Introduction
The journey of medical device development is a multifaceted process that requires meticulous planning, rigorous testing, and adherence to stringent regulatory standards. From the initial spark of innovation to the final market launch, each phase plays a crucial role in ensuring that devices not only meet clinical needs but also comply with safety regulations.
In regions such as Latin America, companies face unique hurdles that can complicate this journey, including regulatory complexities and resource constraints. Recent collaborations between industry leaders aim to streamline these processes, enhancing both communication and efficiency.
Understanding the intricacies of this development framework is essential for stakeholders, as it underscores the collaborative efforts necessary to transform innovative concepts into viable healthcare solutions.
The following sections will delve into the key phases of medical device development, the challenges faced, and the regulatory considerations that shape the landscape of this vital industry.
An Overview of the Medical Device Development Process
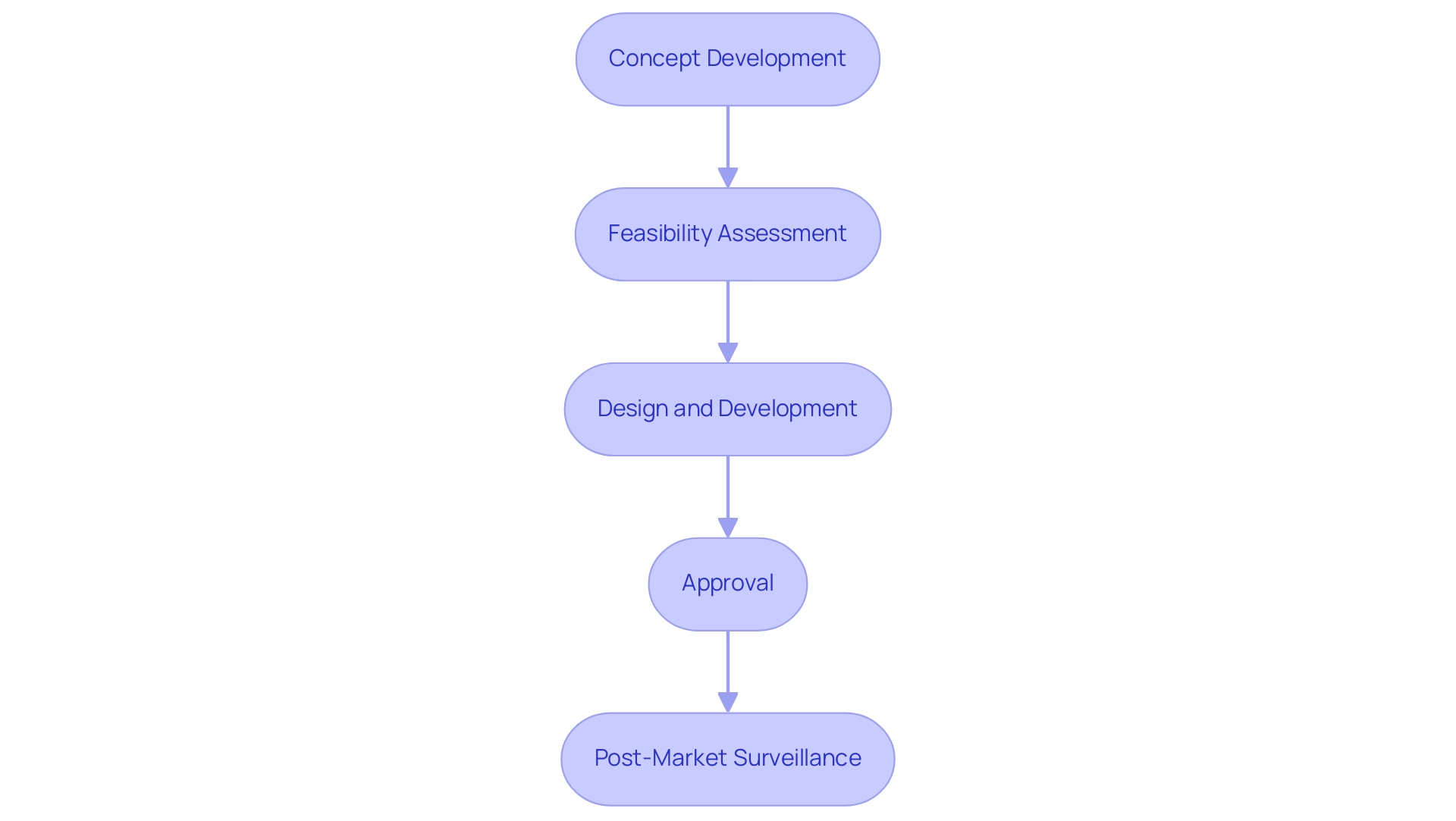
The process of medical device development signifies a complex journey, starting with the generation of innovative ideas and concluding with the successful introduction of a product in the market. This intricate process of Medical Device Development typically unfolds in several pivotal stages:
- Concept development
- Feasibility assessment
- Design and development
- Approval
- Post-market surveillance
Notably, the average time for medical device development from concept to market is approximately 3 to 7 years, influenced by rigorous compliance and testing requirements.
