Overview
Choosing the largest Clinical Research Organization (CRO) in the world for your trials involves evaluating key criteria such as experience, regulatory knowledge, resources, and flexibility. The article emphasizes that selecting a CRO with a robust track record and comprehensive capabilities can significantly enhance the efficiency and success of clinical studies, especially in navigating complex regulatory environments and optimizing patient recruitment.
Introduction
In the ever-evolving landscape of clinical research, Clinical Research Organizations (CROs) have emerged as vital partners, streamlining the complexities of clinical trials for sponsors. By offering a wide range of services—from project management and regulatory compliance to patient recruitment and data management—CROs play a crucial role in navigating the stringent requirements that can often hinder the progress of medical innovations.
As the demand for clinical trials grows, particularly in regions like Latin America, the importance of selecting the right CRO becomes paramount. This article delves into the multifaceted role of CROs, the criteria for choosing the best fit for specific needs, and the advantages of conducting trials in diverse geographical locations, all while emphasizing the significance of regulatory compliance and inclusivity in research.
With insights into emerging trends such as technology and AI integration, the discussion highlights how these elements collectively shape the future of clinical research, ensuring more efficient pathways for bringing new therapies to market.
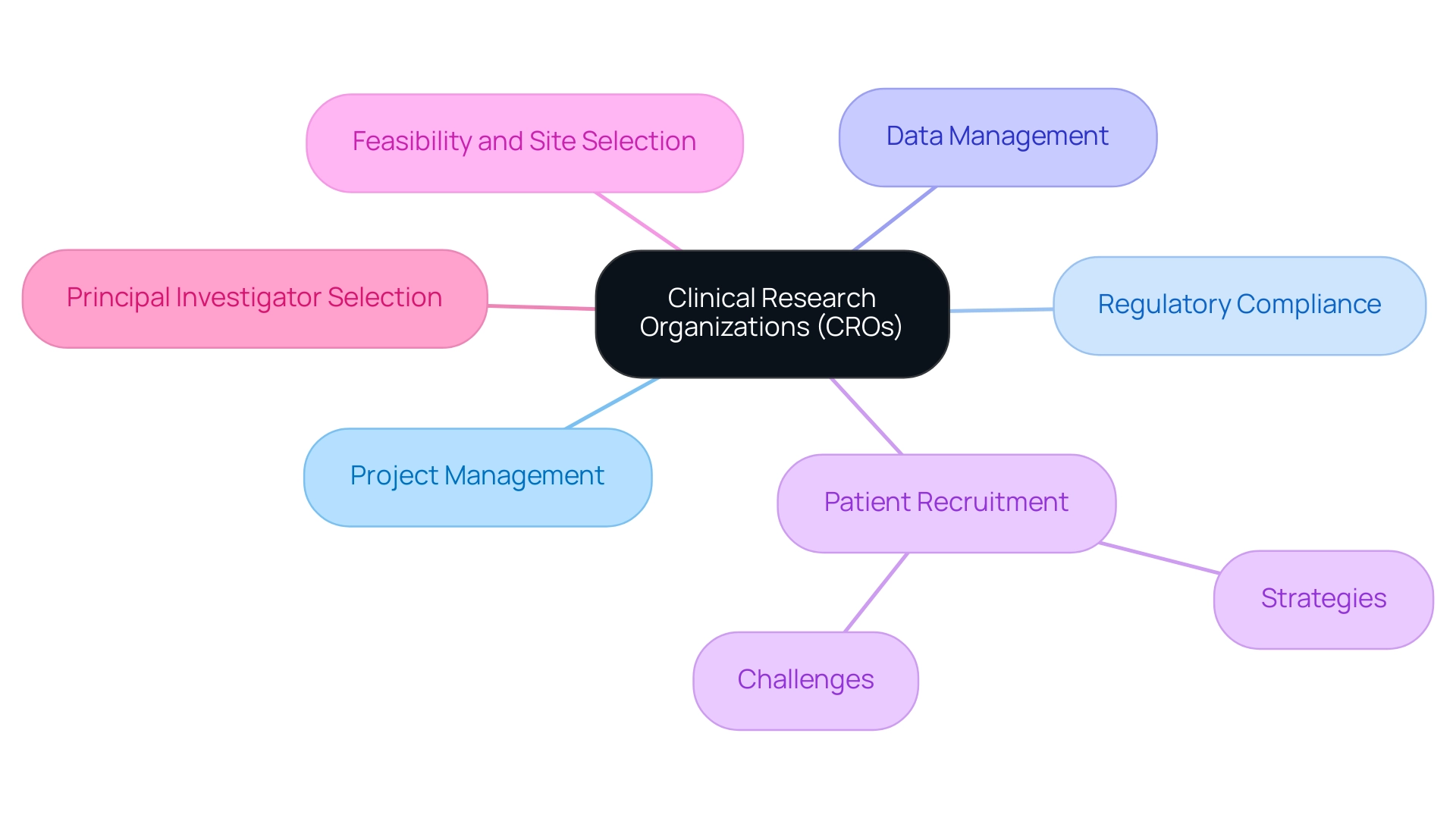
Understanding the Role of Clinical Research Organizations (CROs)
The largest clinical research organization in the world has become essential in the trial ecosystem, offering a comprehensive array of services that facilitate the effective management and execution of studies. They provide essential support to sponsors through various functions, including:
- Project management
- Regulatory compliance
- Data management
- Patient recruitment
- Feasibility and selection of research sites
- Principal investigator (PI) selection
Given the stringent regulatory requirements and high costs associated with research trials—challenges particularly acute for medical device startups such as regulatory hurdles, competition, recruitment issues, and financial constraints—CROs enable sponsors to navigate these complexities effectively.
