Introduction
Informed consent is a fundamental pillar of ethical research, ensuring that participants are not only willing but also fully informed about the studies in which they engage. This complex process goes far beyond merely obtaining a signature; it encompasses a series of critical components designed to empower individuals with the knowledge necessary to make informed decisions.
- From articulating the purpose of the research to outlining potential risks and benefits, the informed consent document serves as a vital communication tool.
- However, despite the established guidelines and ethical frameworks, significant challenges remain in achieving true comprehension among participants.
This article delves into the core components of informed consent, additional considerations for specific populations, and best practices for drafting effective forms, ultimately highlighting the ongoing need for clarity and understanding in the informed consent process.
Core Components of Informed Consent Documents
Informed consent documents are essential for ensuring that individuals are fully educated about what must be included in the informed consent for research. Key components of these documents typically include:
- Purpose of the Research: A clear explanation detailing the objectives of the research and its significance in advancing medical knowledge.
- Procedures Involved: Comprehensive descriptions of the tasks individuals will undertake, encompassing any interventions or assessments they will experience.
- Risks and Benefits: An outline of potential risks or discomforts individuals might face, alongside the expected benefits both for the people involved and the broader society.
- Confidentiality: A description of the measures implemented to safeguard individuals' information and the degree to which confidentiality will be maintained throughout the research.
- Voluntary Participation: A clear statement reaffirming that involvement is voluntary, allowing individuals the freedom to withdraw at any time without any repercussions.
- Contact Information: Relevant details on whom to reach out to with questions about the study or inquiries regarding individuals' rights.
These components are designed to empower participants with the knowledge necessary for understanding what must be included in the informed consent for research, enabling them to make informed decisions about their involvement. Significantly, the historical case of Schloendorff v. Society of New York Hospital (1914) established the foundational principle that patients must agree to medical procedures, which remains a vital aspect of clinical research today. A study conducted by Harrison in 1995 found that 95-100% of adult patients understood issues related to confidentiality, while 83-100% grasped the potential side effects.