In Latin America, Medtech companies encounter unique challenges, including:
- Compliance hurdles
- Fragmented resources
- Language barriers
- Financial limitations
- Prolonged subject recruitment timelines
These challenges can impede effective collaboration with American clinical trial clients. Recent collaborations, such as that between Greenlight Guru and bioaccess™, aim to bridge these gaps and accelerate the clinical trial process in the region, particularly for early-stage studies like First-In-Human trials. This partnership specifically focuses on streamlining compliance processes and enhancing communication, thereby addressing the financial and recruitment challenges faced by Medtech companies.
Additionally, navigating the regulatory environment is essential; INVIMA, Colombia's National Food and Drug Surveillance Institute, plays a key role in overseeing product approvals and ensuring adherence to health standards, classified as a Level 4 health authority by PAHO/WHO. As automation becomes increasingly important in streamlining quality systems, stakeholders must also keep abreast of software advancements that enhance compliance and operational efficiency, as noted by AAMI. Grasping this comprehensive framework is crucial for stakeholders within the healthcare equipment industry, as it highlights the teamwork required for medical device development to convert a concept into a feasible product.
The Key Phases of Medical Device Development
The Medical Device Development process is structured and comprises several crucial phases, each designed to ensure that the final product is both safe and effective. These phases include:
-
Concept Development: This initial stage involves identifying a specific clinical need followed by brainstorming potential solutions, shaping the foundation of the apparatus.
-
Feasibility Assessment: Here, the technical and commercial viability of the suggested apparatus is evaluated.
This assessment is pivotal, as it determines whether the concept can successfully transition to the next phase. Recent statistics indicate that successful feasibility assessments can significantly enhance project outcomes in medical device development, with studies showing that projects with thorough feasibility evaluations have a 30% higher success rate in subsequent phases. Furthermore, the knowledge of specialists like Katherine Ruiz, an affairs expert with experience at INVIMA, guarantees that these evaluations adhere to local regulations, including acquiring necessary import permits and following health ministry requirements.
-
Design and Development: This phase focuses on creating prototypes and conducting iterative testing, enabling refinements to the design based on feedback and performance metrics.
-
Regulatory Approval: Once the design is finalized, it must be submitted for review by regulatory bodies, such as the FDA or INVIMA, to ensure compliance with established safety standards and regulations. The review process is essential for reducing risks related to equipment use.
-
Trial Setup and Monitoring: This phase involves selecting appropriate research sites and principal investigators, ensuring that the clinical study is conducted in compliance with local regulations. Continuous monitoring during the trial is essential to maintain data integrity and participant safety.
-
Market Launch: The final phase involves introducing the product to the market, accompanied by strategic marketing efforts to reach potential users.
Each of these stages is essential to the overall success of medical device development, ensuring that healthcare instruments fulfill both compliance standards and clinical requirements. Furthermore, insights from industry experts suggest that thorough feasibility assessments during the early stages can lead to higher success rates in subsequent phases, reinforcing the importance of a robust planning strategy. Moreover, the impact of Medtech clinical studies on local economies cannot be overlooked; they create jobs, promote economic growth, and improve healthcare, leading to international collaboration and recognition.
Navigating Challenges in Medical Device Development
The terrain of medical device development is becoming more intricate, characterized by major obstacles that encompass technical issues, strict compliance barriers, and fierce market rivalry. A notable issue in medical device development is the necessity for devices to comply with the rigorous standards established by governing bodies, such as INVIMA in Colombia, which oversees the approval of medical devices and ensures adherence to health standards. This can lead to substantial delays in the approval process.
