Introduction
Informed consent is a cornerstone of ethical practice in therapy, serving as a vital process that empowers patients to make informed decisions about their treatment. This multifaceted concept encompasses key components such as:
- Disclosure
- Comprehension
- Voluntariness
Each plays a critical role in fostering trust and ensuring that patients fully understand their therapeutic options. As the landscape of mental health care evolves, therapists face the challenge of navigating complex ethical and legal considerations while addressing the diverse needs of their patients.
This article delves into the essential elements of informed consent, highlighting the importance of:
- Effective communication
- The impact of cultural sensitivity
- The necessity of tailored approaches to enhance patient engagement and satisfaction
By exploring the challenges and ethical imperatives associated with informed consent, this discussion underscores its significance in establishing a collaborative therapeutic relationship that ultimately leads to improved treatment outcomes.
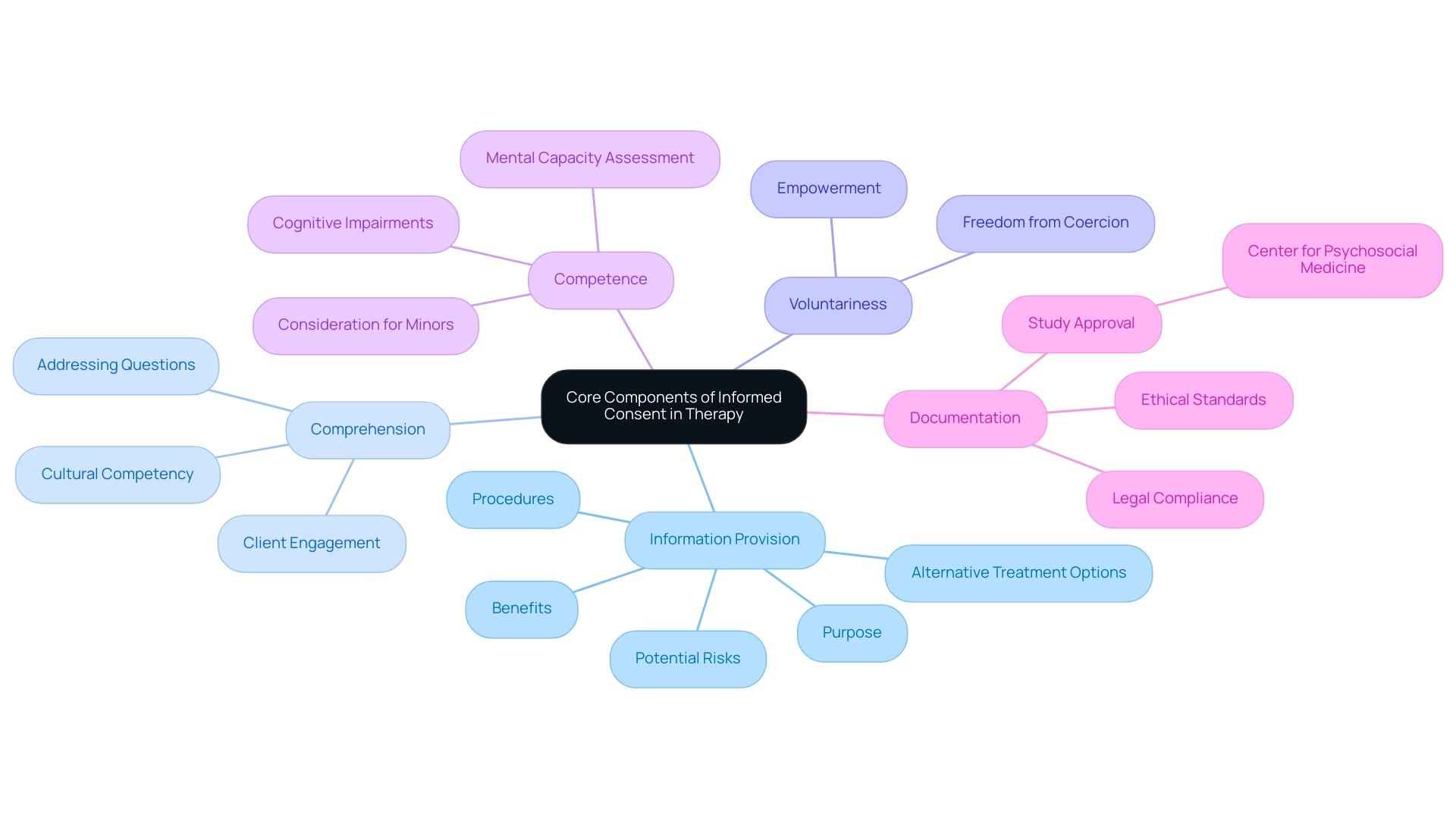
Core Components of Informed Consent in Therapy
A fundamental process in therapy is informed consent, which encompasses what should be included in informed consent for therapy to ensure that individuals are adequately informed and capable of making educated decisions about their treatment. These components encompass:
- Therapists must ensure that individuals are informed about what should be included in informed consent for therapy, detailing its purpose, procedures, potential risks, benefits, and alternative treatment options. This transparency is essential in fostering trust and enhancing understanding for individuals.
