Overview
To conduct medical device research in Peru, one must navigate the regulatory framework established by the Peruvian Ministry of Health and secure necessary registrations, ethics approvals, and compliance with local standards. The article outlines critical steps including understanding registration requirements, engaging with ethics committees, and staying informed about regulatory changes, all of which are essential for ensuring the success and integrity of medical device research in the country.
Introduction
Navigating the regulatory landscape for medical devices in Peru presents a unique set of challenges and opportunities for researchers and companies alike. With stringent requirements established by the Peruvian Ministry of Health and the National Institute of Health, understanding the intricacies of device registration, compliance with local standards, and ethical considerations is paramount.
This article delves into essential aspects of medical device research in Peru, including:
- The selection of an appropriate Clinical Research Organization (CRO)
- Conducting feasibility studies
- Designing effective clinical trial protocols
- Implementing robust recruitment strategies
By equipping stakeholders with comprehensive insights and practical guidance, this exploration aims to foster successful outcomes in the evolving Medtech environment, ultimately enhancing patient access to innovative therapies.
Navigating the Regulatory Landscape for Medical Devices in Peru
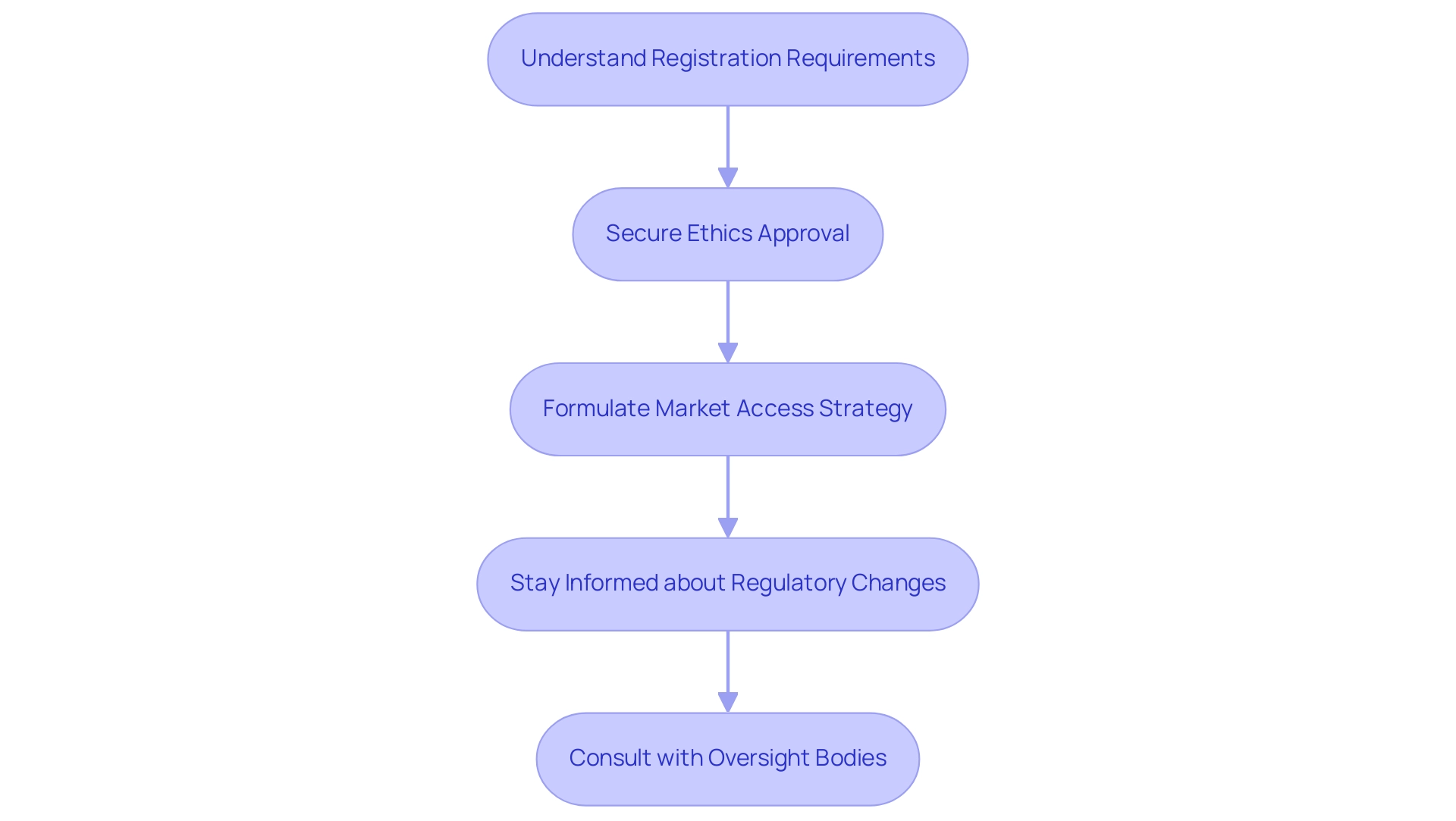
To successfully navigate the landscape of Medical Device Research Peru, it is essential to understand the regulatory framework established by the Peruvian Ministry of Health (MINSA) and the National Institute of Health (INS). Key considerations in Medical Device Research Peru include:
-
Understanding Registration Requirements: All medical products related to Medical Device Research Peru must be registered with the Directorate General of Medicines, Supplies, and Drugs (DIGEMID).