For instance, an ASPE report highlighted a 16.6% increase in drug prices during shortages, illustrating the financial implications of administrative inefficiencies and the broader impact on healthcare systems. Hospitals often face challenges in procuring drugs during these shortages, resulting in higher costs and staff overtime, underscoring the need for effective resource allocation. The AHA has urged Congress to support policies that ensure hospitals have the necessary resources to provide continuous care.
Furthermore, those involved in Medical Device Development must adeptly navigate funding constraints and resource allocation, especially in the critical early stages where investment is paramount. Efficient communication among different stakeholders—such as engineers, clinicians, and compliance experts—is crucial to guarantee that all viewpoints are incorporated into the medical device development process. Insights from case studies illustrate the importance of early collaboration with oversight authorities and statisticians to enhance the structure of statistical analysis plans.
Experts like Katherine Ruiz, a regulatory affairs authority, and Juan Cuya, MD, a Clinical Trial Associate, emphasize the necessity of understanding local regulations and conducting thorough feasibility studies for successful Medical Device Development project outcomes. Addressing technology-related challenges, especially in AI and ML applications in the creation of in-vivo diagnostic tools, is vital. Furthermore, it is crucial to handle the import permit and nationalization of investigational items and to uphold strict reporting on study status, inventory, and adverse events.
By proactively addressing these complex challenges, project teams can significantly improve their chances of successful results in clinical trials, ultimately contributing to job creation, economic growth, and healthcare enhancement in local economies.
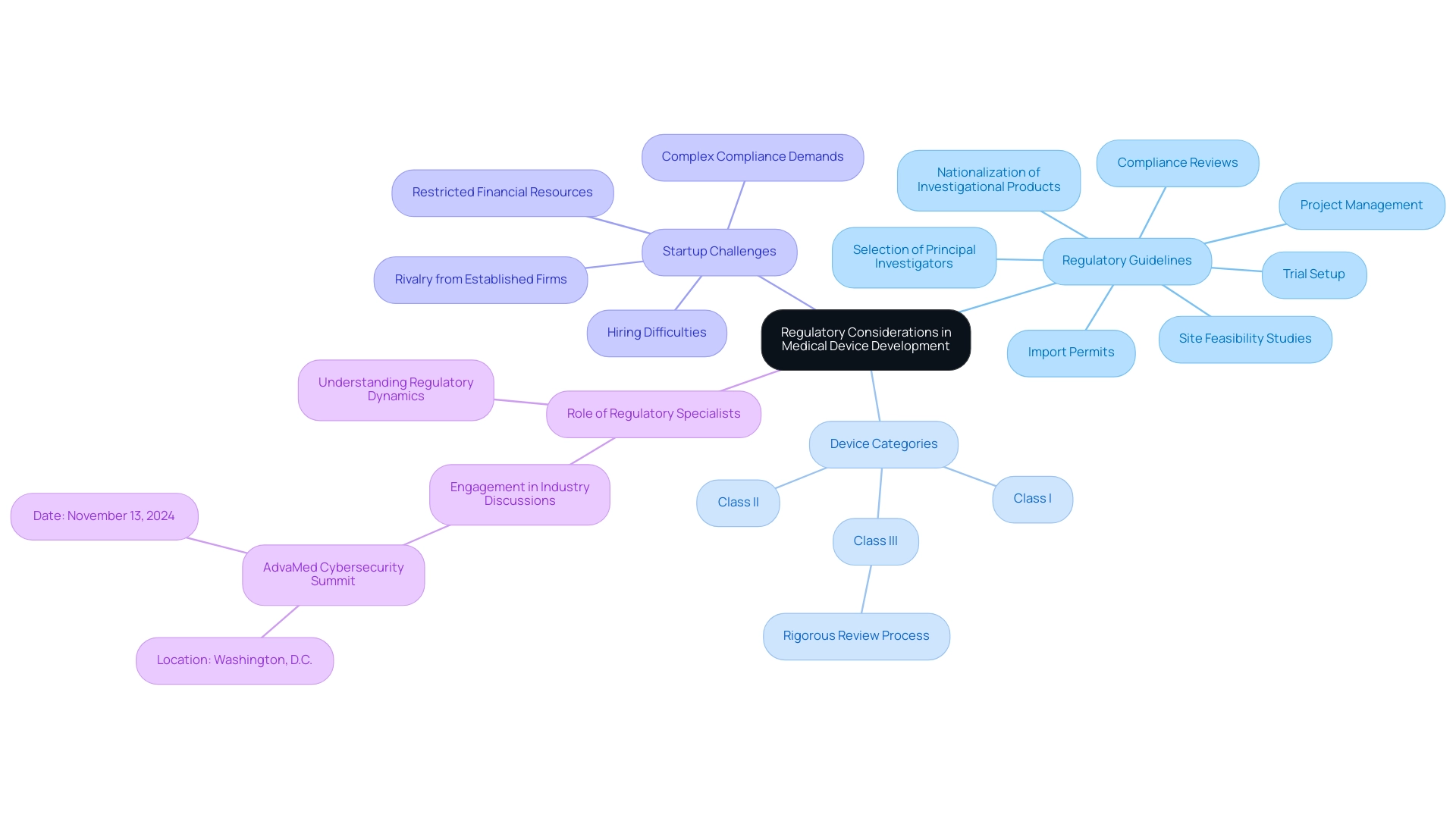
Regulatory Considerations in Medical Device Development
Regulatory considerations are paramount in medical device development for healthcare tools, ensuring their safety and efficacy for public use. In Colombia, the National Food and Drug Surveillance Institute (INVIMA) plays a crucial role in this process, overseeing the marketing and manufacturing of health products. Founded in 1992, INVIMA is acknowledged as a Level 4 health authority by the Pan American Health Organization (PAHO)/World Health Organization (WHO), indicating its proficiency in overseeing health-related products.
Developers must navigate a comprehensive set of guidelines that include:
- Site feasibility studies
- Selection of principal investigators
- Compliance reviews
- Trial setup
- Import permits
- Nationalization of investigational products
