Introduction
Navigating the complex landscape of medical device regulation is a critical endeavor for any organization aiming to enter this highly scrutinized market.
With authorities such as the FDA and EMA setting stringent guidelines, understanding the intricacies of regulatory requirements is paramount for success.
This article offers a comprehensive guide, detailing essential steps from classifying medical devices to implementing effective post-market surveillance strategies.
By engaging with key stakeholders and developing robust market access strategies, manufacturers can not only ensure compliance but also enhance the safety and efficacy of their products.
This exploration will equip industry professionals with the knowledge needed to thrive in a competitive environment while adhering to regulatory standards.
Understanding Regulatory Requirements for Medical Devices
Entering the medical equipment sector necessitates a thorough understanding of the regulatory framework established by authorities such as the FDA in the United States and the EMA in Europe. To facilitate a successful entry into the industry, consider the following structured approach:
-
Identify the Classification of Your Equipment: Establish whether your equipment falls into Class I, II, or III, as determined by its associated risk level. This classification significantly influences the regulatory pathway you must navigate.
- Class I: Generally categorized as low risk, these devices typically require only general controls.
- Class II: Devices classified under this category present moderate risk and generally necessitate premarket notification (510(k)).
- Class III: High-risk devices fall into this category, demanding premarket approval (PMA) to assure safety and efficacy before market entry.
-
Conduct a Pathway Analysis: Examine the specific compliance requirements relevant to your product's classification, including essential documentation and testing protocols. This is where the expertise of professionals like Ana Criado, Director of Compliance Affairs and CEO of Mahu Pharma, and Katherine Ruiz, a medical device and in vitro diagnostic compliance expert, can be invaluable. For instance, Ana's extensive experience with INVIMA and her consulting work with various global companies have equipped her with insights that can help navigate complex compliance challenges. Similarly, Katherine has successfully assisted foreign manufacturers in obtaining market clearance, demonstrating her practical knowledge of the compliance landscape.
-
Prepare Required Documentation: Compile all necessary documentation, which should encompass descriptions of the equipment, intended use, labeling, and, if applicable, clinical data to support your application.
-
Engage with Oversight Entities: It may be beneficial to request a pre-submission meeting with oversight authorities. This interaction can clarify expectations and provide valuable guidance regarding your submission process.
-
Submit Your Application: Complete the submission process meticulously, ensuring that all provided information is accurate and comprehensive to prevent delays.
-
Respond to Feedback: Be prepared to handle any questions or requests for extra details from oversight bodies promptly and effectively.
Importantly, the MHRA has implemented a transition phase for CE Marked products, lasting until 2028-2030, depending on the type of product. Moreover, guidance released on July 12, 2004, describes the regulation of healthcare instruments containing animal tissue, highlighting the necessity for adherence in this field. Furthermore, the recent guidance for interpreting sections 28 to 31, issued on January 12, 1999, provides essential context for understanding the governance framework.
Case studies, like the Guidance Document on the information needed by manufacturers for the reprocessing and sterilization of reusable health instruments, emphasize the significance of adherence to improve safety and effectiveness. This document outlines the essential details that manufacturers must supply, emphasizing its importance to the compliance process. By following these steps and being proactive about regulatory updates, you can effectively navigate the regulatory environment, ensuring your product complies with all necessary requirements for successful entry into the marketplace.