Nevertheless, despite high satisfaction indicated by research subjects concerning the awareness process, worries persist about their understanding of essential information. This discrepancy highlights the importance of not only acquiring approval but also ensuring that participants genuinely comprehend what must be included in the informed consent for research, making knowledgeable agreement a cornerstone of patient-centered care and medical ethics. As noted, "authorized agreement evolved to not only include a patient's signature but also the process of clear communication... ultimately making it a cornerstone of patient-centered care and medical ethics."
Furthermore, the case study titled "Participant Understanding vs. 'Satisfaction'" emphasizes that although research subjects indicate high contentment with the awareness process, they frequently possess a limited grasp of essential elements of the trial. This corresponds with recent discoveries that team members voice concerns regarding individuals' grasp of the information given during the approval process, highlighting the persistent difficulties in attaining genuine understanding in the agreement.
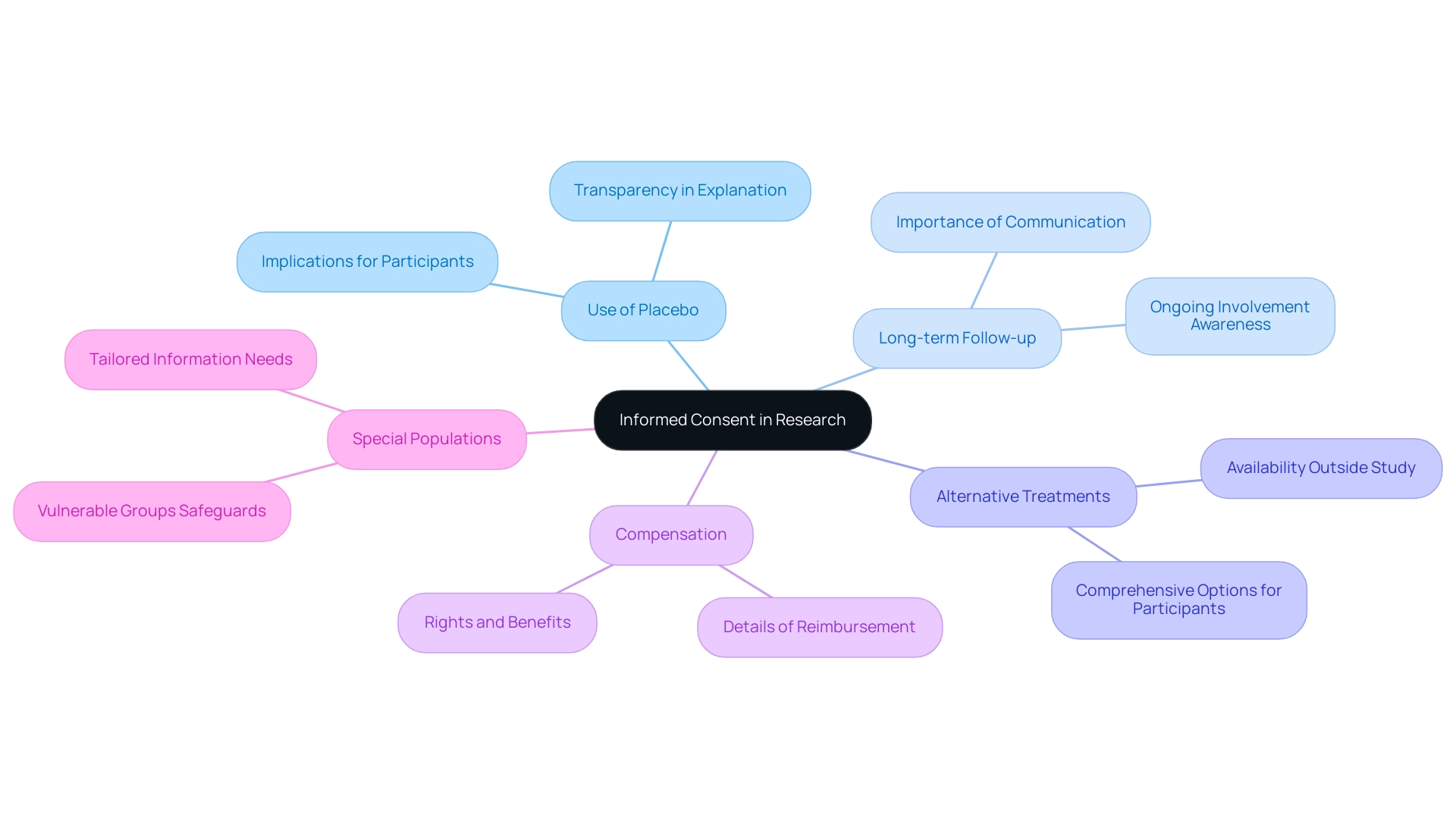
Additional Considerations for Informed Consent in Research
In addition to the basic elements of consent, it is crucial for researchers to understand what must be included in the informed consent for research, taking into account the specific details of the study and the populations involved. These elements include:
- Use of Placebo: A transparent explanation regarding the use of placebo treatments, clarifying their implications for those involved, is essential. This clarity is essential considering the ongoing discussion about the effect of placebo use on knowledge consent.
- Long-term Follow-up: Individuals should be made aware of any necessary long-term follow-up required after the conclusion of the study, ensuring they comprehend the ongoing nature of their involvement.
- Alternative Treatments: It is important to discuss the availability of alternative treatments or procedures that may be accessible outside the parameters of the study, providing individuals with a comprehensive view of their options.
- Compensation: Clear details regarding any compensation or reimbursement for involvement must be communicated to individuals, emphasizing their rights and potential benefits.
- Special Populations: Additional safeguards and tailored information are particularly necessary for vulnerable groups, including children and individuals with cognitive impairments. Emmanuel and Boyle highlighted the necessity to rethink the approval procedure within the clinical research field, particularly for these groups.
These factors aim to guarantee that individuals are not only knowledgeable about what must be included in the informed consent for research but can give agreement that is truly aware and voluntary. Worryingly, studies show that the percentage of individuals who completely grasp the concept of agreement has not risen in the last 30 years, emphasizing a crucial area for enhancement. The systematic review titled The Reality of Patient Agreement: Empirical Studies on Patient Comprehension found that many patients continue to struggle with understanding the approval process, underscoring the necessity for continuous enhancement of patient agreement practices.