- Project management
The categorization of a healthcare instrument, whether Class I, II, or III, greatly impacts its oversight process and the examination it will face. Class III items, for instance, are subject to the most rigorous review processes due to their higher associated risks.
Furthermore, healthcare equipment startups frequently encounter obstacles like:
- Complex compliance demands
- Rivalry from established firms
- Hiring difficulties
- Restricted financial resources
Regulatory specialists, such as Katherine Ruiz, who has considerable experience with INVIMA, highlight the significance of comprehending these dynamics to effectively maneuver through the intricate realm of trials for healthcare equipment. Engaging with regulatory guidelines and participating in industry discussions, such as the upcoming AdvaMed Cybersecurity Summit on November 13, 2024, can provide essential insights into best practices and FDA approval processes, ultimately enhancing medical device development and the market readiness of healthcare products.
Furthermore, comprehensive reporting on study status, inventory, and serious and non-serious adverse events is crucial for maintaining transparency and compliance throughout the trial process.
Post-Market Surveillance and Continuous Improvement
Post-market surveillance serves as a pivotal element in the lifecycle of healthcare products, especially in Medical Device Development, by providing essential oversight of performance and safety after public release. This process encompasses the systematic collection of data regarding adverse events, conducting regular evaluations, and implementing necessary modifications driven by user feedback. In Colombia, bioaccess™ stands out as a vetted CRO and consulting partner, assisting U.S. healthcare product companies in navigating the complexities of INVIMA regulations.
INVIMA (Colombia National Food and Drug Surveillance Institute) plays a crucial role in this context, overseeing the compliance and safety of healthcare instruments, monitoring their performance, and suggesting technical standards for their manufacturing and marketing, all while maintaining its classification as a Level 4 health authority by PAHO/WHO. Recent advances in surveillance techniques, including the application of deep learning models—such as a ResNet-50 architecture for classifying fundus images into diabetic retinopathy grades, supported by an additional out-of-distribution set of 7,767 very low-quality images—demonstrate the potential for enhancing monitoring accuracy through technology. Furthermore, MUKS tests utilize a black-box task classifier for dimensionality reduction and apply two-sample KS tests to softmax predictions, providing a clearer understanding of the methodologies used in post-market surveillance.