Implementing Effective Post-Market Surveillance Strategies
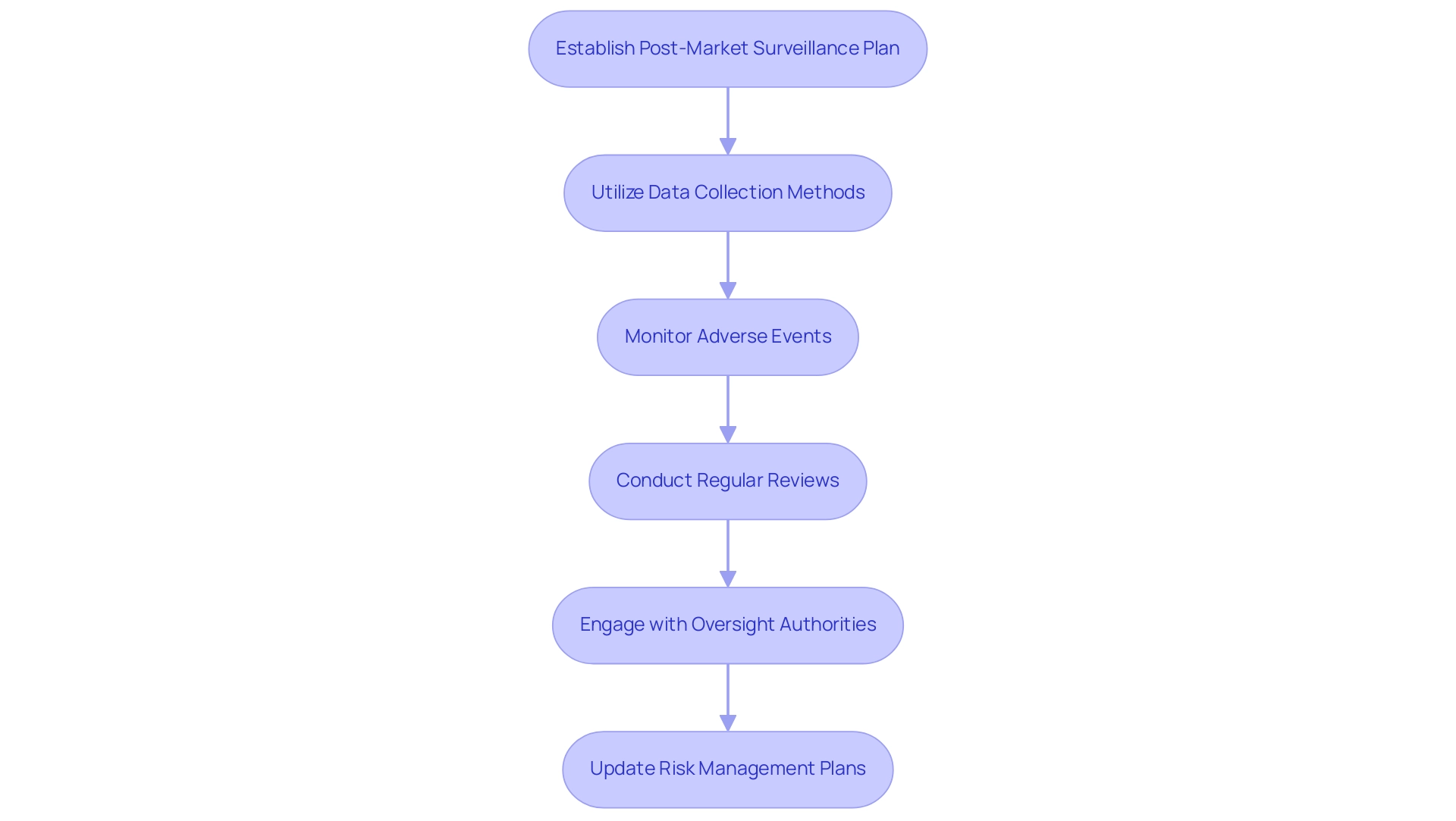
To ensure the ongoing safety and compliance of your healthcare product after market entry in Colombia, it is crucial to implement effective post-market surveillance strategies while adhering to INVIMA regulations. INVIMA, the Colombia National Food and Drug Surveillance Institute, is accountable for supervising health product marketing and production, including medical equipment, through its Directorate for Medical Equipment and Other Technologies. Its classification as a Level 4 health authority by PAHO/WHO underscores its competence in ensuring safety, efficacy, and quality in health regulation.
Here are key approaches to consider:
-
Establish a Post-Market Surveillance Plan: Develop a comprehensive strategy that details how you will continuously monitor the product’s performance and safety over time, in compliance with INVIMA's regulatory requirements.
-
Utilize Data Collection Methods: Implement diverse data collection approaches, including:
- User Feedback: Actively encourage healthcare professionals and patients to report any adverse events or issues encountered with the device. Creating an easy-to-use online portal for reporting can significantly increase the volume of feedback received, crucial for identifying potential risks.
- Clinical Registries: Engage in or create registries that systematically track device performance and patient outcomes, which facilitates a better understanding of real-world effectiveness and aligns with INVIMA’s monitoring practices.
- Surveys and Questionnaires: Distribute surveys to gather insights on user experience and device effectiveness, which can inform enhancements and safety measures.