Assess the classification of your equipment to identify the appropriate documentation and approval pathway. It is crucial that your equipment adheres to the local safety and efficacy standards mandated by Peruvian regulations in the context of Medical Device Research Peru. This often necessitates conducting clinical trials to validate your claims, which bioaccess® can assist with through their comprehensive clinical trial management services for Medical Device Research Peru.
-
Securing ethics approval from an ethics committee prior to commencing any Medical Device Research Peru is paramount. This process safeguards the rights and welfare of participants involved in Medical Device Research Peru, ensuring ethical integrity in research. Formulating a robust market access strategy, which incorporates pricing and reimbursement considerations, is crucial for the commercial viability of your device in the context of Medical Device Research Peru.
-
Stay Informed: Given the dynamic nature of rules, it is essential to remain updated about any changes or modifications to the compliance landscape that may affect your Medical Device Research Peru projects. Regular consultation with oversight bodies, such as the Superintendency of National Health, can provide invaluable insights into the evolving requirements for Medical Device Research Peru.
Additionally, the National Authority for Pharmaceutical Products, Medical Devices and Medical Products (ANM) plays a crucial role in authorizing post-study access to investigational products related to Medical Device Research Peru when they demonstrate benefits. With a proven background of over 20 years in Medtech, bioaccess® offers tailored support in navigating the complexities of Medical Device Research Peru, including managing Early-Feasibility Studies (EFS), First-In-Human Studies (FIH), Pilot Studies, Pivotal Studies, and Post-Market Clinical Follow-Up Studies (PMCF). Our customized approach ensures that your unique needs are met throughout the clinical trial process.
For further inquiries, you may contact Ms. Ana Rojas of the Economics Office of the National Institute of Health at arojas@ins.gob.pe. Furthermore, drawing comparisons with the FDA's accelerated procedures for drug approval can demonstrate how regulatory structures can promote medical innovation and approval, enhancing patient access to groundbreaking therapies.
