Overview
Best practices for trial reporting in the realm of medical devices underscore the paramount importance of accuracy and compliance, which are essential for ensuring the safety and effectiveness of these products. This article asserts that precise documentation serves not only as a regulatory necessity but also as a cornerstone for maintaining trust with stakeholders. It highlights how meticulous reporting can avert costly delays and bolster the credibility of clinical research outcomes. In a landscape where the stakes are high, understanding these practices is crucial for all involved in clinical research.
Introduction
In the intricate world of medical device research, the significance of accurate trial reporting cannot be overstated. Organizations are compelled to navigate the complexities of regulatory frameworks while maintaining the integrity of clinical data, which amplifies the pressure to ensure transparency and reliability. Recent shifts in regulatory requirements underscore the critical need for precise documentation, not only to safeguard patient safety but also to facilitate timely device approvals. With the stakes higher than ever, establishing robust reporting protocols emerges as a fundamental pillar of ethical research practices. This article delves into the essential elements of accurate trial reporting, the challenges faced by researchers, and the innovative solutions provided by organizations like bioaccess® to enhance the clinical trial landscape in Latin America.
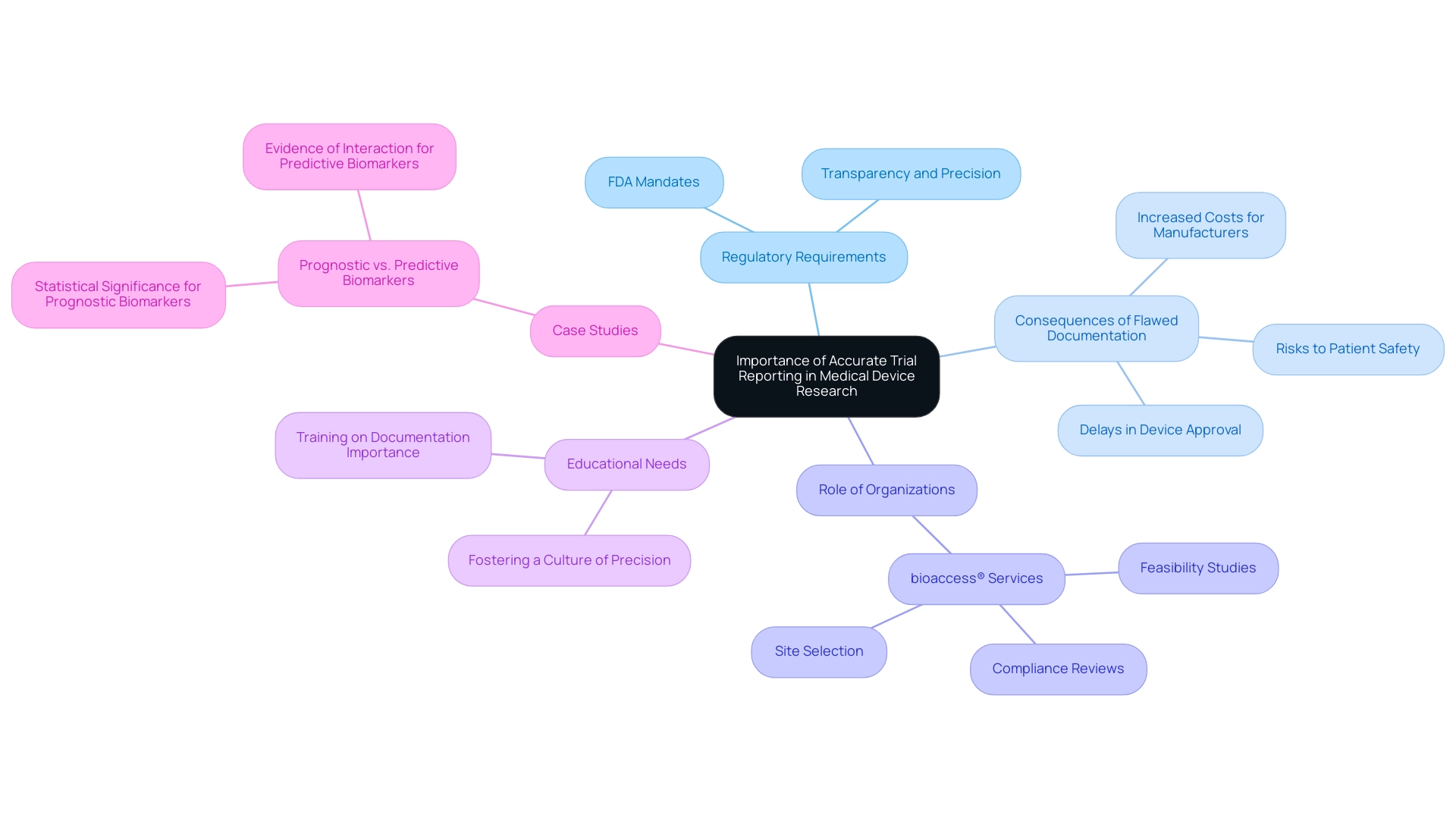
The Importance of Accurate Trial Reporting in Medical Device Research
Precise trial reporting for medical devices is crucial in medical device research, ensuring that the information gathered during evaluations is both trustworthy and usable for assessing device safety and effectiveness. Regulatory authorities, including the FDA, mandate thorough and precise documentation to effectively evaluate the associated risks and benefits of medical devices. Recent FDA requirements have underscored the necessity for transparency and precision in clinical research information, reflecting a growing emphasis on accountability within the industry.
Flawed documentation can have severe repercussions, including delays in device approval, increased costs for manufacturers, and potential risks to patient safety. Research has demonstrated that inconsistencies in experimental data can lead to a substantial decrease in approval rates, emphasizing the essential importance of precise documentation. Thus, creating robust documentation protocols is not merely a regulatory requirement but a crucial element of ethical medical research.
Furthermore, the methods section of any medical study must provide sufficient detail for informed readers to confirm reported results, ensuring transparency and promoting trust in the findings. Educating personnel on the significance of precision in testing documentation is equally crucial. By fostering a culture of precision and accountability, organizations can enhance the integrity of their research studies.
This commitment to accuracy not only supports compliance with regulatory standards but also builds trust with stakeholders and the public.
Organizations like bioaccess® play a pivotal role in this landscape, providing extensive research management services that encompass feasibility studies, site selection, compliance reviews, setup, import permits, project management, and reporting. With over 20 years of experience in Medtech, bioaccess® possesses the knowledge and tailored strategy required to navigate the intricacies of research studies. Their expertise in managing Early-Feasibility Studies (EFS), First-In-Human Studies (FIH), Pilot Studies, Pivotal Studies, and Post-Market Follow-Up Studies (PMCF) ensures that trials are conducted with the utmost precision and adherence to regulatory requirements.