-
Monitor Adverse Events: Establish a robust system for tracking and analyzing adverse events associated with your product. This should include a streamlined reporting mechanism for healthcare providers and patients, ensuring timely identification of issues, in accordance with INVIMA's expectations.
-
Conduct Regular Reviews: Schedule routine reviews of collected data to spot trends or emerging safety concerns. This proactive strategy allows for timely interventions if issues arise, particularly as research indicates that adverse event ICD-10 codes were underrecognized in 1.13% of cases in US mortality data, as highlighted in the case study titled 'Medical Adverse Events in the US 2018 Mortality Data'.
-
Engage with Oversight Authorities: Maintain an open line of communication with INVIMA and other governing bodies regarding your post-market surveillance findings and any necessary actions taken in response to identified adverse events.
-
Update Risk Management Plans: Regularly revise your risk management plans based on surveillance findings to ensure ongoing compliance and safety, incorporating the best practices and technical standards suggested by INVIMA.
Implementing these strategies will enhance the monitoring of your product's safety and effectiveness, thus ensuring continued regulatory compliance in Colombia and enabling Quick Market Entry Medical Devices to meet the needs of patients and healthcare providers. The importance of effective monitoring is further emphasized by recent findings that many adverse events remain underreported or misclassified, underscoring the need for comprehensive post-market surveillance.
Developing a Comprehensive Clinical Evaluation Plan
To develop a comprehensive Clinical Evaluation Plan, adhere to the following systematic steps:
- Define the Objectives: Articulate the specific objectives of the clinical evaluation, focusing on the key questions related to the safety and performance of the medical instrument. This foundation is crucial for guiding the evaluation process.
- Gather Existing Data: Conduct a thorough collection and analysis of existing clinical data relevant to your apparatus. This includes systematic literature reviews and insights from previous clinical studies, which provide a valuable context for your evaluation. Incorporating predictive distributions in Bayesian analysis can significantly enhance this step, as these distributions allow for the estimation of unobserved outcomes based on observed data, aiding in trial decisions.
- Identify Data Gaps: Critically assess the existing data to pinpoint any gaps that may necessitate additional clinical evidence to substantiate the device's safety and efficacy claims. Clearly identify the areas that require further investigation to ensure a robust evaluation. It is important to recognize that if 20 independent subgroups of a frequentist trial are tested at a Type I error level of 5%, the chance of at least one falsely significant result can be as high as 64%. This statistic underscores the need for rigorous data analysis to avoid misleading conclusions.
- Design Clinical Studies: Should additional data be required, meticulously design the necessary clinical studies. bioaccess® provides specialized services in Early-Feasibility Studies (EFS), First-In-Human Studies (FIH), Pilot Studies, and Pivotal Studies, ensuring adherence to requirements and ethical standards to uphold the integrity of the evaluation process. As the FDA suggests, it is essential to submit the program code and any data utilized to perform simulations as part of the IDE submission, highlighting compliance expectations.
- Implement the Plan: Execute the clinical evaluation plan as designed, ensuring that data is collected meticulously and according to the outlined protocols. bioaccess® provides comprehensive project management, trial setup, and monitoring services, maintaining thorough records to guarantee accuracy and adherence to compliance standards.
- Analyze and Report Findings: Upon completion of data collection, analyze the results comprehensively and prepare a detailed report summarizing the findings. This report will be crucial for compliance submissions and for illustrating the safety and effectiveness of the apparatus. The Bayesian approach, particularly through predictive distributions, can assist in handling missing data, providing a more robust analysis.
- Revise the Plan as Needed: Remain adaptable to changes in data availability or compliance requirements by adjusting your Clinical Evaluation Plan accordingly. This adaptability is essential to guaranteeing that the assessment stays pertinent and demanding.
By adhering to these steps to create a detailed Clinical Evaluation Plan, you will enable a comprehensive review of your product, thereby streamlining the approval process and improving the overall dependability of the evaluation. Additionally, referencing case studies that demonstrate the effectiveness of predictive distributions in Bayesian analysis and the regulatory oversight by INVIMA can provide real-world context and bolster the credibility of your evaluation approach.
Engaging Stakeholders and Building Collaborative Partnerships
To effectively engage stakeholders and foster collaborative partnerships in the medical device sector, consider implementing the following strategies:
- Identify Key Stakeholders: Clearly define who the key stakeholders are for your medical device project. This encompasses governing agencies such as INVIMA, healthcare providers, patient advocacy groups, and any other pertinent parties.