It is important to note that the elements discussed here are not exhaustive and serve as an informational piece, rather than a comprehensive guideline.
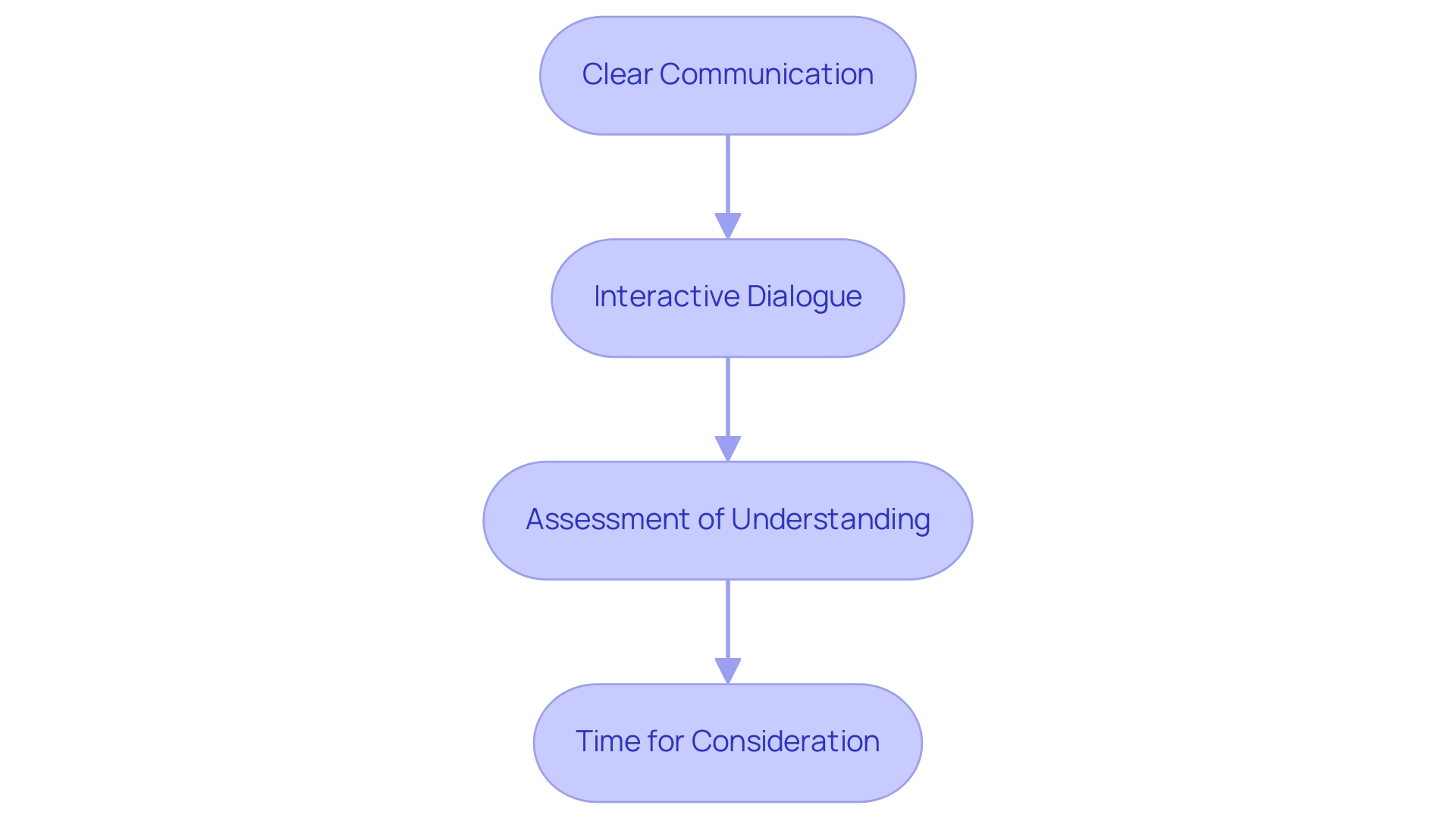
The Informed Consent Process: Ensuring Participant Understanding
The informed consent process encompasses what must be included in the informed consent for research, going beyond simple signature gathering to ensure that individuals have a thorough understanding of the research in which they are contemplating involvement. Key steps in this process include:
- Clear Communication: Researchers must convey information in straightforward language, steering clear of technical jargon that could confuse potential participants.