- Comprehension: It is vital that individuals not only receive information but also understand it. Therapists should actively engage with clients, encouraging dialogue and addressing any questions to ensure clarity. This aligns with what should be included in informed consent for therapy, as emphasized by the U.S. Department of Health and Human Services in promoting cultural competency in health literacy to cater to diverse patient needs.
- Voluntariness: Consent must be provided freely, without any form of coercion or undue influence. Patients should feel empowered to refuse or withdraw approval at any point during the therapeutic process, reinforcing their autonomy.
- Competence: Patients are expected to have the mental capacity necessary for making knowledgeable decisions about their treatment. Therapists should evaluate a client's competence, especially in situations involving minors or individuals with cognitive impairments, to ensure that agreement is suitably informed.
- Documentation: Thorough documentation of the approval process is crucial. This guarantees that individuals' approval is precisely documented and safely kept, complying with both legal and ethical standards. A recent study highlighted the importance of such documentation and received ethical approval from the local ethics committee of the Center for Psychosocial Medicine, University-Medical Center Hamburg-Eppendorf.
In a relevant finding by Tlach et al., it is noted that, "Because specific mental disorders may be accompanied by different individual needs regarding information about treatment, coping mechanisms, working and living conditions, and self-help." This emphasizes the importance of customized strategies for what should be included in informed consent for therapy, which can significantly enhance individual satisfaction and treatment outcomes. In fact, satisfaction with received information is measured by 8 items on a 4-point Likert scale, with total scores ranging from 8 to 32, underscoring the importance of effectively communicating information to patients.
Additionally, the case study titled 'Model 3: Capacity to Consent' highlights the evaluation of capacity for agreement, achieving acceptable fit indices with CFI > 0.95 and TLI > 0.90. This model offers insights into the factors affecting the ability to agree, illustrating the practical application of these core components in therapy settings. As approved agreement continues to develop, especially in mental health treatment, comprehending these fundamental elements remains crucial for ensuring ethical practice and promoting client trust.