Choosing the Right Clinical Research Organization for Your Device
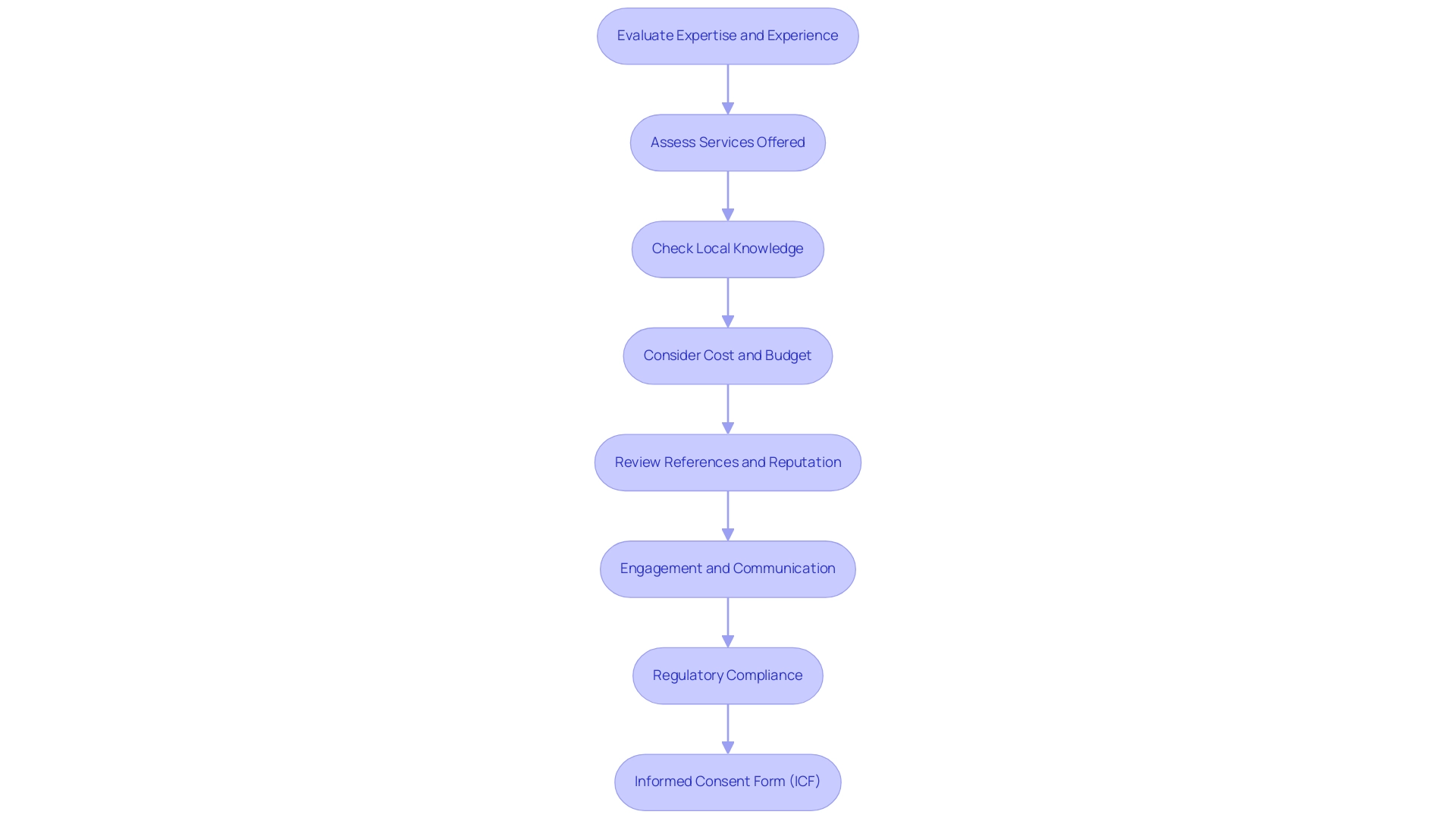
Choosing the appropriate Clinical Research Organization (CRO) for medical equipment studies in Peru entails several essential steps:
- Evaluate Expertise and Experience: Prioritize CROs with a robust track record in medical device research in Peru, particularly in the specific category of your device. Analyzing their past projects, including published results, can provide valuable insights into their capabilities and reliability. With over 20 years of experience, bioaccess® offers specialized knowledge in managing Early-Feasibility Studies (EFS), First-In-Human (FIH) studies, Pilot Studies, Pivotal Studies, and Post-Market Clinical Follow-Up Studies (PMCF).
- Assess Services Offered: CROs differ in the variety of services they offer, including everything from compliance assistance to comprehensive clinical trial management. Ensure that your selected CRO can fulfill all aspects of your study needs, including essential functions such as data management and biostatistics. Bioaccess® is equipped to handle the complete spectrum of clinical trial management services, ensuring a tailored approach to your project.