Significantly, bioaccess™, in partnership with Caribbean Health Group, is striving to establish Barranquilla as a premier location for medical studies in Latin America, an initiative backed by Colombia's Minister of Health. This initiative aims to enhance the research study environment in the region while addressing the competitive and regulatory obstacles that can impede progress. Furthermore, partnerships like that of GlobalCare Clinical Trials with bioaccess™ have demonstrated tangible success, achieving over a 50% reduction in recruitment time and impressive 95% retention rates.
Reporting on study status, inventory, and serious and non-serious adverse events is also a critical component of the services provided by CROs. As the CRO market continues to expand—driven by a rise in studies and new drug approvals—sponsors must acknowledge the crucial role of the largest clinical research organization in the world in ensuring compliance and efficiency throughout the scientific investigation process. By outsourcing to a CRO, organizations can tap into specialized expertise, streamline their operations, and concentrate on their core business objectives, ultimately accelerating the timeline for bringing new therapies to market.
To explore how we can assist you further, BOOK A MEETING today.
Key Criteria for Selecting a CRO for Your Clinical Trials
Choosing a suitable Clinical Research Organization (CRO), particularly the largest clinical research organization in the world, is essential for the success of clinical studies, especially in the changing environment of global research. Key criteria to consider include:
-
Experience and Expertise: Prioritize CROs that demonstrate a robust track record in your specific therapeutic area, as experience can significantly influence study outcomes. For example, as of May 2023, 77% of registered studies are interventional, with 40% focusing on drugs or biologics.
This highlights the need for CROs adept in these sectors. Additionally, the clinical study success rate of only 33.4 percent for vaccines targeting infectious diseases highlights the importance of choosing the largest clinical research organization in the world.
-
Regulatory Knowledge: It’s essential that the CRO possesses comprehensive knowledge of the regulatory framework that governs your study, including compliance with local requirements such as those enforced by INVIMA in Colombia, which oversees medical device regulations as a Level 4 health authority by PAHO/WHO.
-
Resources and Capabilities: Evaluate the operational capacities of the largest clinical research organization in the world, focusing on their access to cutting-edge technology and the expertise of their personnel, which can greatly enhance efficiency. Their service capabilities should include:
- Feasibility assessments
- Site selection
- Compliance evaluations
- Setup of experiments—including the process of obtaining necessary approvals
- Reporting on project status, inventory, and serious and non-serious adverse events
-
Flexibility and Customization: Investigate whether the CRO can adapt their services to your unique trial requirements, providing tailored solutions that align with your specific goals.
-
Reputation and References: Gather insights from other sponsors regarding their experiences with the CRO. Feedback regarding reliability and performance can be invaluable in making your selection. Research indicates that satisfaction and performance ratings for over 30 CROs are accessible through Industry Standard Research reports, offering further guidance in your decision-making process.
As a reminder, findings from Google indicate that individuals with a negative experience on mobile sites are 62% less likely to buy from that brand in the future, which underscores the significance of user experience in CRO selection. Furthermore, understanding the types of registered studies, including the significant portion that are interventional, can guide your decision-making in selecting a CRO that aligns with your research goals while also considering the broader impact of medtech clinical studies on local economies.
