ultimately contributing to a more effective and inclusive healthcare system. The ICF stands not only as a tool for assessment but as a transformative framework that shapes the future of healthcare delivery and policy.
Frequently Asked Questions
What is the International Classification of Functioning, Disability, and Health (ICF)?
The ICF is a system created by the World Health Organization (WHO) that provides a standardized language for understanding and expressing well-being, health conditions, and their interplay with contextual factors such as environmental influences and personal circumstances.
How does the ICF support healthcare professionals?
The ICF aids healthcare professionals by providing a comprehensive framework for assessing and classifying functioning and limitations, which informs the development of effective treatment plans and interventions.
What advancements have been made to the ICF recently?
Recent advancements include the launch of a new online version of the ICF in 2020, aimed at improving global participation and enhancing the collection of data on functioning and impairment.
What is the significance of the ICF in medical documentation?
The ICF enhances communication among healthcare providers by offering a thorough and standardized structure for evaluating patient functioning and disability, leading to improved health records and coordinated patient care.
How long can extended ICFs be, and what does this indicate?
Extended ICFs can be up to 25 pages long and may take between 34 to 48 minutes to read, indicating the depth of information they contain and the comprehensive nature of the classification system.
What training is needed for effective use of the ICF in clinical practice?
Specific ICF training is needed in clinical practice, as emphasized by Jaana Paltamaa, to maximize the advantages of the ICF model and enhance patient care outcomes.
How does the ICF relate to the biopsychosocial model of illness?
The ICF aligns closely with the biopsychosocial model of illness, emphasizing the importance of a holistic approach to patient care that considers biological, psychological, and social factors.
What is the future focus for ICF advancements?
Future advancements should concentrate on improving cooperation and guidance between higher education institutions and clinical practice to ensure effective incorporation of the ICF model into training programs.