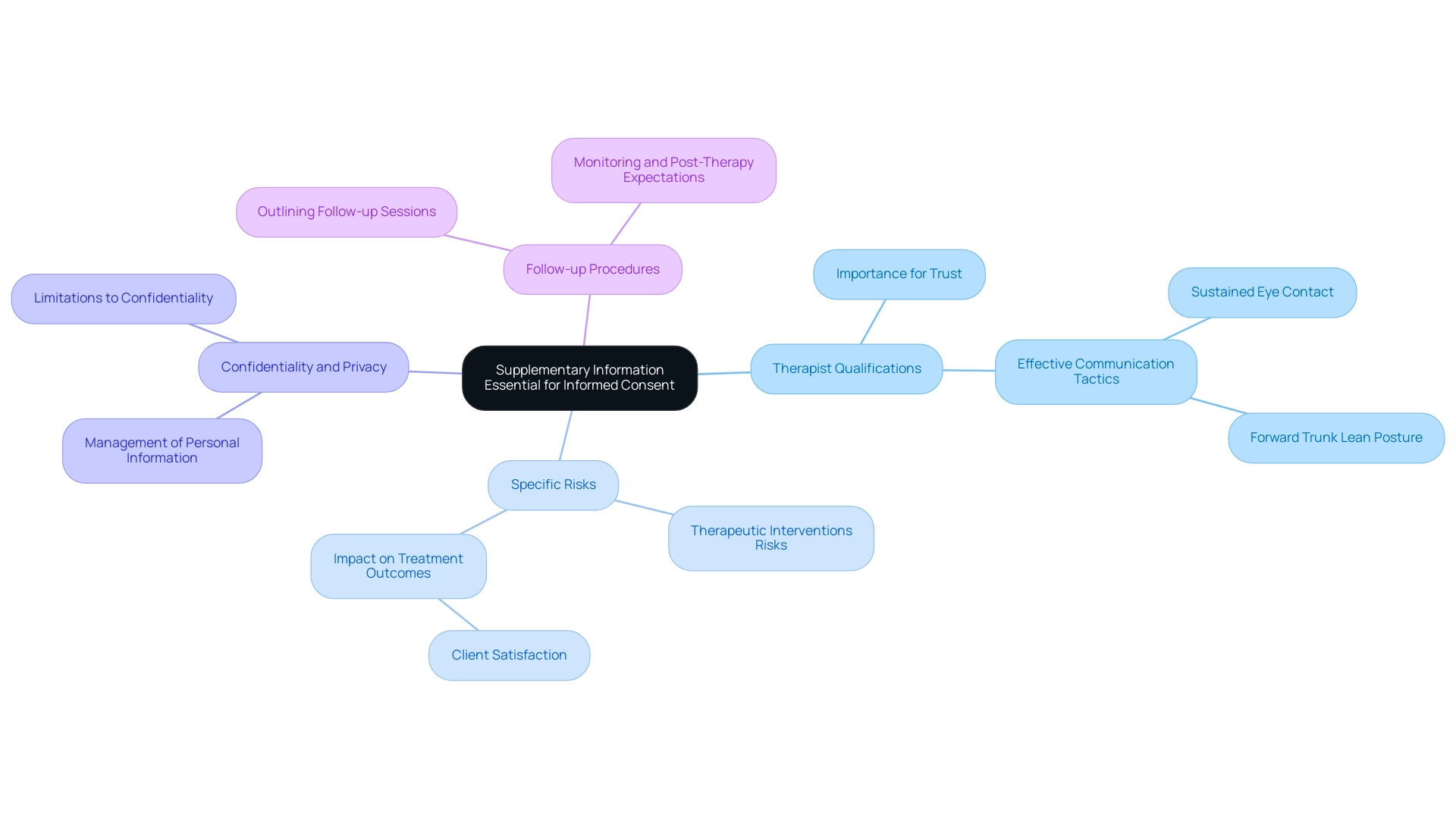
Supplementary Information Essential for Informed Consent
Supplementary information plays a vital role in the informed consent process and encompasses several key components that enhance patient understanding and trust:
- Therapist Qualifications: Disclosing the therapist's credentials, experience, and areas of expertise is essential in fostering trust. Studies indicate that an individual's perception of their therapist's qualifications significantly influences their overall trust in the therapeutic relationship. In fact, the mean score for individuals who feel they can count on their doctor or therapist is only 6.29, indicating a notable concern regarding trust. Dowell and Berman emphasize that clinicians can further enhance credibility by employing effective communication tactics, such as sustained eye contact and a forward trunk lean posture, which can positively influence individuals’ perceptions.
- Specific Risks: In discussing what should be included in informed consent for therapy, it is important to specify the risks associated with particular therapeutic interventions, in addition to the general risks outlined in core consent components. For instance, the side effects of medications or potential emotional distress from specific therapeutic techniques must be clearly communicated to individuals to ensure informed choices. A meta-analysis by Wampold et al. (1997) indicates that understanding these risks can affect treatment outcomes and client satisfaction.
Providing information about what should be included in informed consent for therapy, particularly regarding alternative therapies, empowers individuals in their decision-making process. This transparency can lead to greater involvement and satisfaction with their care.