Evaluating the Size and Capabilities of Leading CROs
Assessing the largest clinical research organization in the world requires a thorough analysis of their size and capabilities, as these elements greatly impact their efficiency in carrying out studies. The largest clinical research organization in the world typically boasts vast resources that encompass a global presence, diverse teams, and advanced technology platforms. This extensive network, as the largest clinical research organization in the world, can facilitate complex studies across multiple regions, ultimately accelerating the drug development process.
Conversely, smaller CROs often provide a more personalized approach, offering specialized expertise that can be advantageous for niche studies.
When assessing CROs, consider the following critical areas:
- Global Reach: Confirm whether the CRO has the infrastructure necessary to carry out studies in different countries. As emphasized by the World Health Organization (WHO), the count of medical studies recorded in Southeast Asia reached 11,030 in 2022, indicating a 48.5% increase from 2019. This underscores the importance of a CRO's ability to navigate diverse regulatory landscapes and local market dynamics. The rise in clinical experiments is anticipated to enhance the creation of new medications and stimulate expansion in the market for the largest clinical research organization in the world services throughout the forecast duration, as mentioned in the case analysis titled "Increase in Clinical Experiments and CRO Services Adoption."
- Service Capabilities: Assess the CRO's service offerings, which should encompass feasibility and selection of research locations and principal investigators (PIs), comprehensive review and feedback on research documents to ensure adherence to local regulations, setup and approval processes involving ethics committees and health ministries, import permits, and nationalization of investigational devices. Effective study project management and monitoring, alongside comprehensive reporting on study status and adverse events, are essential elements for successful study execution. Significantly, organizations like bioaccess® exemplify innovation and regulatory excellence in Latin America, enhancing the clinical study landscape.
- Staff Expertise: Assess the qualifications and experience of their research teams. A highly skilled team can significantly influence outcome results, ensuring adherence to protocols and regulatory requirements.
- Technology Utilization: Investigate the tools and platforms used for data management and monitoring. Advanced technology can streamline operations, improve data accuracy, and enhance overall efficiency.
- Capacity for Scalability: Ensure the CRO can adapt its operations to meet changing study demands. The growing number of research trials, particularly in cost-effective regions outside the U.S. and EU, is set to propel growth in the CRO services market. Organizations that can grow effectively will be better equipped to support the changing environment of medical studies.
By systematically assessing these areas, project directors can identify the largest clinical research organization in the world that aligns with their specific requirements, balancing the advantages of both large and small organizations. As the WHO highlights, grasping the dynamics of study expansion is essential in choosing the appropriate CRO to facilitate successful health outcomes. Moreover, the function of INVIMA as a Level 4 health authority by PAHO/WHO is crucial in guaranteeing adherence and supervision in medical studies within Colombia, emphasizing the significance of regulatory agencies in promoting an atmosphere favorable to scientific investigation.
Geographical Considerations: The Benefits of Latin America for Clinical Trials
Carrying out research studies in Latin America offers numerous strategic benefits that can greatly improve research results. The recent partnership between bioaccess™ and Caribbean Health Group, revealed on March 29, 2019, in Miami, FL, seeks to establish Barranquilla as a prominent location for medical research in the area, with backing from Colombia's Minister of Health. This initiative exemplifies how localized approaches are pivotal in conducting successful clinical studies in Latin America, as highlighted by H. Silva.
Moreover, the collaboration with GlobalCare Clinical Studies has proven effective, achieving over a 50% reduction in recruitment time and 95% retention rates, showcasing the potential for improved recruitment and retention in these studies. Additionally, the diverse patient populations across the region provide access to various demographics, enhancing the generalizability of research outcomes. Trials in this area often experience faster recruitment rates due to lower competition among research efforts, contributing to the reliability of the data collected.
The cost-effectiveness of conducting experiments here is notable, as operational expenses tend to be lower, resulting in significant savings for research budgets. Furthermore, many Latin American countries are improving their regulatory support, with streamlined processes that facilitate faster approvals and study initiations. Although disparities exist between countries regarding approval times and ethical oversight, the overall trend aligns with international standards.
Notably, Latinos are significantly underrepresented in US-based studies, with a median enrollment rate of only 6.0% compared to a census population of 16.3%, underscoring the necessity of engaging diverse populations. Lastly, collaborating with knowledgeable local Clinical Research Organizations (CROs), including the group of eight prominent healthcare institutions in Barranquilla that are part of the Caribbean Health Group, can significantly improve study execution and ensure adherence to regional regulations, especially when partnering with the largest clinical research organization in the world. These factors together place Latin America as an appealing option for research in 2024 and beyond.