- Check Local Knowledge: The capacity to maneuver through the local governance landscape can greatly influence study efficiency. A CRO with strong local expertise will better understand the intricacies of conducting Medical Device Research in Peru, facilitating smoother processes and compliance. Katherine Ruiz, a specialist in regulatory matters for medical instruments and In Vitro Diagnostics in Colombia, has significant experience in navigating the regulatory environment, improving study outcomes in the region.
- Consider Cost and Budget: It’s imperative to obtain quotes from multiple CROs and compare their pricing structures. While aligning with your budget, also consider the quality of services they offer, as the cheapest option may not always provide the best value.
- Review References and Reputation: Engage with other researchers who have previously collaborated with potential CROs to assess their reputation and reliability. Such discussions can provide insights into the CRO's performance and help you make a more informed choice.
- Engagement and Communication: Opt for a CRO that prioritizes effective communication and collaboration. Strong engagement is vital for the successful execution of your project, ensuring that all stakeholders are aligned and informed throughout the process.
- Regulatory Compliance: Be aware that in cases of serious adverse events (SAE), serious adverse reactions (SAR), or suspected unexpected serious adverse reactions (SUSAR), the Principal Investigator (PI), sponsor, or CRO must notify the Drug and Health Surveillance Institute (DIIS) within seven calendar days. This compliance is essential for maintaining the integrity and safety of your study.
- Informed Consent Form (ICF): Ensure that the CRO understands the required elements of the Informed Consent Form (ICF), which must include trial title, sponsor information, trial rationale, expected risks, and participant rights. This structured approach ensures that participants receive all necessary information to make an informed decision about their participation.
Conducting Feasibility Studies
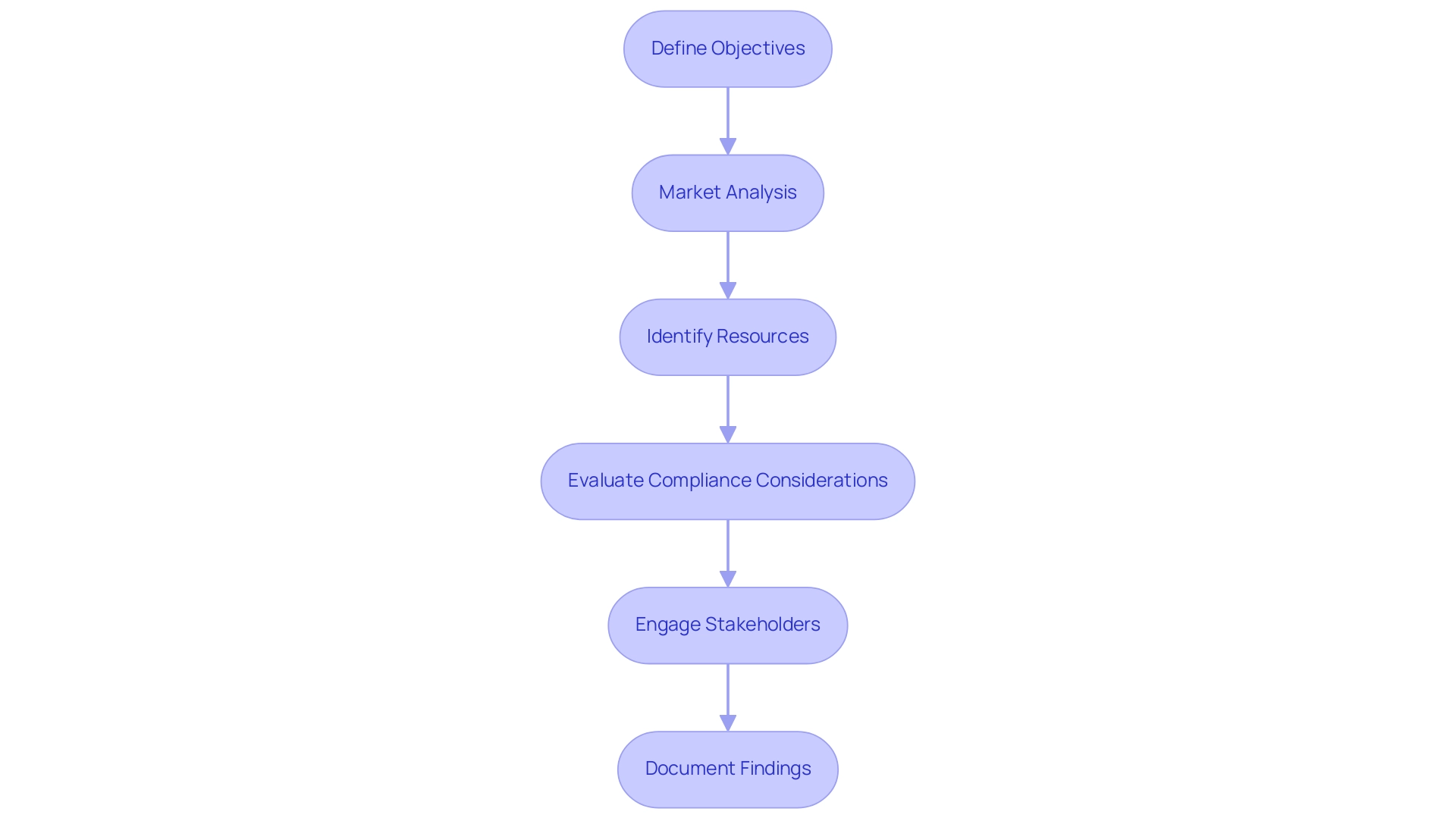
To effectively conduct a feasibility study for your medical device research in Peru, adhere to the following structured steps:
- Define Objectives: Establish clear, specific objectives for your research, detailing what you aim to accomplish with the instrument. This clarity will guide your entire study.
- Market Analysis: Conduct a comprehensive assessment of the market demand for your device. This includes analyzing potential competitors, understanding customer needs, and identifying gaps in the market. A robust market analysis is crucial for validating the significance of your Medical Device Research Peru study. Notably, 61% of U.S. adults have sought health or medical information online, underscoring the importance of digital engagement in assessing market demand.