- Interactive Dialogue: Encouraging a two-way conversation allows individuals to engage actively, enabling them to ask questions and express any concerns, thereby enhancing their understanding of the details.
- Educational Materials: Supplementing verbal discussions with written documents, videos, or other educational resources can reinforce the information shared, catering to diverse learning styles. The effectiveness of the teach-back method, where individuals are encouraged to repeat information in their own words, has been shown to significantly enhance understanding in patient education contexts.
- Assessment of Understanding: It is crucial for researchers to evaluate individuals' grasp of the study by prompting them to articulate the study in their own words or to discuss any lingering concerns.
- Time for Consideration: Participants should be afforded adequate time to contemplate their involvement, which allows them to process the information thoroughly before making a decision about what must be included in the informed consent for research. Implementing these steps not only ensures that participants are well-informed but also contributes to their comfort and confidence in their decision to engage in the research. Recent findings indicate that the mean response for overall understanding of clinical trials while signing the agreement form was 4.73 ± 0.46, underscoring the importance of these practices.
As Sasitorn Phumdoung from the Prince of Songkla University suggests, > Also the report part should provide information more on the total scores <, emphasizing the need for comprehensive communication strategies. Furthermore, a case study on the study selection process for a meta-analysis demonstrated a rigorous approach to assessing understanding of informed agreement, ensuring that only relevant studies were included based on eligibility criteria. Enhancing participant understanding is particularly crucial, especially considering the prevalence of lower health literacy among disadvantaged populations, which can impede their participation in clinical trials.
This highlights the necessity for tailored communication strategies that address these disparities.
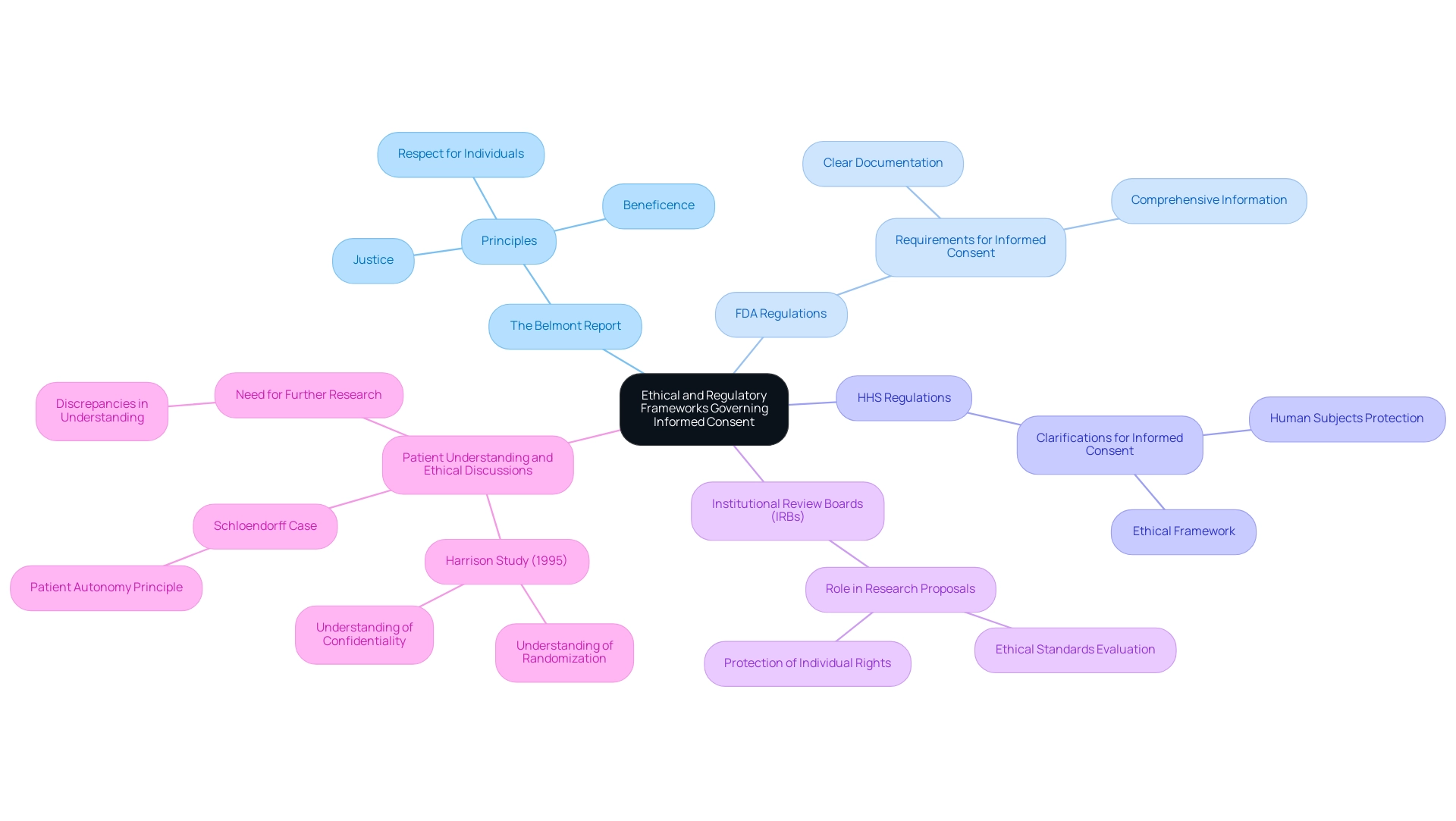
Ethical and Regulatory Frameworks Governing Informed Consent
Informed agreement is framed by a range of ethical and regulatory guidelines that researchers are mandated to follow. These include:
- The Belmont Report: Serving as a cornerstone in ethical research, this report articulates the principles of respect for individuals, beneficence, and justice, which are essential to the process of obtaining agreement. Its influence has shaped the way agreement is understood and implemented in clinical environments.
- FDA Regulations: The Food and Drug Administration outlines specific rules that regulate knowledgeable permission in clinical trials. These regulations emphasize what must be included in the informed consent for research, highlighting the necessity for clear, comprehensive agreement documents that facilitate an informed decision-making process for individuals.
- HHS Regulations: The Department of Health and Human Services has developed additional regulations that clarify what must be included in the informed consent for research involving human subjects, ensuring a robust ethical framework.
- Institutional Review Boards (IRBs): These boards play a crucial role in evaluating research proposals, ensuring that the informed agreement processes align with ethical standards and adequately protect individual rights.
A well-coordinated informed agreement process fosters a culture of trust, respect, and shared responsibility among healthcare professionals and patients, highlighting what must be included in the informed consent for research. Recent research emphasizes the need to explore discrepancies in patients' perceived understanding of agreement versus their actual comprehension, particularly in therapeutic settings. For instance, the Harrison Study (1995) found that while 95–100% of participants understood confidentiality, only 68–96% grasped the concept of randomization.
This ongoing discussion highlights the significance of maintaining the integrity of the knowledgeable agreement process, reflecting the principles established in landmark cases like Schloendorff v. Society of New York Hospital, which affirmed that every adult has the right to decide what shall be done with their own body. Furthermore, as one patient representative pointed out, there are troubling patterns concerning approval practices in Europe, emphasizing the necessity for ethical discussion surrounding knowledgeable agreement. Furthermore, researchers recommend additional studies to bridge the gap between perceived and actual comprehension of agreement, underscoring the continuous challenges in this area.