Navigating Regulatory Compliance in Clinical Trials
Navigating regulatory compliance is essential for the success of clinical studies, and several key considerations must be prioritized:
- Understanding Local Regulations: It is imperative to thoroughly familiarize yourself with the regulations governing clinical studies in each country where the research will be conducted, especially in Colombia, where INVIMA serves as a Level 4 health authority overseeing medical devices and diagnostics.
- Ethics Committees and IRBs: Establishing strong relationships with local ethics committees and Institutional Review Boards (IRBs) is crucial for expediting study approvals. Engaging these bodies early can mitigate delays and enhance the likelihood of a favorable review.
- Adverse Event Reporting: Systems must be implemented to ensure that adverse events are reported promptly and in compliance with regulatory requirements, safeguarding participant safety and maintaining study integrity.
- Documentation and Record-Keeping: Maintaining meticulous records of all trial-related activities, including comprehensive documentation of protocol amendments and informed consent processes, is vital for demonstrating compliance during audits and inspections.
- Trial Setup and Import Permits: Effective trial setup and obtaining necessary import permits for investigational devices are critical steps that require thorough planning and adherence to regulatory standards.
- Training and Education: Ongoing training for all team members on regulatory requirements and best practices for compliance is essential. This is reflected in findings that 77% of corporate risk and compliance professionals consider staying informed on ESG developments as important, emphasizing the wider responsibility organizations hold in research. As noted by Saravanan, > 91% of business leaders believe their company has a responsibility to act on ESG issues <, which underscores the ethical dimensions of compliance.
- Leveraging Technology and Best Practices: Organizations must leverage technology and implement best practices to enhance compliance efficiency, ensuring that processes are streamlined and effective. The recent introduction of the estimand framework allows for tailored strategies in addressing various types of evidence gaps, reflecting the dynamic nature of regulatory challenges as we adapt to the ongoing pandemic. For instance, the expertise of professionals like Katherine Ruiz in Regulatory Affairs for medical devices and in vitro diagnostics in Colombia can be instrumental in navigating these complexities.
Moreover, the case analysis on managing absent information in medical studies illustrates the challenges presented by the pandemic, highlighting the necessity for strong strategies to evaluate patterns of missing data and utilize suitable statistical techniques. Through these measures, organizations can enhance compliance efficiency and promote ethical behavior in research studies.
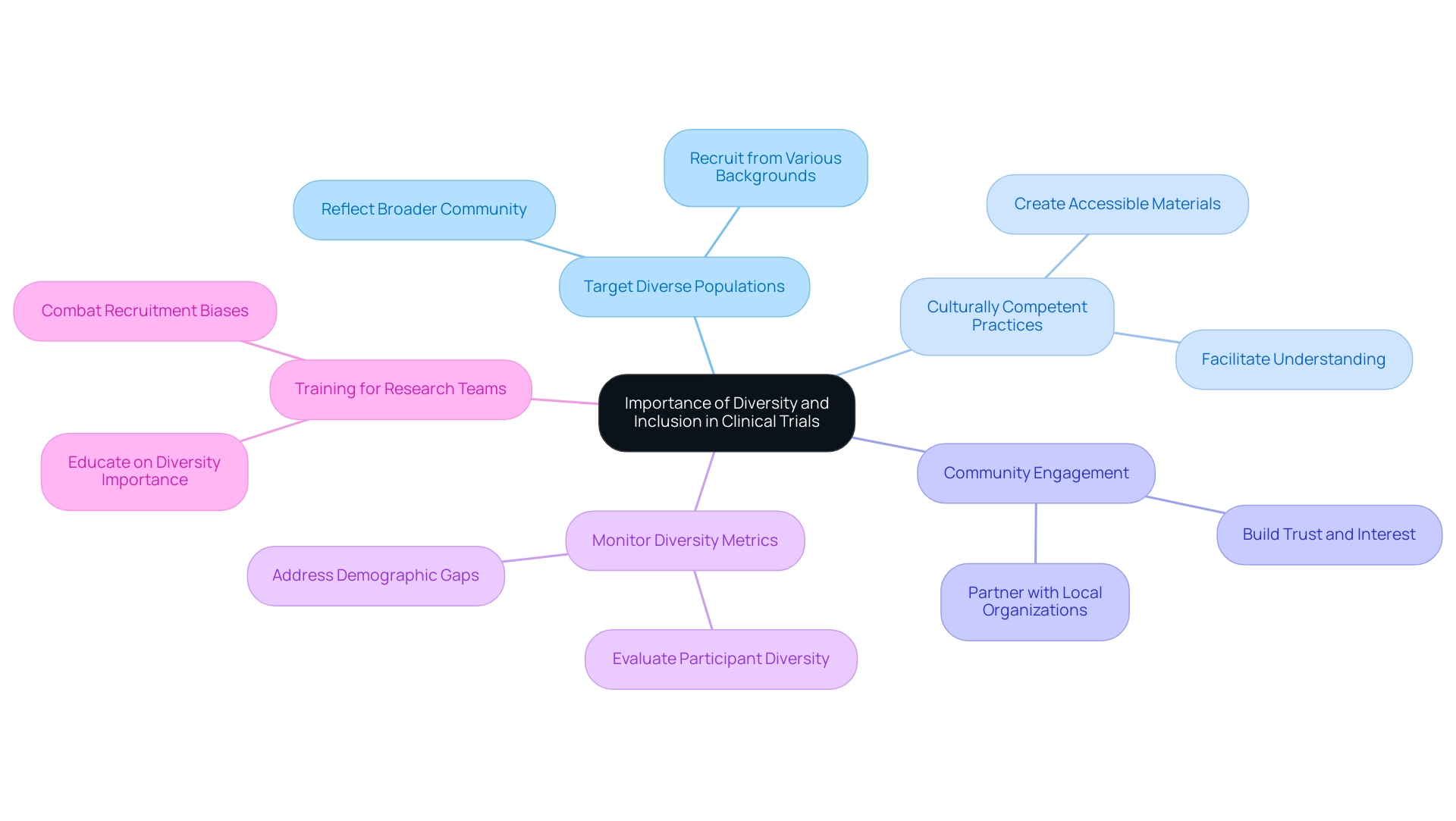
The Importance of Diversity and Inclusion in Clinical Trials