Case studies, such as the distinction between prognostic and predictive biomarkers, illustrate the significance of meticulous documentation in clinical research. These studies emphasize that while demonstrating a statistically significant association suffices for declaring a biomarker as prognostic, predictive biomarkers necessitate evidence of interaction with treatment. This distinction underscores the need for careful study design and accurate reporting to evaluate these biomarkers effectively.
As Piantadosi noted, "To establish a hypothesis requires both a theoretical basis in biology and statistical support for the hypothesis, based on the observed information and the theoretical statistical model." This highlights the necessity of a solid foundation in both theory and data accuracy in medical research.
In summary, the impact of accurate trial reporting for medical devices on approval cannot be overstated. It is a cornerstone of successful medical research that ultimately influences the advancement of innovative medical technologies. Furthermore, bioaccess® plays a crucial role in bridging the gap between innovative medtech companies and the potential for conducting clinical research studies in Latin America, offering a unique value proposition that enhances the overall landscape of medical device development.
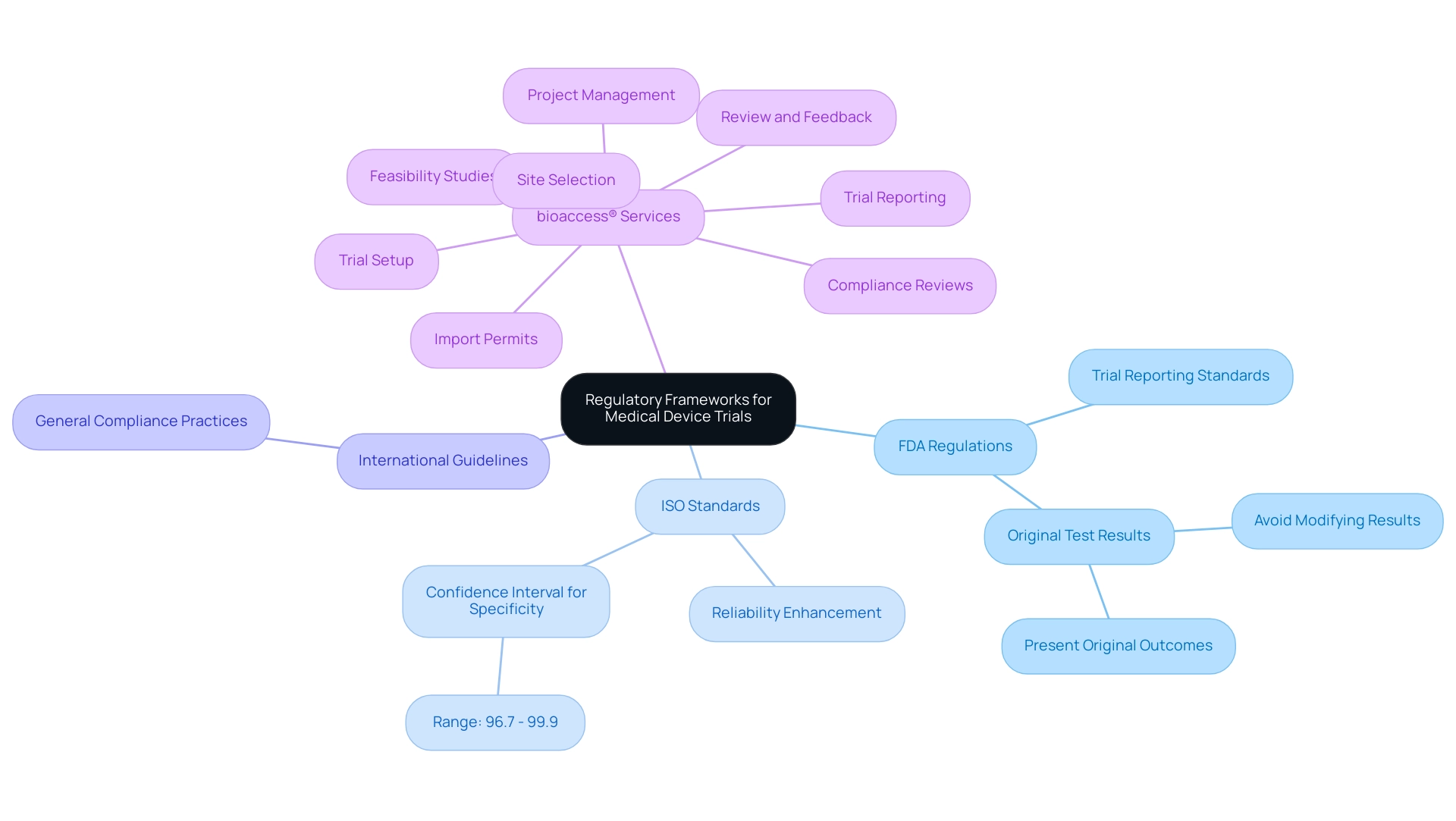
Navigating Regulatory Frameworks for Medical Device Trials
Navigating the regulatory landscape for medical device studies, particularly regarding trial reporting, necessitates a comprehensive understanding of various frameworks, including FDA regulations, ISO standards, and international guidelines. Each regulatory authority enforces specific criteria for study documentation, underscoring the importance of transparency, data integrity, and ethical considerations. For instance, the FDA strongly advises against modifying original test results based on discrepant resolution, as illustrated in the case study 'Discrepant Resolution and Its Associated Problems.'
This study critiques the effectiveness of using resolver results to alter original test outcomes, noting that such practices can misrepresent test performance and lead to incorrect calculations, ultimately introducing bias in sensitivity and specificity estimates. Instead, the FDA recommends presenting original outcomes alongside appropriate agreement measures to maintain precision.
Compliance with ISO standards is equally vital, with statistics indicating that adherence can significantly enhance the reliability of medical studies. For example, a two-sided 95% confidence interval for specificity in medical device studies ranges between 96.7% and 99.9%. This statistic emphasizes the necessity of rigorous trial reporting and testing standards, reflecting the reliability of results obtained during medical trials.
To effectively advance medical device trials, bioaccess® provides a comprehensive suite of services, including trial reporting for medical devices, feasibility studies, site selection, compliance reviews, trial setup, import permits, project management, and review and feedback on study documents. These services ensure that research teams remain vigilant and well-informed about regulatory requirements, particularly in Colombia, where obtaining IRB/EC approval, INVIMA approval, and MinCIT import permits is crucial.
Regular training sessions and updates on regulatory changes are essential for preparing teams for audits and inspections, fostering a culture of compliance and excellence in research. By connecting innovative Medtech firms with opportunities to conduct research studies in Latin America, bioaccess® emphasizes the significance of these regulatory practices within its mission and the broader industry context.