- Establish Communication Channels: Develop open lines of communication with stakeholders to facilitate ongoing information exchange and feedback. Frequent updates not only foster trust but also ensure all parties are aware of project advancements, particularly concerning compliance with INVIMA's guidelines.
- Involve Stakeholders Early: Engage stakeholders at the outset of the development process to gather valuable insights and address concerns proactively. Their input is vital in influencing the product and ensuring compliance with standards, including those established by INVIMA for medical equipment.
- Foster Collaborative Research: Pursue opportunities for joint research initiatives with academic institutions or healthcare organizations. Collaborative studies enhance the credibility of your product and provide additional data that can support its effectiveness and safety, ultimately contributing to job creation and economic growth in local economies.
- Attend Conferences and Workshops: Actively engage in industry conferences and workshops to network with stakeholders and remain informed about the latest trends and policy changes. These events are excellent platforms for building relationships and sharing knowledge, particularly about INVIMA's evolving guidelines.
- Solicit Feedback: Consistently seek feedback from stakeholders throughout the development process and regarding the performance of your device. This practice not only helps identify areas for improvement but also enhances the overall quality and compliance of the product, aligning with the standards expected by INVIMA.
- Implement a Structured Quality Management System (QMS): A structured QMS is essential for ensuring product safety, effectiveness, and adherence to regulations in medtech. It provides a framework for managing quality throughout the product lifecycle, which is critical in meeting both regulatory standards and stakeholder expectations. The QMS should include processes for review and feedback on study documents, trial set-up, start-up, and approval, ensuring that all aspects of the clinical trial management services are covered comprehensively.
By strategically involving stakeholders and fostering cooperative partnerships, you can significantly enhance your healthcare product initiative, thereby supporting quick market entry for medical devices. As Simon Mason aptly notes,
Speed is everything in business and in patient care. RWE is all about moving faster while maintaining safety and effectiveness.
Incorporating real-world evidence and stakeholder feedback can streamline submissions and enhance your time-to-market. For instance, as highlighted in the case study titled "Listening to Patients," actively incorporating patient feedback is fundamental to enhancing the patient experience and ensuring that the services provided align with the needs and expectations of all stakeholders.
Creating a Robust Market Access Strategy