Diversity and inclusion in clinical studies are vital for generating research findings that are both representative and relevant across populations. For instance, in 2013, Phase 3 studies reported 64.2 percent females, while all studies reported just 44.3 percent females, highlighting the need for improved representation. To effectively promote diversity, consider implementing the following strategies:
- Target Diverse Populations: Focus on actively recruiting participants from a variety of ethnic, racial, and socioeconomic backgrounds to ensure that studies reflect the broader community.
- Culturally Competent Practices: Create materials and procedures that are culturally sensitive and accessible, facilitating better understanding and participation among diverse groups.
- Community Engagement: Partner with local organizations to increase awareness and promote involvement from underrepresented communities, building trust and interest in research studies.
- Monitor Diversity Metrics: Regularly evaluate and report the diversity of participants to ensure adherence to inclusion goals, thereby addressing the significant gaps in demographic data that persist, particularly concerning race and ethnicity.
- Training for Research Teams: Equip all research team members with training focused on the importance of diversity and inclusion, as this knowledge is essential in combating biases that may hinder recruitment efforts. As emphasized by Singh, there are numerous research efforts indicating negative biases against African Americans and Latinos in accessing care, which can extend to their recruitment in experiments.
Furthermore, collaborating with patient advocates early in the study design phase can offer insights into the needs of varied patient communities and enhance involvement in research studies. By prioritizing these strategies, organizations can enhance scientific progress and treatment options for all patients, leading to more equitable healthcare outcomes.
Future Trends: The Role of Technology and AI in Clinical Research
The incorporation of technology and artificial intelligence (AI) in clinical research is fundamentally transforming the landscape of clinical studies, particularly in Latin America. Several key trends are emerging:
- Data Analytics: The application of AI to analyze extensive datasets has proven to enhance patient recruitment and retention strategies significantly, with organizations increasingly leveraging this technology to identify suitable candidates efficiently.
- Remote Monitoring: The advent of remote monitoring tools facilitates real-time oversight of study activities, improving compliance and reducing the burden on participants.
This is critical as the market for AI in pharma and biotech is experiencing rapid growth, signaling a promising future for the industry.
- Patient Engagement Tools: Digital platforms are essential in improving participant involvement and ensuring compliance with research protocols, which is crucial for success.
- Predictive Modeling: With AI's capabilities in predictive modeling, researchers can forecast outcomes and enhance study designs using historical data, optimizing the process.