- Confidentiality and Privacy: Patients should be informed about what should be included in informed consent for therapy, specifically regarding how their personal information will be managed and any potential limitations to confidentiality. Clear communication regarding privacy policies is fundamental to maintaining trust, especially in sensitive healthcare settings.
- Follow-up Procedures: Outlining follow-up sessions, monitoring, and what individuals can expect post-therapy is essential. This information assists individuals in feeling more prepared and secure in their decisions, ultimately enhancing their overall experience. Recent developments in trust and respect scales suggest that understanding these dynamics can significantly influence treatment outcomes, indicating the importance of thorough follow-up communication.
Additionally, a case study titled "Meta-regressions and Subgroup Analyses" found that the correlation between trust and health outcomes was influenced by study quality, with lower correlations observed in higher quality studies. By addressing these elements in the awareness agreement process, healthcare providers can enhance trust and engagement, ultimately leading to better therapeutic outcomes.
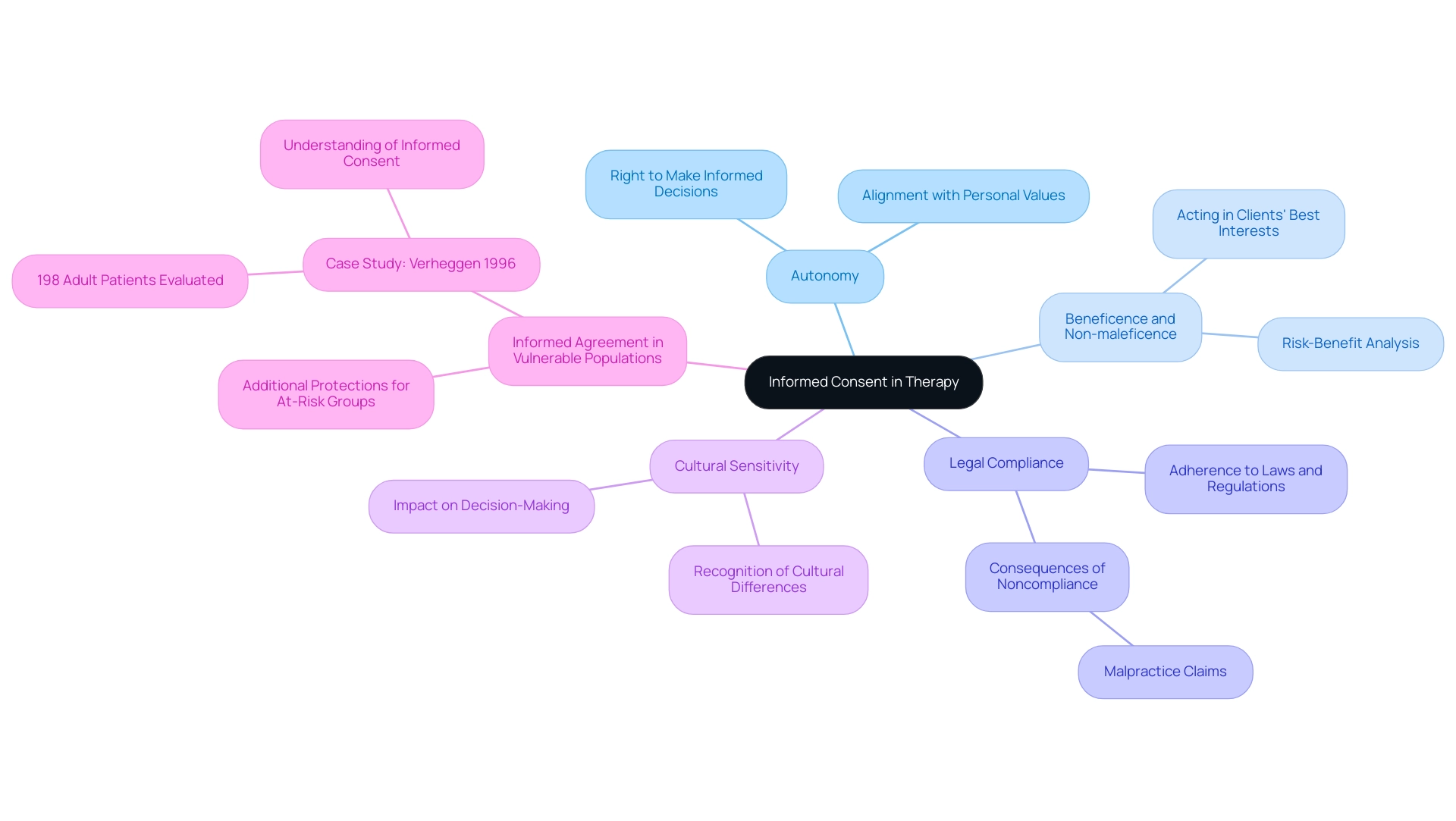
Ethical and Legal Considerations in Informed Consent
Informed agreement is essential for therapists, highlighting what should be included in informed consent for therapy as both a regulatory requirement and an ethical imperative. Key ethical and legal considerations include:
- Autonomy: Upholding individual autonomy is essential, as people have the right to make knowledgeable decisions about their treatment that align with their personal values and preferences.