BOOK A MEETING
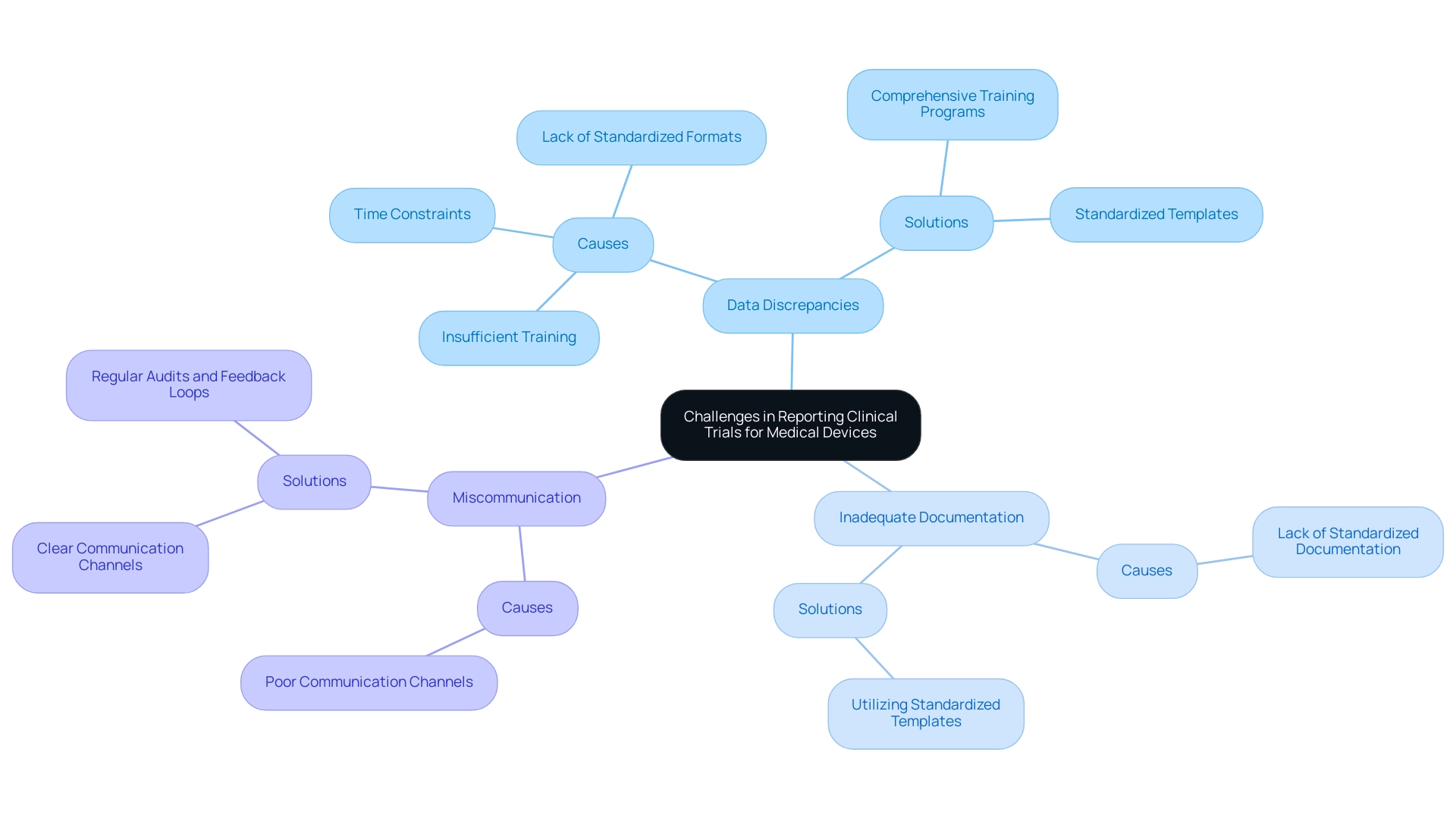
Common Challenges in Reporting Clinical Trials for Medical Devices
Trial reporting for medical devices poses several common challenges, notably data discrepancies, inadequate documentation, and miscommunication among stakeholders. These issues frequently stem from factors such as insufficient training, the lack of standardized documentation formats, and pressing time constraints. A significant number of research studies fail to comply with the CONSORT Statement, which outlines a 22-item checklist and flow diagram essential for accurately reporting randomized studies.
To tackle these challenges, organizations like bioaccess® strive to expedite the advancement of medical devices through their expertise and tailored approach. bioaccess® has established a partnership with Caribbean Health Group to position Barranquilla as a premier location for health studies in Latin America, a decision supported by Colombia's Minister of Health. This collaboration aims to enhance the clinical research environment in the region, making it more attractive for research initiatives.
Prioritizing the implementation of comprehensive training programs equips staff with essential skills and knowledge. Establishing clear communication channels among all stakeholders is crucial to ensure alignment and information sharing throughout the process. Furthermore, utilizing standardized templates for documentation can streamline operations and minimize the potential for errors.
Regular audits and feedback loops are vital for identifying and addressing issues before they escalate. A case study highlighting cultural influences on medical studies underscores the necessity of considering local contexts, as cultural conditions can significantly impact participant engagement and information gathering. By learning from such cases, organizations can devise strategies to mitigate data discrepancies and improve the overall quality of research reporting.
Additionally, GlobalCare Clinical Studies has partnered with bioaccess™ to enhance ambulatory services in Colombia, achieving over a 50% reduction in recruitment time and impressive 95% retention rates. Expert opinions emphasize that while advanced statistical techniques can provide insights, they cannot compensate for fundamental flaws in research design and execution. As Scott R. Evans, Ph.D., states, 'Sophisticated statistical techniques cannot save shortcomings in medical studies.'
Thus, a proactive strategy for training, communication, and standardization is essential for ensuring adherence and precision in trial reporting for medical devices.
For users visiting the bioaccess website, managing cookie preferences is straightforward. You can modify your cookie preferences at any time by clicking the cookie settings button, allowing you to revisit the cookie consent banner and adjust your preferences or withdraw your consent immediately. For further assistance, please refer to the support documents for managing cookies in your specific web browser.