Ongoing enhancement methods are essential in medical device development, perfecting these products, tackling new challenges, and ensuring adherence to changing legal frameworks. For instance, the evaluation criteria established for shift detection highlight the importance of achieving high detection rates and low false positive rates. These metrics are crucial for a reliable monitoring framework that identifies distribution shifts effectively.
By prioritizing robust post-market surveillance as part of medical device development, companies can significantly enhance patient safety, uphold product quality, and cultivate trust among healthcare providers and patients alike. As noted by Lisa M. Koch, 'Continuous improvement in medical device development safety is not merely a regulatory obligation but a commitment to advancing healthcare standards.' Moreover, the impact of clinical studies conducted by Medtech associates in Colombia creates ripples in the local economy, fostering job creation, economic growth, and improved healthcare outcomes.
For example, these studies have led to the establishment of new healthcare facilities and increased employment opportunities in research and development sectors, thereby strengthening international collaboration.
Conclusion
The medical device development process is a complex journey that demands careful navigation through various stages, from concept generation to market launch. Each phase, including:
- Concept development
- Feasibility assessment
- Design and development
- Regulatory approval
- Post-market surveillance
plays a critical role in ensuring that devices are not only innovative but also safe and effective. The challenges faced by Medtech companies in regions like Latin America—such as regulatory hurdles, financial constraints, and resource fragmentation—underscore the importance of collaboration and strategic partnerships to enhance communication and streamline processes.
In particular, the role of regulatory bodies like INVIMA in Colombia is pivotal, as they oversee compliance and safety standards that significantly impact development timelines. Understanding the nuances of these regulatory frameworks is essential for stakeholders, as is the recognition that thorough feasibility assessments can lead to higher success rates in subsequent phases. Moreover, the integration of advanced technologies and continuous monitoring practices in post-market surveillance can further enhance device safety and efficacy, fostering trust among healthcare providers and patients.
Ultimately, the development of medical devices is not just a technical endeavor; it is a collaborative effort that requires input from various stakeholders, including engineers, clinicians, and regulatory experts. As the medical device landscape continues to evolve, embracing innovation while adhering to stringent regulatory requirements will be crucial for transforming ideas into viable healthcare solutions. By addressing the unique challenges within the industry and prioritizing robust development strategies, stakeholders can contribute significantly to improved healthcare outcomes and economic growth in their communities.
Frequently Asked Questions
What are the main stages of the medical device development process?
The medical device development process typically unfolds in several pivotal stages: 1) Concept development, 2) Feasibility assessment, 3) Design and development, 4) Approval, and 5) Post-market surveillance.
How long does it usually take to develop a medical device from concept to market?
The average time for medical device development from concept to market is approximately 3 to 7 years, influenced by rigorous compliance and testing requirements.
What challenges do Medtech companies face in Latin America?
Medtech companies in Latin America encounter unique challenges including compliance hurdles, fragmented resources, language barriers, financial limitations, and prolonged subject recruitment timelines.
How can collaborations help Medtech companies in Latin America?
Collaborations, such as that between Greenlight Guru and bioaccess™, aim to bridge gaps and accelerate the clinical trial process, particularly for early-stage studies like First-In-Human trials, by streamlining compliance processes and enhancing communication.
What role does INVIMA play in medical device development in Colombia?
INVIMA, Colombia's National Food and Drug Surveillance Institute, oversees product approvals and ensures adherence to health standards, classified as a Level 4 health authority by PAHO/WHO.
What is the significance of feasibility assessments in medical device development?
Feasibility assessments evaluate the technical and commercial viability of a proposed device and can significantly enhance project outcomes, with studies showing that projects with thorough feasibility evaluations have a 30% higher success rate in subsequent phases.
What is involved in the design and development phase of medical device development?
The design and development phase focuses on creating prototypes and conducting iterative testing, allowing refinements based on feedback and performance metrics.
What is required for regulatory approval in medical device development?
The finalized design must be submitted for review by regulatory bodies, such as the FDA or INVIMA, to ensure compliance with established safety standards and regulations.
What is the importance of post-market surveillance in medical device development?
Post-market surveillance provides essential oversight of performance and safety after public release, including systematic data collection regarding adverse events and regular evaluations to implement necessary modifications.
How do clinical studies conducted by Medtech associates impact local economies?
Clinical studies lead to job creation, promote economic growth, and improve healthcare, ultimately strengthening international collaboration and recognition.