- Identify Resources: Thoroughly evaluate the resources necessary for the study, including funding, personnel, and equipment. Ensure you have access to the necessary resources before proceeding with your study plan.
- Evaluate Compliance Considerations: Carefully review the oversight landscape that may affect your research design and timelines. Comprehending the compliance requirements of Medical Device Research Peru early in the process can facilitate smoother planning and execution. For instance, companies like Avantec Vascular successfully navigated challenges such as obtaining necessary approvals and addressing compliance issues with the support of bioaccess™ during their first-in-human clinical study in Latin America. bioaccess™ offered extensive services, including strategy development and trial management, highlighting the significance of expert guidance in compliance matters.
- Engage Stakeholders: Actively consult with stakeholders, including potential users, healthcare professionals, and regulatory bodies. As Pete Kiehart states, "Not convinced yet? Here, we share the top healthcare marketing statistics of 2024 to show how content marketing can help guide one through an increasingly-complicated landscape." Collecting insights and feedback from these parties is essential for improving your equipment and strategy.
- Document Findings: Compile your findings into a detailed feasibility report. This report should include a SWOT analysis, outlining the strengths, weaknesses, opportunities, and threats related to your research project. Documenting these findings not only aids in decision-making but also enhances communication with stakeholders. Moreover, it's important to mention that 1 out of 2 surveyed medtech companies reported at least a 20% return on investment from content marketing, emphasizing the effectiveness of digital strategies in the medical sector.
Designing the Clinical Trial Protocol
When designing a clinical trial protocol for medical devices, particularly in the evolving regulatory landscapes of Latin America, it is crucial to include the following components:
- Title and Background: Clearly articulate the trial's title and provide background information on the medical device, including its intended use and significance within the medical field.
- Objectives: Explicitly state the primary and secondary objectives of the trial. These objectives will act as a foundation for the project's design and anticipated outcomes.
- Study Design: Describe the chosen experimental framework, such as a randomized controlled trial or observational analysis, and justify this selection based on the project objectives.