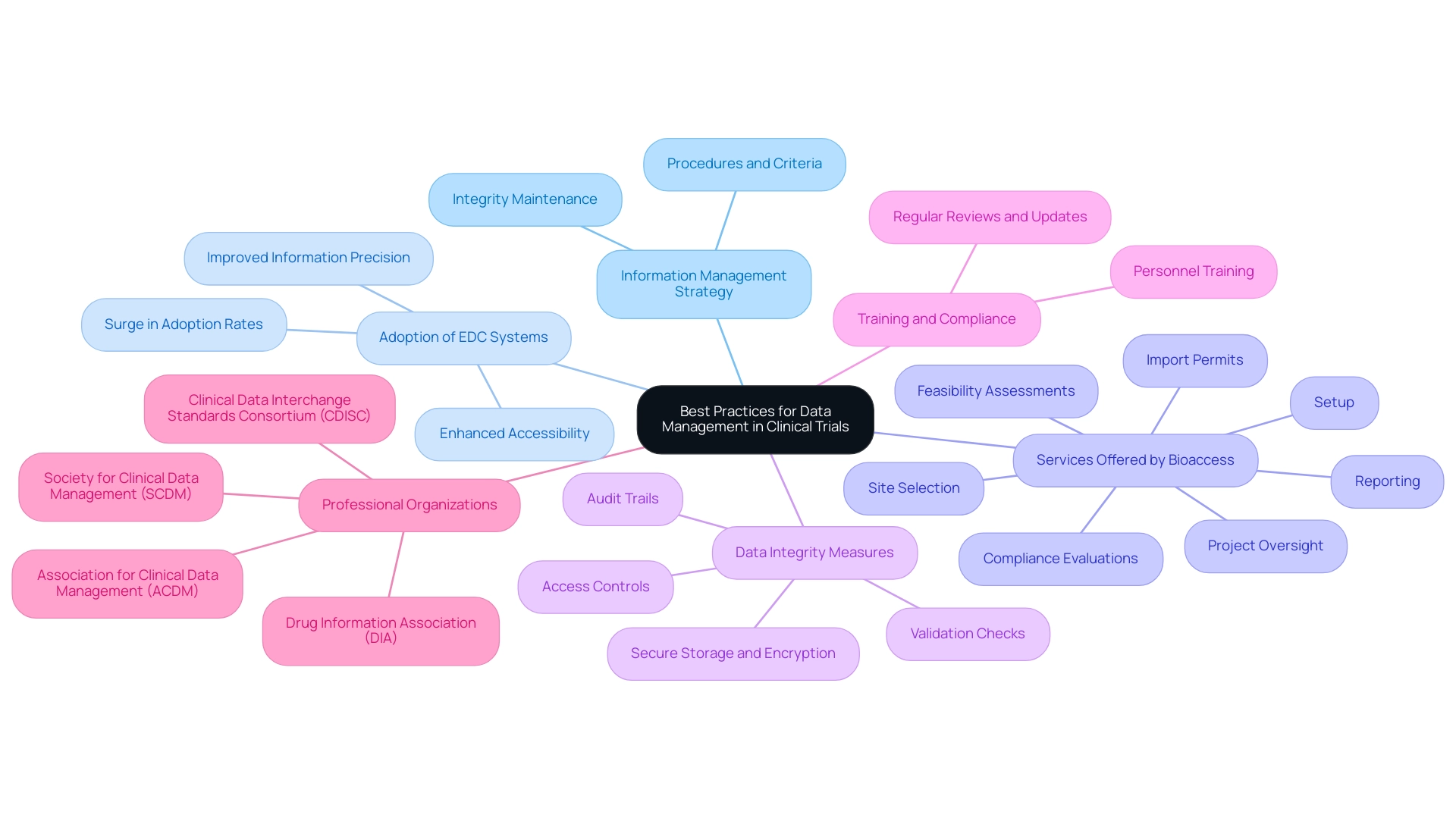
Best Practices for Data Management and Reporting in Clinical Trials
Efficient information management and documentation in clinical studies are essential for trial reporting of medical devices, relying on various best practices that guarantee compliance and precision. A comprehensive information management strategy is crucial, detailing the procedures and criteria necessary for upholding integrity throughout the study. The adoption of electronic data capture (EDC) systems is particularly vital; these systems facilitate information collection and enhance the effectiveness of study documentation.
Statistics indicate a significant surge in the adoption of EDC systems, with a notable percentage of research studies now utilizing these technologies to improve information precision and accessibility. Bioaccess notably provides extensive clinical study management services, including:
- Feasibility assessments
- Site selection
- Compliance evaluations
- Setup
- Import permits
- Project oversight
- Reporting
These services are crucial for ensuring the success of clinical studies.
To further enhance information integrity, organizations must implement stringent access controls and maintain detailed audit trails. This approach not only safeguards patient information confidentiality through secure storage and encryption but also aligns with privacy regulations, ensuring that sensitive details are protected. Regular validation checks are essential for detecting discrepancies early, thereby improving the reliability of experimental results.
As highlighted in the case study on medical coding, proper medical coding is vital for categorizing medical terms linked to healthcare studies, ensuring consistency and preventing redundancy of information related to adverse events and medications. This practice is essential for identifying safety concerns and ensuring that clinical research information meets regulatory standards.
Training personnel on information management protocols is another critical element. By fostering a culture of precision and adherence, organizations can significantly elevate the quality of research information. Moreover, it is imperative to regularly review and update information management practices to adapt to evolving regulatory requirements and industry standards.
Professional organizations such as the Society for Clinical Data Management (SCDM) and the Clinical Data Interchange Standards Consortium (CDISC) offer valuable resources and guidelines that can support this continuous improvement process. As Dr. Andy Liu observes, selecting dependable endpoints from real-world digital health technology (DHT) data is essential for ensuring the validity of study outcomes.
Integrating these best practices not only enhances the overall quality of research data but also improves trial reporting for medical devices, enabling organizations to meet the stringent requirements of regulatory bodies and ultimately facilitating the successful progression of medical devices in the market.