- Beneficence and Non-maleficence: Therapists are obligated to act in their clients' best interests, ensuring that the therapeutic benefits significantly outweigh any potential risks.
- Legal Compliance: Adherence to relevant laws and regulations governing knowledgeable agreement is critical, as these mandates can differ across jurisdictions. Noncompliance may lead to severe legal consequences, including malpractice claims. Evidence suggests that 82.8% of retrospective studies indicated obtaining ethical approval, emphasizing the significance of these practices.
- Cultural Sensitivity: Recognizing and honoring cultural differences is crucial, as these elements can significantly affect an individual's understanding of agreement and their decision-making processes.
- Informed Agreement in Vulnerable Populations: When interacting with at-risk groups, such as children or individuals with cognitive impairments, therapists must establish additional protections to ensure that their rights are upheld. The case study by Verheggen in 1996, which assessed informed agreement through questionnaires given to 198 adult individuals four weeks after ICPs in 26 trials, illustrates the ongoing challenges in achieving effective understanding in diverse populations.
A concerning aspect of informed agreement is the low level of comprehension regarding its components, which undermines ethical practices in clinical trials. This emphasizes the essential need for additional research on patients' comprehension of agreements in standard therapeutic environments, as current studies mainly concentrate on clinical trials. Furthermore, Connor W. Boyle emphasizes the complexity often introduced in authorization forms, noting,
The revisions proposed by Emmanuel and Boyle to the relatively straightforward COVID-19 vaccine trials’ authorization documents yielded a document that was substantially longer than ideal.
This indicates an essential requirement for clarity and understanding in agreement procedures, especially considering recent conversations regarding ethical standards in therapeutic environments. Instances of legal adherence in knowledgeable approval procedures involve guaranteeing that all essential information, specifically what should be included in informed consent for therapy, is communicated clearly and securing explicit agreement prior to proceeding with treatment.