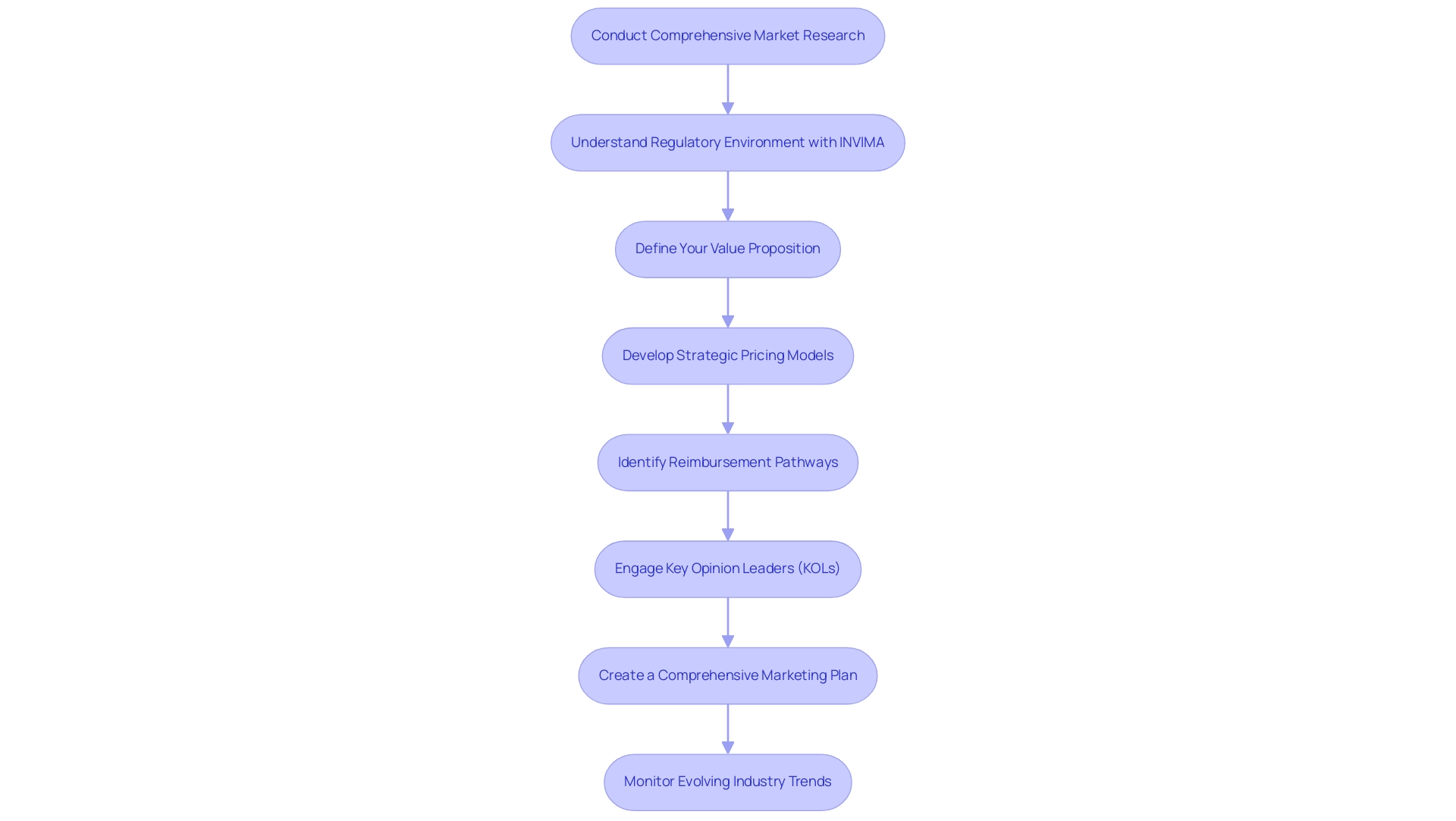
Creating a strong access strategy for your healthcare product involves several essential steps:
- Conduct Comprehensive Market Research: Analyze the competitive landscape, identify potential competitors, and understand the target demographics. This will also include reviewing current pricing strategies within the market, particularly in light of recent publications focusing on innovative licensing pathways and the economic burden of hemophilia A and B. Notably, a systematic literature review on this topic will be presented on November 17, 2024, in Barcelona, Spain, providing fresh insights into these economic challenges.
- Understand Regulatory Environment with INVIMA: Familiarize yourself with INVIMA, the Colombia National Food and Drug Surveillance Institute, which plays a crucial role in inspecting and supervising health products. Acknowledged as a Level 4 health authority by PAHO/WHO, INVIMA's supervision guarantees the safety, efficacy, and quality of healthcare products. The institute is responsible for monitoring and controlling medical equipment, suggesting technical standards, and evaluating compliance with health regulations. This understanding is vital for navigating the regulatory landscape and ensuring compliance.
- Define Your Value Proposition: It is essential to articulate the unique advantages of your product, highlighting how it addresses specific unmet demands in the industry. This clarity will aid in communicating the value to both stakeholders and potential users.
- Develop Strategic Pricing Models: Establish pricing that reflects the value of your product while being mindful of reimbursement policies and prevailing market conditions. Insights from healthcare economists can provide valuable perspectives on competitive yet sustainable pricing strategies.
- Identify Reimbursement Pathways: Investigate available reimbursement options for your equipment, including those from private insurers and government programs. Understanding the specific criteria for reimbursement is crucial to facilitate access in the healthcare system.
- Engage Key Opinion Leaders (KOLs): Collaborating with KOLs in the healthcare sector can significantly enhance the credibility of your product. Their endorsements can validate the clinical benefits, making a persuasive case for adoption by healthcare providers.
- Create a Comprehensive Marketing Plan: Develop a marketing strategy that clearly outlines how you will promote your product to both healthcare providers and patients. This may involve leveraging digital marketing, educational resources, and outreach programs to effectively communicate the advantages of your product.
- Monitor Evolving Industry Trends: Continuously track trends and be prepared to adapt your strategy in response to changes within the healthcare landscape. This proactive approach ensures your access strategy remains relevant and effective.