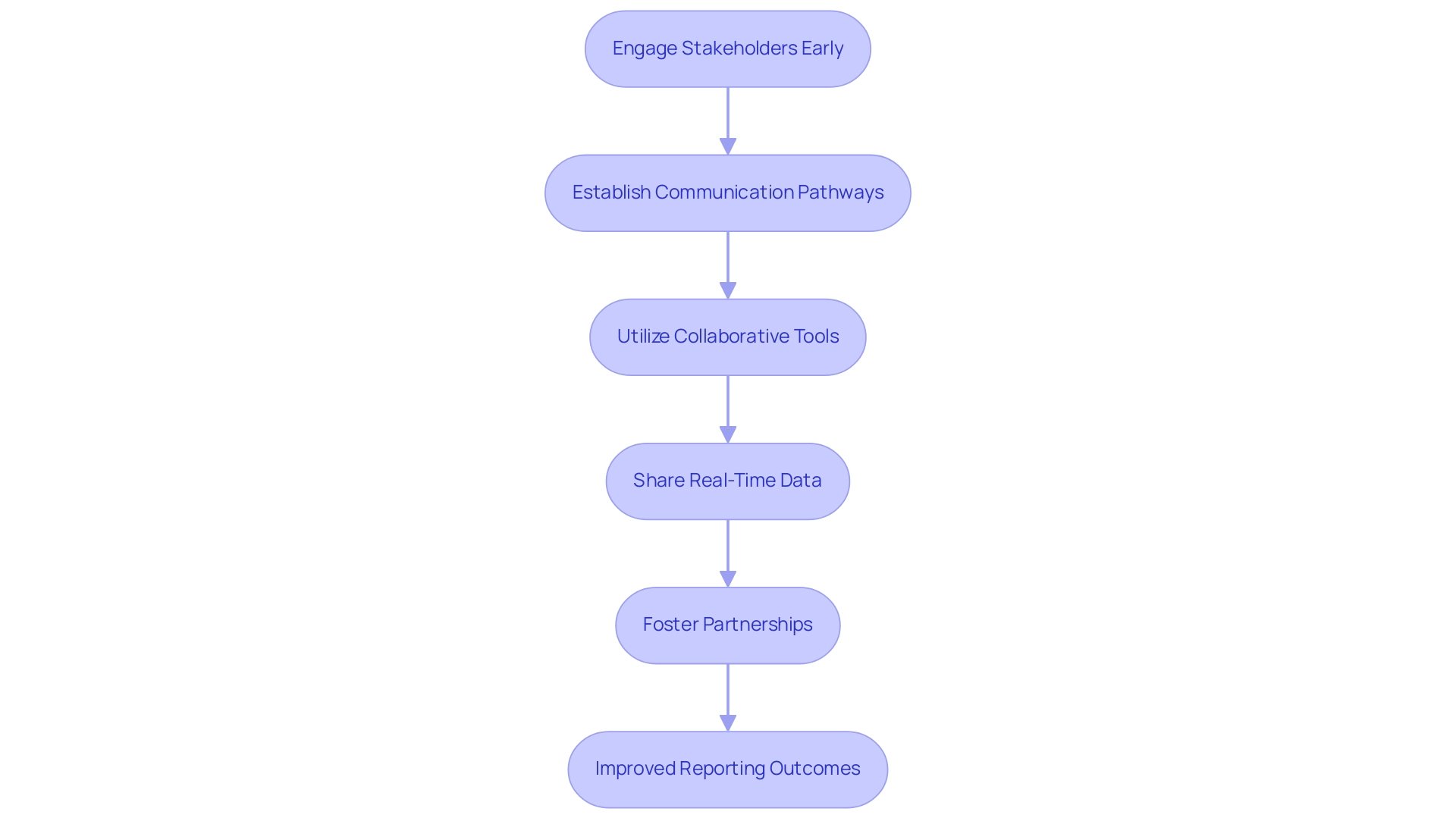
Enhancing Collaboration Among Stakeholders for Better Reporting Outcomes
Enhancing cooperation among stakeholders—including sponsors, researchers, and regulatory entities—is essential for improving outcomes in clinical studies and ensuring effective trial reporting for medical devices. Establishing consistent communication pathways, such as planned meetings and progress updates, guarantees that all parties remain aligned on objectives and documentation requirements. The utilization of collaborative tools and platforms facilitates real-time data sharing and feedback, leading to more accurate and timely reporting.
Engaging stakeholders early in the design process fosters a sense of ownership and accountability, further enhancing collaboration. For instance, the partnership between bioaccess™ and Caribbean Health Group (CHG) aims to position Barranquilla as a leading hub for medical research in Latin America, supported by Colombia's Minister of Health, Juan Pablo Uribe. This initiative underscores a commitment to improving the research landscape in the region.
Dushyanth Surakanti, Founder and CEO of Sparta Biomedical, shared his favorable experience with bioaccess® during its initial human study in Colombia, highlighting the effectiveness of such collaborations in advancing medical research. Additionally, partnerships with organizations like IDx Technologies and Global Care Clinical Trials have further solidified bioaccess™'s role in enhancing ambulatory services in Colombia, achieving over a 50% reduction in recruitment time and 95% retention rates. The specific outcomes from these collaborations illustrate the tangible benefits of cooperation in medical research.
As Romée Melanie Helena Court observed, "About 15 years ago, pharmaceutical companies were loose [isolated] strongholds. But now you see more and more that the companies are working together [open innovation]." This transition towards collaboration is crucial, especially given the substantial costs associated with sharing research data, particularly for smaller companies that may struggle to absorb these expenses.
Data indicates that effective cooperation can significantly lower expenses, with virtual studies potentially reducing costs per participant by as much as 50% compared to traditional studies. This underscores the importance of communication in medical study documentation, particularly for trial reporting for medical devices, as streamlined processes can lead to more efficient resource utilization and improved outcomes. As the landscape of medical research evolves, fostering open dialogue and collaboration among all participants will be vital for enhancing trial reporting for medical devices and ensuring adherence and accuracy in documentation, particularly in bridging the gap between innovative Medtech firms and the potential for conducting research studies in Latin America.