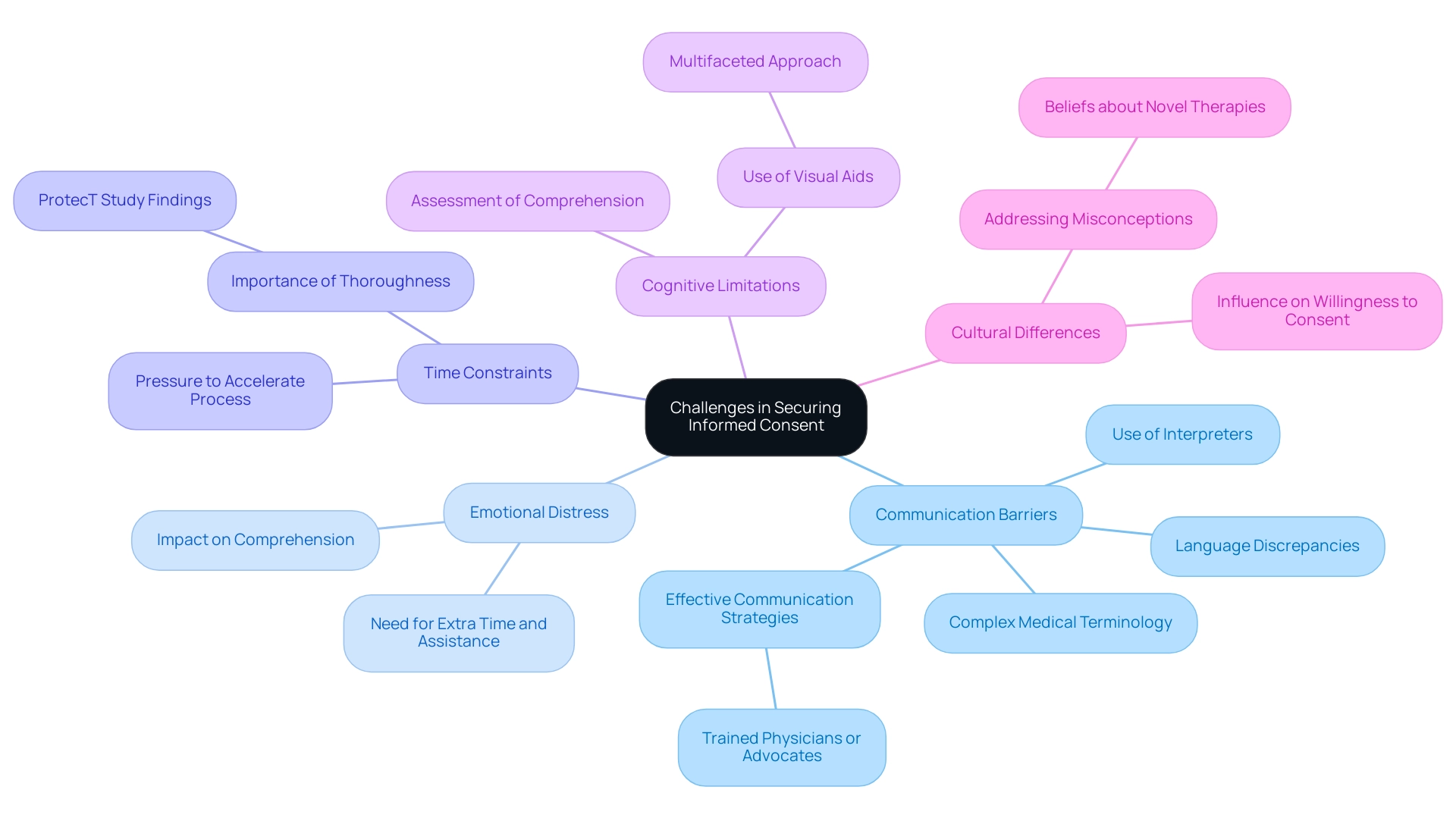
Challenges in Securing Informed Consent in Therapeutic Settings
Obtaining informed agreement in healthcare and research involves navigating several significant challenges:
- Communication Barriers: Many individuals grapple with complex medical terminology, and language discrepancies can further complicate understanding. To mitigate these issues, therapists should utilize straightforward language and ensure that what should be included in informed consent for therapy is clear when employing interpreters if necessary. Recent findings emphasize that effective communication by trained physicians or advocates can significantly improve individuals' understanding of clinical trials, thereby addressing common obstacles related to medical jargon.
- Emotional Distress: Individuals experiencing emotional distress may find it especially difficult to comprehend information. It is crucial for therapists to stay aware of an individual's emotional condition, providing extra time and assistance during the agreement stage to ensure clarity on what should be included in informed consent for therapy. Statistics indicate that emotional distress greatly affects individuals' capacity to understand crucial information, highlighting the necessity for a compassionate approach.
- Time Constraints: In hectic clinical settings, there is frequently pressure to accelerate the agreement procedure. However, prioritizing thoroughness over speed is crucial to ensure that individuals are aware of what should be included in informed consent for therapy. The Protect study demonstrates this effectively; 1643 out of 2664 men (62%) accepted randomization, indicating that a well-organized agreement procedure can produce favorable outcomes even under time constraints.
- Cognitive Limitations: Some individuals may encounter cognitive challenges that impede their comprehension of the agreement. Therapists should actively assess comprehension and adapt their communication methods accordingly to clarify what should be included in informed consent for therapy. Investigators have demonstrated that employing visual aids can significantly enhance understanding during the agreement process. Herman, White, and Barkin emphasized this approach, noting that a multifaceted strategy involving multiple visual tools alongside verbal explanations can greatly improve comprehension.