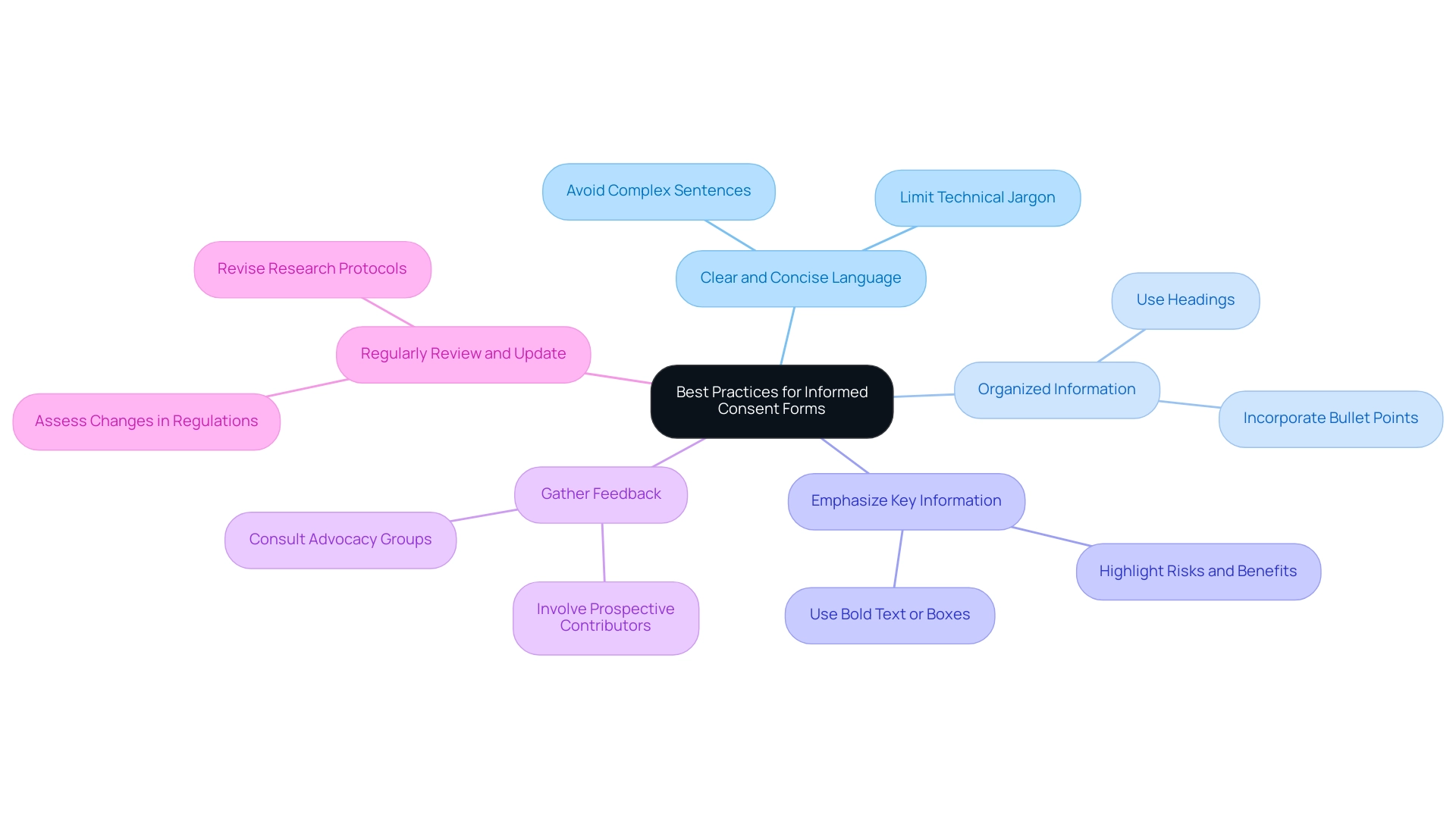
Best Practices for Drafting Effective Informed Consent Forms
A meticulous approach to language, structure, and content is essential for developing effective informed consent forms, especially focusing on what must be included in the informed consent for research. Adhering to best practices can significantly enhance the clarity and effectiveness of these documents:
- Utilize Clear and Concise Language: Simplifying language by avoiding complex sentences and technical jargon enhances readability and comprehension.
- Organize Information Logically: Structuring the document with headings and bullet points allows individuals to navigate the information more easily, facilitating a better understanding of their rights and the research.
- Emphasize Key Information: Highlight critical details, such as potential risks and benefits, using bold text or separate boxes to ensure that attendees can quickly identify essential information.
- Gather Feedback: Involving prospective contributors or advocacy groups for insights before finalizing the form can uncover areas of confusion and enhance clarity.
- Regularly Review and Update Documents: It is crucial to periodically assess and revise permission forms to accommodate changes in regulations or research protocols, ensuring ongoing compliance.