- Participant Criteria: Define the inclusion and exclusion criteria for participant selection meticulously, ensuring that these criteria uphold ethical standards and scientific rigor. The dignity, safety, and welfare of research participants must be guaranteed, as emphasized in Decree 021-2017 and Decree 011-2011.
- Methodology: Outline the research methodology, detailing the procedures for data collection, specifics of the intervention, and follow-up plans.
- Statistical Analysis: Provide a comprehensive overview of the statistical methods intended for data analysis, including sample size calculations that ensure the research is adequately powered, in accordance with regulations that mandate a procedures manual for ethical committees. Ethical committees must have regulations and a procedures manual specifying procedures, internal regulations, and operational requirements.
- Ethical Considerations: Address ethical considerations thoroughly, including informed consent processes and measures to safeguard participant confidentiality. It is imperative to assess consent capacity and ensure that participants fully understand the provided information. As highlighted by Ana Rojas from the Economics Office of the National Institute of Health, "For any additional questions, send an email to Ms. Ana Rojas of the Economics Office of the National Institute of Health at arojas@ins.gob.pe."
- Timeline and Budget: Finally, present an estimated timeline for the study alongside a budget that outlines anticipated costs associated with the research, facilitating better planning and resource allocation throughout the trial.
Furthermore, the recent communication from the Peruvian Clinical Trials Registry (REPEC) regarding the suspension of administrative procedures due to COVID-19 highlights the necessity for researchers to remain adaptable to changes in regulations. By adhering to these structured components, researchers can navigate the complexities of regulatory environments in Latin America effectively, ensuring compliance, ethical integrity, and successful outcomes in clinical trials. Leveraging specialized expertise, such as that offered by bioaccess® in managing projects like Early-Feasibility Assessments (EFS) and First-In-Human Trials (FIH), further enhances the likelihood of navigating these challenges successfully.
Additionally, the flexibility of bioaccess® in adapting to changing regulations is crucial for maintaining research integrity and compliance.

Implementing Effective Recruitment Strategies
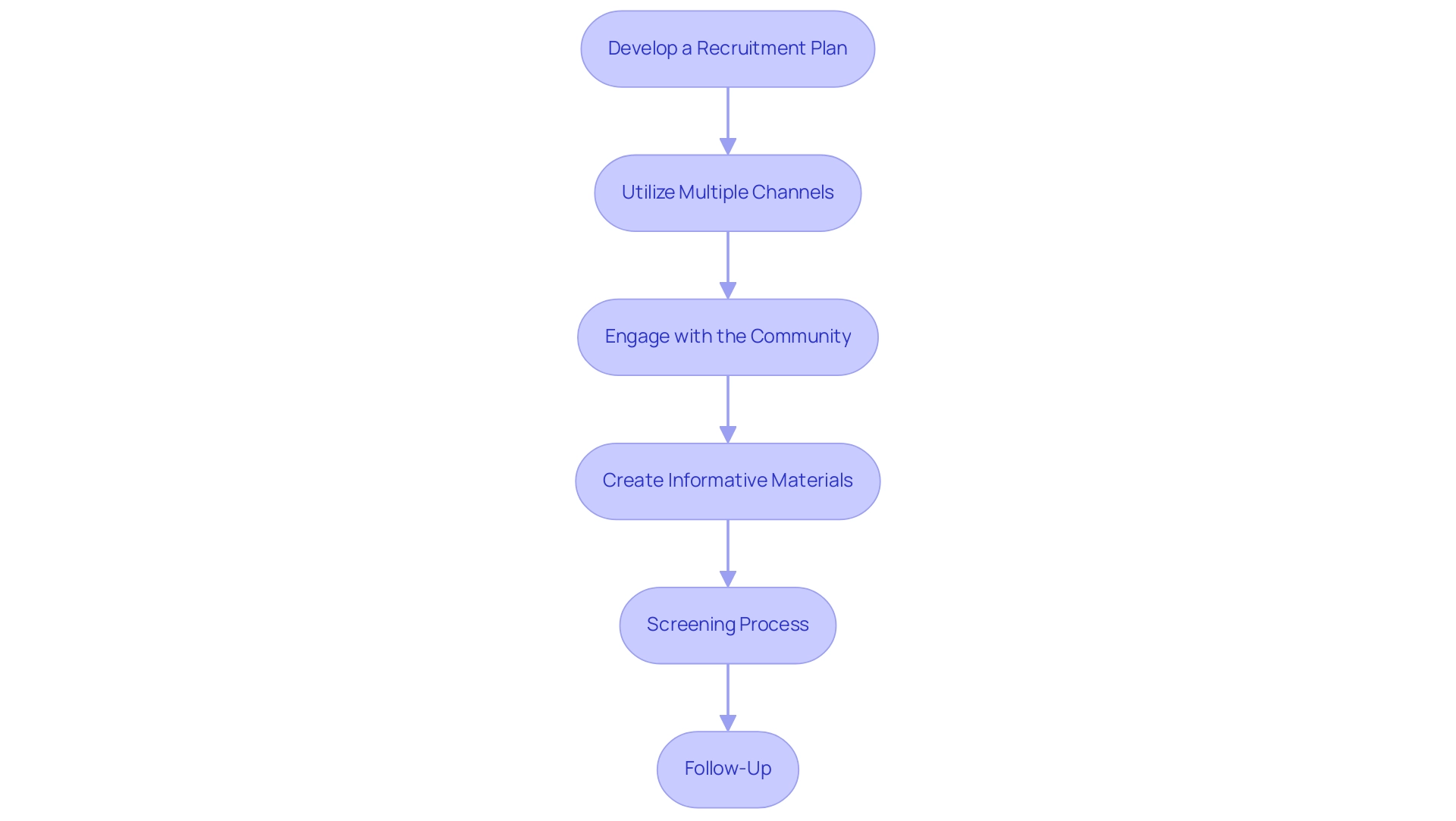
Implementing effective recruitment strategies for clinical trials in Peru is essential for Medical Device Research Peru, as it requires a comprehensive approach to tackle the unique challenges faced by Medtech companies in Latin America. Here are several key strategies to consider:
- Develop a Recruitment Plan: Formulate a robust recruitment plan that specifies your target population, outlines recruitment methods, and establishes clear timelines for each phase of the process. As Jane Smith, CFO, noted, "We expect significant growth next quarter," highlighting the need for effective strategies in clinical research, particularly in navigating the complexities of the regulatory environment.
- Utilize Multiple Channels: Leverage various recruitment channels to maximize reach. This encompasses social media platforms, community outreach initiatives, and referrals from healthcare providers, all of which can significantly boost participant awareness and interest in research, particularly Early-Feasibility and First-In-Human research, overseen by experts with over 20 years of experience in Medtech.
- Engage with the Community: Foster strong relationships with local healthcare providers and community organizations. Involving these groups is crucial for advancing your research and emphasizing its significance within the community, particularly considering the economic growth and healthcare enhancements that clinical trials can offer to the region.
- Create Informative Materials: Design clear and informative recruitment materials, such as brochures and flyers. These should effectively convey the project's purpose, procedures, and potential benefits, ensuring that prospective participants fully understand what participation entails, thus reinforcing the commitment to compliance and ethical standards.
- Screening Process: Implement a comprehensive screening process to verify that potential participants meet the inclusion criteria. This process should also ensure that they are well-informed about the project's requirements and implications. Additionally, if research is terminated early or temporarily suspended, remember that all relevant review bodies should be notified within 15 days to maintain compliance and communication.
- Follow-Up: Maintain open lines of communication with interested participants. Regular follow-ups can provide updates, address questions, and alleviate any concerns, thereby enhancing participant retention and engagement throughout the research, ultimately leading to successful outcomes in early-feasibility and first-in-human trials.
By adopting these strategies, researchers can significantly improve participant recruitment success rates in Medical Device Research Peru, ultimately contributing to the overall effectiveness of clinical trials. Moreover, drawing comparisons with the U.S. case analysis on labeling requirements for investigational products can strengthen the significance of compliance in recruitment strategies, bridging the gap between innovation and implementation in the Medtech landscape. The expertise of the bioaccess® team in managing these studies will be invaluable in navigating the regulatory complexities and ensuring successful outcomes.