- Cultural Differences: Cultural beliefs regarding mental health and therapy can significantly influence an individual's willingness to provide consent. To cultivate an atmosphere of trust and understanding, it is essential for therapists to understand what should be included in informed consent for therapy, such as cultural competence and sensitivity, while acknowledging and valuing the diverse backgrounds of those they serve. Addressing misconceptions, particularly about novel therapies, is essential; for instance, many individuals mistakenly believe that newer treatment modalities, such as targeted therapies and immunotherapies, are inherently less toxic than traditional chemotherapy. Effective communication is essential in dispelling these myths during the informed agreement phase.
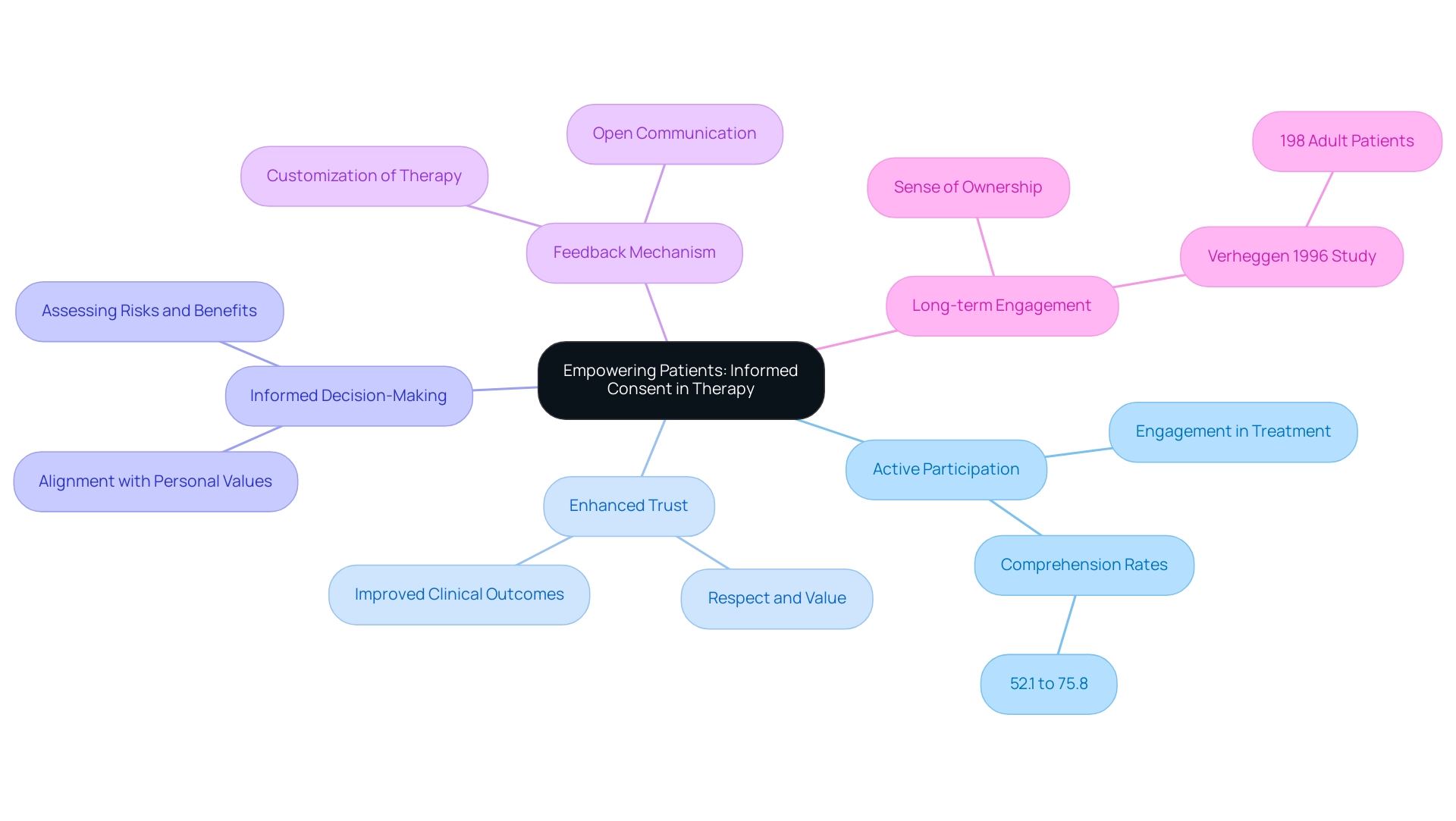
Empowering Patients: The Role of Informed Consent in Therapy
Understanding what should be included in informed consent for therapy is essential to empowering individuals throughout their therapeutic journey. By ensuring comprehensive understanding of what should be included in informed consent for therapy, therapists promote autonomy and agency in treatment decisions. Key elements of this empowerment include:
- Active Participation: Informed consent invites patients to engage actively in their treatment, fostering greater commitment and involvement in the therapeutic process. Research has indicated that the proportion of clinical trial participants who understood the elements of consent varied from 52.1% to 75.8%, emphasizing the inconsistency in participant engagement.