Incorporating these practices not only aligns with ethical standards but also enhances participant comprehension of what must be included in the informed consent for research, fostering informed decision-making. The Montgomery case has highlighted the necessity for healthcare practitioners to prioritize clear communication in the approval process, as it marked a shift away from the previous legal test of duty of care, which required practitioners to act in accordance with acceptable professional standards. Furthermore, the article 'What Is Truly Informed Consent in Medical Practice and What Has the Perception of Risk Got to Do with It?' highlights that patients affected by laws regarding consent should be supported in their decision-making process.
A practical example of best practices can be found in the case study titled 'Screening Processes for Consent Capacity,' which describes informal screening processes that can be used during consent discussions to identify individuals with intellectual disabilities who may struggle with understanding consent-related issues. These screening measures can help ensure that individuals with ID are appropriately informed about research participation, allowing for better inclusion while addressing their understanding of risks and benefits.
Conclusion
Informed consent is a critical component of ethical research, serving as a bridge between participants and researchers. The essential elements of informed consent documents, including:
- Purpose of the research
- Detailed procedures
- Risks and benefits
- Confidentiality
- Voluntary participation
- Contact information
are designed to empower individuals to make informed decisions about their involvement. Despite the historical foundation laid by landmark cases and ongoing regulatory frameworks, challenges persist in ensuring that participants fully comprehend the information presented to them.
Addressing additional considerations, such as:
- The use of placebos
- Long-term follow-up
- Alternative treatments
- Special populations
underscores the complexity of the informed consent process. Researchers must remain vigilant in adapting their communication strategies to meet the diverse needs of participants. The necessity for clear communication, interactive dialogue, and educational materials cannot be overstated, as these practices enhance participant understanding and comfort in the decision-making process.
Ultimately, the informed consent process is not merely a procedural formality but a fundamental ethical obligation that fosters trust and respect in research settings. By adhering to best practices in drafting effective informed consent forms and continuously striving for clarity, researchers can significantly improve the participant experience. The ongoing dialogue surrounding informed consent highlights the importance of bridging the gap between perceived and actual understanding, ensuring that all individuals involved in research are genuinely informed and respected in their autonomy.
Frequently Asked Questions
What are the key components of informed consent documents for research?
Key components typically include the purpose of the research, procedures involved, risks and benefits, confidentiality measures, voluntary participation, and contact information for inquiries.
Why is the purpose of the research important in informed consent?
The purpose provides a clear explanation of the research objectives and its significance in advancing medical knowledge, helping participants understand the study's relevance.
What should be included in the description of procedures involved in research?
The description should comprehensively outline the tasks participants will undertake, including any interventions or assessments they will experience.
What information about risks and benefits is included in informed consent documents?
Informed consent documents outline potential risks or discomforts participants might face, as well as the expected benefits for both the individuals involved and society at large.
How is confidentiality addressed in informed consent?
The documents describe the measures implemented to safeguard participants' information and the extent to which confidentiality will be maintained throughout the research.
What does voluntary participation mean in the context of informed consent?
It means that participation is entirely voluntary, allowing individuals the freedom to withdraw from the study at any time without facing repercussions.
Why is contact information included in informed consent documents?
Contact information is provided so participants can reach out with questions about the study or inquiries regarding their rights.
What historical case established the principle of informed consent in medical procedures?
The historical case of Schloendorff v. Society of New York Hospital (1914) established that patients must agree to medical procedures, a principle that remains vital in clinical research today.
What concerns exist about participants' understanding of informed consent?
Despite high satisfaction regarding the awareness process, there are concerns that participants often have a limited grasp of essential elements of the trial, highlighting the need for genuine understanding.
What additional elements should researchers consider for informed consent?
Researchers should consider the use of placebo treatments, long-term follow-up, alternative treatments, compensation details, and specific safeguards for vulnerable populations.
How have comprehension levels regarding informed consent changed over time?
Studies indicate that the percentage of individuals who fully understand the concept of agreement has not improved in the last 30 years, indicating a critical area for enhancement.
Are the discussed elements of informed consent comprehensive?
No, the elements discussed are not exhaustive and serve as an informational piece rather than a comprehensive guideline.