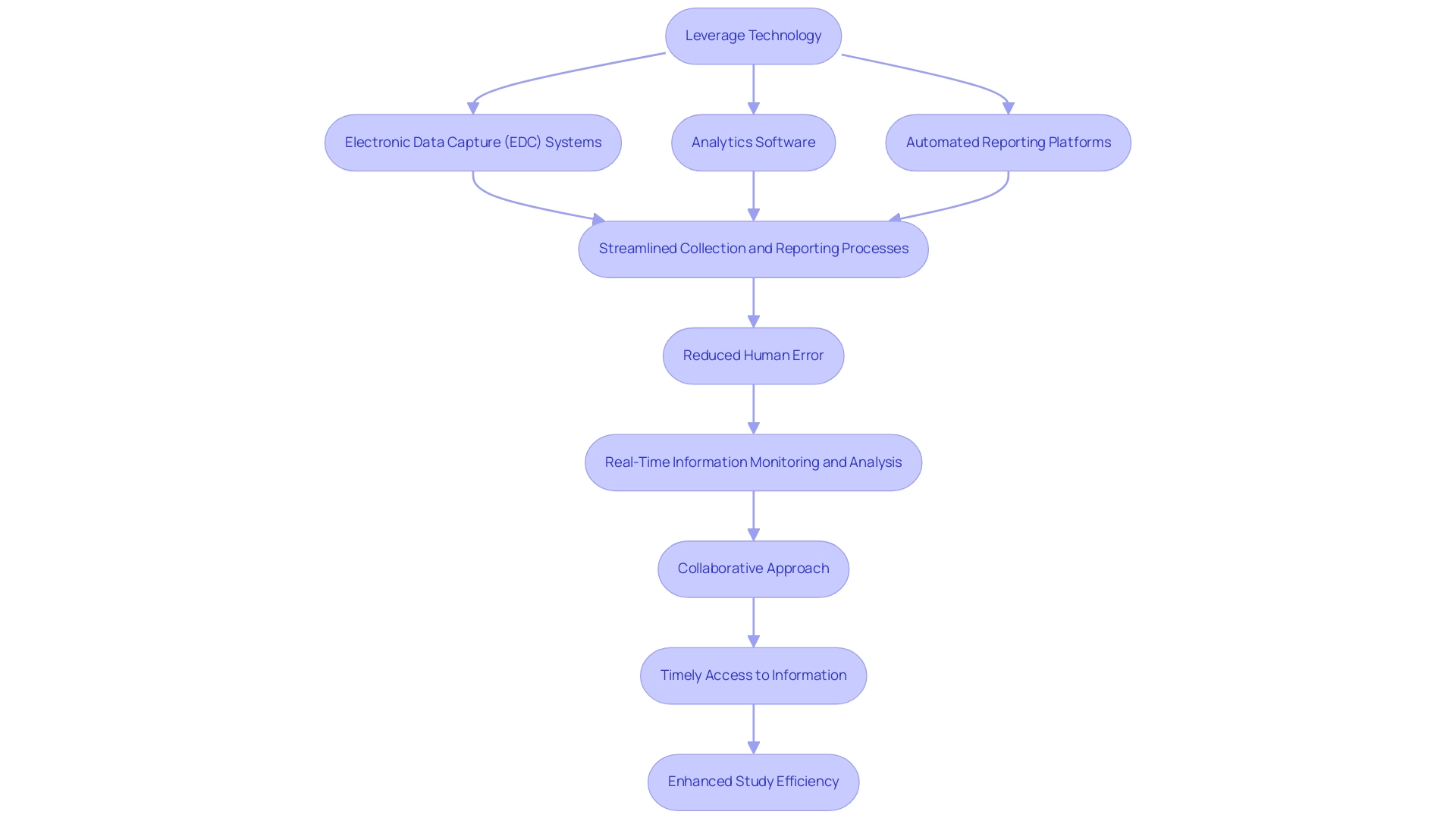
Leveraging Technology for Improved Trial Reporting Efficiency
Leveraging technology in clinical trial documentation is crucial for enhancing both efficiency and accuracy, particularly in the context of trial reporting for medical devices managed by bioaccess®. Electronic information capture (EDC) systems, analytics software, and automated reporting platforms play a pivotal role in streamlining collection and reporting processes. By utilizing these advanced technologies, organizations can significantly lessen the risk of human error, enabling real-time information monitoring and analysis that is essential for informed decision-making.
The adoption of cloud-based solutions further facilitates collaboration among stakeholders, ensuring that all parties have access to the most current information and reports. This collaborative approach is vital, especially in large-scale studies like those conducted by bioaccess®, where timely access to information can influence outcomes. For instance, the All of Us research, which included 1 million contributors, employed mobile technology for thorough information gathering, showcasing the efficacy of creative solutions in handling large datasets and emphasizing the significance of participant involvement.
However, despite these advancements, challenges persist in ensuring information quality and sustaining participant involvement throughout the study process. Training staff on these technologies is essential to maximize their potential benefits. As the landscape of medical research evolves, equipping teams with the necessary skills to navigate these tools will enhance overall study efficiency.
Furthermore, the most recent data indicates that the application of EDC systems has resulted in improved data collection times, demonstrating a learning process among users that ultimately aids in more efficient management of studies.
As Wilhelm and associates propose, utilizing technology can also extend to offering cognitive-behavioral therapy for mental health issues, underscoring the broader applications of technology in healthcare environments. In summary, the incorporation of technology in healthcare research documentation not only streamlines processes but also fosters a culture of precision and adherence, which is critical in the medical device industry, particularly for the comprehensive research management services provided by bioaccess®, including Early-Feasibility Studies, First-In-Human Studies, Pilot Studies, Pivotal Studies, Post-Market Clinical Follow-Up Studies, and trial reporting for medical devices. With over 20 years of experience in Medtech, bioaccess® is well-equipped to tackle the challenges of research in Latin America.
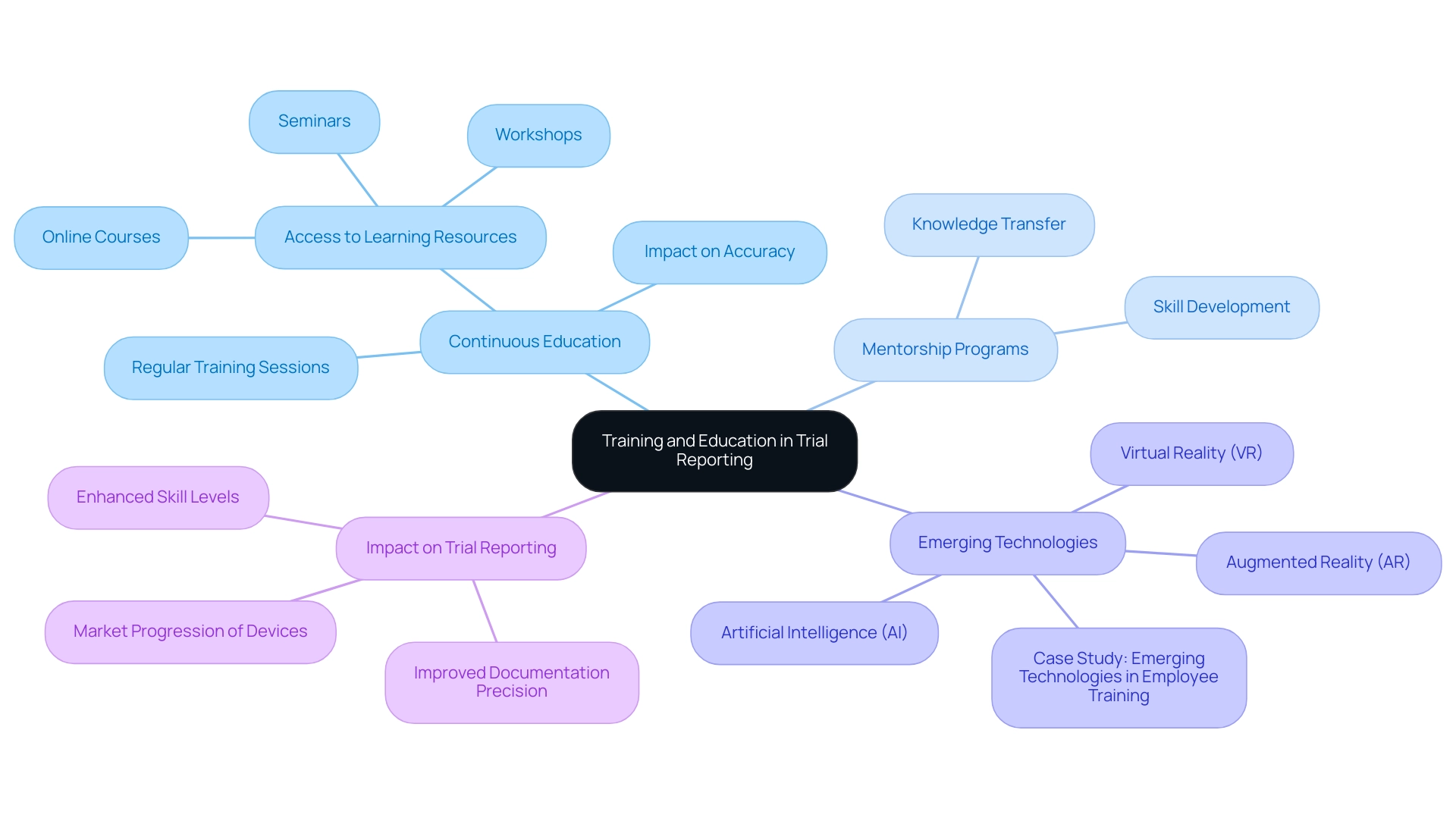
Training and Education: Key to Effective Trial Reporting
Training and education are essential for ensuring precision and adherence in medical device evaluations. Since 1978, the focus within health professions has been heavily on competencies, highlighting the necessity for organizations to prioritize regular training sessions. Keeping research teams informed about evolving regulatory standards, documentation requirements, and industry best practices is vital.