- Blockchain for Data Integrity: The use of blockchain technology provides strong data security and integrity, guaranteeing that study results are verifiable and reliable.
Furthermore, comprehensive management services for studies, including feasibility assessments, site selection, compliance evaluations, setup, and project management, are crucial to navigate the intricate landscape of medical investigations in Latin America. For instance, the setup process involves meticulous planning and coordination with ethics committees and health ministries to secure necessary approvals, while compliance reviews ensure adherence to local regulations. Dr. Sergio Alvarado, a Clinical Trial Manager dedicated to innovative medical studies and artificial intelligence, exemplifies the leadership required to connect gaps in medical exploration and innovation.
Effective partnerships, like those between Greenlight Guru and bioaccess™, further enhance Medtech innovations and research in Latin America, underscored by PAVmed's first-in-human study in Colombia. As these trends progress, the future of technology and AI in clinical research looks increasingly promising, paving the way for more efficient and effective clinical trials.
Conclusion
The role of Clinical Research Organizations (CROs) in the clinical trial ecosystem is increasingly pivotal, especially as the demand for efficient and compliant research grows. By providing a comprehensive suite of services—from regulatory compliance to patient recruitment—CROs enable sponsors to navigate the complex landscape of clinical trials effectively. Selecting the right CRO is crucial, requiring careful consideration of:
- Experience
- Regulatory knowledge
- Operational capabilities
The collaboration between local entities, such as bioaccess™ and Caribbean Health Group, exemplifies the strategic advantages of conducting trials in regions like Latin America, where diverse patient populations and streamlined regulatory processes can enhance research outcomes.
As the industry evolves, embracing diversity and inclusion within clinical trials is essential for generating relevant and representative findings. Implementing targeted recruitment strategies and culturally competent practices can help bridge gaps in representation, ultimately leading to equitable healthcare outcomes. Furthermore, the integration of technology and AI is transforming clinical research, facilitating better patient engagement and optimizing trial designs through data analytics and predictive modeling.
In conclusion, the future of clinical trials is shaped by the collaborative efforts of CROs, the strategic advantages of conducting research in diverse geographical locations, and the adoption of innovative technologies. By prioritizing regulatory compliance, inclusivity, and technological advancements, the clinical research community can accelerate the development of new therapies, ensuring that they are safe, effective, and accessible to all populations.
Frequently Asked Questions
What services do the largest clinical research organizations (CROs) provide?
The largest CROs offer a comprehensive array of services including project management, regulatory compliance, data management, patient recruitment, feasibility and selection of research sites, and principal investigator (PI) selection.
Why are CROs important for medical device startups?
CROs help medical device startups navigate stringent regulatory requirements, competition, recruitment issues, and financial constraints, enabling effective management and execution of research trials.
What initiative is bioaccess™ undertaking in Barranquilla, Colombia?
Bioaccess™, in partnership with Caribbean Health Group, aims to establish Barranquilla as a premier location for medical studies in Latin America, enhancing the research environment and addressing competitive and regulatory challenges.
How have partnerships like GlobalCare Clinical Trials with bioaccess™ been successful?
Such partnerships have achieved over a 50% reduction in recruitment time and impressive retention rates of 95%.
What is the role of CROs in reporting during clinical trials?
CROs are responsible for reporting on study status, inventory, and serious and non-serious adverse events, which are critical components of their services.
How do CROs help sponsors streamline their operations?
By outsourcing to a CRO, sponsors can tap into specialized expertise, enhance compliance and efficiency, and focus on their core business objectives, ultimately accelerating the timeline for bringing new therapies to market.
What criteria should be considered when choosing a CRO?
Key criteria include experience and expertise in the therapeutic area, regulatory knowledge, resources and capabilities, flexibility and customization of services, and reputation and references from other sponsors.
Why is regulatory knowledge important for a CRO?
Comprehensive knowledge of the regulatory framework governing a study is essential for compliance with local requirements, such as those enforced by INVIMA in Colombia.
How can the operational capabilities of a CRO enhance efficiency?
Access to cutting-edge technology and the expertise of personnel can significantly improve the efficiency of trial management, including feasibility assessments, site selection, compliance evaluations, and reporting.
What impact do user experiences on mobile sites have on CRO selection?
Negative experiences on mobile sites can lead to a 62% decrease in the likelihood of future purchases from that brand, highlighting the importance of user experience in CRO selection.