Conclusion
Successfully navigating the regulatory landscape for medical devices in Peru requires a deep understanding of the intricate requirements set forth by the Peruvian Ministry of Health and the National Institute of Health. Key considerations include:
- Thorough registration processes
- Compliance with local standards
- Necessity of obtaining ethics approval prior to conducting clinical trials
A well-structured market access strategy is also essential, as it significantly influences the commercial viability of medical devices in this evolving market.
Choosing the right Clinical Research Organization (CRO) is paramount to the success of medical device research. Evaluating expertise, assessing services, and ensuring local knowledge are critical steps in selecting a CRO that can effectively navigate the regulatory environment. Furthermore, conducting feasibility studies with clear objectives and engaging stakeholders is vital for validating the relevance of research initiatives.
Designing robust clinical trial protocols that include:
- Ethical considerations
- Participant criteria
- Comprehensive methodologies
is crucial for maintaining compliance and ensuring the integrity of research. Implementing effective recruitment strategies, from developing a detailed recruitment plan to engaging with local communities, enhances participation and retention rates in clinical trials.
In conclusion, the complexities of the medical device regulatory landscape in Peru present both challenges and opportunities. By equipping stakeholders with the necessary knowledge and strategies outlined in this article, the potential for successful outcomes in clinical trials increases significantly. This, in turn, fosters patient access to innovative therapies, driving progress in the Medtech sector and ultimately improving healthcare outcomes within the region.
Frequently Asked Questions
What regulatory bodies oversee Medical Device Research in Peru?
The regulatory framework for Medical Device Research in Peru is established by the Peruvian Ministry of Health (MINSA) and the National Institute of Health (INS).
What are the registration requirements for medical devices in Peru?
All medical products related to Medical Device Research in Peru must be registered with the Directorate General of Medicines, Supplies, and Drugs (DIGEMID). It is important to assess the classification of your equipment to identify the necessary documentation and approval pathway.
Is ethics approval required for Medical Device Research in Peru?
Yes, securing ethics approval from an ethics committee is essential before commencing any Medical Device Research in Peru to safeguard the rights and welfare of participants.
How can I ensure my medical device is commercially viable in Peru?
Formulating a robust market access strategy that includes pricing and reimbursement considerations is crucial for the commercial viability of your device in the context of Medical Device Research in Peru.
How can I stay informed about changes in the regulatory landscape for Medical Device Research in Peru?
It is important to remain updated about any changes or modifications to compliance requirements by regularly consulting with oversight bodies like the Superintendency of National Health.
What role does the National Authority for Pharmaceutical Products, Medical Devices and Medical Products (ANM) play?
The ANM authorizes post-study access to investigational products related to Medical Device Research in Peru when they demonstrate benefits.
What types of studies does bioaccess® manage in Medical Device Research in Peru?
Bioaccess® manages various studies including Early-Feasibility Studies (EFS), First-In-Human Studies (FIH), Pilot Studies, Pivotal Studies, and Post-Market Clinical Follow-Up Studies (PMCF).
What should I consider when choosing a Clinical Research Organization (CRO) for medical equipment studies in Peru?
Evaluate the CRO's expertise, services offered, local knowledge, cost, references, communication, regulatory compliance, and understanding of the Informed Consent Form (ICF).
How important is local knowledge when selecting a CRO?
Strong local expertise can greatly influence study efficiency by facilitating smoother processes and compliance with local regulations.
What should I do in case of serious adverse events during the study?
The Principal Investigator (PI), sponsor, or CRO must notify the Drug and Health Surveillance Institute (DIIS) within seven calendar days of serious adverse events (SAE), serious adverse reactions (SAR), or suspected unexpected serious adverse reactions (SUSAR).
What elements must be included in the Informed Consent Form (ICF)?
The ICF must include the trial title, sponsor information, trial rationale, expected risks, and participant rights to ensure participants are fully informed about their participation.