Research demonstrates that continuous education significantly influences the accuracy of trial reporting for medical devices. Studies indicate that well-trained teams are more adept at navigating the complex reporting landscapes associated with these devices.
To enhance knowledge and skills, providing access to a diverse array of learning resources—such as online courses, workshops, and seminars—is crucial. This strategy not only equips team members with the latest information but also fosters a culture of continuous learning, motivating staff to actively pursue new insights and remain current with industry trends. As Jessica R. Cranfill from Duke University noted, "This program really gave me the confidence to speak up and say ‘this is what has been successful for me,’ or you know ‘thanks for sharing that problem with the group, here’s a resource that might be helpful.’"
Mentorship programs are pivotal in nurturing the next generation of clinical research professionals. By pairing experienced researchers with newcomers, organizations can facilitate knowledge transfer and practical skill development, ensuring that best practices are upheld across the board.
Emerging technologies, including virtual reality (VR), augmented reality (AR), and artificial intelligence (AI), are being explored to enhance training programs. A case study titled "Emerging Technologies in Employee Training" illustrates how these technologies enable immersive learning experiences, improving the personalization and effectiveness of skill development in training. These innovations represent the latest trends in research education, aligning with the industry's shift towards more dynamic and engaging training methodologies.
In summary, investing in thorough training and education not only improves study documentation precision but also enhances trial reporting for medical devices. This investment ultimately boosts the overall skill level of research teams and aids the successful progression of these devices in the market. Moreover, efficient management services offered by bioaccess—including feasibility studies, site selection, compliance reviews, setup, import permits, project management, and reporting—are essential for the successful execution of these studies. These services can positively impact local economies through job creation and healthcare improvements while ensuring compliance with regulatory frameworks established by INVIMA.
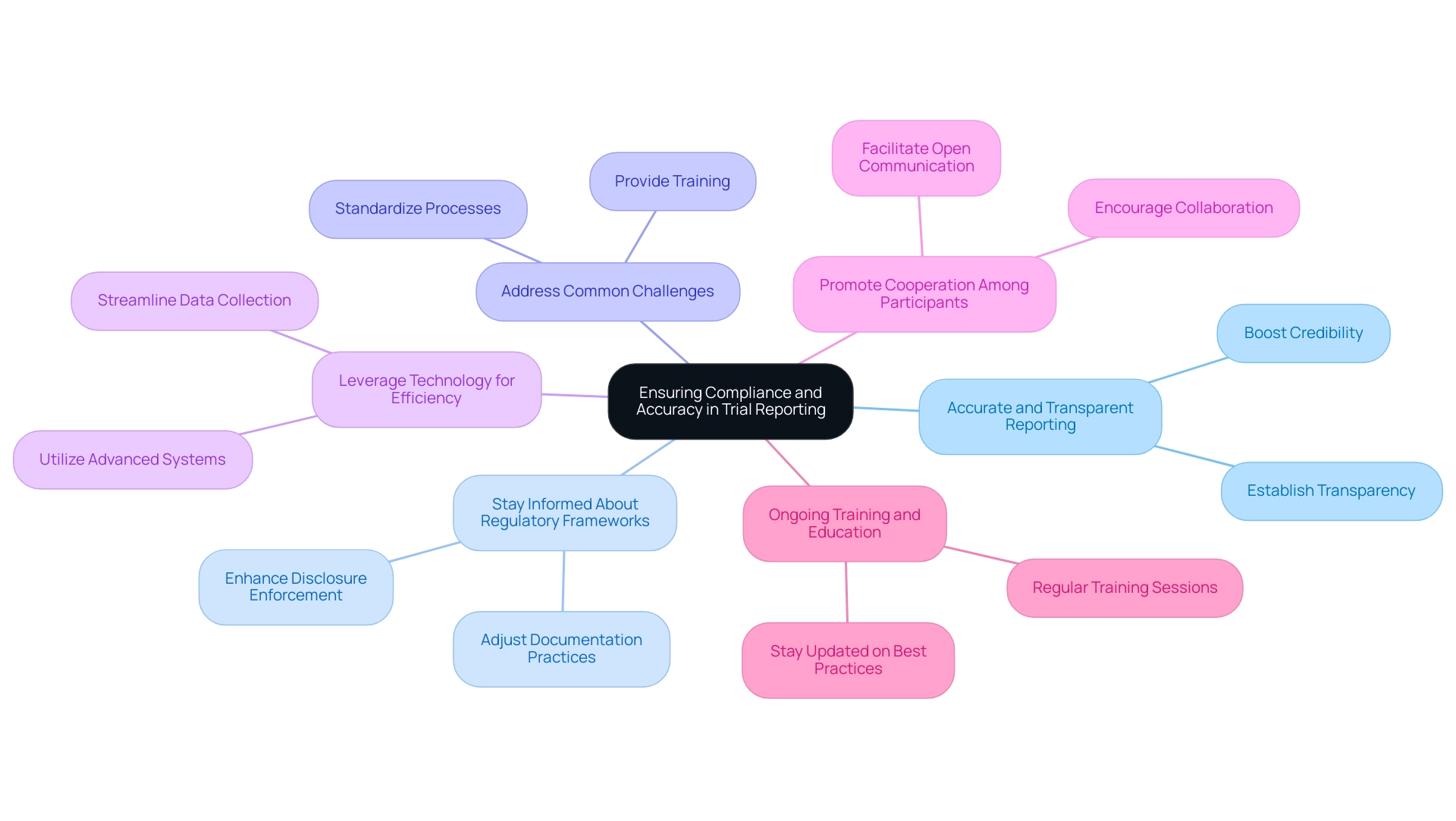
Key Takeaways for Ensuring Compliance and Accuracy in Trial Reporting
To ensure compliance and accuracy in trial reporting, clinical research teams must concentrate on several essential strategies:
- Prioritize Accurate and Transparent Reporting: Establishing a culture of transparency is crucial for building trust with regulatory bodies and stakeholders. Precise documentation not only meets ethical obligations but also boosts the credibility of the research. The industry has demonstrated improved adherence to disclosures; however, there remains a significant need for ethical transparency across all sectors. bioaccess® is committed to addressing client concerns through its grievance procedures, ensuring that any issues related to data processing are handled with compliance and transparency. For any queries or concerns, clients may contact our Grievance Officer at IMH ASSETS CORP (doing business as "bioaccess®"), 1200 Brickell Avenue, Suite 1950 #1034, email: info@bioaccessla.com.