By implementing these strategies, you enhance the likelihood of successful entry for your quick market entry medical devices, ensuring it meets the needs of both patients and healthcare providers. Recent insights shared at events like ISPOR Europe 2024 highlight the significance of adapting to current trends and economic realities, further emphasizing the importance of a well-rounded access strategy. As Kati Copley-Merriman, Vice President of Value and Access, stated, 'Our researchers are happy to meet with you to show you how our integrated project teams can partner with you to help you get the most out of your real-world evidence.'
This collaboration can be crucial in navigating the complexities of market access strategies. Additionally, the systematic literature review on the economic burden of hemophilia A and B underscores the financial impacts on patients and healthcare systems, providing a real-world context for your strategy. Furthermore, conducting clinical studies in Colombia not only advances medical knowledge but also fosters local economic growth by creating jobs and improving healthcare, thus contributing to international collaboration.
Conclusion
Navigating the regulatory landscape for medical devices is an intricate process that demands careful attention to detail and a thorough understanding of various requirements. This article has outlined the essential steps for successfully entering the medical device market, including:
- Classifying devices according to risk levels
- Implementing effective post-market surveillance strategies
Engaging with regulatory authorities and maintaining open communication with stakeholders are pivotal in ensuring compliance and enhancing the safety and efficacy of medical devices.
Moreover, the development of a comprehensive clinical evaluation plan and robust market access strategy is critical for gaining the necessary approvals and facilitating successful market entry. By conducting thorough market research, defining clear value propositions, and establishing strategic partnerships, organizations can not only meet regulatory standards but also position their products competitively in the healthcare landscape.
In summary, the path to successfully launching a medical device is paved with challenges, yet it offers significant opportunities for innovation and improvement in patient care. Adhering to regulatory guidelines, fostering collaboration, and remaining responsive to market dynamics will ultimately empower manufacturers to thrive in this highly regulated environment. The commitment to compliance and proactive engagement with all stakeholders will ensure that medical devices not only meet regulatory requirements but also truly serve the needs of patients and healthcare providers alike.
Frequently Asked Questions
What is the first step to enter the medical equipment sector?
The first step is to identify the classification of your equipment, determining whether it falls into Class I, II, or III based on its associated risk level.
What are the classifications of medical devices?
Class I: Low risk, requiring only general controls. Class II: Moderate risk, requiring premarket notification (510(k)). Class III: High risk, requiring premarket approval (PMA) to ensure safety and efficacy.
Why is a pathway analysis important?
A pathway analysis is crucial to examine the specific compliance requirements for your product's classification, including necessary documentation and testing protocols.
What documentation is required for submitting an application?
Required documentation includes descriptions of the equipment, intended use, labeling, and clinical data if applicable.
How can engaging with oversight entities benefit the submission process?
Requesting a pre-submission meeting with oversight authorities can clarify expectations and provide guidance on the submission process.
What should be done after submitting the application?
Be prepared to respond promptly to any feedback or requests for additional information from oversight bodies.
What is the significance of the transition phase for CE Marked products by MHRA?
The MHRA has implemented a transition phase for CE Marked products that lasts until 2028-2030, depending on the type of product.
What is INVIMA's role in Colombia regarding medical devices?
INVIMA oversees health product marketing and production, ensuring safety, efficacy, and quality in health regulation.
What are key strategies for post-market surveillance?
Key strategies include establishing a post-market surveillance plan, utilizing data collection methods, monitoring adverse events, conducting regular reviews, and engaging with oversight authorities.
What is a Clinical Evaluation Plan?
A Clinical Evaluation Plan outlines the objectives, existing data, data gaps, study designs, implementation, analysis, and reporting of clinical evaluations for medical devices.
How can stakeholder engagement enhance medical device projects?
Engaging stakeholders early, establishing communication channels, and soliciting feedback can improve product development and compliance with standards.
What is the importance of market access strategies?
A comprehensive market access strategy enhances the likelihood of successful entry for medical devices, ensuring they meet the needs of patients and healthcare providers.
What should be included in a marketing plan for healthcare products?
A marketing plan should outline promotional strategies targeting healthcare providers and patients, including digital marketing and educational outreach.
How can collaboration with Key Opinion Leaders (KOLs) benefit a medical device?
Collaborating with KOLs enhances credibility and can validate the clinical benefits of the product, facilitating adoption by healthcare providers.