- Enhanced Trust: An informed individual is more likely to feel respected and valued, which significantly strengthens trust in the therapeutic relationship. This trust is essential, as it can lead to improved clinical outcomes and satisfaction among individuals.
- Informed Decision-Making: By providing detailed and understandable information, therapists empower individuals to assess potential risks and benefits, facilitating choices that resonate with their personal values and preferences. This decision-making procedure is essential for individual autonomy.
- Feedback Mechanism: The awareness agreement process serves as a platform for therapists to request input, encouraging open communication and enabling essential modifications to the treatment plan. This dynamic is essential for customizing therapy to individual requirements.
- Long-term Engagement: Patients who feel empowered are more likely to maintain their engagement in therapy over time, fostering a sense of ownership in their treatment journey. The significance of this involvement is highlighted by discoveries from Verheggen's 1996 research, which assessed comprehension of agreement among 198 adult individuals across 26 trials, revealing the essential nature of agreement in individual empowerment.
Moreover, as pointed out by Purav Dave, "Informed consent for therapy, which outlines what should be included in informed consent for therapy, is not merely a formality; it’s an essential element that influences the therapeutic relationship and boosts client involvement." This highlights the importance of knowledgeable agreement in promoting trust and cooperation.
Furthermore, insights from Briones-Vozmediano et al. concerning the management of fibromyalgia emphasize the importance of knowledgeable agreement in addressing individual concerns and preferences, especially in intricate therapeutic situations. However, it is essential to recognize the constraints of knowledge agreement procedures, such as the possible exclusion of pertinent documents and cultural influences, which can influence individual comprehension and involvement.
Ultimately, informed consent not only enhances patient autonomy but also builds a collaborative therapeutic environment that can significantly improve treatment outcomes.
Conclusion
Informed consent is a fundamental aspect of ethical therapy practice, ensuring that patients are fully informed and empowered to make decisions about their treatment. The key components—disclosure, comprehension, voluntariness, competence, and documentation—foster trust and engagement between therapists and patients. Effective communication and cultural sensitivity are crucial for enhancing understanding and promoting a collaborative therapeutic relationship.
Providing supplementary information, such as:
- Therapist qualifications
- Specific risks
- Alternative therapies
- Confidentiality
- Follow-up procedures
enriches the informed consent process. This transparency empowers patients to actively participate in their care, ultimately improving satisfaction and treatment outcomes. Ethical and legal considerations, including the protection of vulnerable populations and respect for patient autonomy, further emphasize the importance of informed consent.
Despite challenges such as communication barriers and emotional distress, therapists must strive to create an environment that promotes understanding and trust. By prioritizing these elements, informed consent can serve as a powerful tool for patient empowerment, allowing individuals to make informed choices aligned with their values.
In summary, informed consent is not merely a procedural requirement; it is essential for enhancing patient autonomy and fostering collaboration in therapy. As the field of mental health care evolves, therapists must remain committed to refining their informed consent practices, ensuring that every patient feels respected and understood throughout their therapeutic journey.