- Stay Informed About Regulatory Frameworks: Keeping abreast of evolving regulatory requirements is vital. Organizations must adjust their documentation practices to align with the latest guidelines from authorities such as the FDA and the National Library of Medicine, which emphasize the importance of compliance. Enhanced enforcement of disclosure requirements is essential to ensure that sponsors are well-informed about their obligations. bioaccess® provides comprehensive clinical trial management services, including compliance reviews, feasibility studies, site selection, and project management, to support organizations in navigating these frameworks.
- Proactively Address Common Challenges: Training and standardized processes can alleviate common documentation challenges. By providing teams with the necessary skills and knowledge, organizations can improve their accuracy and compliance. Inferential statistics play a crucial role in determining the likelihood that results are statistically significant, underscoring the importance of precise documentation.
- Leverage Technology for Efficiency: Utilizing advanced information management systems can significantly enhance efficiency in documentation. Technology can streamline data collection, analysis, and documentation processes, reducing the likelihood of errors and enhancing overall accuracy.
- Promote Cooperation Among Participants: Encouraging collaboration among all participants involved in the medical study process can lead to enhanced documentation outcomes. Open communication and shared goals can help identify potential issues early and facilitate timely resolutions.
- Invest in Ongoing Training and Education: Continuous education empowers research teams to stay updated on best practices and regulatory changes. Regular training sessions can strengthen the significance of adherence and precision in study documentation. The repercussions of non-reporting can be severe, including potential penalties and a loss of public trust in research, as discussed in the case study titled 'Consequences of Non-Reporting.'
By applying these strategies, organizations can greatly improve the quality and reliability of their trial reporting for medical devices, ultimately building greater trust with regulatory authorities and enhancing the overall integrity of medical research. bioaccess®'s commitment to data protection and comprehensive clinical trial management services further supports these efforts.
Conclusion
Accurate trial reporting stands as a cornerstone of medical device research, serving both as a safeguard for patient safety and a facilitator for timely regulatory approvals. This article underscores the critical need for transparent and reliable data, emphasizing that adherence to rigorous reporting standards is not merely a regulatory requirement but an ethical imperative. The repercussions of inaccurate reporting can be profound, leading to delays in device approvals and undermining public trust in clinical research.
Organizations like bioaccess® play a pivotal role in enhancing the clinical trial landscape, particularly in Latin America, by offering comprehensive management services that ensure compliance with evolving regulatory frameworks. The focus on training, collaboration, and technological innovation further highlights the necessity of establishing robust reporting protocols. By fostering a culture of accountability and precision, stakeholders can navigate the complexities of clinical trials with greater efficacy.
In conclusion, the commitment to accurate and transparent trial reporting is essential for the advancement of innovative medical technologies. As the industry continues to evolve, prioritizing these practices will not only bolster the credibility of clinical research but also fortify the overall integrity of the medical device sector. Moving forward, it is imperative that all stakeholders collaborate to uphold these standards, ultimately benefiting patients and the healthcare community at large.
Frequently Asked Questions
Why is precise trial reporting important in medical device research?
Precise trial reporting is crucial because it ensures that the information gathered during evaluations is trustworthy and usable for assessing the safety and effectiveness of medical devices. It supports regulatory evaluations and enhances accountability within the industry.
What are the consequences of flawed documentation in medical device trials?
Flawed documentation can lead to severe repercussions, including delays in device approval, increased costs for manufacturers, and potential risks to patient safety. It can also result in a decrease in approval rates due to inconsistencies in experimental data.
What role does the methods section play in a medical study?
The methods section must provide sufficient detail for informed readers to confirm reported results, ensuring transparency and promoting trust in the findings.
How can organizations enhance the integrity of their research studies?
Organizations can enhance the integrity of their research studies by fostering a culture of precision and accountability and educating personnel on the significance of accurate testing documentation.
What services does bioaccess® provide in the context of medical device research?
Bioaccess® offers extensive research management services, including feasibility studies, site selection, compliance reviews, trial setup, import permits, project management, and reporting, ensuring trials adhere to regulatory requirements.
What is the significance of the distinction between prognostic and predictive biomarkers in clinical research?
The distinction is significant because while a statistically significant association is sufficient for declaring a biomarker as prognostic, predictive biomarkers require evidence of interaction with treatment. This highlights the need for careful study design and accurate reporting.
What does the FDA recommend regarding original test results and discrepancies?
The FDA advises against modifying original test results based on discrepancies and recommends presenting original outcomes alongside appropriate agreement measures to maintain precision and avoid bias.
Why is compliance with ISO standards important in medical studies?
Compliance with ISO standards enhances the reliability of medical studies. For instance, adherence can ensure that confidence intervals for specificity in medical device studies are statistically significant, reflecting the reliability of results.
How does bioaccess® support regulatory compliance for medical device trials in Latin America?
Bioaccess® provides services that ensure research teams are informed about regulatory requirements, including obtaining IRB/EC approval, INVIMA approval, and MinCIT import permits, which are crucial for conducting studies in Colombia.
What is the importance of regular training for research teams in medical device studies?
Regular training sessions and updates on regulatory changes prepare teams for audits and inspections, fostering a culture of compliance and excellence in research.




